Comparing Catastrophic Costs: Active vs. Passive Tuberculosis Case Finding in Urban Vietnam
Abstract
:1. Introduction
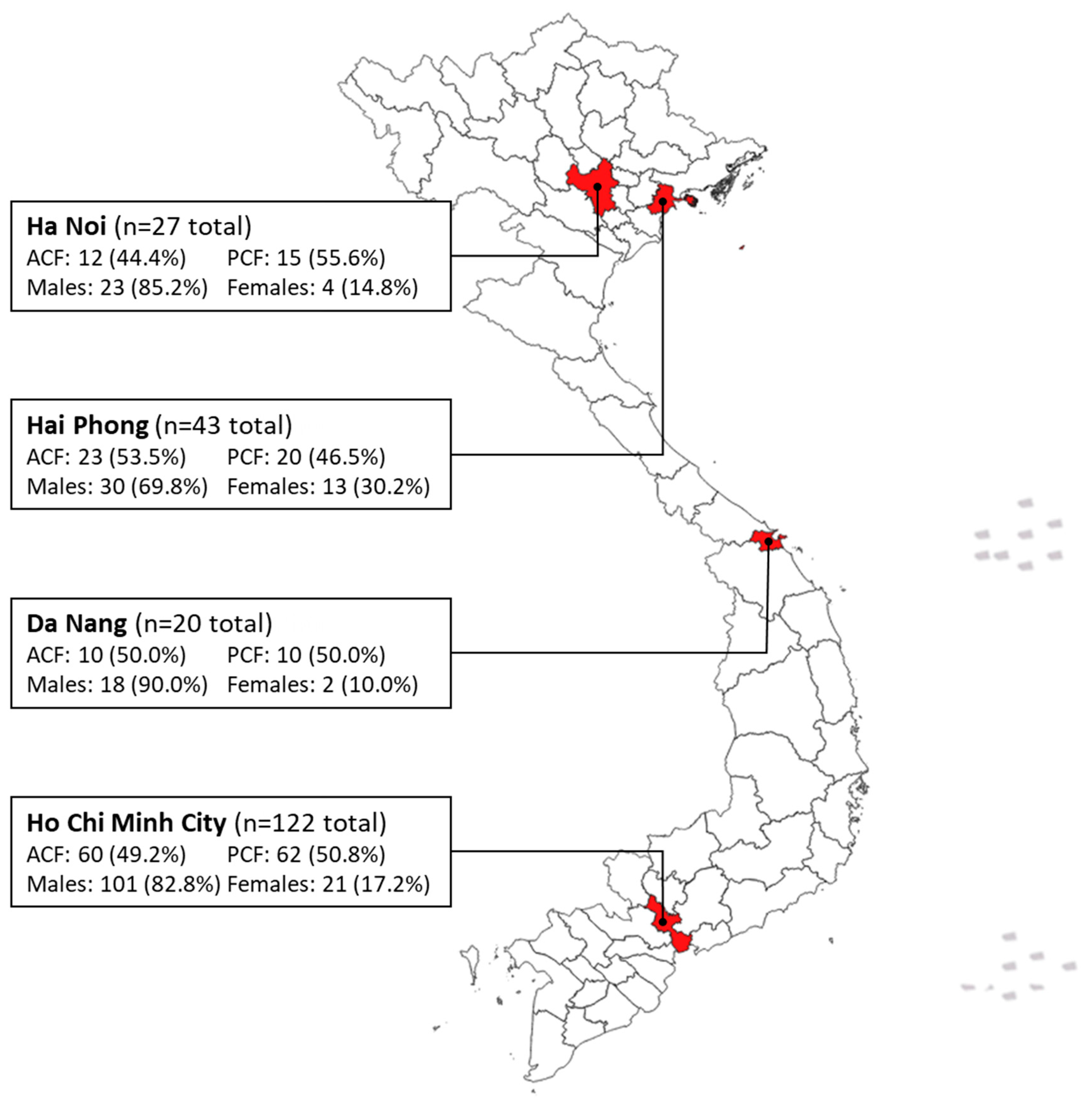
2. Materials and Methods
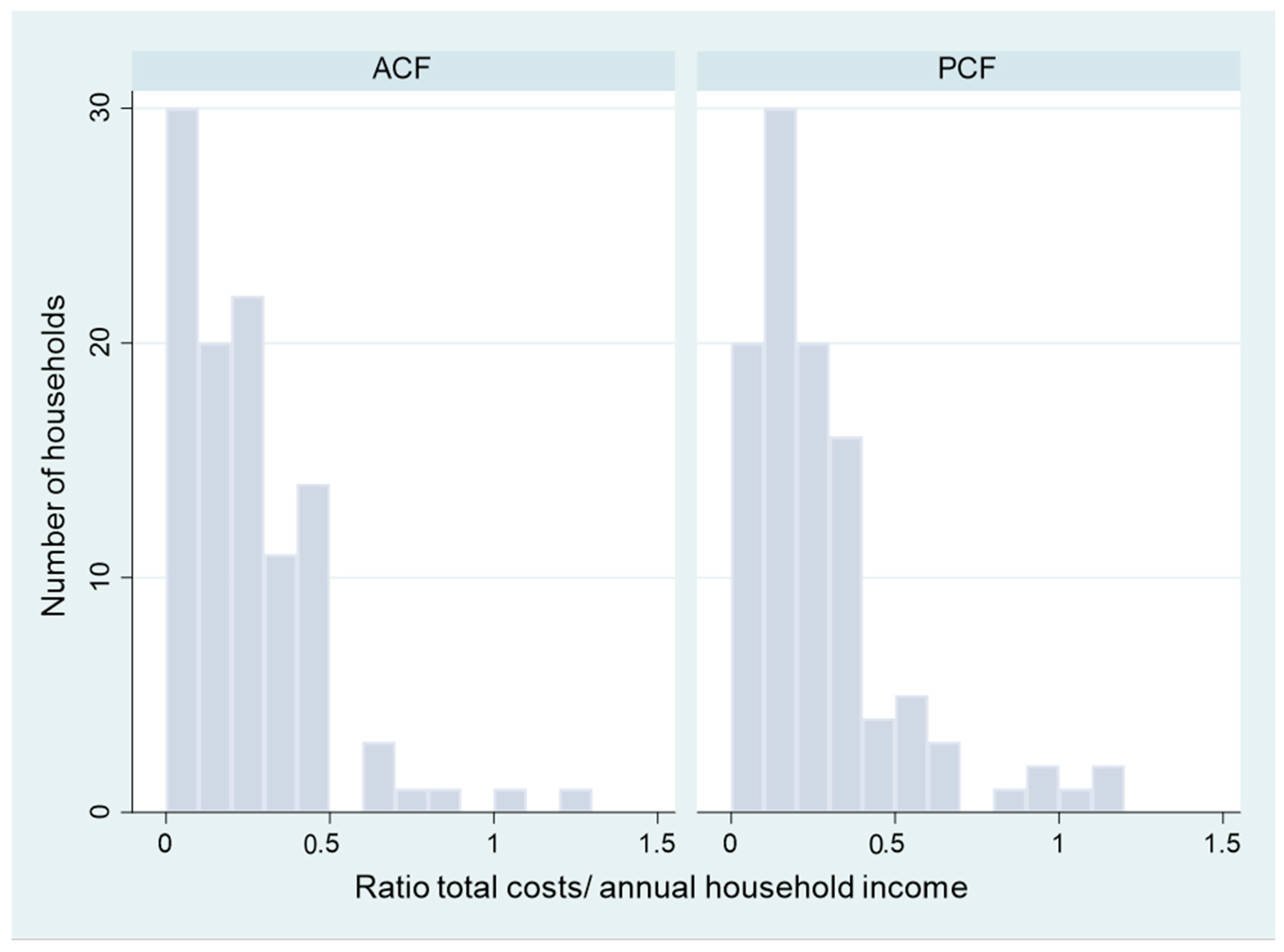
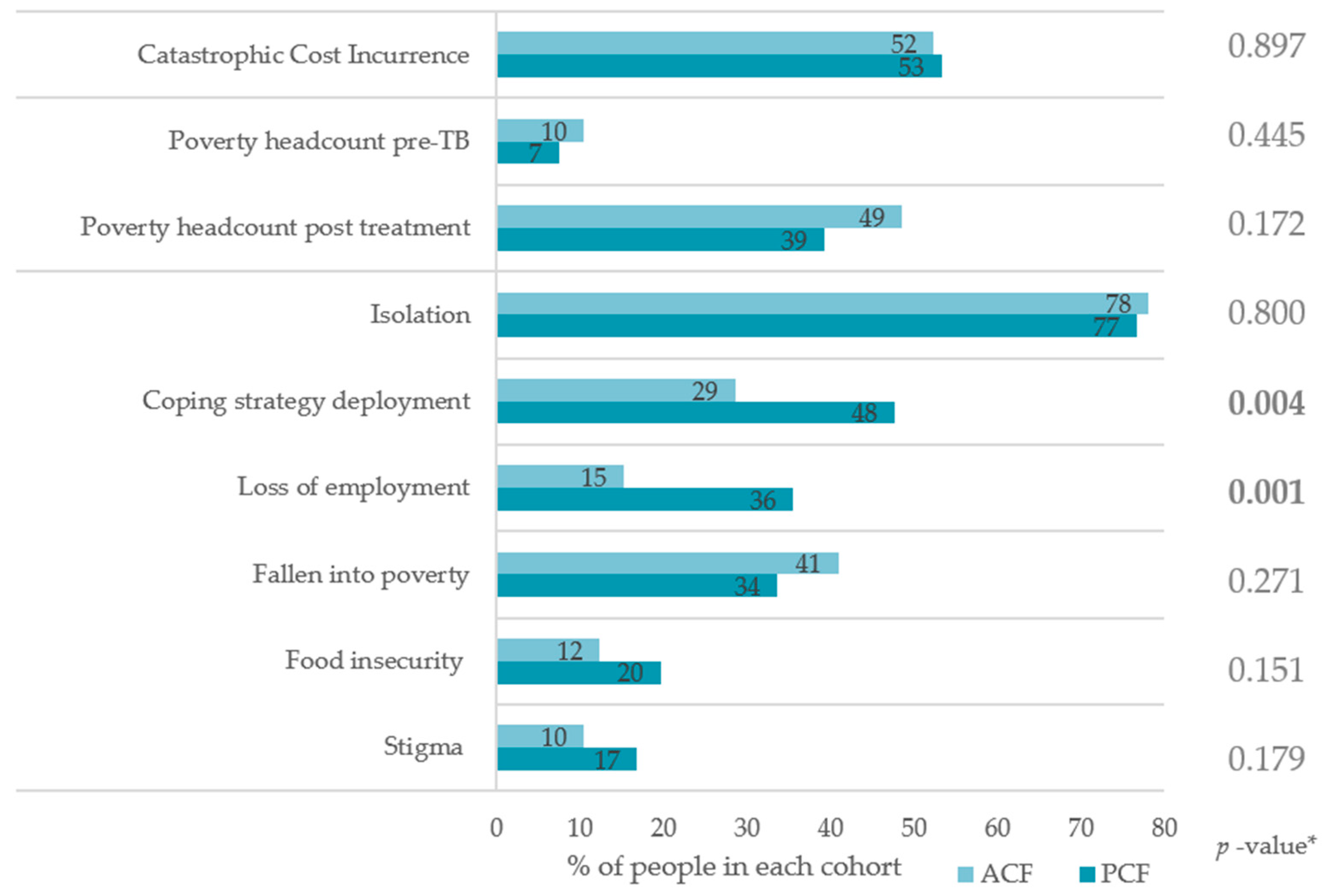
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Baseline Characteristic | Catastrophic Cost Incurrence, N (%) | Crude OR * (95% CI) | Adjusted OR ** (95% CI) |
|---|---|---|---|
| Case finding model | |||
| PCF | 55/105 (52.4%) | 1.00 | 1.00 |
| ACF | 57/107 (53.3%) | 0.96 (0.56–1.65) | 0.93 (0.52–1.69) |
| Sex | |||
| Men | 89/172 (51.7%) | 1.00 | 1.00 |
| Women | 23/40 (57.5%) | 1.26 (0.63–2.53) | 1.27 (0.62–2.57) |
| Age category | |||
| ≤50 years | 38/73 (52.1%) | 1.00 | 1.00 |
| >50 years | 74/139 (53.2%) | 1.05 (0.59–1.85) | 1.10 (0.56–2.00) |
