Anopheles funestus Populations across Africa Are Broadly Susceptible to Neonicotinoids but with Signals of Possible Cross-Resistance from the GSTe2 Gene
Abstract
1. Introduction
2. Materials and Methods
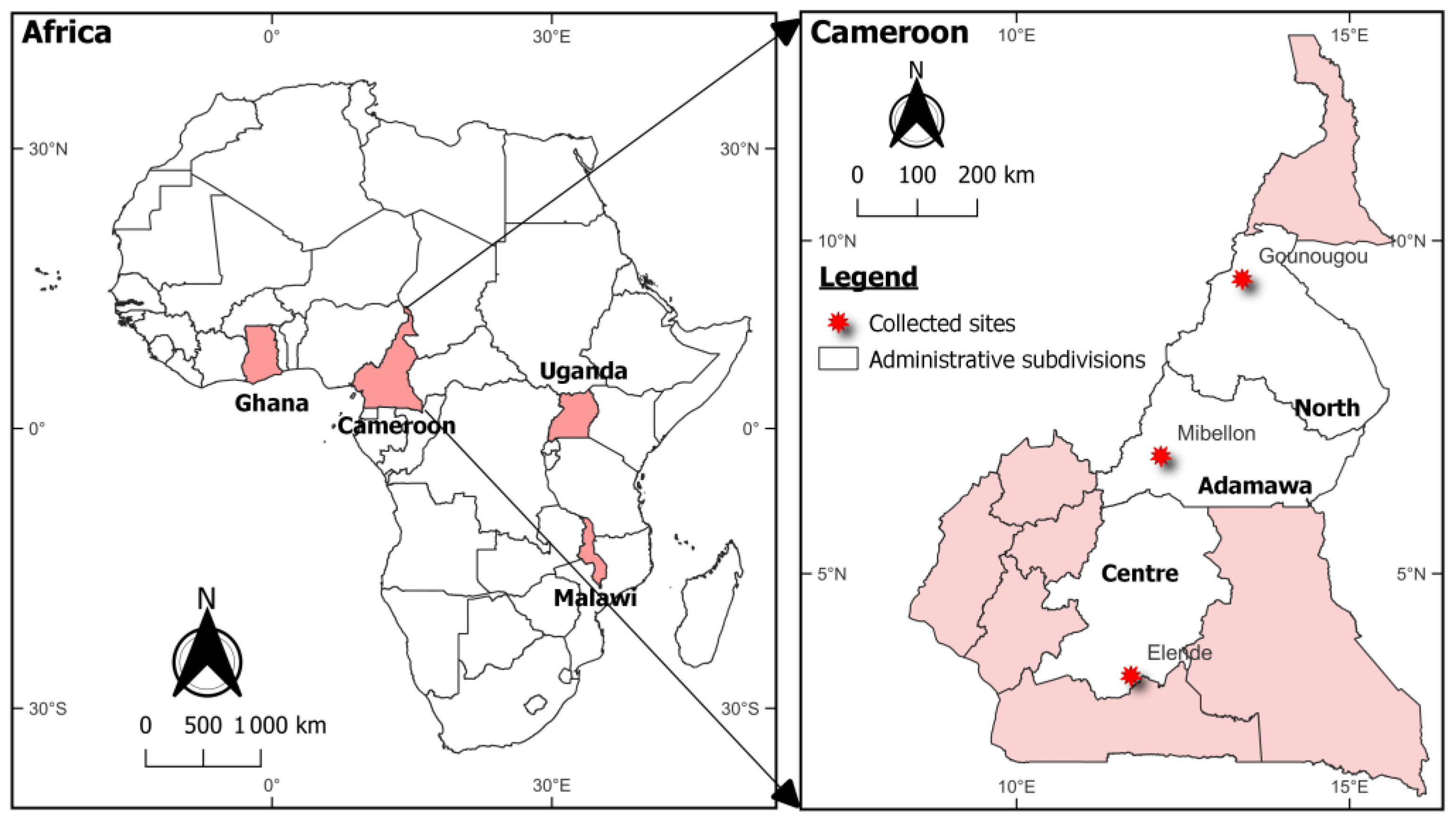
2.1. Study Sites and Mosquitoes Sampling
2.2. Molecular Identification of Species Collected
2.3. Determination of Susceptibility Profile to Neonicotinoids