Morbidity of Returning Travelers Seen in Community Urgent Care Centers throughout Israel †
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population and Data Collection
3. Definitions
3.1. Categorizing Travel Destinations
3.2. The Link between Morbidity and Travel
3.3. Statistical Analysis
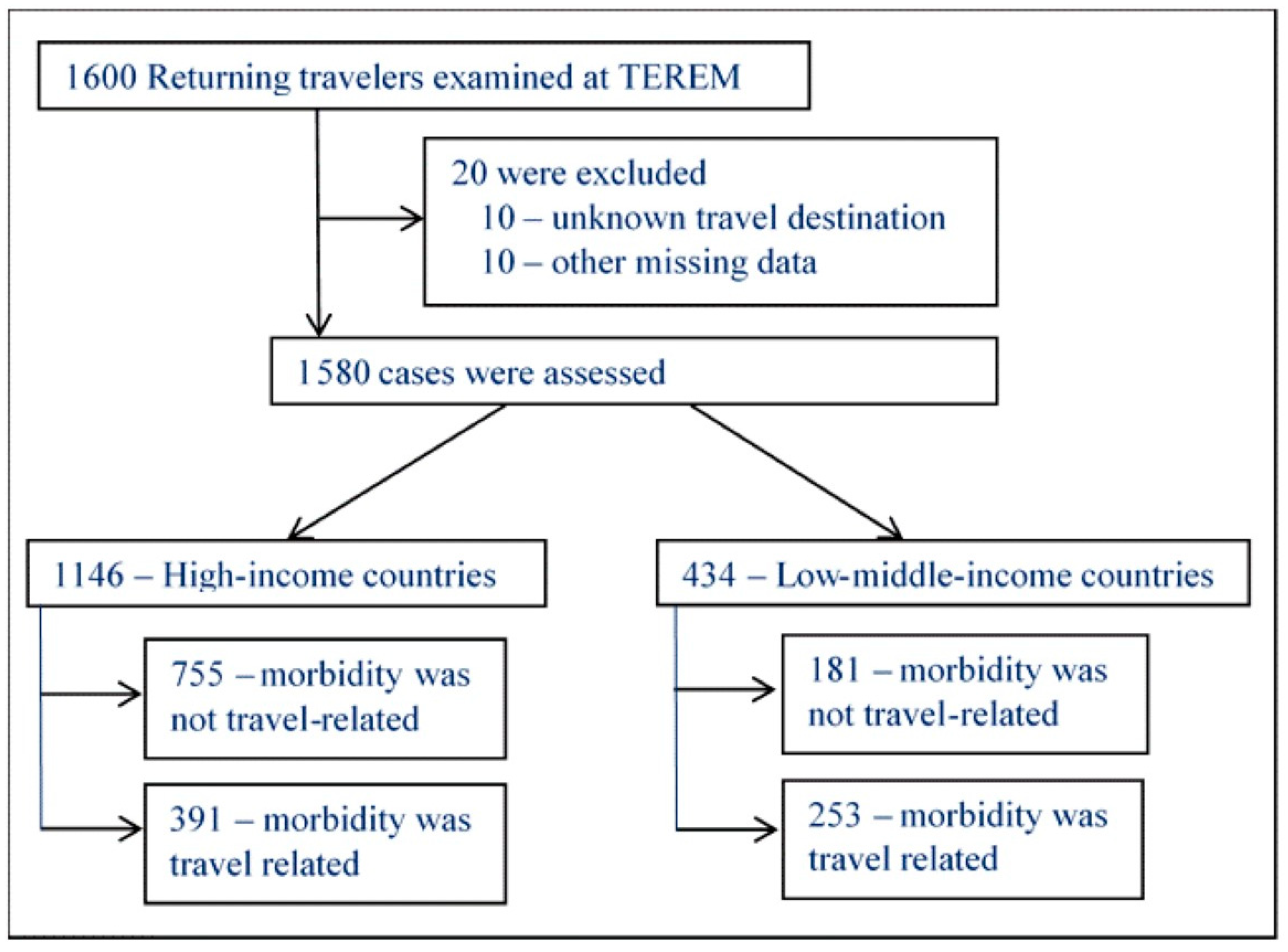
4. Results
5. Discussion
6. Limitations
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- International Tourist Arrivals Reach 1.4 Billion Two Years Ahead of Forecasts. Available online: https://www2.unwto.org/press-release/2019-01-21/international-tourist-arrivals-reach-14-billion-two-years-ahead-forecasts (accessed on 30 April 2023).
