Comprehensive Tuberculosis Screening and Treatment at a Prison in Central Papua Province, Indonesia
Abstract
1. Introduction
2. Materials and Methods
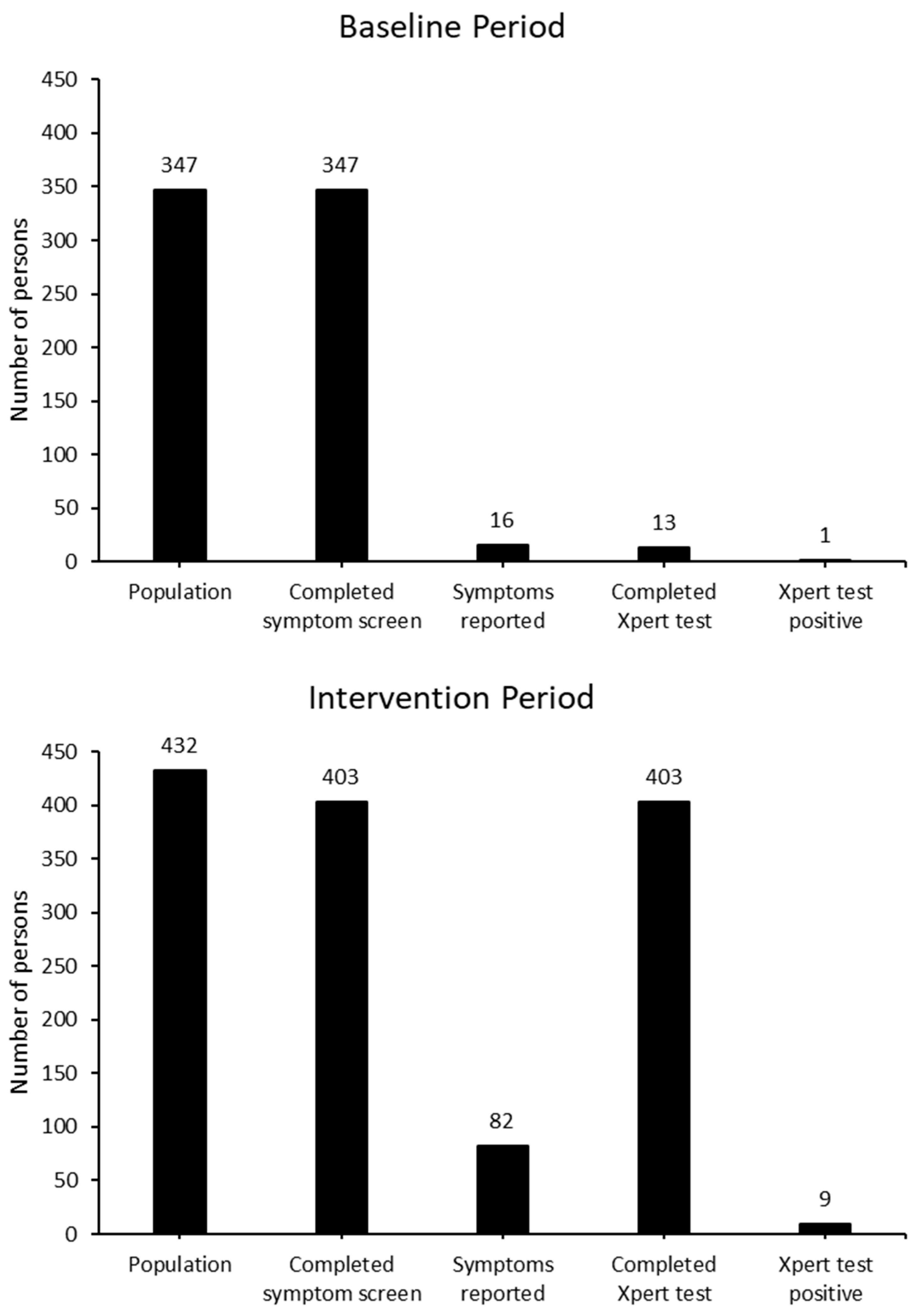
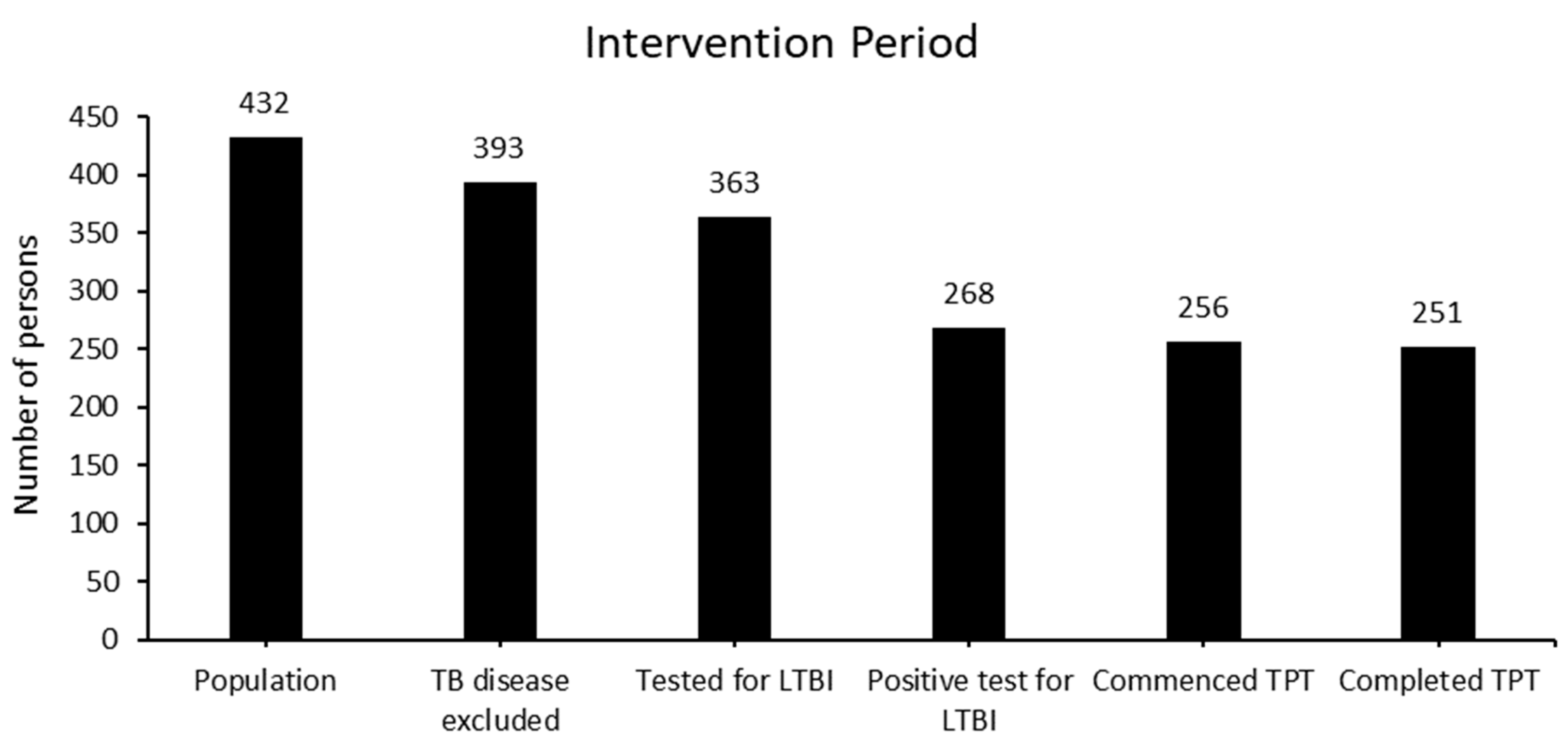
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cords, O.; Martinez, L.; Warren, J.L.; O’Marr, J.M.; Walter, K.S.; Cohen, T.; Zheng, J.; Ko, A.I.; Croda, J.; Andrews, J.R. Incidence and prevalence of tuberculosis in incarcerated populations: A systematic review and meta-analysis. Lancet Public Health 2021, 6, e300–e308. [Google Scholar] [CrossRef] [PubMed]
- Martinez, L.; Warren, J.L.; Harries, A.D.; Croda, J.; Espinal, M.A.; Olarte, R.A.; Avedillo, P.; Lienhardt, C.; Bhatia, V.; Liu, Q.; et al. Global, regional, and national estimates of tuberculosis incidence and case detection among incarcerated individuals from 2000 to 2019: A systematic analysis. Lancet Public Health 2023, 8, e511–e519. [Google Scholar] [CrossRef] [PubMed]
- Placeres, A.F.; de Almeida Soares, D.; Delpino, F.M.; Moura, H.S.; Scholze, A.R.; Dos Santos, M.S.; Arcêncio, R.A.; Fronteira, I. Epidemiology of TB in prisoners: A metanalysis of the prevalence of active and latent TB. BMC Infect. Dis. 2023, 23, 20. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Tuberculosis Report 2023; World Health Organization: Geneva, Switzerland, 2022.