and Establishment of the Diagnostic Dose of Imidacloprid and Acetamiprid Diluted in Acetone + MERO
2.4. Synergist Assays
Potential Cross-Resistance between Neonicotinoids and Pyrethroids
3. Results
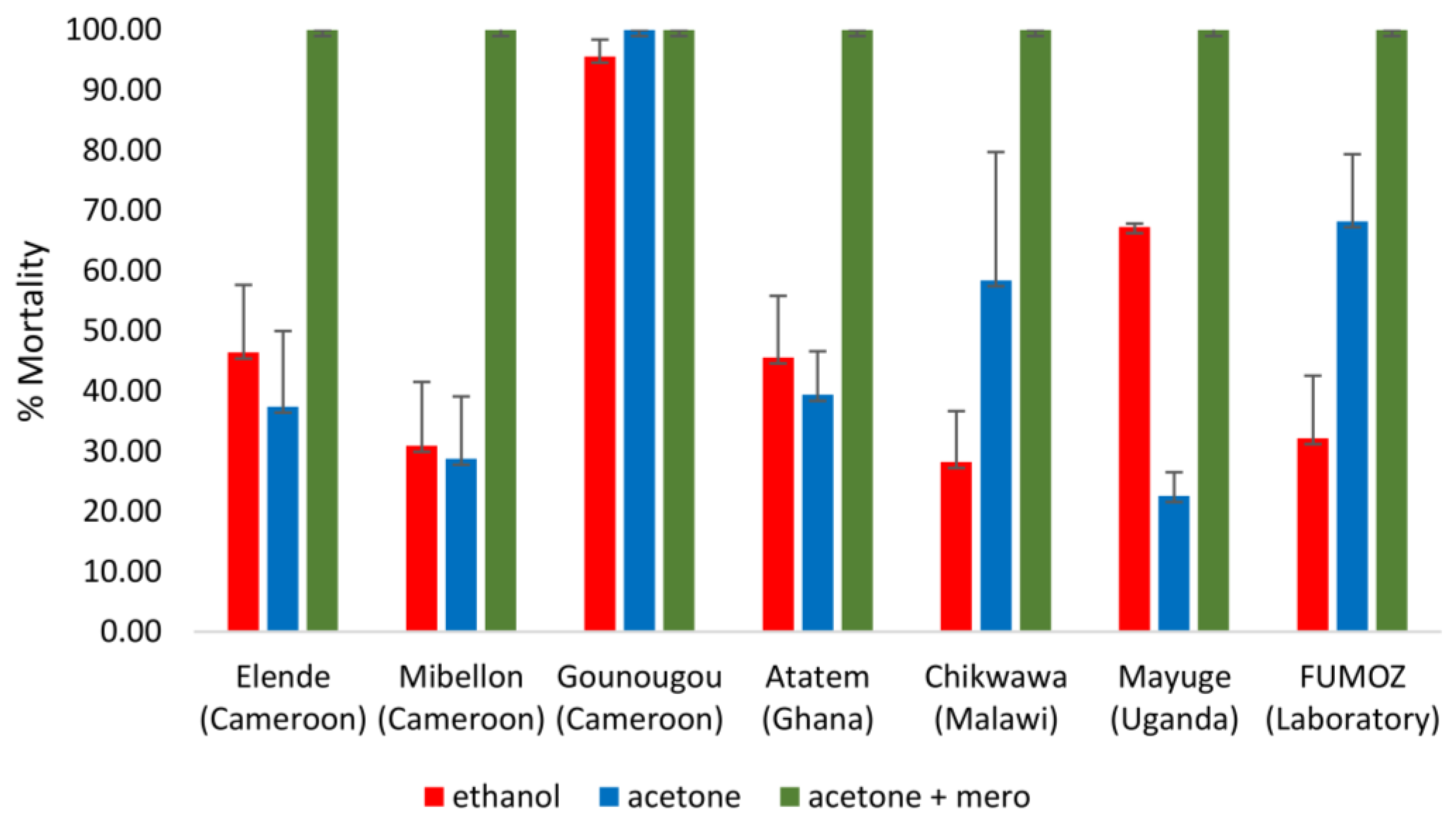
3.1. Susceptibility Profile of Mosquitoes to Clothianidin
3.2. Susceptibility Profile to Clothianidin with Synergists
3.3. Susceptibility Profile of Mosquitoes to Imidacloprid
