Frequency and Factors Associated with Disabilities among Leprosy Patients Admitted to the Kindia Disability Prevention and Physical Rehabilitation Centre (Pirp) in Guinea from 2017 to 2021
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
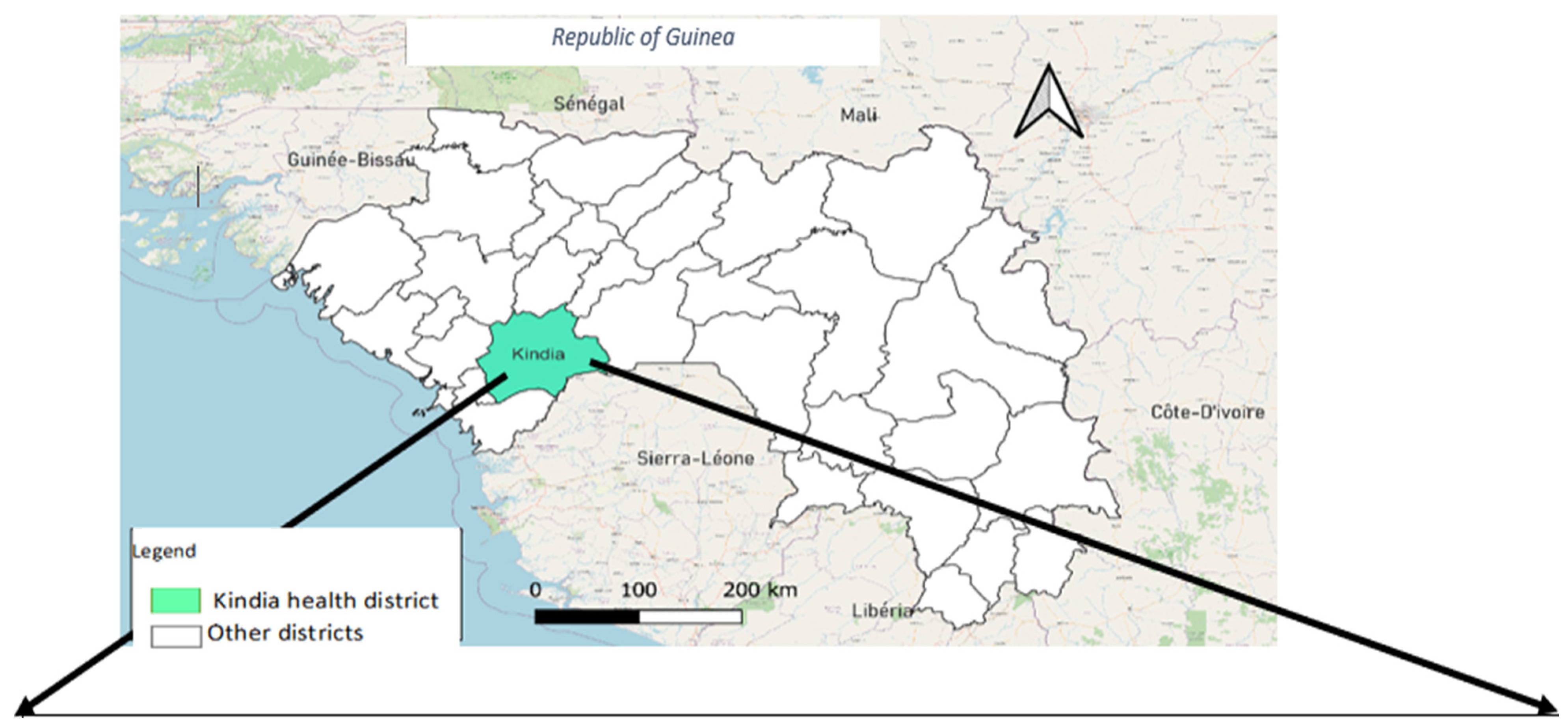
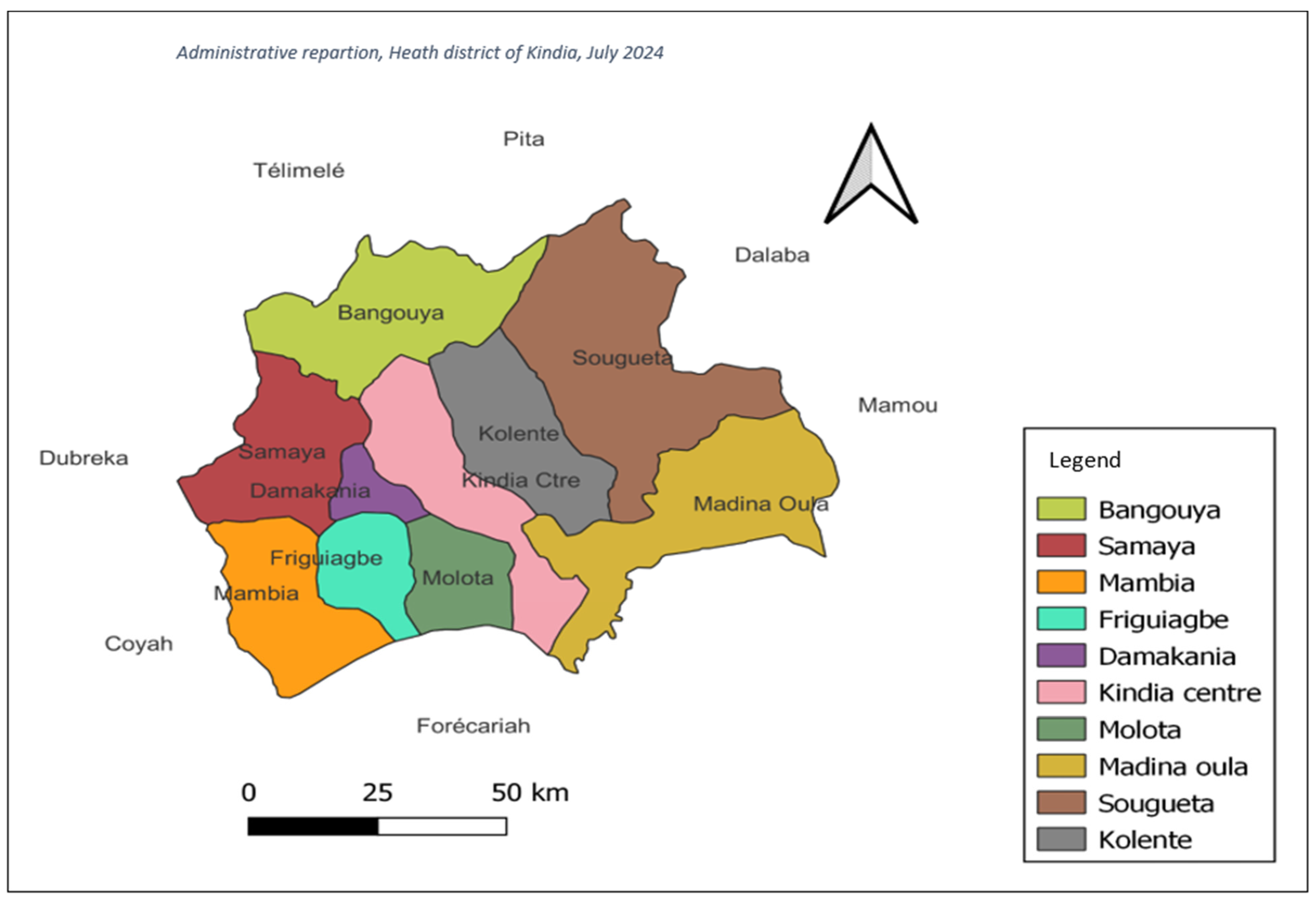
2.2. General Setting
2.3. Specific Setting
2.4. Population and Study Period
2.5. Collection of Data and Variables
2.6. Data Management and Analysis
3. Results
3.1. Socio-Demographic and Clinical Characteristics
3.2. Degrees of Disability of Leprosy Cases
3.3. Factors Associated with the Occurrence of Disabilities
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- White, C.; Franco-Paredes, C. Leprosy in the 21st century. Clin. Microbiol. Rev. 2015, 28, 80–94. [Google Scholar] [CrossRef] [PubMed]
- OMS Situation de la lèpre (maladie de Hansen) dans le Monde, 2021: Vers l’interruption de la Transmission [Internet]. 2022. Available online: https://apps.who.int/iris/rest/bitstreams/1464293/retrieve (accessed on 29 May 2022).
