Under-Reporting of Tuberculosis Disease among Children and Adolescents in Low and Middle-Income Countries: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Quality Assessment
3. Results
4. Discussion
4.1. Reporting Gap
4.2. Interventions
4.3. Limitations
4.4. Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Article | Title/ Abstract | Background/ Rationale | Objectives | Study Design | Setting | Participants | Variables | Data Sources/ Measurement | Bias | Study Size | Quantitative Variables | Statistical Methods | Participants | Descriptive Data | Outcome Data | Main Results | Other Analyses | Key Results | Limitations | Interpretation | Generalisability | Funding | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Berman 1992 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 15 | |||||||
| Edginton 2005 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 18 | ||||
| Edginton 2006 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 14 | ||||||||
| Marais 2006 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 18 | ||||
| Du Preez 2011 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 20 | ||
| Lestari 2011 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 21 | |
| Rose 2013 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 20 | ||
| Ade 2013 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 20 | ||
| Coghlan 2015 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 14 | ||||||||
| Joshi 2015 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 20 | ||
| Tollefson 2016 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 20 | ||
| Li 2019 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 21 | |
| Du Preez 2018 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 21 | |
| Fatima 2019 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 18 | ||||
| Siddaiah 2019 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 21 | |
| Du Preez 2020 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 21 | |
| Shibu 2020 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 20 | ||
| Yaqoob 2021 | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | 20 |
References
- World Health Organization. Global Tuberculosis Report. Available online: https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022 (accessed on 5 March 2023).
- Verkuijl, S.; Sekadde, M.P.; Dodd, P.J.; Arinaitwe, M.; Chiang, S.S.; Brands, A.; Viney, K.; Sismanidis, C.; Jenkins, H.E. Addressing the Data Gaps on Child and Adolescent Tuberculosis. Pathogens 2022, 11, 352. [Google Scholar] [CrossRef] [PubMed]
- Dodd, P.J.; Gardiner, E.; Coghlan, R.; Seddon, J.A. Burden of childhood tuberculosis in 22 high-burden countries: A mathematical modelling study. Lancet Glob. Health 2014, 2, e453–e459. [Google Scholar] [CrossRef] [PubMed]
- Ranasinghe, L.; Achar, J.; Gröschel, M.I.; Whittaker, E.; Dodd, P.J.; Seddon, J.A. Global impact of COVID-19 on childhood tuberculosis: An analysis of notification data. Lancet Glob. Health 2022, 10, e1774–e1781. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Assessment of Surveillance Data Workbook. Available online: https://cdn.who.int/media/docs/default-source/hq-tuberculosis/global-task-force-on-tb-impact-measurement/meetings/2010-11/3_workbook_en.pdf?sfvrsn=79a1aa86_3 (accessed on 22 February 2023).
- Basile, F.W.; Nabeta, P.; Ruhwald, M.; Song, R. Pediatric Tuberculosis Diagnostics: Present and Future. J. Pediatr. Infect. Dis. Soc. 2022, 11 (Suppl. 3), S85–S93. [Google Scholar] [CrossRef] [PubMed]
- Arscott-Mills, T.; Ejelonu, A.; Mokalane, K.; Machao, G.; Kololo, S.; Ncube, R.; Caiphus, C.; Steenhoff, A.P. One third of child TB cases were missing from the national TB register in Botswana. Int. J. Tuberc. Lung Dis. 2021, 25, 142–144. [Google Scholar] [CrossRef]
- PRISMA. PRISMA: Transparent Reporting of Systematic Reviews and Meta-Analyses. Available online: http://www.prisma-statement.org/?AspxAutoDetectCookieSupport=1 (accessed on 5 October 2022).
- Registration PROSPERO. PRISMA. Available online: http://prisma-statement.org/Protocols/Registration (accessed on 22 May 2023).
- MacPherson, P.; Houben, R.M.G.J.; Glynn, J.R.; Corbett, E.L.; Kranzer, K. Pre-treatment loss to follow-up in tuberculosis patients in low- and lower-middle-income countries and high-burden countries: A systematic review and meta-analysis. Bull. World Health Organ. 2014, 92, 126–138. [Google Scholar] [CrossRef]
- Low & Middle Income Countries. The World Bank. Available online: https://data.worldbank.org/country/XO (accessed on 5 October 2022).