| Education level | |||
| Up to primary education | 55/92 (59.8%) | 1.00 | 1.00 |
| Secondary school or above | 57/120 (47.5%) | 0.61 (0.35–1.05) | 0.60 (0.34–1.07) |
| Employment status | |||
| Unemployed | 102/191 (53.4%) | 1.00 | 1.00 |
| Employed | 10/21 (47.6%) | 1.26 (0.51–3.11) | 1.41 (0.56–3.56) |
| Social Health Insurance status | |||
| Uninsured | 21/36 (58.3%) | 1.00 | 1.00 |
| Insured | 91/176 (51.7%) | 0.76 (0.37–1.58) | 0.84 (0.39–1.78) |
References
- Lönnroth, K.; Jaramillo, E.; Williams, B.G.; Dye, C.; Raviglione, M. Drivers of Tuberculosis Epidemics: The Role of Risk Factors and Social Determinants. Soc. Sci. Med. 2009, 68, 2240–2246. [Google Scholar] [CrossRef]
- Sachdeva, K.S.; Kumar, N. Closing the Gaps in Tuberculosis Detection—Considerations for Policy Makers. Lancet Glob. Health 2023, 11, e185–e186. [Google Scholar] [CrossRef]
- Global Tuberculosis Programme. Global Tuberculosis Report 2022; World Health Organization: Geneva, Switzerland, 2022.
- Burke, R.M.; Nliwasa, M.; Feasey, H.R.A.; Chaisson, L.H.; Golub, J.E.; Naufal, F.; Shapiro, A.E.; Ruperez, M.; Telisinghe, L.; Ayles, H.; et al. Community-Based Active Case-Finding Interventions for Tuberculosis: A Systematic Review. Lancet Public Health 2021, 6, e283–e299. [Google Scholar] [CrossRef]
- Yuen, C.M.; Amanullah, F.; Dharmadhikari, A.; Nardell, E.A.; Seddon, J.A.; Vasilyeva, I.; Zhao, Y.; Keshavjee, S.; Becerra, M.C. Turning off the Tap: Stopping Tuberculosis Transmission through Active Case-Finding and Prompt Effective Treatment. Lancet 2015, 386, 2334–2343. [Google Scholar] [CrossRef] [PubMed]
- Alsdurf, H.; Empringham, B.; Miller, C.; Zwerling, A. Tuberculosis Screening Costs and Cost-Effectiveness in High-Risk Groups: A Systematic Review. BMC Infect. Dis. 2021, 21, 935. [Google Scholar] [CrossRef] [PubMed]
- Telisinghe, L.; Ruperez, M.; Amofa-Sekyi, M.; Mwenge, L.; Mainga, T.; Kumar, R.; Hassan, M.; Chaisson, L.H.; Naufal, F.; Shapiro, A.E.; et al. Does Tuberculosis Screening Improve Individual Outcomes? A Systematic Review. eClinicalMedicine 2021, 40, 101127. [Google Scholar] [CrossRef] [PubMed]
- Tanimura, T.; Jaramillo, E.; Weil, D.; Raviglione, M.; Lönnroth, K. Financial Burden for Tuberculosis Patients in Low- and Middle-Income Countries: A Systematic Review. Eur. Respir. J. 2014, 43, 1763–1775. [Google Scholar] [CrossRef]
- World Health Organization. Tuberculosis Patient Cost Surveys: A Handbook; World Health Organization: Geneva, Switzerland, 2017; ISBN 978-92-4-151352-4.