- Shumet, T.; Demissie, M.; Bekele, Y. Prevalence of Disability and Associated Factors among Registered Leprosy Patients in All Africa Tb and Leprosy Rehabilitation and Training Centre (ALERT), Addis Ababa, Ethiopia. Ethiop. J. Health Sci. 2015, 25, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Sakral, A.; Dogra, N.; Dogra, D.; Sharma, K. Clinical and epidemiological trends in childhood leprosy: A 20-year retrospective analysis from a tertiary care hospital in Jammu, North India. Indian J. Dermatol. Venereol. Leprol. 2022, 88, 755–760. [Google Scholar] [CrossRef] [PubMed]
- Nkehli, L.J.; Menezes, C.N.; Tsitsi, J.M.L. Patterns of leprosy at Chris Hani Baragwanath Academic Hospital, Johannesburg, South Africa, and review of current clinical practice. S. Afr. Med. J. Suid-Afr. Tydskr. Vir Geneeskd. 2021, 111, 879–885. [Google Scholar]
- Garbino, J.A.; Heise, C.O.; Marques, W. Assessing nerves in leprosy. Clin. Dermatol. 2016, 34, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Paul, M.S.K.; Kumar, D.P. International Textbook of Leprosy. Physical Rehabilitation in Leprosy. Available online: https://internationaltextbookofleprosy.org/chapter/physical-rehabilitation (accessed on 29 May 2022).
- Lèpre [Internet]. Available online: https://www.who.int/fr/news-room/fact-sheets/detail/leprosy (accessed on 27 May 2022).
- van Brakel, W.H.; Sihombing, B.; Djarir, H.; Beise, K.; Kusumawardhani, L.; Yulihane, R.; Kurniasari, I.; Kasim, M.; Kesumaningsih, K.I.; Wilder-Smith, A. Disability in people affected by leprosy: The role of impairment, activity, social participation, stigma and discrimination. Glob. Health Action 2012, 5, 18394. [Google Scholar] [CrossRef]
- Chukwu, J.N.; Ekeke, N.; Nwafor, C.C.; Meka, A.O.; Alphonsus, C.; Mbah, O.K.; Eze, C.C.; Ukwaja, K.N. Worsening of the disability grade during leprosy treatment: Prevalence and its determinants in Southern Nigeria. Trans. R. Soc. Trop. Med. Hyg. 2018, 112, 492–499. [Google Scholar] [CrossRef]
- de Paula, H.L.; de Souza, C.D.F.; Silva, S.R.; Martins-Filho, P.R.S.; Barreto, J.G.; Gurgel, R.Q.; Cuevas, L.E.; Santos, V.S. Risk Factors for Physical Disability in Patients With Leprosy: A Systematic Review and Meta-analysis. JAMA Dermatol. 2019, 155, 1120–1128. [Google Scholar] [CrossRef] [PubMed]
- Srinivas, G.; Muthuvel, T.; Lal, V.; Vaikundanathan, K.; Schwienhorst-Stich, E.-M.; Kasang, C. Risk of disability among adult leprosy cases and determinants of delay in diagnosis in five states of India: A case-control study. PLoS Negl. Trop. Dis. 2019, 13, e0007495. [Google Scholar] [CrossRef] [PubMed]
- Dharmawan, Y.; Fuady, A.; Korfage, I.J.; Richardus, J.H. Delayed detection of leprosy cases: A systematic review of healthcare-related factors. PLoS Negl. Trop. Dis. 2022, 16, e0010756. [Google Scholar] [CrossRef] [PubMed]
- Organisation mondiale de la santé. Vers zéro lèpre. Stratégie mondiale de Lutte contre la Lèpre (Maladie de Hansen) 2021–2030. Dr EA Cooreman/Lèpre. Available online: https://www.who.int/publications/i/item/9789290228509 (accessed on 25 May 2022).
- Direction Nationale de l’épidémiologie et de la lutte Contre La Maladie Direction Nationale de l’épidémiologie et de la lutte Contre La Maladie: Plan Directeur de la Lutte Contre les Maladies Tropicales Négligées en Guinée (2019–2023). Available online: https://portail.sante.gov.gn/wp-content/uploads/2020/09/PD-Corrig%C3%A9-MLO-2.pdf (accessed on 25 May 2022).
- WHO. GHO|By category|Leprosy—Leprosy Registered Prevalence Rate per 1,000,000 Population—Data by Country. Available online: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/5299 (accessed on 29 May 2022).
- Keita, M.; Sow, I.S.; Soumah, M.M.; Diané, B.; Kaba, M.S.; Tounkara, T.M.; Baldé, H.; Cissé, M. Les infirmités liées à la lèpre dans les sites de prise en charge de la ville de Conakry. Ann. Dermatol. Vénéréologie 2015, 142, S612–S613. [Google Scholar] [CrossRef]
- Institut National de la Statistique [Internet]. Available online: https://www.stat-guinee.org/ (accessed on 25 May 2022).