- WHO. Adolescent Health. Published 2023. Available online: https://www.who.int/health-topics/adolescent-health#tab=tab_1 (accessed on 10 April 2023).
- Covidence Systematic Review Software, Veritas Health Innovation, Melbourne, Australia. Available online: www.covidence.org (accessed on 5 October 2022).
- The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Equator Network. Available online: https://www.equator-network.org/reporting-guidelines/strobe/ (accessed on 5 March 2023).
- Tollefson, D.; Ngari, F.; Mwakala, M.; Gethi, D.; Kipruto, H.; Cain, K.; Bloss, E. Under-reporting of sputum smear-positive tuberculosis cases in Kenya. Int. J. Tuberc. Lung Dis. 2016, 20, 1334–1341. [Google Scholar] [CrossRef]
- Marais, B.J.; Hesseling, A.C.; Gie, R.P.; Schaaf, H.S.; Beyers, N. The burden of childhood tuberculosis and the accuracy of community-based surveillance data. Int. J. Tuberc. Lung Dis. 2006, 10, 259–263. [Google Scholar]
- du Preez, K.; Schaaf, H.S.; Dunbar, R.; Swartz, A.; Bissell, K.; Enarson, D.A.; Hesseling, A.C. Incomplete registration and reporting of culture-confirmed childhood tuberculosis diagnosed in hospital. Public Health Action 2011, 1, 19–24. [Google Scholar] [CrossRef]
- du Preez, K.; Schaaf, H.S.; Dunbar, R.; Swartz, A.; Naidoo, P.; Hesseling, A.C. Closing the reporting gap for childhood tuberculosis in South Africa: Improving hospital referrals and linkages. Public Health Action 2020, 10, 38–46. [Google Scholar] [CrossRef]
- Ade, S.; Harries, A.D.; Trébucq, A.; Hinderaker, S.G.; Ade, G.; Agodokpessi, G.; Affolabi, D.; Koumakpaï, S.; Anagonou, S.; Gninafon, M. The burden and outcomes of childhood tuberculosis in Cotonou, Benin. Public Health Action 2013, 3, 15–19. [Google Scholar] [CrossRef]
- Yaqoob, A.; Hinderaker, S.G.; Fatima, R.; Najmi, H.; Haq, A.U. How do private practitioners in Pakistan manage children suspected having tuberculosis? A cross sectional study. BMC Public Health 2021, 21, 71. [Google Scholar] [CrossRef]
- Fatima, R.; Yaqoob, A.; Qadeer, E.; Hinderaker, S.G.; Ikram, A.; Sismanidis, C. Measuring and addressing the childhood tuberculosis reporting gaps in Pakistan: The first ever national inventory study among children. PLoS ONE 2019, 14, e0227186. [Google Scholar] [CrossRef]
- Edginton, M.E.; Wong, M.L.; Hodkinson, H.J. Tuberculosis at Chris Hani Baragwanath Hospital: An intervention to improve patient referrals to district clinics. Int. J. Tuberc. Lung Dis. 2006, 10, 1018–1022. [Google Scholar]
- Shibu, V.; Daksha, S.; Rishabh, C.; Sunil, K.; Devesh, G.; Lal, S.; Jyoti, S.; Kiran, R.; Bhavin, V.; Amit, K.; et al. Tapping private health sector for public health program? Findings of a novel intervention to tackle TB in Mumbai, India. Indian J. Tuberc. 2020, 67, 189–201. [Google Scholar] [CrossRef]
- Joshi, B.; Chinnakali, P.; Shrestha, A.; Das, M.; Kumar, A.M.V.; Pant, R.; Lama, R.; Sarraf, R.R.; Dumre, S.P.; Harries, A.D. Impact of intensified case-finding strategies on childhood TB case registration in Nepal. Public Health Action 2015, 5, 93–98. [Google Scholar] [CrossRef]
- Lestari, T.; Probandari, A.; Hurtig, A.-K.; Utarini, A. High caseload of childhood tuberculosis in hospitals on Java Island, Indonesia: A cross sectional study. BMC Public Health 2011, 11, 784. [Google Scholar] [CrossRef]