- Nhung, N.V.; Hoa, N.B.; Anh, N.T.; Anh, L.T.N.; Siroka, A.; Lönnroth, K.; Baena, I.G. Measuring Catastrophic Costs Due to Tuberculosis in Viet Nam. Int. J. Tuberc. Lung Dis. Off. J. Int. Union Against Tuberc. Lung Dis. 2018, 22, 983–990. [Google Scholar] [CrossRef]
- Gurung, S.C.; Rai, B.; DIxit, K.; Worrall, E.; Paudel, P.R.; Dhital, R.; Sah, M.K.; Pandit, R.N.; Aryal, T.P.; Majhi, G.; et al. How to Reduce Household Costs for People with Tuberculosis: A Longitudinal Costing Survey in Nepal. Health Policy Plan. 2021, 36, 594–605. [Google Scholar] [CrossRef]
- Vo, L.N.Q.; Forse, R.J.; Codlin, A.J.; Dang, H.M.; Truong, V.V.; Nguyen, L.H.; Nguyen, H.B.; Nguyen, N.V.; Sidney-Annerstedt, K.; Lonnroth, K.; et al. Socio-Protective Effects of Active Case Finding on Catastrophic Costs from Tuberculosis in Ho Chi Minh City, Viet Nam: A Longitudinal Patient Cost Survey. BMC Health Serv. Res. 2021, 21, 1051. [Google Scholar] [CrossRef]
- Nguyen, L.H.; Codlin, A.J.; Vo, L.N.Q.; Dao, T.; Tran, D.; Forse, R.J.; Vu, T.N.; Le, G.T.; Luu, T.; Do, G.C.; et al. An Evaluation of Programmatic Community-Based Chest X-Ray Screening for Tuberculosis in Ho Chi Minh City, Vietnam. Trop. Med. Infect. Dis. 2020, 5, 185. [Google Scholar] [CrossRef] [PubMed]
- What Are Poverty Lines? Available online: https://www.worldbank.org/en/news/video/2017/04/14/what-are-poverty-lines (accessed on 7 March 2023).
- Currency Converter|Foreign Exchange Rates|OANDA. Available online: https://www.oanda.com/currency-converter/en/ (accessed on 7 March 2023).
- Shewade, H.D.; Gupta, V.; Satyanarayana, S.; Kharate, A.; Sahai, K.N.; Murali, L.; Kamble, S.; Deshpande, M.; Kumar, N.; Kumar, S.; et al. Active Case Finding among Marginalised and Vulnerable Populations Reduces Catastrophic Costs Due to Tuberculosis Diagnosis. Glob. Health Action 2018, 11, 1494897. [Google Scholar] [CrossRef] [PubMed]
- Morishita, F.; Yadav, R.-P.; Eang, M.T.; Saint, S.; Nishikiori, N. Mitigating Financial Burden of Tuberculosis through Active Case Finding Targeting Household and Neighbourhood Contacts in Cambodia. PLoS ONE 2016, 11, e0162796. [Google Scholar] [CrossRef] [PubMed]
- Muniyandi, M.; Thomas, B.E.; Karikalan, N.; Kannan, T.; Rajendran, K.; Saravanan, B.; Vohra, V.; Okorosobo, T.; Lönnroth, K.; Tripathy, S.P. Association of Tuberculosis With Household Catastrophic Expenditure in South India. JAMA Netw. Open 2020, 3, 20973. [Google Scholar] [CrossRef]
- Gurung, S.C.; Dixit, K.; Rai, B.; Caws, M.; Paudel, P.R.; Dhital, R.; Acharya, S.; Budhathoki, G.; Malla, D.; Levy, J.W.; et al. The Role of Active Case Finding in Reducing Patient Incurred Catastrophic Costs for Tuberculosis in Nepal. Infect. Dis. Poverty 2019, 8, 99. [Google Scholar] [CrossRef]