- Ministère de la Sante. Plan-National-de-Développement-Sanitaire-2015-2024.-Guinée. [Internet]. 2015. Available online: https://www.prb.org/wp-content/uploads/2018/05/Plan-National-de-De%CC%81veloppement-Sanitaire-2015-2024.-Guine%CC%81e.pdf (accessed on 25 May 2022).
- Commune de Kindia. Plan de Developpement Communal Horizon 2015 [Internet]. 2015. Available online: http://guinee44.org/wp-content/uploads/2007/07/photo_doc-6-2.pdf (accessed on 25 May 2022).
- Institut National de la Statistique (INS). Recensement général de la Population et de l’habitation (Rgph3_perspectives_demographiques.). Available online: https://www.stat-guinee.org/images/Documents/Publications/INS/rapports_enquetes/RGPH3/RGPH3_perspectives_demographiques.pdf (accessed on 25 May 2022).
- Carte Sanitaire de la Préfecture de Kindia. Source Direction préfectorale de la Sante de Kindia Juillet 2024. Available online: https://commons.wikimedia.org/wiki/File:GN-Kindia.png (accessed on 27 June 2022).
- Reibel, F.; Cambau, E.; Aubry, A. Update on the epidemiology, diagnosis, and treatment of leprosy. Méd. Mal. Infect. 2015, 45, 383–393. [Google Scholar] [CrossRef] [PubMed]
- Raposo, M.T.; Reis, M.C.; Caminha, A.V.D.Q.; Heukelbach, J.; Parker, L.A.; Pastor-Valero, M.; Nemes, M.I.B. Grade 2 disabilities in leprosy patients from Brazil: Need for follow-up after completion of multidrug therapy. PLoS Negl. Trop. Dis. 2018, 12, e0006645. [Google Scholar] [CrossRef] [PubMed]
- Urgesa, K.; de Bruijne, N.D.; Bobosha, K.; Seyoum, B.; Mihret, A.; Geda, B.; Schoenmakers, A.; Mieras, L.; van Wijk, R.; Kasang, C.; et al. Prolonged delays in leprosy case detection in a leprosy hot spot setting in Eastern Ethiopia. PLoS Negl. Trop. Dis. 2022, 16, e0010695. [Google Scholar] [CrossRef] [PubMed]
- Romero-Montoya, M.; Beltran-Alzate, J.C.; Cardona-Castro, N. Evaluation and Monitoring of Mycobacterium leprae Transmission in Household Contacts of Patients with Hansen’s Disease in Colombia. PLoS Negl. Trop. Dis. 2017, 11, e0005325. [Google Scholar] [CrossRef] [PubMed]
- Kabo, A.K.; Kaman, K.; Doungous, D.M.; Ouedraogo, L.; Abakar, M.; Godreuil, S.; Beng, V.P. Epidémiologie de la lèpre au Tchad de 2015 à 2019. Pan Afr. Med. J. 2022, 41, 120. [Google Scholar] [CrossRef] [PubMed]
- Scollard, D.M.; Martelli, C.M.; Stefani, M.M.; de Fatima Maroja, M.; Villahermosa, L.; Pardillo, F.; Tamang, K.B. Risk Factors for Leprosy Reactions in Three Endemic Countries. Am. J. Trop. Med. Hyg. 2015, 92, 108–114. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Frequency % |
|---|---|
| Age group in years: | |
| ≤14 | 4 (3.5) |
| 15 to 30 | 50 (43.5) |
| 31 to 50 | 38 (33) |
| ≥51 and more | 23 (20) |
| Sex: | |
| Male | 60 (52.2) |
| Female | 55 (47.8) |
| Residence: | |
| Kindia Urban | 37 (32.2) |
| Kindia Rural | 64 (55.7) |
| Other area | 14 (12.2) |
| Contact with other patients (leprosy): | |
| Yes | 39 (33.3) |
| Medical history: | |
| Type 1 reactions | 114 (99.1) |
| Erythema nodosum leprosum (ENL) | 1 (0.9) |
| Clinical signs: | |
| Macule | 74 (63) |
| Papule | 7 (7.4) |
| Nodule | 10 (9.6) |
| Infiltrate | 9 (9) |
| Ulcer | 15 (11) |
| Duration of symptoms (months): | |
| ≤6 | 32 (27.4) |
| 7 to 12 | 65 (55.6) |
| 13 to 24 | 14 (12) |
| ≥25 | 4 (3.4) |
| Types of leprosy: | |