- Coghlan, R.; Gardiner, E.; Amanullah, F.; Ihekweazu, C.; Triasih, R.; Grzemska, M.; Sismanidis, C. Understanding Market Size and Reporting Gaps for Paediatric TB in Indonesia, Nigeria and Pakistan: Supporting Improved Treatment of Childhood TB in the Advent of New Medicines. PLoS ONE 2015, 10, e0138323. [Google Scholar] [CrossRef]
- Li, T.; Shewade, H.D.; Soe, K.T.; Rainey, J.J.; Zhang, H.; Du, X.; Wang, L. Under-reporting of diagnosed tuberculosis to the national surveillance system in China: An inventory study in nine counties in 2015. BMJ Open 2019, 9, e021529. [Google Scholar] [CrossRef]
- Edginton, M.E.; Wong, M.L.; Phofa, R.; Mahlaba, D.; Hodkinson, H.J. Tuberculosis at Chris Hani Baragwanath Hospital: Numbers of patients diagnosed and outcomes of referrals to district clinics. Int. J. Tuberc. Lung Dis. 2005, 9, 398–402. [Google Scholar]
- Satyanarayana, S.; Shivashankar, R.; Vashist, R.P.; Chauhan, L.S.; Chadha, S.S.; Dewan, P.K.; Wares, F.; Sahu, S.; Singh, V.; Wilson, N.C.; et al. Characteristics and Programme-Defined Treatment Outcomes among Childhood Tuberculosis (TB) Patients under the National TB Programme in Delhi. PLoS ONE 2010, 5, e13338. [Google Scholar] [CrossRef] [PubMed]
- Siddaiah, A.; Ahmed, M.N.; Kumar, A.M.V.; D’souza, G.; Wilkinson, E.; Maung, T.M.; Rodrigues, R. Tuberculosis notification in a private tertiary care teaching hospital in South India: A mixed-methods study. BMJ Open 2019, 9, e023910. [Google Scholar] [CrossRef] [PubMed]
- Teo, S.S.S.; Alfaham, M.; Evans, M.R.; Watson, J.M.; Riordan, A.; Sonnenberg, P.; Clark, J.; Hayward, A.; Sharland, M.; Moore-Gillon, J.; et al. An evaluation of the completeness of reporting of childhood tuberculosis. Eur. Respir. J. 2009, 34, 176–179. [Google Scholar] [CrossRef] [PubMed]
- Snow, K.; Yadav, R.; Denholm, D.; Sawyer, S.; Graham, S. Tuberculosis among children, adolescents and young adults in the Philippines: A surveillance report. West. Pac. Surveill. Response J. 2018, 9, 16–20. [Google Scholar] [CrossRef] [PubMed]
- du Preez, K.; Schaaf, H.S.; Dunbar, R.; Walters, E.; Swartz, A.; Solomons, R.; Hesseling, A.C. Complementary surveillance strategies are needed to better characterise the epidemiology, care pathways and treatment outcomes of tuberculosis in children. BMC Public Health 2018, 18, 397. [Google Scholar] [CrossRef]
- Rose, P.C.; Schaaf, H.S.; Du Preez, K.; Seddon, J.; Garcia-Prats, A.; Zimri, K.; Dunbar, R.; Hesseling, A.C. Completeness and accuracy of electronic recording of paediatric drug-resistant tuberculosis in Cape Town, South Africa. Public Health Action 2013, 3, 214–219. [Google Scholar] [CrossRef]
- Berman, S.; Kibel, M.A.; Fourie, P.B.; Strebel, P.M. Childhood tuberculosis and tuberculous meningitis: High incidence rates in the Western Cape of South Africa. Tuber. Lung Dis. 1992, 73, 349–355. [Google Scholar] [CrossRef]
- Dunbar, R.; Lawrence, K.; Verver, S.; Enarson, D.A.; Lombard, C.; Hargrove, J.; Caldwell, J.; Beyers, N.; Barnes, J.M. Accuracy and completeness of recording of confirmed tuberculosis in two South African communities. Int. J. Tuberc. Lung Dis. 2011, 15, 337–343. [Google Scholar] [CrossRef]