- Tran, B.X.; Nguyen, H.T.; Le, H.T.; Latkin, C.A.; Pham, H.Q.; Vu, L.G.; Le, X.T.T.; Nguyen, T.T.; Pham, Q.T.; Ta, N.T.K.; et al. Impact of COVID-19 on Economic Well-Being and Quality of Life of the Vietnamese During the National Social Distancing. Front. Psychol. 2020, 11, 565153. [Google Scholar] [CrossRef]
- Yang, J.; Panagoulias, P.; Demarchi, G. Monitoring COVID-19 Impacts on the Households in Vietnam. Results Snapshot from a High-Frequency Phone Survey of Households; World Bank Group: Washington, DC, USA, 2020. [Google Scholar]
- Wiemers, A.M.C.; Sidney Annerstedt, K.; Forse, R.J.; Phan, T.H.Y.; Codlin, A.J.; Dang, T.M.H.; Nguyen, H.L.; Vo, N.Q.L.; Lonnroth, K.; Nguyen, B.H.; et al. COVID-19 Lockdowns Resulting in Household Income Decline for People with TB in Ho Chi Minh City: Interrupted Time Series Analysis of Household Income Changes. In Proceedings of the 53rd Union World Conference on Lung Health, Virtual, 8–11 November 2022. [Google Scholar]
- Meghji, J.; Gregorius, S.; Madan, J.; Chitimbe, F.; Thomson, R.; Rylance, J.; Banda, N.P.; Gordon, S.B.; Corbett, E.L.; Mortimer, K.; et al. The Long Term Effect of Pulmonary Tuberculosis on Income and Employment in a Low Income, Urban Setting. Thorax 2021, 76, 387–395. [Google Scholar] [CrossRef]
- Pande, T.; Vasquez, N.A.; Cazabon, D.; Creswell, J.; Brouwer, M.; Ramis, O.; Stevens, R.H.; Ananthakrishnan, R.; Qayyum, S.; Alphonsus, C.; et al. Finding the Missing Millions: Lessons from 10 Active Case Finding Interventions in High Tuberculosis Burden Countries. BMJ Glob. Health 2020, 5, e003835. [Google Scholar] [CrossRef]
- Optimizing Active Case-Finding for Tuberculosis. Available online: https://www.who.int/publications-detail-redirect/9789290228486 (accessed on 17 March 2023).
- Lönnroth, K.; Glaziou, P.; Weil, D.; Floyd, K.; Uplekar, M.; Raviglione, M. Beyond UHC: Monitoring Health and Social Protection Coverage in the Context of Tuberculosis Care and Prevention. PLOS Med. 2014, 11, e1001693. [Google Scholar] [CrossRef]
- Aragão, F.B.A.; Arcêncio, R.A.; Fuentealba-Torres, M.; Carneiro, T.S.G.; Souza, L.L.L.; Alves, Y.M.; Fiorati, R.C. Impact of Social Protection Programs on Adults Diagnosed with Tuberculosis: Systematic Review. Rev. Bras. Enferm. 2021, 74, 3. [Google Scholar] [CrossRef]
- Siroka, A.; Ponce, N.A.; Lönnroth, K. Association between Spending on Social Protection and Tuberculosis Burden: A Global Analysis. Lancet Infect. Dis. 2016, 16, 473–479. [Google Scholar] [CrossRef] [PubMed]
- Wingfield, T.; Boccia, D.; Tovar, M.; Gavino, A.; Zevallos, K.; Montoya, R.; Lönnroth, K.; Evans, C.A. Defining Catastrophic Costs and Comparing Their Importance for Adverse Tuberculosis Outcome with Multi-Drug Resistance: A Prospective Cohort Study, Peru. PLOS Med. 2014, 11, e1001675. [Google Scholar] [CrossRef] [PubMed]
- National Surveys of Costs Faced by Tuberculosis Patients and Their Households 2015–2021. Available online: https://www.who.int/publications-detail-redirect/9789240065536 (accessed on 7 March 2023).
