Gender and Intersecting Barriers and Facilitators to Access the HIV Cascade of Care in Manitoba, Canada, Before and During the COVID-19 Pandemic: A Qualitative Study
Abstract
1. Background
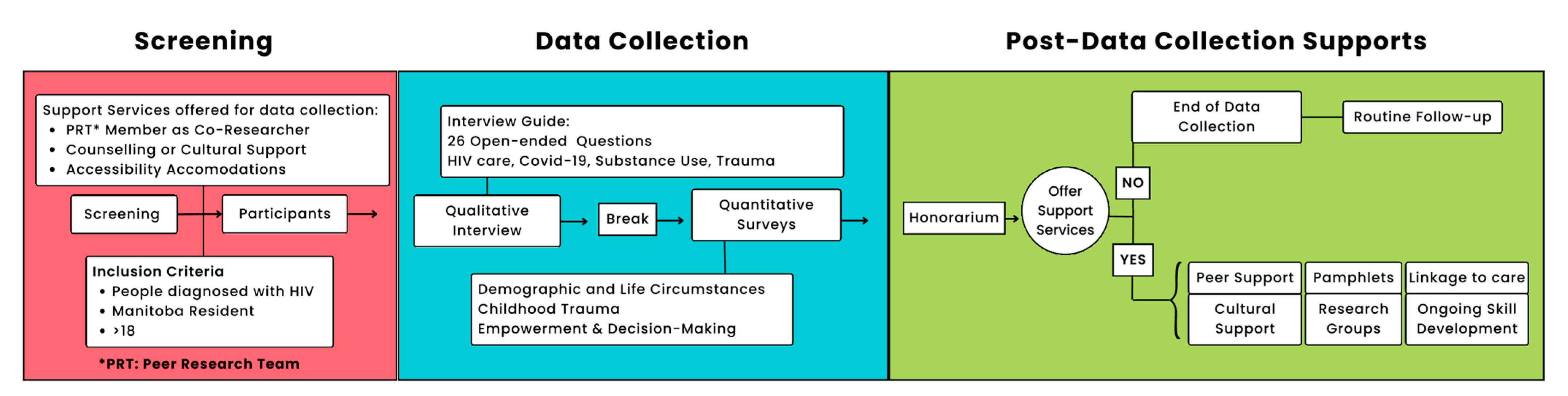
2. Materials and Methods
2.1. Ethics
2.2. Study Setting
2.3. Researchers Reflexivity
2.4. Participants
2.5. Data Collection
2.6. Data Analysis
3. Results
3.1. Participant Characteristics
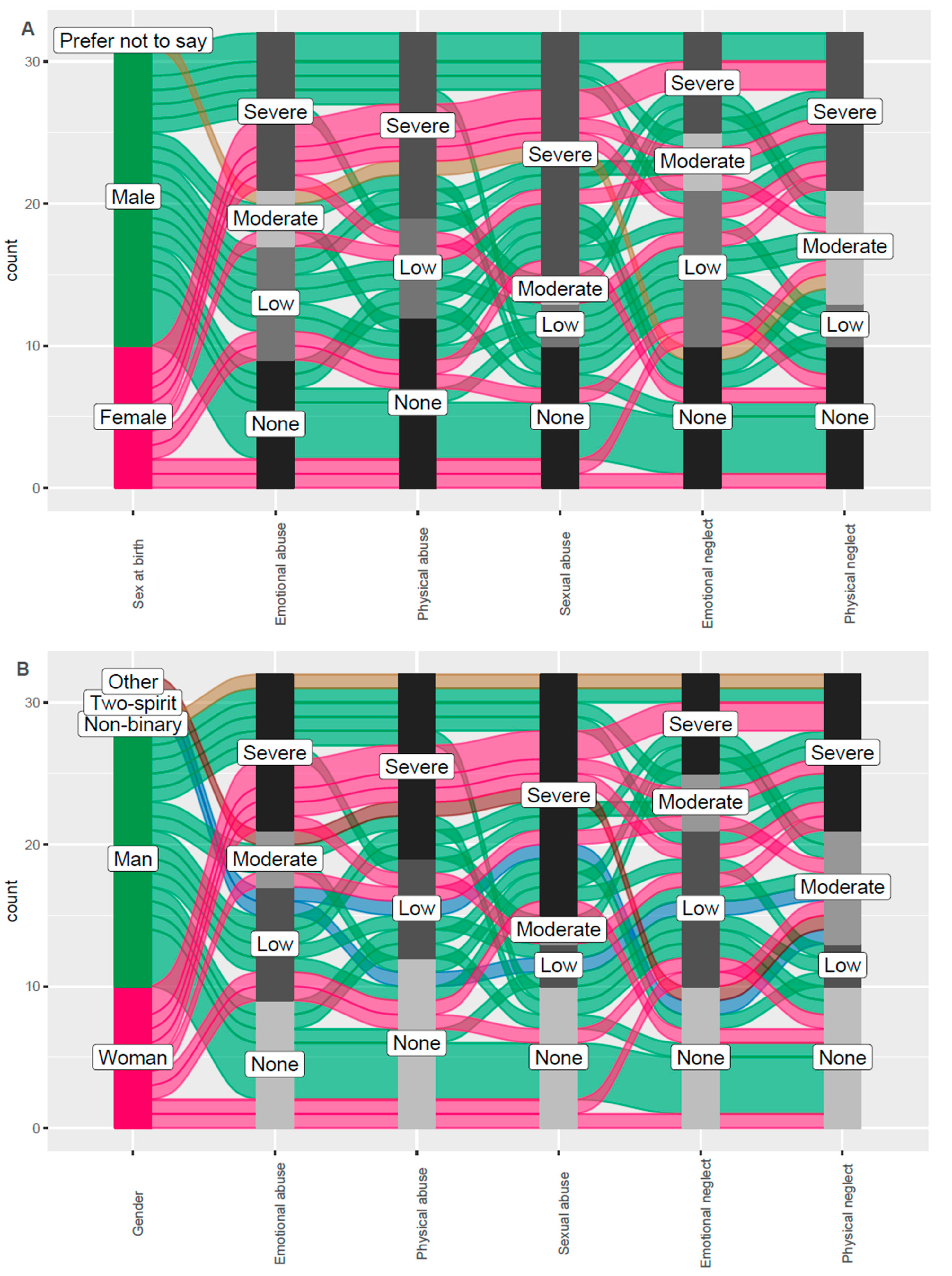
3.2. Childhood Trauma Questionnaire
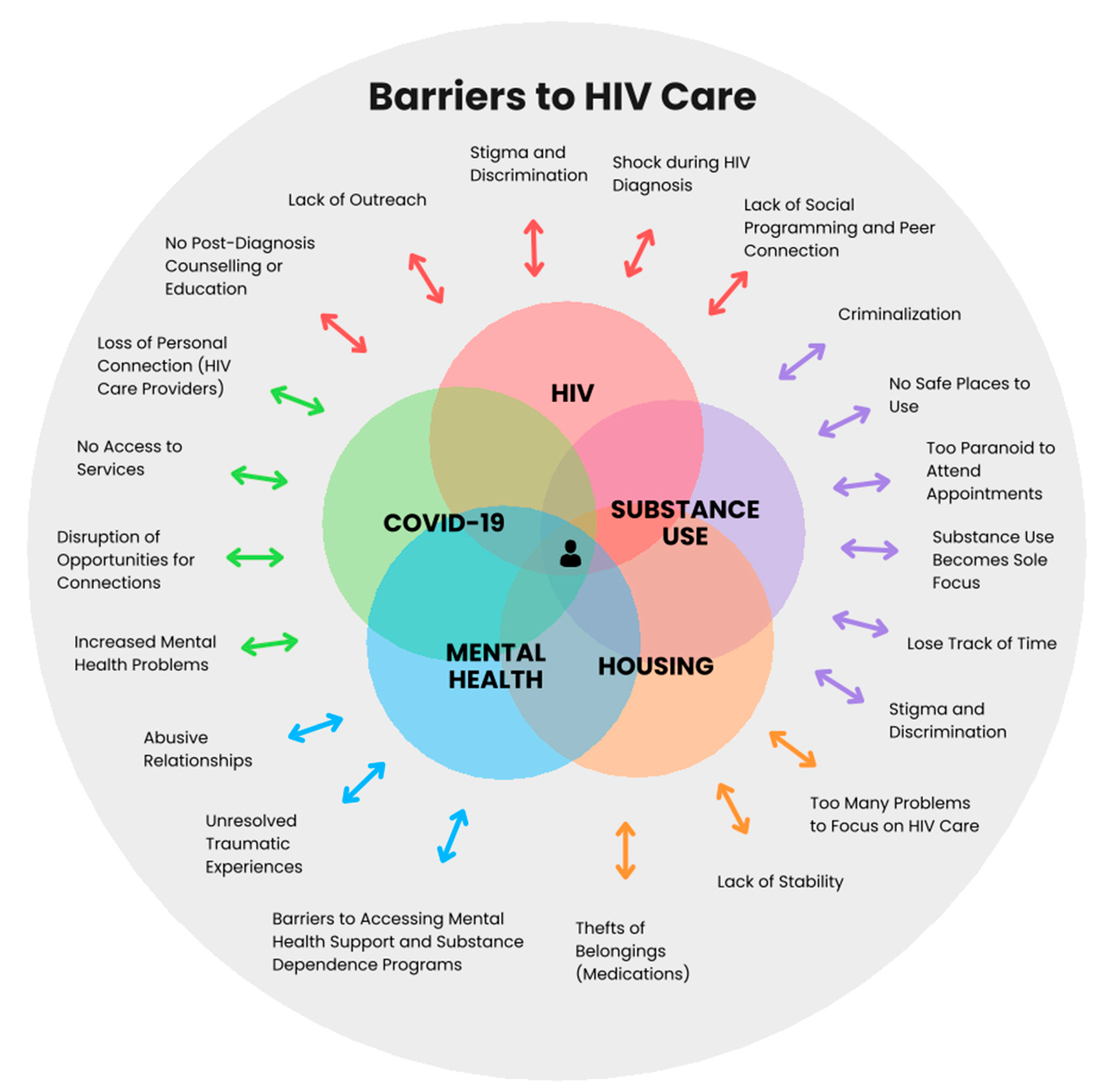
3.3. Barriers
3.3.1. Individual Factors
HIV Diagnosis
Mental Health Challenges
Substance Use Deterring HIV Care
COVID-19
Experiences of Violence
3.3.2. Healthcare Factors
Programmatic/Administrative
Lack of Follow-Up Care and Support During HIV Diagnosis
Compounded Stigma, Discrimination, and Insecurity in Health Settings
Lack of Social Supports
COVID-19
Lack of Prevention Strategies
Inaccessible Mental Health Services
3.3.3. Social and Structural Factors
Housing
Stigma and Discrimination
Lack of Social and Structural Supports