- Yuen, C.; Szkwarko, D.; Dubois, M.; Shahbaz, S.; Yuengling, K.; Urbanowski, M.; Bain, P.; Brands, A.; Masini, T.; Verkuijl, S.; et al. Tuberculosis care models for children and adolescents: A scoping review. Bull. World Health Organ. 2022, 100, 777–788L. [Google Scholar] [CrossRef]
- Zawedde-Muyanja, S.; Nakanwagi, A.; Dongo, J.P.; Sekadde, M.P.; Nyinoburyo, R.; Ssentongo, G.; Detjen, A.K.; Mugabe, F.; Nakawesi, J.; Karamagi, Y.; et al. Decentralisation of child tuberculosis services increases case finding and uptake of preventive therapy in Uganda. Int. J. Tuberc. Lung Dis. 2018, 22, 1314–1321. [Google Scholar] [CrossRef]
- Pembi, E.; John, S.; Dumre, S.P.; Ahmadu, B.U.; Vuong, N.L.; Ebied, A.; Mizukami, S.; Huy, N.T.; Cuevas, L.E.; Hirayama, K. Impact of political conflict on tuberculosis notifications in North-east Nigeria, Adamawa State: A 7-year retrospective analysis. BMJ Open 2020, 10, e035263. [Google Scholar] [CrossRef]
- Hong, S.-J.; Park, Y.-S.; An, H.; Kang, S.-M.; Cho, E.-H.; Shin, S.-S. Factors leading to under-reporting of tuberculosis in the private sector in Korea. Int. J. Tuberc. Lung Dis. 2012, 16, 1221–1227. [Google Scholar] [CrossRef]
- Bassili, A.; Grant, A.D.; El-Mohgazy, E.; Galal, A.; Glaziou, P.; Seita, A.; Abubakar, I.; Bierrenbach, A.L.; Crofts, J.P.; Van Hest, N.A. Estimating tuberculosis case detection rate in resource-limited countries: A cap-ture-recapture study in Egypt. Int. J. Tuberc. Lung Dis. 2010, 14, 727–732. [Google Scholar]
- Huseynova, S.; Hashim, D.S.; Tbena, M.R.; Harris, R.; Bassili, A.; Abubakar, I.; Glaziou, P.; Floyd, K.; Van Hest, N.A. Estimating tuberculosis burden and reporting in resource-limited countries: A cap-ture-recapture study in Iraq. Int. J. Tuberc. Lung Dis. 2013, 17, 462–467. [Google Scholar] [CrossRef]
- Bassili, A.; Al-Hammadi, A.; Al-Absi, A.; Glaziou, P.; Seita, A.; Abubakar, I.; Bierrenbach, A.L.; Van Hest, N.A. Estimating the tuberculosis burden in resource-limited countries: A capture-recapture study in Yemen. Int. J. Tuberc. Lung Dis. 2013, 17, 456–461. [Google Scholar] [CrossRef]
- Podewils, L.J.; Bantubani, N.; Bristow, C.; Bronner, L.E.; Peters, A.; Pym, A.; Mametja, L.D. Completeness and Reliability of the Republic of South Africa National Tuberculosis (TB) Surveillance System. BMC Public Health 2015, 15, 765. [Google Scholar] [CrossRef]
- Dunbar, R.; Van Hest, R.; Lawrence, K.; Verver, S.; Enarson, D.A.; Lombard, C.; Beyers, N.; Barnes, J.M. Capture-recapture to estimate completeness of tuberculosis surveillance in two communities in South Africa. Int. J. Tuberc. Lung Dis. 2011, 15, 1038–1043. [Google Scholar] [CrossRef]

| Set | PubMed/MedLine |
|---|---|
| 1 | Childhood tuberculosis |
| 2 | Childhood TB |
| 3 | Pediatric TB |
| 4 | Paediatric TB |
| 5 | Pediatric tuberculosis |
| 6 | Paediatric tuberculosis |
| 7 | Sets 1–6 were combined with “OR” |
| 8 | Under-reporting |
| 9 | Under reporting |
| 10 | Reporting gap |
| 11 | Registration |
| 12 | Notification |
| 13 | Sets 11–12 were combined with “OR” |
| 14 | Set 7 and Sets 8–10, 13 were combined with “AND” |
| 15 | Sets 1–14 were limited to 1992–2022 |
| Articles Describing Reporting Gap | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| # | Paper | Study Type | Year | Country (ies) | Age Range (Years) | TB Type | Hospital Type/ Reporting Body | Reported Gap | Characteristics of Reported Gap |