- Marius, O. Viet Nam Social Security Legal Reform: An Integrated Framework; International Labour Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Madan, J.; Lönnroth, K.; Laokri, S.; Squire, S.B. What Can Dissaving Tell Us about Catastrophic Costs? Linear and Logistic Regression Analysis of the Relationship between Patient Costs and Financial Coping Strategies Adopted by Tuberculosis Patients in Bangladesh, Tanzania and Bangalore, India. BMC Health Serv. Res. 2015, 15, 476. [Google Scholar] [CrossRef] [PubMed]

| All N = 212 | ACF N = 105 | PCF N = 107 | p-Value * | |
|---|---|---|---|---|
| Men, N (%) | 172 (81.1%) | 85 (80.9%) | 87 (81.3%) | 0.947 |
| Age, mean (SD) | 54 (16) | 62 (12) | 47 (15) | <0.001 |
| Age group, N (%) | <0.001 | |||
| 18–24 | 11 | 0 | 11 | |
| 25–34 | 22 | 3 | 19 | |
| 35–44 | 20 | 5 | 15 | |
| 45–54 | 42 | 20 | 22 | |
| 55–64 | 64 | 40 | 24 | |
| 65+ | 53 | 37 | 16 | |
| Completed secondary school, N (%) | 60 (28.3%) | 23 (21.9%) | 35 (34.6%) | 0.040 |
| Employment (including informal) pre-TB, N (%) | 191 (90.1%) | 95 (90.5%) | 96 (89.7%) | 0.854 |
| Monthly household income pre-TB in USD, median (IQR) | 529 (301–817) | 477 (258–774) | 581 (344–860) | 0.069 |
| Households living below poverty line **, N (%) | 19 (9%) | 11 (10%) | 8 (7%) | 0.445 |
| Number of household members, mean (SD) | 4 (2) | 4 (2) | 4 (2) | 0.061 |
| Enrolled in Social Health Insurance, N (%) | 176 (83.0%) | 88 (83.8%) | 88 (82.2%) | 0.761 |
| Diagnosed with at least one comorbidity, N (%) | 151 (71.2%) | 75 (71.4%) | 76 (71.0%) | 0.949 |
| History of TB, N (%) | 12 (5.7%) | 8 (7.6%) | 4 (3.7%) | 0.250 |
| Self-reported positive HIV status, N (%) | 5 (2.4%) | 0 (0.0%) | 5 (4.7%) | 0.060 |
| Weeks before treatment, median (IQR) | 5 (1–15) | 4 (0–12) | 6 (3–15) | 0.002 |
| Health provider visits before diagnosis, median (IQR) | 4 (3–7) | 3 (2–4) | 6 (3–7) | <0.001 |
| All (N = 212) | ACF (N = 105) | PCF (N = 107) | |||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | p-Value * | |
| Total cost (pre-treatment and treatment) | |||||||
| Direct medical | 201 (374) | 76 (17–226) | 118 (269) | 21 (6–76) | 282 (440) | 141 (75–292) | <0.001 |
| Direct non-medical | 338 (442) | 236 (106–431) | 298 (337) | 200 (82–391) | 376 (524) | 304 (136–448) | 0.095 |
| Total direct | 536 (683) | 350 (151–668) | 416 (555) | 258 (108–483) | 655 (773) | 429 (250–701) | <0.001 |
| Indirect | 1052 (1292) | 651 (12–1485) | 979 (1497) | 468 (0–1328) | 1124 (1147) | 925 (75–1559) | 0.067 |
| Total treatment | 1588 (1466) | 1208 (520–218) | 1395 (1498) | 957 (361–1862) | 1779 (1415) | 1359 (724–2482) | 0.006 |
| Pre-Treatment | |||||||
| Direct medical | 113 (276) | 30 (3–97) | 39 (118) | 6 (0–20) | 186 (356) | 82 (40–164) | <0.001 |
| Direct non-medical | 28 (72) | 4 (1–23) | 12 (37) | 2 (1–5) | 51 (153) | 10 (1–26) | <0.000 |
| Total direct | 141 (328) | 46 (5–143) | 51 (153) | 10 (1–26) | 229 (420) | 101 (56–198) | <0.000 |
| Treatment | |||||||
| Direct medical | 87 (212) | 13 (0–78) | 79 (234) | 7 (0–34) | 96 (188) | 35 (0–105) | 0.025 |
| Direct non-medical | 310 (426) | 218 (85–396) | 286 (332) | 188 (66–356) | 334 (502) | 231 (95–419) | 0.294 |