- United Nations Office on Drugs and Crime. Unsentenced with Prisons Overcrowded in Half of All Countries; United Nations Office on Drugs and Crime: Vienna, Austria, 2021. [Google Scholar]
- Marhaenjati, B. Indonesian Prison System at More than Double Its Capacity. Jakarta Globe. 27 September 2021. Available online: https://jakartaglobe.id/news/indonesian-prison-system-at-more-than-double-its-capacity (accessed on 19 August 2024).
- Llewellyn, A. Why Are Indonesian Prisons So Dangerous? Aljazeera News. 30 October 2021. Available online: https://www.aljazeera.com/news/2021/10/30/why-are-indonesian-prisons-so-dangerous (accessed on 19 August 2024).
- Kementerian Kesehatan Republic of Indonesia. Dashboard TB Indonesia; Kementerian Kesehatan: Jakarta, Indonesia, 2021.
- Lestari, T.; Kamaludin; Lowbridge, C.; Kenangalem, E.; Poespoprodjo, J.R.; Graham, S.M.; Ralph, A.P. Impacts of tuberculosis services strengthening and the COVID-19 pandemic on case detection and treatment outcomes in Mimika District, Papua, Indonesia: 2014–2021. PLoS Glob. Public Health 2022, 2, e0001114. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Consolidated Guidelines on Tuberculosis, Module 2: Screening; World Health Organization: Geneva, Switzerland, 2021.
- World Health Organization. WHO Consolidated Guidelines on Tuberculosis, Module 1: Prevention; World Health Organization: Geneva, Switzerland, 2020.
- World Health Organization. WHO Operational Handbook on Tuberculosis. Module 2: Screening—Systematic Screening for Tuberculosis Disease; World Health Organization: Geneva, Switzerland, 2021.
- Idris, N.A.; Zakaria, R.; Muhamad, R.; Husain, N.R.; Ishak, A.; Mohammad, W.M. The Effectiveness of Tuberculosis Education Programme in Kelantan, Malaysia on Knowledge, Attitude, Practice and Stigma towards Tuberculosis among Adolescents. Malays. J. Med. Sci. 2020, 27, 102–114. [Google Scholar] [CrossRef] [PubMed]
- Bisallah, C.I.; Rampal, L.; Lye, M.S.; Mohd Sidik, S.; Ibrahim, N.; Iliyasu, Z.; Onyilo, M.O. Effectiveness of health education intervention in improving knowledge, attitude, and practices regarding Tuberculosis among HIV patients in General Hospital Minna, Nigeria—A randomized control trial. PLoS ONE 2018, 13, e0192276. [Google Scholar] [CrossRef] [PubMed]
- Kendall, E.A.; Kitonsa, P.J.; Nalutaaya, A.; Erisa, K.C.; Mukiibi, J.; Nakasolya, O.; Isooba, D.; Baik, Y.; Robsky, K.O.; Kato-Maeda, M.; et al. The Spectrum of Tuberculosis Disease in an Urban Ugandan Community and Its Health Facilities. Clin. Infect. Dis. 2020, 72, e1035–e1043. [Google Scholar] [CrossRef] [PubMed]
- Frascella, B.; Richards, A.S.; Sossen, B.; Emery, J.C.; Odone, A.; Law, I.; Onozaki, I.; Esmail, H.; Houben, R.M. Subclinical Tuberculosis Disease—A Review and Analysis of Prevalence Surveys to Inform Definitions, Burden, Associations, and Screening Methodology. Clin. Infect. Dis. 2021, 73, e830–e841. [Google Scholar] [CrossRef] [PubMed]
- Santos, A.D.; de Oliveira, R.D.; Lemos, E.F.; Lima, F.; Cohen, T.; Cords, O.; Martinez, L.; Gonçalves, C.; Ko, A.; Andrews, J.R.; et al. Yield, Efficiency, and Costs of Mass Screening Algorithms for Tuberculosis in Brazilian Prisons. Clin. Infect. Dis. 2021, 72, 771–777. [Google Scholar] [CrossRef] [PubMed]