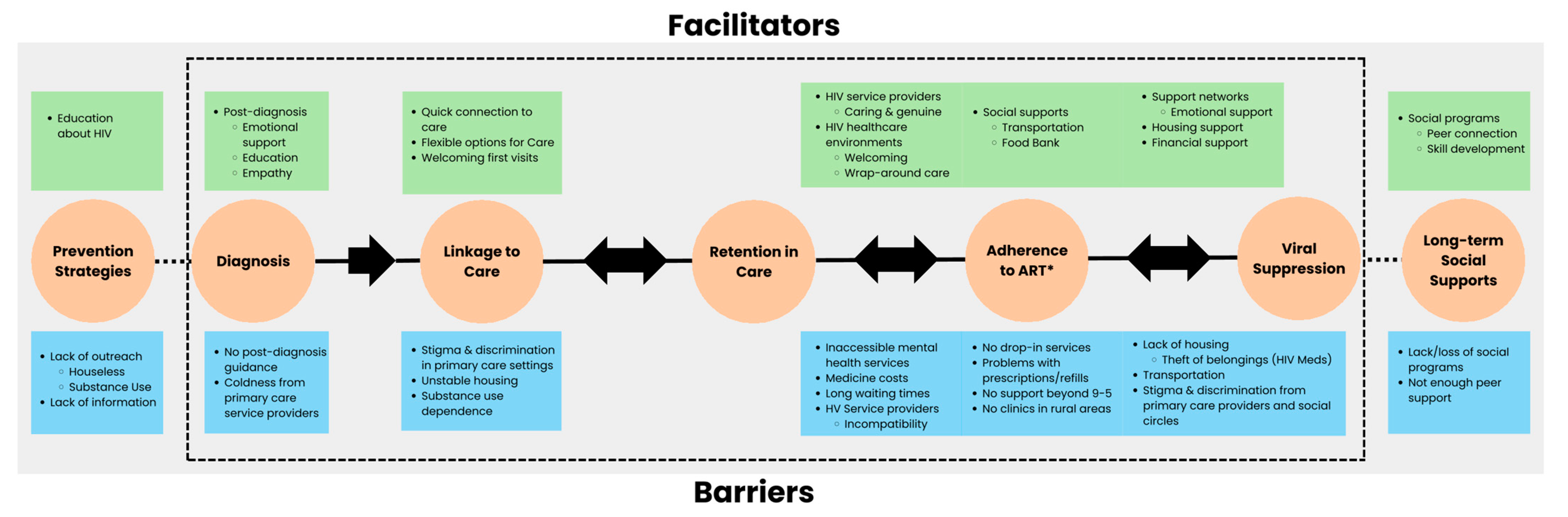
3.4. Facilitators
3.4.1. Individual Factors
Stopping Substance Use
Will to Survive
3.4.2. Healthcare Factors
HIV Service Providers
HIV Healthcare Environments
Social Supports
Post-HIV Diagnosis Emotional Support and Education
3.4.3. Social and Structural Factors
Support Networks
Structural Supports
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- UNAIDS Global HIV & AIDS Statistics 2023. Available online: https://www.unaids.org/en/resources/fact-sheet (accessed on 1 September 2023).
- Public Health Agency of Canada Estimates of HIV Incidence, Prevalence and Canada’s Progress on Meeting the 90-90-90 HIV Targets. 2020. Available online: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/estimates-hiv-incidence-prevalence-canada-meeting-90-90-90-targets-2020.html (accessed on 10 August 2023).
- Manitoba HIV Program Manitoba HIV Program Report 2018–2021. 2022. Available online: https://mbhiv.ca/wp-content/uploads/2022/11/Report-MB-HIV-Program-FINAL-Nov-30-2022-Reduced-size.pdf (accessed on 1 August 2023).