- Klinger, C.; Burns, J.; Movsisyan, A.; Biallas, R.; Norris, S.L.; Rabe, J.E.; Stratil, J.M.; Voss, S.; Wabnitz, K.; Rehfuess, E.A.; et al. Unintended health and societal consequences of international travel measures during the COVID-19 pandemic: A scoping review. J. Travel Med. 2021, 28, taab123. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.M.; Chen, J.L.; Li, G.; Baláž, V. Risk, uncertainty and ambiguity amid Covid-19: A multi-national analysis of international travel intentions. Ann. Tour Res. 2022, 92, 103346. [Google Scholar] [CrossRef] [PubMed]
- Flaherty, G.T.; Hamer, D.H.; Chen, L.H. Travel in the Time of COVID: A Review of International Travel Health in a Global Pandemic. Curr. Infect. Dis. Rep. 2022, 24, 129–145. [Google Scholar] [CrossRef]
- Stienlauf, S.; Meltzer, E.; Leshem, E.; Rendi-Wagner, P.; Schwartz, E. The profile of Israeli travelers to developing countries: Perspectives of a travel clinic. Harefuah 2010, 149, 559–562, 621. [Google Scholar] [PubMed]
- Han, C.T.; Flaherty, G. Profile of Travelers With Preexisting Medical Conditions Attending a Specialist Travel Medicine Clinic in Ireland. J. Travel Med. 2015, 22, 312–317. [Google Scholar] [CrossRef]
- Darrat, M.; Flaherty, G.T. Retrospective analysis of older travellers attending a specialist travel health clinic. Trop. Dis. Travel Med. Vaccines 2019, 5, 17. [Google Scholar] [CrossRef]
- Bühler, S.; Rüegg, R.; Steffen, R.; Hatz, C.; Jaeger, V.K. A profile of travelers—An analysis from a large swiss travel clinic. J. Travel Med. 2014, 21, 324–331. [Google Scholar] [CrossRef]
- Vlot, J.A.; Vive, M.G.D.; Brockhoff, H.J.; van Genderen, P.J.J.; Trompenaars, M.E.; van Steenbergen, J.E.; Visser, L.G. Predicting morbidity in older travellers during a short-term stay in the tropics: The ELDEST study. J. Travel Med. 2021, 28, taaa216. [Google Scholar] [CrossRef]
- Leder, K.; Torresi, J.; Libman, M.D.; Cramer, J.P.; Castelli, F.; Schlagenhauf, P.; Wilder-Smith, A.; Wilson, M.E.; Keystone, J.S.; Schwartz, E.; et al. GeoSentinel surveillance of illness in returned travelers, 2007–2011. Ann. Intern. Med. 2013, 158, 456–468. [Google Scholar] [CrossRef]
- Freedman, D.O.; Weld, L.H.; Kozarsky, P.E.; Fisk, T.; Robins, R.; von Sonnenburg, F.; Keystone, J.S.; Pandey, P.; Cetron, M.S. Spectrum of disease and relation to place of exposure among ill returned travelers. N. Engl. J. Med. 2006, 354, 119–130. [Google Scholar] [CrossRef]
- Boggild, A.K.; Castelli, F.; Gautret, P.; Torresi, J.; von Sonnenburg, F.; Barnett, E.D.; Greenaway, C.A.; Lim, P.L.; Schwartz, E.; Wilder-Smith, A.; et al. Vaccine preventable diseases in returned international travelers: Results from the GeoSentinel Surveillance Network. Vaccine 2010, 28, 7389–7395. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.E.; Weld, L.H.; Boggild, A.; Keystone, J.S.; Kain, K.C.; von Sonnenburg, F.; Schwartz, E. Fever in returned travelers: Results from the GeoSentinel Surveillance Network. Clin. Infect. Dis. 2007, 44, 1560–1568. [Google Scholar] [CrossRef] [PubMed]
- Urgent Care Centers. Ann. Emerg. Med. 2017, 70, 115–116. [CrossRef] [PubMed]
- The World Bank. Available online: https://data.worldbank.org/country/XN (accessed on 30 April 2023).