| 1 | Berman et al. | Descriptive study | 1992 | South Africa | 0–14 | TB meningitis | 75 hospitals in the Western Cape Health Region/ Department of National Health and Population Development | 44% (105/238) | Noted that 16% of cases were excluded for an incorrect diagnosis, double notification, or other documentation errors. |
| 2 | Edginton et al. | Descriptive study including qualitative interviews | 2005 | South Africa | * | * | Chris Hani Baragwanath Hospital (tertiary hospital)/NTP | 31% (285/1291) | Most patients who died were not recorded. |
| 3 | Marais et al. | Prospective Observational Study | 2006 | South Africa | 0–12 | General | 5 primary healthcare clinics in Cape Town/NTP | 12% (54/443) | Patients were less likely to be reported if diagnosed at a referral hospital or if had more severe disease. |
| 4 | du Preez et al. | Retrospective cohort study | 2011 | South Africa | 0–12 | General | Tygerberg Children’s Hospital in Cape Town/ETR.net | 38% (101/267) | Patients were less likely to be reported if had disseminated TB (in sub-analysis if had TB meningitis, but not miliary TB) or death prior to referral. |
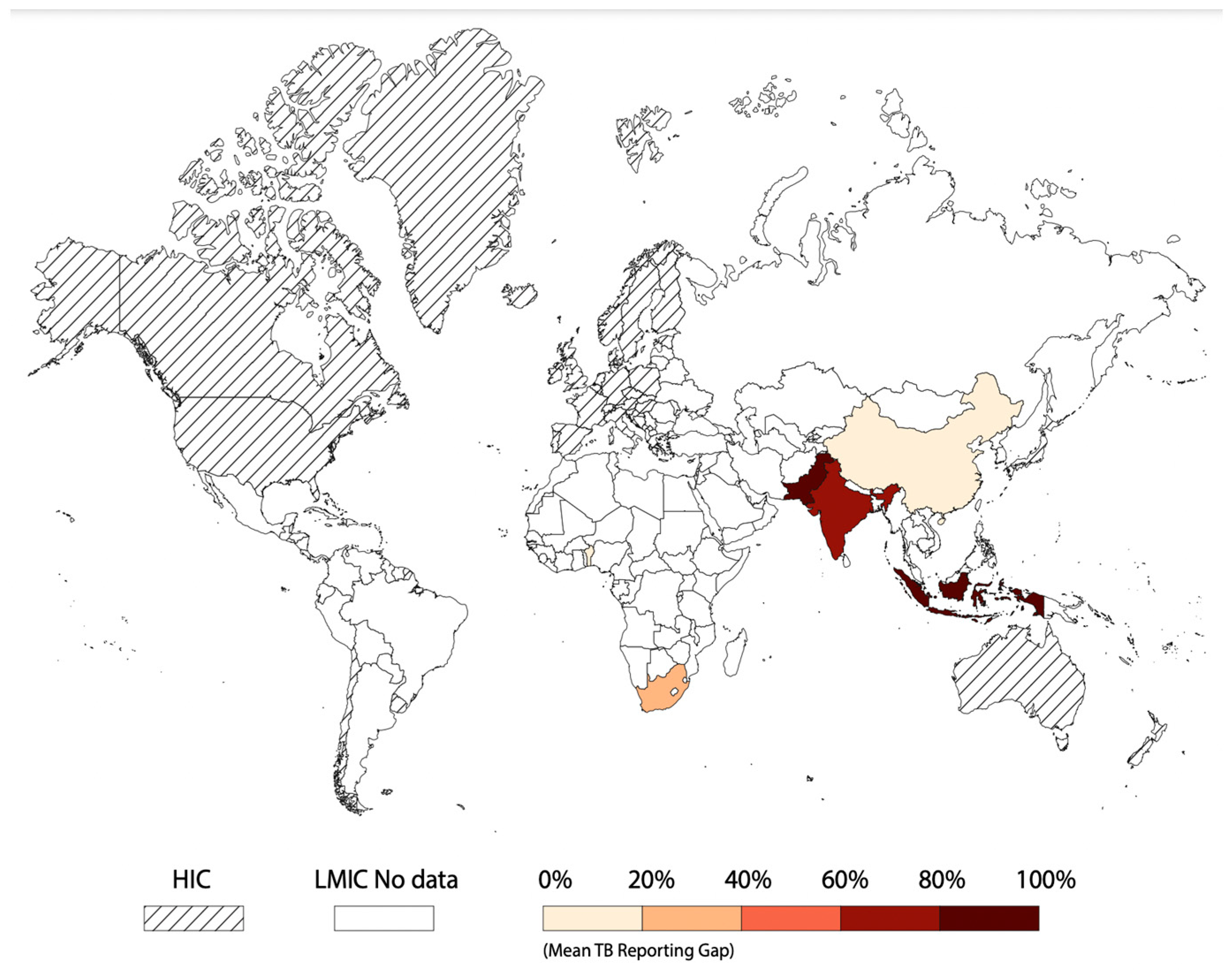
| 5 | Lestari et al. | Cross sectional study | 2011 | Indonesia | 0–14 | General | 32 DOTS hospitals/NTP | 98% (4746/ 4821) | More than half of child TB cases were in children less than 5 years old. Many DOTS hospitals did not have records of cases of child TB or report these cases to the NTP. |
| 6 | Rose et al. | Retrospective cohort study | 2013 | South Africa | 0–14 | General, drug- resistant | Tygerberg Children’s Hospital and its outreach clinics or Brooklyn Hospital for Chest Diseases (BHCD)/NTP | 36% (28/77) | Only a small number of online registrations were children. If children were not referred to local TB hospitals or clinics, there was no mechanism to ensure they were registered in EDR.web. |
| 7 | Ade et al. | Cross- sectional, retrospective cohort study | 2013 | Benin | 0–14 | General | 5 public or private basic management units (BMUs) in Cotonou/NTP | 16% (29/182) | There was more under-reporting in children under 5 years old. Extrapulmonary TB was less likely to be reported, thought to be due to misdiagnosis by healthcare workers due to lack of training. |
| 8 | Coghlan et al. | Exploratory assessments, record reviews, interviews of healthcare providers | 2015 | Indonesia, Nigeria, Pakistan | * | * | Both public and private sector health facilities outside the network of national TB control programs (non-NTP facilities)/NTP | Varied; cases diagnosed but unreported— Indonesia (985), Pakistan (463), Nigeria (24) ** | Private sector did not provide data to the NTP. There is a low level of suspicion for childhood TB in Nigeria generally. |
| 9 | Tollefson et al. | National-level retrospective TB inventory study | 2016 | Kenya | 0–55+ (0–24) | General | Laboratory registers from public or private laboratories/ National TB surveillance systems (TIBU) | 21% (715/3409) | Under-reporting was the greatest in the sub-counties with a high burden of TB, thought this may be due to pre-treatment loss to follow-up. Unreported cases were more likely if diagnosed at private and large facilities. |