- Sharp, A.; Sorokopud-Jones, M.; Haworth-Brockman, M.; Kasper, K.; MacKenzie, L.; Ireland, L.; Gawlik, K.; Lopez, L.; Vanegas, J.M.; Bullard, J.; et al. Sex Differences in Houselessness, Injection Drug Use, and Mental Health Conditions among People Newly Diagnosed with HIV in Manitoba, Canada from 2018 to 2021: A Retrospective Cohort Study. Lancet Reg. Health–Am. 2024, 36, 100805. [Google Scholar] [CrossRef] [PubMed]
- Sorokopud-Jones, M.; Sharp, A.; Haworth-Brockman, M.; Kasper, K.; MacKenzie, L.; Ireland, L.; Gawlik, K.; Lopez, L.; Vanegas, J.M.; Bullard, J.; et al. Sexually Transmitted and Blood-Borne Infections by Sex, Methamphetamine Use, and Houselessness before, at, and after HIV Diagnosis in Manitoba, Canada. IJID Reg. 2024, 13, 100433. [Google Scholar] [CrossRef] [PubMed]
- Shiau, S.; Krause, K.; Valera, P.; Swaminathan, S.; Halkitis, P. The Burden of COVID-19 in People Living with HIV: A Syndemic Perspective. AIDS Behav. 2020, 24, 2244–2249. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada Focus on Geography Series, 2016 Census. Available online: https://www12.statcan.gc.ca/census-recensement/2016/as-sa/fogs-spg/Facts-PR-Eng.cfm?TOPIC=9&LANG=Eng&GK=PR&GC=46 (accessed on 27 July 2022).
- Brandon, J. The Winnipeg Street Census 2022: Final Report 2022. Available online: https://endhomelessnesswinnipeg.ca/street-census/ (accessed on 2 October 2023).
- Gabel, C.; Powell, A. The Future of Indigenous Healthcare in Manitoba: Moving Beyond Soft Reconciliation in Health. Int. Indig. Policy J. 2023, 14, 1–18. [Google Scholar] [CrossRef]
- Bromberg, D.J.; Mayer, K.H.; Altice, F.L. Identifying and Managing Infectious Disease Syndemics in Patients with HIV. Curr. Opin. HIV AIDS 2020, 15, 232. [Google Scholar] [CrossRef] [PubMed]
- Singer, M. A Dose of Drugs, a Touch of Violence, a Case of AIDS: Conceptualizing the Sava Syndemic. Free Inq. Creat. Sociol. 1996, 28, 13–24. [Google Scholar]
- Jain, J.P.; Strathdee, S.A.; Patterson, T.L.; Semple, S.J.; Harvey-Vera, A.; Magis-Rodríguez, C.; Martinez, G.; Pines, H.A. Perceived Barriers to Pre-Exposure Prophylaxis Use and the Role of Syndemic Factors among Female Sex Workers in the Mexico-United States Border Region: A Latent Class Analysis. AIDS Care 2020, 32, 557–566. [Google Scholar] [CrossRef]
- Rhodes, T.; Singer, M.; Bourgois, P.; Friedman, S.R.; Strathdee, S.A. The Social Structural Production of HIV Risk among Injecting Drug Users. Soc. Sci. Med. 2005, 61, 1026–1044. [Google Scholar] [CrossRef]
- Tyagi, M.; Bukrinsky, M.; Simon, G.L. Mechanisms of HIV Transcriptional Regulation by Drugs of Abuse. Curr. HIV Res. 2016, 14, 442–454. [Google Scholar] [CrossRef]
- Wang, L.-B.; Xu, L.-L.; Chen, L.-J.; Zhang, K.-K.; Zhang, Q.-Y.; Chen, Y.-K.; Li, J.-H.; Liu, J.-L.; Wang, Q.; Xie, X.-L. Methamphetamine Induces Intestinal Injury by Altering Gut Microbiota and Promoting Inflammation in Mice. Toxicol. Appl. Pharmacol. 2022, 443, 116011. [Google Scholar] [CrossRef]
- Li, Y.; Kong, D.; Bi, K.; Luo, H. Related Effects of Methamphetamine on the Intestinal Barrier via Cytokines, and Potential Mechanisms by Which Methamphetamine May Occur on the Brain-Gut Axis. Front. Med. 2022, 9, 783121. [Google Scholar] [CrossRef]
- Fulcher, J.A.; Shoptaw, S.; Makgoeng, S.B.; Elliott, J.; Ibarrondo, F.J.; Ragsdale, A.; Brookmeyer, R.; Anton, P.A.; Gorbach, P.M. Brief Report: Recent Methamphetamine Use Is Associated With Increased Rectal Mucosal Inflammatory Cytokines, Regardless of HIV-1 Serostatus. J. Acquir. Immune Defic. Syndr. 2018, 78, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, M.; Stanwick, T.L.; Dempsey, M.P.; Lamonica, C.A. HIV-1 Replication Is Controlled at the Level of T Cell Activation and Proviral Integration. EMBO J. 1990, 9, 1551–1560. [Google Scholar] [CrossRef] [PubMed]
- Carrico, A.W.; Flentje, A.; Kober, K.; Lee, S.; Hunt, P.; Riley, E.D.; Shoptaw, S.; Flowers, E.; Dilworth, S.E.; Pahwa, S.; et al. Recent Stimulant Use and Leukocyte Gene Expression In Methamphetamine Users with Treated HIV Infection. Brain Behav. Immun. 2018, 71, 108. [Google Scholar] [CrossRef] [PubMed]
- Massanella, M.; Gianella, S.; Schrier, R.; Dan, J.M.; Pérez-Santiago, J.; Oliveira, M.F.; Richman, D.D.; Little, S.J.; Benson, C.A.; Daar, E.S.; et al. Methamphetamine Use in HIV-Infected Individuals Affects T-Cell Function and Viral Outcome during Suppressive Antiretroviral Therapy. Sci. Rep. 2015, 5, 13179. [Google Scholar] [CrossRef] [PubMed]
- Walter, T.J.; Iudicello, J.; Cookson, D.R.; Franklin, D.; Tang, B.; Young, J.W.; Perry, W.; Ellis, R.; Heaton, R.K.; Grant, I.; et al. The Relationships between HIV-1 Infection, History of Methamphetamine Use Disorder, and Soluble Biomarkers in Blood and Cerebrospinal Fluid. Viruses 2021, 13, 1287. [Google Scholar] [CrossRef]
- Hobkirk, A.L.; Towe, S.L.; Lion, R.; Meade, C.S. Primary and Secondary HIV Prevention among Persons with Severe Mental Illness: Recent Findings. Curr. HIV/AIDS Rep. 2015, 12, 406–412. [Google Scholar] [CrossRef]
- Arranz, L.; de Vicente, A.; Muñoz, M.; De la Fuente, M. Impaired Immune Function in a Homeless Population with Stress-Related Disorders. Neuroimmunomodulation 2009, 16, 251–260. [Google Scholar] [CrossRef]
- Currie, L.B.; Patterson, M.L.; Moniruzzaman, A.; McCandless, L.C.; Somers, J.M. Examining the Relationship between Health-Related Need and the Receipt of Care by Participants Experiencing Homelessness and Mental Illness. BMC Health Serv. Res. 2014, 14, 404. [Google Scholar] [CrossRef]