| Multibacillary (MB) | 96 (82.1) |
| Paucibacillary (PB) | 19 (16.2) |
| Patient categories: | |
| New | 102 (87.7) |
| Other | 13 (11.3) |
| Smear result: | |
| Negative smear | 100 (87) |
| Positive smear | 15 (13) |
| Corticosteroid therapy: | |
| Yes | 91 (77.8) |
| Patient outcome after treatment: | |
| Cured | 106 (92.2) |
| Transferred | 1 (9) |
| Lost to follow-up | 7 (6.1) |
| Died | 1 (9) |
| Variables | Disability | ||
|---|---|---|---|
| Present | Absent | p-Value | |
| n = 87 (75.7%) | n = 28 (24.3) | ||
| Sex: | |||
| Man | 52 (86.7) | 8 (13.3) | 0.004 |
| Woman | 35 (63.6) | 20 (36.4) | |
| Age group in year: | |||
| ≤14 | 2 (50) | 2 (50) | 0.32 |
| ≥15 to 30 | 37 (74) | 13 (26) | |
| ≥31 to 50 | 32 (84.2) | 6 (15.8) | |
| ≥51 and more | 16 (69.6) | 7 (30.4) | |
| Provenance: | |||
| Kindia Urban | 25 (67.6) | 12 (32.4) | 0.13 |
| Kindia Rural | 53 (82.8) | 11 (17.2) | |
| Others provinces | 9 (64.3) | 5 (35.7) | |
| Medical history: | |||
| Type 1 reactions | 86 (75.4) | 28 (24.6) | 0.001 |
| Erythema nodosum leprosum (ENL) | 1 (100) | 0 | |
| Type of leprosy: | |||
| Multibacillary (MB) | 85 (88.5) | 11 (11.5) | 0.001 |
| Paucibacillary (PB) | 2 (10.5) | 17 (89.5) | |
| Patient category: | |||
| New | 74 (72.5) | 28 (27.5) | 0.02 |
| Other | 0 | 13 (100) | |
| Smear result | |||
| Negative smear | 76 (76) | 24 (24) | 0.82 |
| Positive smear | 11 (73.3) | 4 (26.7) | |
| Corticosteroid therapy | |||
| Yes | 71 (78) | 20 (22) | 0.24 |
| No | 16 (66.7) | 8 (33.3) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sy Savané, I.S.; Sidibé, S.; Kolié, D.; Camara, M.; Sakho, F.; Sidibé, S.; Chérif, M.S.; Doumbouya, S.; Nabé, A.K.; Delamou, A. Frequency and Factors Associated with Disabilities among Leprosy Patients Admitted to the Kindia Disability Prevention and Physical Rehabilitation Centre (Pirp) in Guinea from 2017 to 2021. Trop. Med. Infect. Dis. 2024, 9, 237. https://doi.org/10.3390/tropicalmed9100237
Sy Savané IS, Sidibé S, Kolié D, Camara M, Sakho F, Sidibé S, Chérif MS, Doumbouya S, Nabé AK, Delamou A. Frequency and Factors Associated with Disabilities among Leprosy Patients Admitted to the Kindia Disability Prevention and Physical Rehabilitation Centre (Pirp) in Guinea from 2017 to 2021. Tropical Medicine and Infectious Disease. 2024; 9(10):237. https://doi.org/10.3390/tropicalmed9100237
Chicago/Turabian StyleSy Savané, Ibrahima Sory, Sidikiba Sidibé, Delphin Kolié, Mamadou Camara, Fatoumata Sakho, Sadan Sidibé, Mahamoud Sama Chérif, Sékou Doumbouya, Abdoul Karim Nabé, and Alexandre Delamou. 2024. "Frequency and Factors Associated with Disabilities among Leprosy Patients Admitted to the Kindia Disability Prevention and Physical Rehabilitation Centre (Pirp) in Guinea from 2017 to 2021" Tropical Medicine and Infectious Disease 9, no. 10: 237. https://doi.org/10.3390/tropicalmed9100237
APA StyleSy Savané, I. S., Sidibé, S., Kolié, D., Camara, M., Sakho, F., Sidibé, S., Chérif, M. S., Doumbouya, S., Nabé, A. K., & Delamou, A. (2024). Frequency and Factors Associated with Disabilities among Leprosy Patients Admitted to the Kindia Disability Prevention and Physical Rehabilitation Centre (Pirp) in Guinea from 2017 to 2021. Tropical Medicine and Infectious Disease, 9(10), 237. https://doi.org/10.3390/tropicalmed9100237