| 10 | Li et al. | Retrospective inventory study (record review) | 2018 | China | <15, 15–64, ≥65 | Pulmonary TB or TB pleurisy | Nine provinces across the eastern, central, and western regions of China/ Tuberculosis Information Management Systems (TBIMS) | 19.3% (1082/ 5606) | Noted that age < 15 years, type of TB (pleurisy), recording source and region (eastern or central) were more likely to be under- reported. Discussed that large national and regional reference hospitals have high workload and limited resources for extra staff that affects reporting. The location where pediatric patients are typically treated (pediatric hospitals or large general hospitals) are not directly connected to TBIMS. Reporting regulations for TB pleurisy vary by province which can lead to under-reporting. |
| 11 | Fatima et al. | Nationwide cluster-based cross-sectional study | 2019 | Pakistan | 0–14 | General | Health facilities in 12 districts including NTP and non-NTP public health services, private health services, private laboratories/ NTP | 78% (5070/ 6525) | Reporting differed by province; under-reporting was higher in boys (84%) than girls (68%). Under-reporting was more common in clinically diagnosed cases (78%) than bacteriologically confirmed cases (76%). |
| 12 | Siddaiah et al. | Mixed-methods study with retrospective review and key informant interviews and focus groups | 2019 | India | 1–65+ (1–14, 15–24) | General | Private tertiary-level teaching hospital in Bengaluru, Karnataka State, South India/Indian RNTCP, a vertical national health program, with online notification portal Nikshay | 76.8% (2935/ 3820) missing notifications, 9.3% (82/885) cases recorded in electronic portal For ages 0–14 (24/264, 9.1% notified) and for ages 15–24 (118/476, 24.8% notified) | Quantitative Data: - Seven percent of the total patients were children <15 years - Notification was significantly higher with microbiologically confirmed diagnoses - Notification was significantly lower in inpatients, children, and patients found through laboratory/pharmacy systems Qualitative Data: - Interviews described barriers to notification including diagnostic procedures and treatment, misconceptions about the notification process are common - Interviews described solutions including establishing more hospital systems for notifications |
| 13 | Yaqoob et al. | Cross-sectional study | 2021 | Pakistan | 0–14 | General | Non-NTP private facilities in 12 districts across Pakistan/NTP | 97% (6332/ 6519) | Cases were less likely to be reported if private doctors started TB therapy themselves. Noted poor coordination between treatment centers and laboratories as potential cause for under-reporting. Noted inadequate counseling for patients with presumed TB and weak referral mechanisms. |
| Interventions Described to Close Reporting Gap | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| # | Paper | Study Type | Year | Country (ies) | Age Range (Years) | TB Type | Hospital Type/ Reporting Body | Intervention | Effectiveness |
| 14 | Edginton et al. | Intervention study | 2006 | South Africa | 0–55+, (0–14, 15–34) | General | Chris Hani Baragwanath hospital, (tertiary hospital) | Establishment of TB care center with registration within the hospital, death registration, education, and referrals | Increased patient registration with 94% of patients successfully referred to clinics. |