- Holtzman, C.W.; Shea, J.A.; Glanz, K.; Jacobs, L.M.; Gross, R.; Hines, J.; Mounzer, K.; Samuel, R.; Metlay, J.P.; Yehia, B.R. Mapping Patient–Identified Barriers and Facilitators to Retention in HIV Care and Antiretroviral Therapy Adherence to Andersen’s Behavioral Model. AIDS Care 2015, 27, 817–828. [Google Scholar] [CrossRef]
- Pantelic, M.; Casale, M.; Cluver, L.; Toska, E.; Moshabela, M. Multiple Forms of Discrimination and Internalized Stigma Compromise Retention in HIV Care among Adolescents: Findings from a South African Cohort. J. Int. AIDS Soc. 2020, 23, e25488. [Google Scholar] [CrossRef] [PubMed]
- Yuvaraj, A.; Mahendra, V.S.; Chakrapani, V.; Yunihastuti, E.; Santella, A.J.; Ranauta, A.; Doughty, J. HIV and Stigma in the Healthcare Setting. Oral Dis. 2020, 26, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Laprise, C.; Bolster-Foucault, C. Understanding Barriers and Facilitators to HIV Testing in Canada from 2009-2019: A Systematic Mixed Studies Review. Can. Commun. Dis. Rep. Releve Mal. Transm. Au Can. 2021, 47, 105–125. [Google Scholar] [CrossRef] [PubMed]
- Gahagan, J.C.; Fuller, J.L.; Proctor-Simms, E.M.; Hatchette, T.F.; Baxter, L.N. Barriers to Gender-Equitable HIV Testing: Going beyond Routine Screening for Pregnant Women in Nova Scotia, Canada. Int. J. Equity Health 2011, 10, 18. [Google Scholar] [CrossRef]
- Khan, M.; MacEntee, K.; Kiptui, R.; Van Berkum, A.; Oudshoorn, A.; Ayuku, D.O.; Apondi, E.; Lee, E.O.J.; Abramovich, A.; MacDonald, S.-A.; et al. Barriers to and Facilitators of Accessing HIV Services for Street-Involved Youth in Canada and Kenya. BMC Public Health 2022, 22, 1901. [Google Scholar] [CrossRef]
- Liboro, R.M.; Bell, S.; Ranuschio, B.; Barnes, L.; Despres, J.; Sedere, A.; Puno, T.; Shuper, P.A. Barriers and Facilitators to Promoting Resilience to HIV/AIDS: A Qualitative Study on the Lived Experiences of HIV-Positive, Racial and Ethnic Minority, Middle-Aged and Older Men Who Have Sex with Men from Ontario, Canada. Int. J. Environ. Res. Public Health 2021, 18, 8084. [Google Scholar] [CrossRef]
- Rueda, Z.V.; Haworth-Brockman, M.; Sobie, C.; Villacis, E.; Larcombe, L.; Maier, K.; Deering, K.; Sanguins, J.; Templeton, K.; MacKenzie, L.; et al. Social and Structural Barriers and Facilitators to HIV Healthcare and Harm Reduction Services for People Experiencing Syndemics in Manitoba: Study Protocol. BMJ Open 2023, 13, e067813. [Google Scholar] [CrossRef]
- Singer, M.; Bulled, N.; Ostrach, B.; Mendenhall, E. Syndemics and the Biosocial Conception of Health. Lancet 2017, 389, 941–950. [Google Scholar] [CrossRef]
- Mendenhall, E.; Singer, M. What Constitutes a Syndemic? Methods, Contexts, and Framing from 2019. Curr. Opin. HIV AIDS 2020, 15, 213. [Google Scholar] [CrossRef]
- Mendenhall, E. Beyond Co-Morbidity: A Critical Anthropological Perspective of Syndemic Depression and Diabetes in Cross-Cultural Contexts. Med. Anthropol. Q. 2015, 30, 462. [Google Scholar] [CrossRef]
- Government of Canada, S.C. Focus on Geography Series, 2021 Census—Manitoba. Available online: https://www12.statcan.gc.ca/census-recensement/2021/as-sa/fogs-spg/Page.cfm?lang=E&topic=1&dguid=2021A000246 (accessed on 14 September 2024).
- Bernstein, D.; Stein, J.; Newcomb, M.; Walker, E.; Pogge, D.; Ahluvalia, T.; Stokes, J.; Handelsman, L.; Medrano, M.; Desmond, D.; et al. Development and Validation of a Brief Screening Version of the Childhood Trauma Questionnaire. Child Abus. Negl. 2003, 27, 169–190. [Google Scholar] [CrossRef] [PubMed]
- Rogers, E.S.; Ralph, R.O.; Salzer, M.S. Validating the Empowerment Scale with a Multisite Sample of Consumers of Mental Health Services. Psychiatr. Serv. Wash. DC 2010, 61, 933–936. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. A Conceptual Framework for Action on the Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Reflecting on Reflexive Thematic Analysis. Qual. Res. Sport Exerc. Health 2019, 11, 589–597. [Google Scholar] [CrossRef]
- Kohrt, B.A.; Worthman, C.M.; Adhikari, R.P.; Luitel, N.P.; Arevalo, J.M.G.; Ma, J.; McCreath, H.; Seeman, T.E.; Crimmins, E.M.; Cole, S.W. Psychological Resilience and the Gene Regulatory Impact of Posttraumatic Stress in Nepali Child Soldiers. Proc. Natl. Acad. Sci. USA 2016, 113, 8156–8161. [Google Scholar] [CrossRef]
- Cole, S.W.; Levine, M.E.; Arevalo, J.M.G.; Ma, J.; Weir, D.R.; Crimmins, E.M. Loneliness, Eudaimonia, and the Human Conserved Transcriptional Response to Adversity. Psychoneuroendocrinology 2015, 62, 11–17. [Google Scholar] [CrossRef]
- Seedat, S. Interventions to Improve Psychological Functioning and Health Outcomes of HIV-Infected Individuals with a History of Trauma or PTSD. Curr. HIV/AIDS Rep. 2012, 9, 344–350. [Google Scholar] [CrossRef]
- Leserman, J. Role of Depression, Stress, and Trauma in HIV Disease Progression. Psychosom. Med. 2008, 70, 539–545. [Google Scholar] [CrossRef]
- Remien, R.H.; Stirratt, M.J.; Nguyen, N.; Robbins, R.N.; Pala, A.N.; Mellins, C.A. Mental Health and HIV/AIDS: The Need for an Integrated Response. AIDS 2019, 33, 1411–1420. [Google Scholar] [CrossRef]
- Gilbert, L.; Raj, A.; Hien, D.; Stockman, J.; Terlikbayeva, A.; Wyatt, G. Targeting the SAVA (Substance Abuse, Violence and AIDS) Syndemic among Women and Girls: A Global Review of Epidemiology and Integrated Interventions. J. Acquir. Immune Defic. Syndr. 2015, 69, S118. [Google Scholar] [CrossRef]
- Trauma and Substance Abuse: Causes, Consequences, and Treatment of Comorbid Disorders; American Psychological Association: Washington, DC, USA, 2014; ISBN 978-1-4338-1523-2.