- Greenwood, Z.; Black, J.; Weld, L.; O’Brien, D.; Leder, K.; Von Sonnenburg, F.; Pandey, P.; Schwartz, E.; Connor, B.A.; Brown, G.; et al. Gastrointestinal infection among international travelers globally. J. Travel Med. 2008, 15, 221–228. [Google Scholar] [CrossRef]
- Swaminathan, A.; Torresi, J.; Schlagenhauf, P.; Thursky, K.; Wilder-Smith, A.; Connor, B.A.; Schwartz, E.; Vonsonnenberg, F.; Keystone, J.; O’Brien, D.P. A global study of pathogens and host risk factors associated with infectious gastrointestinal disease in returned international travellers. J. Infect. 2009, 59, 19–27. [Google Scholar] [CrossRef]
- Stoney, R.J.; Esposito, D.H.; Kozarsky, P.; Hamer, D.H.; Grobusch, M.P.; Gkrania-Klotsas, E.; Libman, M.; Gautret, P.; Lim, P.L.; Leder, K.; et al. Infectious diseases acquired by international travellers visiting the USA. J. Travel Med. 2018, 25, tay053. [Google Scholar] [CrossRef]
- Tonellato, D.J.; Guse, C.E.; Hargarten, S.W. Injury deaths of US citizens abroad: New data source, old travel problem. J. Travel Med. 2009, 16, 304–310. [Google Scholar] [CrossRef]
- Guse, C.E.; Cortés, L.M.; Hargarten, S.W.; Hennes, H.M. Fatal injuries of US citizens abroad. J. Travel Med. 2007, 14, 279–287. [Google Scholar] [CrossRef]
- Wyler, B.A.; Young, H.M.; Hargarten, S.W.; Cahill, J.D. Risk of deaths due to injuries in travellers: A systematic review. J. Travel Med. 2022, 29, taac074. [Google Scholar] [CrossRef]
- Driessen, S.O.; Cobelens, F.G.; Ligthelm, R.J. Travel-related morbidity in travelers with insulin-dependent diabetes mellitus. J. Travel Med. 1999, 6, 12–15. [Google Scholar] [CrossRef]
- Stienlauf, S.; Streltsin, B.; Meltzer, E.; Kopel, E.; Leshem, E.; Segal, G.; Kivity, S.; Schwartz, E. Chronic illnesses in travelers to developing countries. Travel Med. Infect. Dis. 2014, 12, 757–763. [Google Scholar] [CrossRef] [PubMed]
- Leder, K.; Tong, S.; Weld, L.; Kain, K.C.; Wilder-Smith, A.; von Sonnenburg, F.; Black, J.; Brown, G.V.; Torresi, J. Illness in travelers visiting friends and relatives: A review of the GeoSentinel Surveillance Network. Clin. Infect. Dis. 2006, 43, 1185–1193. [Google Scholar] [CrossRef] [PubMed]
- Gorodetzer, R.; Alpert, E.A.; Orr, Z.; Unger, S.; Zalut, T. Lessons learned from an evaluation of referrals to the emergency department. Isr. J. Health Policy Res. 2020, 9, 18. [Google Scholar] [CrossRef] [PubMed]