| Total direct | 395 (542) | 245 (102–540) | 365 (528) | 224 (81–409) | 425 (556) | 276 (115–591) | 0.141 |
| Total treatment | 1449 (1393) | 1088 (477–2041) | 1343 (1497) | 888 (317–1693) | 1553 (1282) | 1213 (649–2153) | 0.043 |
| Total (n = 212) | Ha Noi (n = 27) | Hai Phong (n = 43) | Da Nang (n = 20) | HCMC (n = 122) | p-Value * | |
|---|---|---|---|---|---|---|
| Household income pre-TB | ||||||
| Median monthly income (IQR) | 529 (301–817) | 473 (301–718) | 505 (237–688) | 645 (241–871) | 581 (505–237) | 0.106 |
| Pre-Treatment costs | ||||||
| Median direct costs (IQR) | 30 (3–97) | 46 (12–93) | 91 (9–160) | 13 (0–42) | 21 (0–84) | 0.008 |
| Treatment costs | ||||||
| Median direct costs (IQR) | 245 (102–540) | 550 (196–847) | 372 (224–696) | 257 (205–334) | 181 (54–356) | <0.001 |
| Median indirect costs (IQR) | 651 (16–1485) | 344 (0–1134) | 169 (0–1333) | 16 (0–778) | 1066 (301–1832) | <0.001 |
| Median total costs (IQR) | 1088 (477–2041) | 979 (587–2131) | 823 (307–1806) | 668 (249–988) | 1249 (527–2266) | 0.033 |
| Total costs (pre-treatment and treatment) | ||||||
| Median direct costs (IQR) | 350 (151–668) | 602 (272–959) | 517 (300–980) | 317 (219–398) | 227 (110–494) | <0.001 |
| Median indirect costs (IQR) | 651 (16–1485) | 344 (0–1134) | 169 (0–1333) | 16 (0–778) | 1066 (301–1832) | <0.001 |
| Median total costs (IQR) | 1208 (520–2189) | 1125 (587–2328) | 1152 (398–1932) | 668 (258–1000) | 1360 (591–2470) | 0.020 |
| Catastrophic cost incurrence | ||||||
| Number of households (%) | 122 (52.8%) | 16 (59.3%) | 26 (60.5%) | 4 (20.0%) | 66 (54.1%) | 0.016 ° |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dinh, L.V.; Wiemers, A.M.C.; Forse, R.J.; Phan, Y.T.H.; Codlin, A.J.; Annerstedt, K.S.; Dong, T.T.T.; Nguyen, L.; Pham, T.H.; Nguyen, L.H.; et al. Comparing Catastrophic Costs: Active vs. Passive Tuberculosis Case Finding in Urban Vietnam. Trop. Med. Infect. Dis. 2023, 8, 423. https://doi.org/10.3390/tropicalmed8090423
Dinh LV, Wiemers AMC, Forse RJ, Phan YTH, Codlin AJ, Annerstedt KS, Dong TTT, Nguyen L, Pham TH, Nguyen LH, et al. Comparing Catastrophic Costs: Active vs. Passive Tuberculosis Case Finding in Urban Vietnam. Tropical Medicine and Infectious Disease. 2023; 8(9):423. https://doi.org/10.3390/tropicalmed8090423
Chicago/Turabian StyleDinh, Luong V., Anja M. C. Wiemers, Rachel J. Forse, Yen T. H. Phan, Andrew J. Codlin, Kristi Sidney Annerstedt, Thuy T. T. Dong, Lan Nguyen, Thuong H. Pham, Lan H. Nguyen, and et al. 2023. "Comparing Catastrophic Costs: Active vs. Passive Tuberculosis Case Finding in Urban Vietnam" Tropical Medicine and Infectious Disease 8, no. 9: 423. https://doi.org/10.3390/tropicalmed8090423
APA StyleDinh, L. V., Wiemers, A. M. C., Forse, R. J., Phan, Y. T. H., Codlin, A. J., Annerstedt, K. S., Dong, T. T. T., Nguyen, L., Pham, T. H., Nguyen, L. H., Dang, H. M. T., Tuan, M. H., Le, P. T., Lonnroth, K., Creswell, J., Khan, A., Kirubi, B., Nguyen, H. B., Nguyen, N. V., & Vo, L. N. Q. (2023). Comparing Catastrophic Costs: Active vs. Passive Tuberculosis Case Finding in Urban Vietnam. Tropical Medicine and Infectious Disease, 8(9), 423. https://doi.org/10.3390/tropicalmed8090423