- Carrico, A.W. Substance Use and HIV Disease Progression in the HAART Era: Implications for the Primary Prevention of HIV. Life Sci. 2011, 88, 940–947. [Google Scholar] [CrossRef] [PubMed]
- Berg, R.C.; Page, S.; Øgård-Repål, A. The Effectiveness of Peer-Support for People Living with HIV: A Systematic Review and Meta-Analysis. PLoS ONE 2021, 16, e0252623. [Google Scholar] [CrossRef] [PubMed]
- Brezing, C.; Ferrara, M.; Freudenreich, O. The Syndemic Illness of HIV and Trauma: Implications for a Trauma-Informed Model of Care. Psychosomatics 2015, 56, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Larcombe, L.; Ringaert, L.; Restall, G.; McLeod, A.; Hydesmith, E.; Favel, A.; Morris, M.; Payne, M.; Souleymanov, R.; Keynan, Y.; et al. “Because of COVID…”: The Impacts of COVID-19 on First Nation People Accessing the HIV Cascade of Care in Manitoba, Canada. PLoS ONE 2023, 18, e0288984. [Google Scholar] [CrossRef] [PubMed]
- Bonn, M.; Palayew, A.; Bartlett, S.; Brothers, T.D.; Touesnard, N.; Tyndall, M. Addressing the Syndemic of HIV, Hepatitis C, Overdose, and COVID-19 Among People Who Use Drugs: The Potential Roles for Decriminalization and Safe Supply. J. Stud. Alcohol Drugs 2020, 81, 556–560. [Google Scholar] [CrossRef]
- Public Health Agency of Canada Survey of the Impact of COVID-19 on Access to STBBI-Related Health Services Including Harm Reduction Services Among People Who Use Drugs or Alcohol in Canada. Available online: https://health-infobase.canada.ca/datalab/covid-19-stbbi-services.html (accessed on 22 July 2022).
- McLinden, T.; Stover, S.; Hogg, R.S. HIV and Food Insecurity: A Syndemic Amid the COVID-19 Pandemic. AIDS Behav. 2020, 24, 2766–2769. [Google Scholar] [CrossRef]
- Spinelli, M.A.; Hickey, M.D.; Glidden, D.V.; Nguyen, J.Q.; Oskarsson, J.J.; Havlir, D.; Gandhi, M. Viral Suppression Rates in a Safety-Net HIV Clinic in San Francisco Destabilized during COVID-19. AIDS 2020, 34, 2328–2331. [Google Scholar] [CrossRef]
- Viswasam, N.; Schwartz, S.; Baral, S. Characterizing the Role of Intersecting Stigmas and Sustained Inequities in Driving HIV Syndemics Across Low- and Middle-Income Settings. Curr. Opin. HIV AIDS 2020, 15, 243. [Google Scholar] [CrossRef]
- Operario, D.; Sun, S.; Bermudez, A.N.; Masa, R.; Shangani, S.; van der Elst, E.; Sanders, E. Integrating HIV and Mental Health Interventions to Address a Global Syndemic among Men Who Have Sex with Men. Lancet HIV 2022, 9, e574–e584. [Google Scholar] [CrossRef]
- Smith, L.R.; Patel, V.V.; Tsai, A.C.; Mittal, M.L.; Quinn, K.; Earnshaw, V.A.; Poteat, T. Integrating Intersectional and Syndemic Frameworks for Ending the US HIV Epidemic. Am. J. Public Health 2022, 112, S340. [Google Scholar] [CrossRef]
- Laidley, J.; Tabbara, M. Welfare in Canada, 2022. Récupéré le 2023, 30. [Google Scholar]
- Saha, R.; Miller, A.P.; Parriott, A.; Horvath, H.; Kahn, J.G.; Malekinejad, M. Viral Blood-Borne Infections Testing and Linkage to Care Cascade among Persons Who Experience Homelessness in the United States: A Systematic Review and Meta-Analysis. BMC Public Health 2022, 22, 1421. [Google Scholar] [CrossRef] [PubMed]
- Riley, E.D.; Hickey, M.D.; Imbert, E.; Clemenzi-Allen, A.A.; Gandhi, M. Coronavirus Disease 2019 (COVID-19) and HIV Spotlight the United States Imperative for Permanent Affordable Housing. Clin. Infect. Dis. 2021, 72, 2042–2043. [Google Scholar] [CrossRef] [PubMed]
- Maggiolo, F.; Di Filippo, E.; Comi, L.; Callegaro, A.; Colombo, G.L.; Di Matteo, S.; Valsecchi, D.; Rizzi, M. Reduced Adherence to Antiretroviral Therapy Is Associated with Residual Low-Level Viremia. Pragmatic Obs. Res. 2017, 8, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Wood, E.; Hogg, R.S.; Yip, B.; Harrigan, P.R.; O’Shaughnessy, M.V.; Montaner, J.S.G. The Impact of Adherence on CD4 Cell Count Responses among HIV-Infected Patients. J. Acquir. Immune Defic. Syndr. 1999 2004, 35, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Abara, W.E.; Adekeye, O.A.; Xu, J.; Rust, G. Adherence to Combination Antiretroviral Treatment and Clinical Outcomes in a Medicaid Sample of Older HIV-Infected Adults. AIDS Care 2017, 29, 441–448. [Google Scholar] [CrossRef]
- Fielden, S.J.; Rusch, M.L.A.; Yip, B.; Wood, E.; Shannon, K.; Levy, A.R.; Montaner, J.S.G.; Hogg, R.S. Nonadherence Increases the Risk of Hospitalization among HIV-Infected Antiretroviral Naive Patients Started on HAART. J. Int. Assoc. Physicians AIDS Care 2008, 7, 238–244. [Google Scholar] [CrossRef]
- Castillo-Mancilla, J.R.; Cavassini, M.; Schneider, M.P.; Furrer, H.; Calmy, A.; Battegay, M.; Scanferla, G.; Bernasconi, E.; Günthard, H.F.; Glass, T.R.; et al. Association of Incomplete Adherence to Antiretroviral Therapy With Cardiovascular Events and Mortality in Virologically Suppressed Persons With HIV: The Swiss HIV Cohort Study. Open Forum Infect. Dis. 2021, 8, ofab032. [Google Scholar] [CrossRef]
- Glass, T.R.; Sterne, J.A.C.; Schneider, M.-P.; De Geest, S.; Nicca, D.; Furrer, H.; Günthard, H.F.; Bernasconi, E.; Calmy, A.; Rickenbach, M.; et al. Self-Reported Nonadherence to Antiretroviral Therapy as a Predictor of Viral Failure and Mortality. AIDS 2015, 29, 2195–2200. [Google Scholar] [CrossRef]
- Rajabiun, S.; Tryon, J.; Feaster, M.; Pan, A.; McKeithan, L.; Fortu, K.; Cabral, H.J.; Borne, D.; Altice, F.L. The Influence of Housing Status on the HIV Continuum of Care: Results From a Multisite Study of Patient Navigation Models to Build a Medical Home for People Living With HIV Experiencing Homelessness. Am. J. Public Health 2018, 108, S539–S545. [Google Scholar] [CrossRef]
- Padilla, M.; Carter, B.; Gutierrez, M.; Fagan, J. The Boundary of HIV Care: Barriers and Facilitators to Care Engagement Among People with HIV in the United States. AIDS Patient Care STDs 2022, 36, 321. [Google Scholar] [CrossRef]
- Kuchinad, K.E.; Hutton, H.E.; Monroe, A.K.; Anderson, G.; Moore, R.D.; Chander, G. A Qualitative Study of Barriers to and Facilitators of Optimal Engagement in Care among PLWH and Substance Use/Misuse. BMC Res. Notes 2016, 9, 229. [Google Scholar] [CrossRef] [PubMed]
- Yehia, B.R.; Stewart, L.; Momplaisir, F.; Mody, A.; Holtzman, C.W.; Jacobs, L.M.; Hines, J.; Mounzer, K.; Glanz, K.; Metlay, J.P.; et al. Barriers and Facilitators to Patient Retention in HIV Care. BMC Infect. Dis. 2015, 15, 246. [Google Scholar] [CrossRef] [PubMed]
- Carey, J.W.; Carnes, N.; Schoua-Glusberg, A.; Kenward, K.; Gelaude, D.; Denson, D.; Gall, E.; Randall, L.A.; Frew, P.M. Barriers and Facilitators for Clinical Care Engagement Among HIV-Positive African American and Latino Men Who Have Sex with Men. AIDS Patient Care STDs 2018, 32, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Taylor, B.S.; Fornos, L.; Tarbutton, J.; Muñoz, J.; Saber, J.A.; Bullock, D.; Villarreal, R.; Nijhawan, A.E. Improving HIV Care Engagement in the South from the Patient and Provider Perspective: The Role of Stigma, Social Support, and Shared Decision-Making. AIDS Patient Care STDs 2018, 32, 368–378. [Google Scholar] [CrossRef] [PubMed]
- Beima-Sofie, K.; Begnel, E.R.; Golden, M.R.; Moore, A.; Ramchandani, M.; Dombrowski, J.C. “It’s Me as a Person, Not Me the Disease”: Patient Perceptions of an HIV Care Model Designed to Engage Persons with Complex Needs. AIDS Patient Care STDs 2020, 34, 267–274. [Google Scholar] [CrossRef]