- Zifodya, J.S.; Kreniske, J.S.; Schiller, I.; Kohli, M.; Dendukuri, N.; Schumacher, S.G.; Ochodo, E.A.; Haraka, F.; Zwerling, A.A.; Pai, M.; et al. Xpert Ultra versus Xpert MTB/RIF for pulmonary tuberculosis and rifampicin resistance in adults with presumptive pulmonary tuberculosis. Cochrane Database Syst. Rev. 2021. [Google Scholar] [CrossRef]
- Qin, Z.Z.; Ahmed, S.; Sarker, M.S.; Paul, K.; Adel, A.S.; Naheyan, T.; Barrett, R.; Banu, S.; Creswell, J. Tuberculosis detection from chest X-rays for triaging in a high tuberculosis-burden setting: An evaluation of five artificial intelligence algorithms. Lancet Digit. Health 2021, 3, e543–e554. [Google Scholar] [CrossRef] [PubMed]
- Matucci, T.; Riccardi, N.; Occhineri, S.; Pontarelli, A.; Tiseo, G.; Falcone, M.; Puci, M.; Saderi, L.; Sotgiu, G. Treatment of latent tuberculosis infection in incarcerated people: A systematic review. Clin. Microbiol. Infect. 2023, 29, 714–721. [Google Scholar] [CrossRef] [PubMed]
- Mangochi, P.; Bossard, C.; Catacutan, C.; Van Laeken, D.; Kwitonda, C.; Ortuno, R.; Chiwaula, L.; Meis, M.; Abura, A.; Furin, J.; et al. TB screening, prevention and treatment cascade in a Malawi prison. Int. J. Tuberc. Lung Dis. 2022, 26, 956–962. [Google Scholar] [CrossRef] [PubMed]
- World Prison Brief, Institute for Crime & Justice Policy Research: Indonesia. Available online: https://www.prisonstudies.org/country/indonesia (accessed on 23 September 2024).

| Incarcerated | Staff | ||||
|---|---|---|---|---|---|
| Characteristics | N | % | N | % | |
| Sex | Male | 326 | 91.3 | 7 | 15.2 |
| Female | 31 | 8.7 | 39 | 84.8 | |
| Ethnicity | Papuan | 70 | 19.6 | 10 | 21.7 |
| Non-Papuan | 287 | 80.4 | 36 | 78.3 | |
| Age group | ≤25 years | 91 | 25.5 | 20 | 43.5 |
| 26–31 years | 79 | 22.1 | 13 | 28.2 | |
| 32–39 years | 95 | 26.6 | 8 | 17.4 | |
| >40 years | 92 | 25.8 | 5 | 10.9 | |
| Area of facility | Area 1 | 31 | 8.7 | ||
| Area 2 | 26 | 7.3 | |||
| Area 3 | 40 | 11.2 | |||
| Area 4 | 29 | 8.1 | |||
| Area 5 | 67 | 18.8 | |||
| Area 6 | 84 | 23.5 | |||
| Area 7 | 80 | 22.4 | |||
| Total | 357 | 88.6 | 46 | 11.4 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aurelia; Kamaludin; Muslimin, C.; Balik, Y.; Lestari, T.; Hafidz, F.; Dewi, C.; Lowbridge, C.; Probandari, A. Comprehensive Tuberculosis Screening and Treatment at a Prison in Central Papua Province, Indonesia. Trop. Med. Infect. Dis. 2024, 9, 241. https://doi.org/10.3390/tropicalmed9100241
Aurelia, Kamaludin, Muslimin C, Balik Y, Lestari T, Hafidz F, Dewi C, Lowbridge C, Probandari A. Comprehensive Tuberculosis Screening and Treatment at a Prison in Central Papua Province, Indonesia. Tropical Medicine and Infectious Disease. 2024; 9(10):241. https://doi.org/10.3390/tropicalmed9100241
Chicago/Turabian StyleAurelia, Kamaludin, Cahya Muslimin, Yetty Balik, Trisasi Lestari, Firdaus Hafidz, Christa Dewi, Christopher Lowbridge, and Ari Probandari. 2024. "Comprehensive Tuberculosis Screening and Treatment at a Prison in Central Papua Province, Indonesia" Tropical Medicine and Infectious Disease 9, no. 10: 241. https://doi.org/10.3390/tropicalmed9100241
APA StyleAurelia, Kamaludin, Muslimin, C., Balik, Y., Lestari, T., Hafidz, F., Dewi, C., Lowbridge, C., & Probandari, A. (2024). Comprehensive Tuberculosis Screening and Treatment at a Prison in Central Papua Province, Indonesia. Tropical Medicine and Infectious Disease, 9(10), 241. https://doi.org/10.3390/tropicalmed9100241