| Low–Middle-Income Countries, n = 434 | High-Income Countries, n = 1146 | p-Value | |
|---|---|---|---|
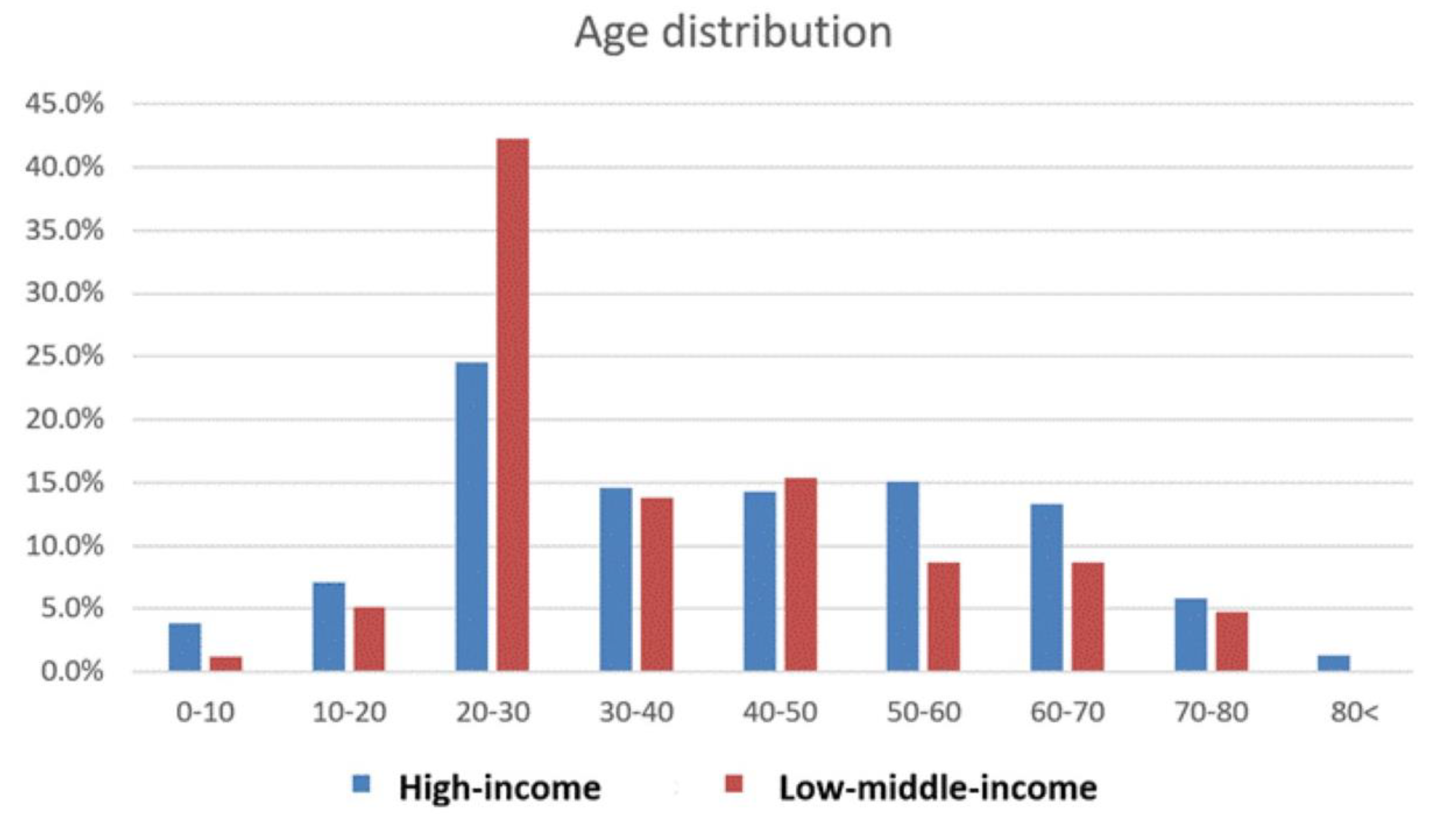
| Mean age (year ± SD) | 36.8 (±16.4) | 41.4 (±19.1) | p = 0.0017 |
| Females, n (%) | 218 (50.2) | 578 (54) | p = 0.35 |
| Pre-travel vaccinations, n (%) | 154 (35.5) | 76(6.6) | p < 0.001 |
| Mean days from return to arrival at TEREM (±SD) | 2.8 (±3.2) | 2.3 (±3.6) | p = 0.16 |
| Mean duration of trip (days ± SD) | 30.1 (±41.2) | 10.0 (±10.6) | p < 0.001 |
| Referred to emergency department, n (%) | 29 (6.7) | 82 (7.2) | p = 0.94 |
| Morbidity | Low–Middle-Income Countries, n = 434 (%) | High-Income Countries, n = 1146 (%) | p-Value |
|---|---|---|---|
| Total of travel related morbidity | 253 (58.3) | 391 (34.1) | <0.001 |
| Acute diarrhea | 73 (28.85) | 26 (6.6) | <0.001 |
| Non-diarrheal gastrointestinal disorder | 15 (5.9) | 23 (5.9) | 0.98 |
| Respiratory illness | 59 (23.3) | 146 (37.3) | 0.002 |
| Dermatologic disorder | 40 (15.8) | 56 (14.3) | 0.6 |
| Injury | 25 (9.9) | 50 (12.8) | 0.26 |
| Cardiovascular disorder | 9 (3.6) | 24 (6.1) | 0.14 |
| Systemic febrile illness | 7 (2.8) | 0 (0.0) | 0.009 |
| Other * | 25 (9.9) | 66 (16.9) | 0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Itzkowitz, E.; Alpert, E.A.; Farojeh, A.Z.; Zimmerman, D.R.; Schwartz, E.; Lachish, T. Morbidity of Returning Travelers Seen in Community Urgent Care Centers throughout Israel. Trop. Med. Infect. Dis. 2023, 8, 319. https://doi.org/10.3390/tropicalmed8060319
Itzkowitz E, Alpert EA, Farojeh AZ, Zimmerman DR, Schwartz E, Lachish T. Morbidity of Returning Travelers Seen in Community Urgent Care Centers throughout Israel. Tropical Medicine and Infectious Disease. 2023; 8(6):319. https://doi.org/10.3390/tropicalmed8060319
Chicago/Turabian StyleItzkowitz, Eyal, Evan A. Alpert, Abdulhadi Z. Farojeh, Deena R. Zimmerman, Eli Schwartz, and Tamar Lachish. 2023. "Morbidity of Returning Travelers Seen in Community Urgent Care Centers throughout Israel" Tropical Medicine and Infectious Disease 8, no. 6: 319. https://doi.org/10.3390/tropicalmed8060319
APA StyleItzkowitz, E., Alpert, E. A., Farojeh, A. Z., Zimmerman, D. R., Schwartz, E., & Lachish, T. (2023). Morbidity of Returning Travelers Seen in Community Urgent Care Centers throughout Israel. Tropical Medicine and Infectious Disease, 8(6), 319. https://doi.org/10.3390/tropicalmed8060319