- Davoust, M.; Drainoni, M.-L.; Baughman, A.; Campos Rojo, M.; Estes, T.; Rajabiun, S.; Ross-Davis, K.; McCann, K.; Sullivan, M.; Todd, L.; et al. “He Gave Me Spirit and Hope”: Client Experiences with the Implementation of Community Health Worker Programs in HIV Care. AIDS Patient Care STDs 2021, 35, 318–326. [Google Scholar] [CrossRef]
- Buchbinder, S.P.; Havlir, D.V. Getting to Zero San Francisco: A Collective Impact Approach. J. Acquir. Immune Defic. Syndr. 2019, 82, S176–S182. [Google Scholar] [CrossRef]
- Crepaz, N.; Baack, B.N.; Higa, D.H.; Mullins, M.M. Effects of Integrated Interventions on Transmission Risk and Care Continuum Outcomes in Persons Living with HIV: Meta-Analysis, 1996–2014. AIDS 2015, 29, 2371–2383. [Google Scholar] [CrossRef]
- Krüsi, A.; Small, W.; Wood, E.; Kerr, T. An Integrated Supervised Injecting Program within a Care Facility for HIV-Positive Individuals: A Qualitative Evaluation. AIDS Care 2009, 21, 638–644. [Google Scholar] [CrossRef]
- Canada, H. Health Portfolio Sex and Gender-Based Analysis Policy. 2017. Available online: https://www.canada.ca/en/health-canada/corporate/transparency/heath-portfolio-sex-gender-based-analysis-policy.html (accessed on 5 December 2023).
- Scandurra, C.; Mezza, F.; Maldonato, N.M.; Bottone, M.; Bochicchio, V.; Valerio, P.; Vitelli, R. Health of Non-binary and Genderqueer People: A Systematic Review. Front. Psychol. 2019, 10, 1453. [Google Scholar] [CrossRef]
- Canadian Institutes of Health Research. Meet the Methods Series: “What and Who Is Two-Spirit?” in Health Research—CIHR. 2020. Available online: https://cihr-irsc.gc.ca/e/52214.html (accessed on 11 December 2023).
- Feyissa, G.T.; Woldie, M.; Munn, Z.; Lockwood, C. Exploration of facilitators and barriers to the implementation of a guideline to reduce HIV-related stigma and discrimination in the Ethiopian healthcare settings: A descriptive qualitative study. PLoS ONE 2019, 14, e0216887. [Google Scholar] [CrossRef] [PubMed]
- Gulliford, M.; Figueroa-Munoz, J.; Morgan, M.; Hughes, D.; Gibson, B.; Beech, R.; Hudson, M. What does “access to health care” mean? J. Health Serv. Res. Policy 2002, 7, 186–188. [Google Scholar] [CrossRef] [PubMed]
- Homeless Hub. Canadian Definition of Homelessness|The Homeless Hub. Available online: https://www.homelesshub.ca/resource/canadian-definition-homelessness (accessed on 5 December 2023).
| Variable (N: Participants Who Answered) | Frequency n (%) |
|---|---|
| Age in years (N = 32) | 44.03 years (24–63) |
| Mean (Range) | |
| Gender Identity (N = 32) | |
| Woman | 10 (31.3) |
| Man | 18 (56.3) |
| Trans Woman | 0 |
| Trans Man | 0 |
| Non-Binary | 1 (3.1) |
| Two-Spirit | 2 (6.3) |
| Other | 1 (3.1) |
| Prefer not to say | 0 |
| Sex (N = 32) | |
| Male | 21 (65.6) |
| Female | 10 (31.3) |
| Intersex | 0 |
| Prefer not to say | 1 (3.1) |
| Sexual Orientation (N = 32) | |
| Lesbian | 0 |
| Gay | 8 (25) |
| Bisexual | 6 (18.8) |
| Asexual | 0 |
| Heterosexual | 15 (46.9) |
| Pansexual | 0 |
| Other | 2 (6.3) |
| Prefer not to say | 1 (3.1) |
| Cultural Background (N = 32) | |
| Indigenous–First Nations | 15 (46.9) |
| Indigenous–Métis | 4 (12.5) |
| White/European | 4 (12.5) |
| Southeast Asian | 4 (12.5) |
| Other | 5 (15.6) |
| Marital Status (N = 27) | |
| Single | 18 (56.3) |
| Married | 0 |
| Divorced | 2 (6.3) |
| Common Law | 7 (21.9) |
| Widowed | 0 |
| Other | 0 |
| Highest Level of Education (N = 30) | |
| K-12 | 21 (65.6) |
| Certificate, Diploma, vocational course from an | 6 (18.8) |
| educational institution | |
| Bachelor’s Degree | 3 (9.4) |
| Master’s Degree | 0 |
| Doctorate | 0 |
| Other | 0 |
| Income (N = 31) | |
| <10,000 CAD/Year | 12 (37.5) |
| 10,000–19,999 CAD/Year | 8 (25) |
| 20,000–29,999 CAD/Year | 2 (6.3) |
| 30,000–39,999 CAD/Year | 3 (9.4) |
| 40,000–49,999 CAD/Year | 3 (9.4) |
| >50,000 CAD/Year | 1 (3.1) |
| Prefer not to say | 2 (6.3) |
| Housing Situation * | |
| Living Alone (N = 32) | 10 (31.25) |
| Living with Partner (N = 32) | 6 (18.75) |
| Living with Children (N = 32) | 3 (9.38) |
| Living with Roommates (N = 32) | 5 (15.63) |
| Living with Extended Family (N = 31) | 8 (25) |
| Experiencing Housing Instability (insecure housing, shelter, transitional housing, houseless) (N = 32) | 14 (43.75) |
| Category | Quote # | Quote | Participant Age and Gender |
|---|---|---|---|
| Individual Factors | |||
| HIV Diagnosis | 1 | I was so in the clouds about it. I don’t even remember them talking to me about any support or anything … I do remember … I felt like garbage and like, as if nobody wanted to be around me, or I felt gross and felt really suicidal. It really embarrassed me to even talk about it. | Participant 39 Woman |
| Mental Health Challenges | 2 | I have flashbacks, and like, it interferes with my work in school, because then I’m spacing out, and it has to do with me not talking about it [sexual abuse] either because I think that if I just keep myself busy, that’ll distract whatever is going on in my head. | Participant 39 Woman |
| 3 | I don’t know what to do with myself, and I just feel if I do anything … (soft cry), I’m just scared to do anything. I’m scared to reach out and start doing things with my life because I always end up backwards headwind, and it just goes away. So, I just think what’s the point? What’s the point in trying to do the same thing? … It’s just recently I’ve been wanting to [get back on HIV treatment] because I just felt like there was no point in trying to fight this disease because there wasn’t much to live for. | Participant 46 Woman | |
| 4 | It was really hard to lose your best friend [mother] and someone who was, your rock, you know. I just turned into an adult [and] I was grieving. I didn’t understand grief and loss. I didn’t realize that there’s a cycle and you can actually deal with it without turning to drugs and alcohol because … I missed my mom, I needed my mother. | Participant 40 Woman | |
| Substance Use Deterring HIV Care | 5 | When they say it’s [having substance use disorder] like, a flu, or whatever. It’s kind of like a flu and it’s not because it is definitely worse. Like you can’t even move. You can’t get up to feed yourself or you can’t get up to even bathe yourself or anything. | Participant 43 Woman |
| 6 | I wasn’t consistent [with HIV medications], you know, like you gotta take it every day. And I wasn’t, you know, it’d be going off and be like, I didn’t go a week without it, but maybe three days. Sometimes it was like, ‘Oh, my God, what am I doing?’ but I was using [methamphetamine] a lot. So, when you using too and you don’t care, your health, like your health doesn’t really matter. | Participant 64 Man | |
| 7 | I just have addictions, like, you know, a lot of my days are based around what I do get like [high]. | Participant 55 Woman | |
| 8 | Like, going to get into an [medical] appointment? Feeling the social anxiety oh no, no. Oh, they think I’m high or they know I’m high or whatever. | Participant 39 Woman | |
| COVID-19 | 9 | Healthcare settings, there was a fear of going to … because I didn’t want to go in because even though my CD4, is okay, I still have this fear of getting in, getting sick. | Participant 33 Man |