| 15 | Joshi et al. | Retrospective record review using routinely collected data | 2015 | Nepal | 0–14 | General | Seven of the 10 districts/ Nepal NTP | Intensified case finding detection with direct registration | Cases of childhood TB increased from 271 to 360 in the intervention districts (case registration rate from 18.2 to 24.2/100,000) compared with 97 to 113 in the control districts (case registration rate from 13.4 to 15.6/100,000). |
| 16 | du Preez et al. | Prospective cohort study | 2018 | South Africa | 0–12 | General | Tygerberg Hospital | Implementation of clinical surveillance along with previous laboratory surveillance, with the support of referral services between hospitals and local clinics | Clinical surveillance identified 237 (60%) of children that would have been missed by prior laboratory-based surveillance. Noted specific populations that were more likely to be identified by clinical surveillance including younger children, children with pulmonary TB, children with TB/HIV coinfection. |
| 17 | du Preez et al. | Prospective and retrospective cohort study | 2020 | South Africa | 0–13 | General | Tygerberg Hospital | Creation of a dedicated TB referral service within a pediatric ward | Successful reporting in 227/272 (84%) of children during the intervention period. Patients with culture-confirmed, drug-susceptible TB were more likely to be reported during the intervention period. |
| 18 | Shibu et al. | Intervention study | 2020 | India | 0–65+ (0–14, 15–24) | General | 8789 private doctors, 3438 chemists, and 985 laboratories | Pilot program “Private-practitioner interface agency (PPIA)” that engaged private providers by providing additional resources, monitoring quality, and supporting patients | PPIA notified 60,366 TB cases of tuberculosis in a 4-year period. The annual case notification rate per 100,000 population increased from 272 in 2013 pre-intervention to 416 in 2017. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Linn, A.R.; Dubois, M.M.; Steenhoff, A.P. Under-Reporting of Tuberculosis Disease among Children and Adolescents in Low and Middle-Income Countries: A Systematic Review. Trop. Med. Infect. Dis. 2023, 8, 300. https://doi.org/10.3390/tropicalmed8060300
Linn AR, Dubois MM, Steenhoff AP. Under-Reporting of Tuberculosis Disease among Children and Adolescents in Low and Middle-Income Countries: A Systematic Review. Tropical Medicine and Infectious Disease. 2023; 8(6):300. https://doi.org/10.3390/tropicalmed8060300
Chicago/Turabian StyleLinn, Alexandra R., Melanie M. Dubois, and Andrew P. Steenhoff. 2023. "Under-Reporting of Tuberculosis Disease among Children and Adolescents in Low and Middle-Income Countries: A Systematic Review" Tropical Medicine and Infectious Disease 8, no. 6: 300. https://doi.org/10.3390/tropicalmed8060300
APA StyleLinn, A. R., Dubois, M. M., & Steenhoff, A. P. (2023). Under-Reporting of Tuberculosis Disease among Children and Adolescents in Low and Middle-Income Countries: A Systematic Review. Tropical Medicine and Infectious Disease, 8(6), 300. https://doi.org/10.3390/tropicalmed8060300