| Experiences of violence | 10 | I feel pretty drained I guess tired. I really wanted to get on my [HIV] medication, but it’s just like, with my boyfriend around, I could never get to go do what I need to do … I connected with them [HIV care] once my boyfriend went into jail … but before that I didn’t see them for like two years. | Participant 46 Woman |
| Internalized Stigma | 11 | I am ashamed of myself. I could say that. I would say to myself I am no longer clean I am dirty and contaminated with the virus. | Participant 35 Man |
| Healthcare Factors | |||
| Programmatic/Administrative | 12 | The only thing is sometimes the waiting … It could take a week, two weeks, or three months to get an appointment for something that you might want to be able to see someone like that day. | Participant 57 Two-Spirit |
| 13 | Have an HIV clinic on the reserve, or more services for HIV in the reserve … I was flying in and out to get here for appointments… It would be expensive because we would be using money everyday here, and we had to bring the kids over here. | Participant 49 Man | |
| Lack of follow-up care and supports during HIV diagnosis | 14 | Because I was homeless at the time, so I had a lot that I was missing to actually be focusing on one thing [HIV diagnosis] so that’s why my head was like everywhere … I think I was looking for someone to tell me that everything was going to be okay and that what I needed to do was do these steps to-to get where I’m trying to go and not give up. I honestly can’t remember when they told me I had HIV. I’m pretty sure they just gave me a phone number and where to call and if I needed support and someone to talk to and that was it. | Participant 39 Woman |
| Stigma, Discrimination, and Insecurity in Health Settings | 15 | They [prison staff] come in and they’re like ‘hey Mr. you know you [got] AIDS right? Do you know you have AIDS right?’ I thought he was joking or whatever but then he is not… A little bit of support a little bit of sympathy like, buddy, you just told me I have fucking AIDS and you just come here like nothing like ‘Hey you know you got AIDS right’. How much of a slap in the face do you think that is? I was a kid man, 23 years old. | Participant 52 Man |
| 16 | The hospitals are fucking ridiculous. I can’t go to emergency rooms, and some of those nurses are vicious because they’re judgmental. You hear them talking because I got HIV, they treat us different because we’re addicted. They treat us differently just because we have addictions … Those chicks [nurses] are mean I hate going to emergency rooms now because a lot of my other friends said the same thing before, they won’t go to hospitals and like the emergency rooms because they treat us so shitty there. | Participant 55 Woman | |
| Lack of Social Supports | 17 | The environment here [hospital] is very sterile sometimes … Well, we started it [food bank] and we had coffee out, and people would sit down, and they were talking, and you would network. I had more confidence in not thinking that I was going to die anytime I had the flu, or anytime I had a spot. Because I met people at the food banks, while I was volunteering, that were there for like 10 years, 20 years, 30 years, you know, I met people there and we all sat around and we talked and we got to know each other. And if somebody passed away, we knew they were dead. Now. You [don’t] hear about it? Maybe on Facebook. | Participant 54 Woman |
| 18 | Definitely someone who’s got it [HIV], someone’s got already. A nurse and doctor no-no, someone who’s got already … More believable, yes. I mean I believe doctors, but you know they still got their own jargon … I want to hear it from someone who’s gone through it. | Participant 58 Man | |
| COVID-19 | 19 | Because there was places that weren’t even open. And you had to have a phone, you had to have internet. | Participant 39 Woman |
| Lack of Prevention Strategies | 20 | I rarely ever see, tables for resources [in shelters] … Like, this [educational materials] wasn’t there when I was on the streets and stuff. They [shelters] kind of just had a place for people to come in eat, you know, sit around and chat. There was no resources being handed out. There was posters hung up. But, I like I would change the fact that people get greeted at the door with people with a whole table of pamphlets like this. ‘Are you struggling with addiction? This is what you can do to help. And this is what you can do to get there’. | Participant 40 Woman |
| 21 | You got to have more outreach going to these people [experiencing houselessness] and saying, ‘Hey how are you guys doing?’ I’ve never seen that here in Winnipeg. Out of all the people in like back lanes and stuff I’ve never seen anybody talk to him like a human being. ‘How are you doing? Are you okay? Is everything okay with you? Sure. Do you need anything? No. Just checking in to make sure because you’re a human being’. … They don’t outreach you gotta reach out to them. | Participant 52 Man | |
| Inaccessible Mental Health Services | 22 | I used to have a hard time getting into detox, I would spend nights at hospitals in the waiting room trying to get into [a] detox place. ‘What am I doing wrong?’ I’m saying that I’m trying to get out of this, and they seem to not be taking me serious or something, or seem to think I could do it by myself … It was discouraging for me to speak up for myself. Yeah, like different hospitals. Sometimes, I’ll just give up and just go back to drugs. | Participant 39 Woman |
| 23 | If I want to talk to a psychologist and fuck it’s two years … And then suddenly you get a psychologist. He’s like, yeah, you don’t need me because you’re gay or because you’re this. | Participant 51 Man | |
| Social and Structural Factors | |||
| Housing | 24 | Because I was homeless at the time so that’s why my head was like everywhere … Well I don’t have a phone, I don’t know where to go, you know, I’m homeless, struggling with an addiction and you’re just gonna set me off on the street expect me to figure out things by myself. | Participant 39 Woman |
| 25 | I had a rooming house experience, but I left it. Fucking awful, overrun with mice. Addictions and homelessness, just like confusion … I’ve been trying to get a place which is a lot. Yeah, I just was trying to survive out there. | Participant 55 Woman | |
| 26 | Having a place to go at night. It’s called mine. Not stay out [at] somebody else’s place. … Like people who are homeless and HIV and all like it’s really important for them to be in stabilized situation to where they don’t get sick and their immune system is like not sick. | Participant 41 Woman | |
| 27 | They [HIV doctors] only give me a week’s worth [of medication] at a time because I live on the streets, and bags get stolen a lot so, they don’t want me to have all my meds on me and when I fall asleep and my bag goes missing … Having the stability of my own place having a steady routine that’s how you get into not forgetting and take your pill every day. Because you have a home you go home that you can fell sleep. | Participant 42 Non-Binary | |
| 28 | When my pills got stolen, they were in my room. I was in this rooming house, they were in a bag, my bag that I take with me everywhere. And they got stolen. And I wasn’t able to go on my meds for two weeks, because they were only given to you once a month. Tried coming here [HIV health centre]. Come here, I couldn’t see the doctor, of course. | Participant 59 Man | |
| Stigma and Discrimination | 29 | After that [HIV diagnosis], everyone started treating me different. You know, everyone wanted to stay away, like, didn’t want to shake my hand and didn’t want to be around me. It was just really hard. | Participant 46 Woman |
| Lack of Structural Supports | 30 | Zero [money] it’s hard for fucking four months already and got no support, no money, no fucking nothing … I try to fucking walk around and I get paid just fucking beating somebody in streets | Participant 32 Other |
| Category | Quote # | Quote | Participant Age and Gender |
|---|---|---|---|
| Individual Factors | |||
| Stopping Substance Use | 31 | Things are starting to get a lot better because I have stopped doing drugs like I used to inject. So, I quit like eight weeks ago now. So, things are getting a lot better for me. | Participant 46 Woman |
| Will to Survive | 32 | You have to learn how to have a thick skin. Take things with salt. You sort of have to look at it. If I was in that situation, what would I do? To help people and stuff like that. | Participant 48 Man |
| Healthcare Factors | |||
| HIV Service Providers | 33 | I’m very close with my nurse, my doctor. So, I’m close with a lot of the receptionist. A lot of them know me by name. And we laugh and we joke and it’s just-it’s just like I said, just having an extended support circle of family, like I wouldn’t even call them friends, they’re more like family because they know my story because they’ve known me for so long. | Participant 40 Woman |
| HIV Healthcare Environments | 34 | Only here [HIV care site] is where I got help. If I wasn’t for this place, I would probably be dead right now. I really don’t know where I would be because I have nobody for talking. | Participant 58 Man |
| 35 | It’s just an accepting, loving environment … like it’s-it’s very friendly and welcoming, there’s no judgment here. They understand everything, you know, it’s a lot more [welcoming] than others [healthcare settings]. | Participant 40 Woman | |
| 36 | I think it’s great because they’re more concerned about me as a whole, not just one little piece of me, and that one little piece of me [HIV] is really almost, I know this might not sound right., but it’s okay. It’s almost like that’s been put on the backburner, you know, they look at the results. You don’t see anything that scares them … It’s like, you know, ‘how you’re feeling otherwise, how’s your aches and pains falls?’ | Participant 44 Man | |
| Social Supports | 37 | How they had their little workshops and programs. I really liked one of their programs that I did … I came to all 10-10 classes … It told me a lot about my disease, and plus I got to meet people that had it too. And I really liked that too, because I felt so alone. When I first got it, I just thought I’m the only one out there [with HIV]. | Participant 46 Woman |
| 38 | And the only reason I came here was because I’d run out of food at home, and I was hungry. And I had this piece of paper from the hospital saying, I was entitled to a food bank here. I was like what the hell, I’ll go down and see if I can find out. | Participant 44 Man | |
| Post-HIV Diagnosis Emotional Support and Education | 39 | They made me feel really [safe] … I was broke down crying. They were talking to me and telling me ‘it’s okay, this isn’t, you know, the end of it’ … she’s like, ‘it’s okay, there’s treatment and stuff’. Because when you hear HIV, people are like, ‘Oh, my God, I’m dying’, right? So, it’s like, that’s initially what I thought … then they-they pretty much calmed me down, made me feel safe, and eventually they were able to tell me that this is, you know, I have an appointment and stuff so and they were willing to pick me up and take me to my appointment. | Participant 40 Woman |
| Social and Structural Factors | |||
| Support Networks | 40 | I told my cousin’s wife first. Of course, and I broke down, and she came over to hug me. ‘You are just sick, that’s all. Don’t worry there are lots of treatments out there available, you’re still young’. And then I told my sister there, and she’s like-she’s like, ‘I don’t care, you’re still my brother. Just take your meds.’ | Participant 49 Man |
| 41 | For myself, I didn’t like being looked at weird, you know, I know my mom never looks at me any different like she’s always there for me. You know so I wish more people were like my mom and just loved us unconditionally. | Participant 62 Woman | |
| Structural Supports | 42 | So, I got in contact with people there [housing services] because I was homeless, I was struggling to stay sober… But when I got my own place [without wrap-around supports], I just went off the handle …My first month’s rent money went to alcohol, drugs, more alcohol, it was-it was crazy … So, and then I got addicted to meth like right before I was kicked out … I’ve been there since the program opened [new recovery home with wrap around services]… I really have, where I live is a support. Like I have an unending circle of support … So, when I get the [HIV care] appointments, I-I write them down, and then make sure to put it in my calendar. And I made sure to tell them so that they know ahead of time. They’re like, ‘does she need a ride?’ | Participant 40 Woman |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Villacis-Alvarez, E.; Sobie, C.; Maier, K.; Lavallee, M.; Daniels, C.; Pashe, H.; Baliddawa, J.; Daniels, N.; Murdock, R.; Russell, R.; et al. Gender and Intersecting Barriers and Facilitators to Access the HIV Cascade of Care in Manitoba, Canada, Before and During the COVID-19 Pandemic: A Qualitative Study. Trop. Med. Infect. Dis. 2024, 9, 287. https://doi.org/10.3390/tropicalmed9120287
Villacis-Alvarez E, Sobie C, Maier K, Lavallee M, Daniels C, Pashe H, Baliddawa J, Daniels N, Murdock R, Russell R, et al. Gender and Intersecting Barriers and Facilitators to Access the HIV Cascade of Care in Manitoba, Canada, Before and During the COVID-19 Pandemic: A Qualitative Study. Tropical Medicine and Infectious Disease. 2024; 9(12):287. https://doi.org/10.3390/tropicalmed9120287
Chicago/Turabian StyleVillacis-Alvarez, Enrique, Cheryl Sobie, Katharina Maier, Margaret Lavallee, Chantal Daniels, Heather Pashe, Joel Baliddawa, Nikki Daniels, Rebecca Murdock, Robert Russell, and et al. 2024. "Gender and Intersecting Barriers and Facilitators to Access the HIV Cascade of Care in Manitoba, Canada, Before and During the COVID-19 Pandemic: A Qualitative Study" Tropical Medicine and Infectious Disease 9, no. 12: 287. https://doi.org/10.3390/tropicalmed9120287
APA StyleVillacis-Alvarez, E., Sobie, C., Maier, K., Lavallee, M., Daniels, C., Pashe, H., Baliddawa, J., Daniels, N., Murdock, R., Russell, R., Dan, C., Woodhouse, F., Cusson, S., Patrick, L., Schenkels, M., Payne, M., Kasper, K., MacKenzie, L. J., Ireland, L., ... Rueda, Z. V. (2024). Gender and Intersecting Barriers and Facilitators to Access the HIV Cascade of Care in Manitoba, Canada, Before and During the COVID-19 Pandemic: A Qualitative Study. Tropical Medicine and Infectious Disease, 9(12), 287. https://doi.org/10.3390/tropicalmed9120287