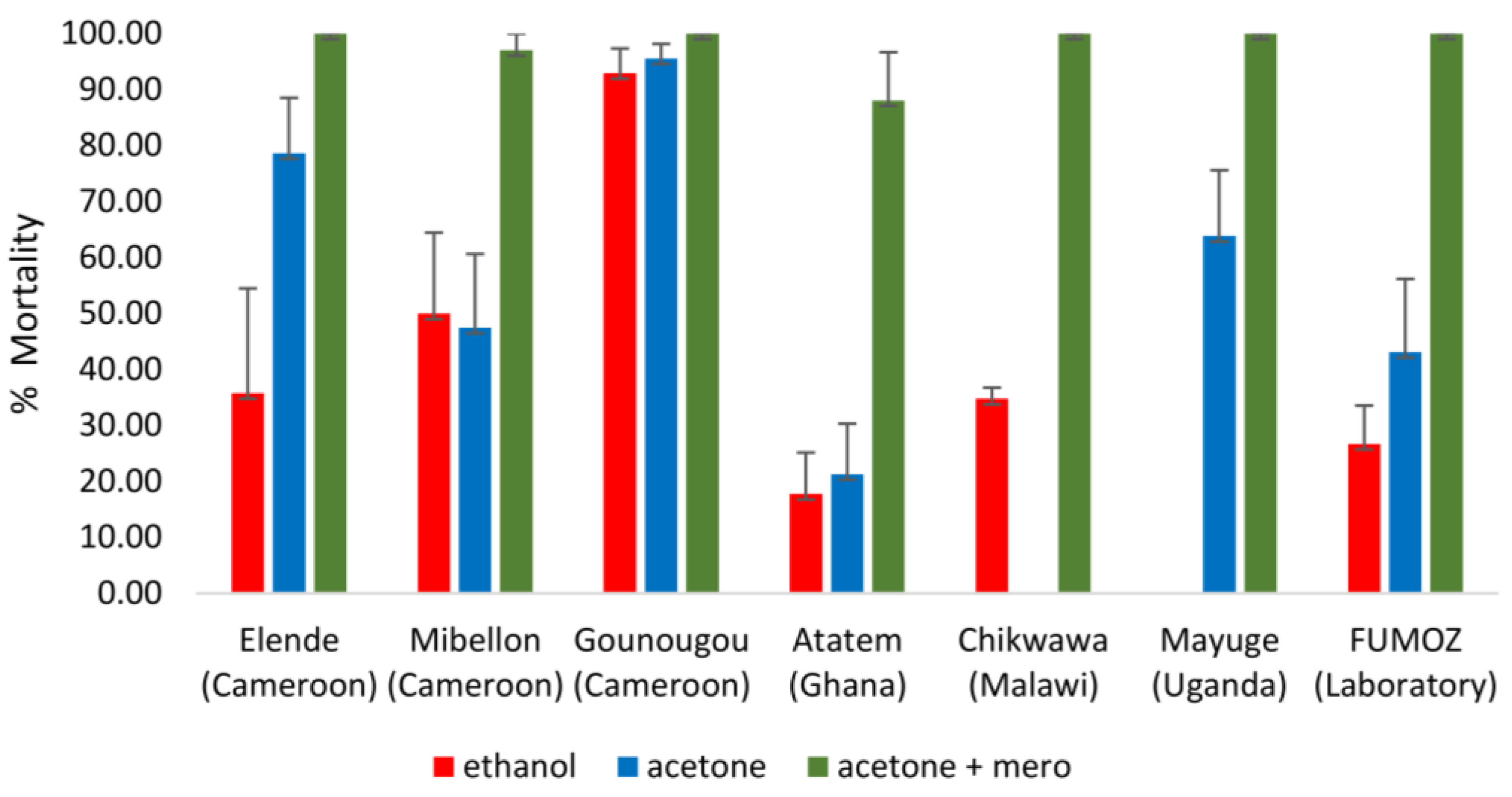
3.4. Susceptibility Profile of Mosquitoes to Acetamiprid
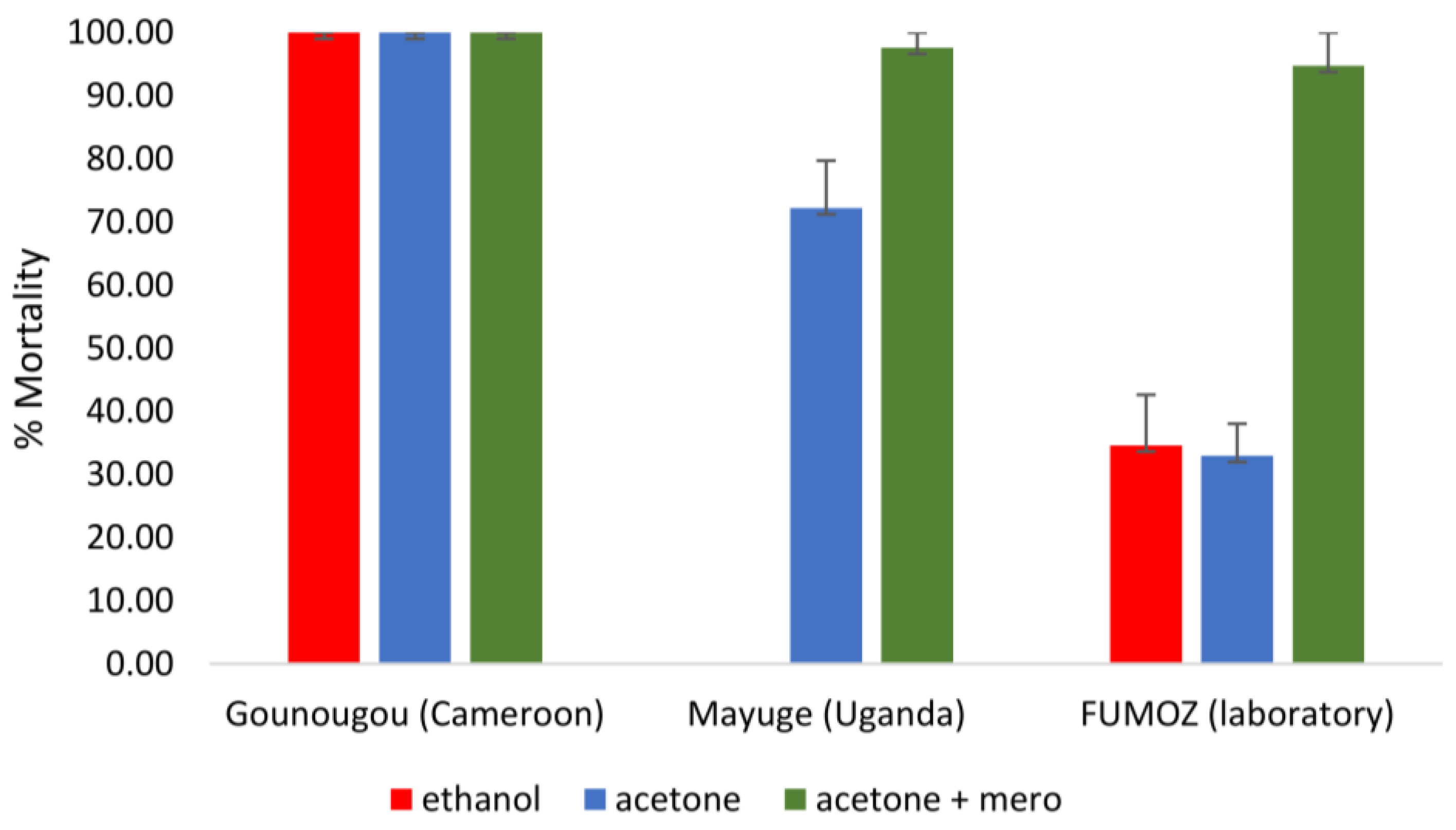
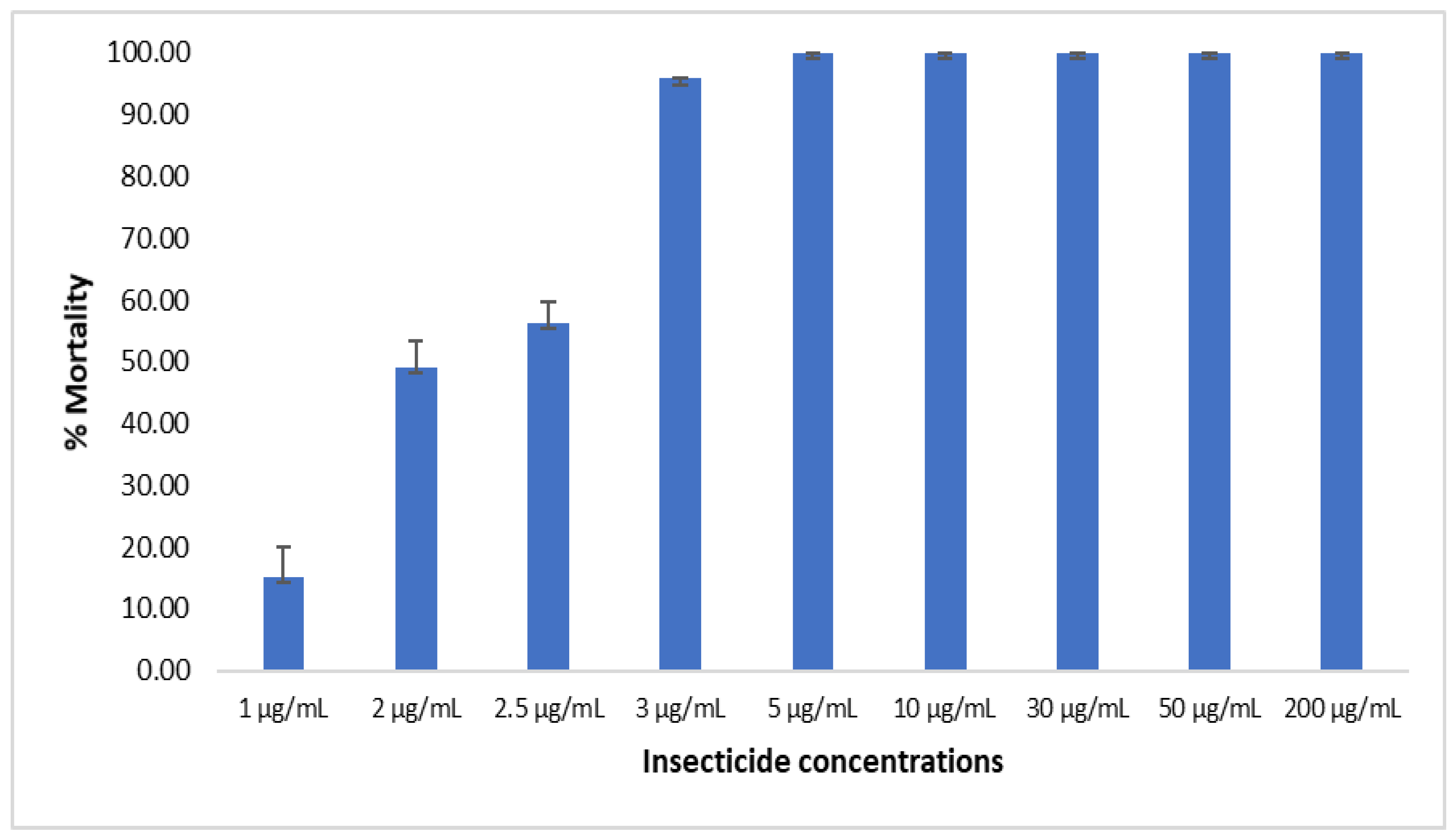
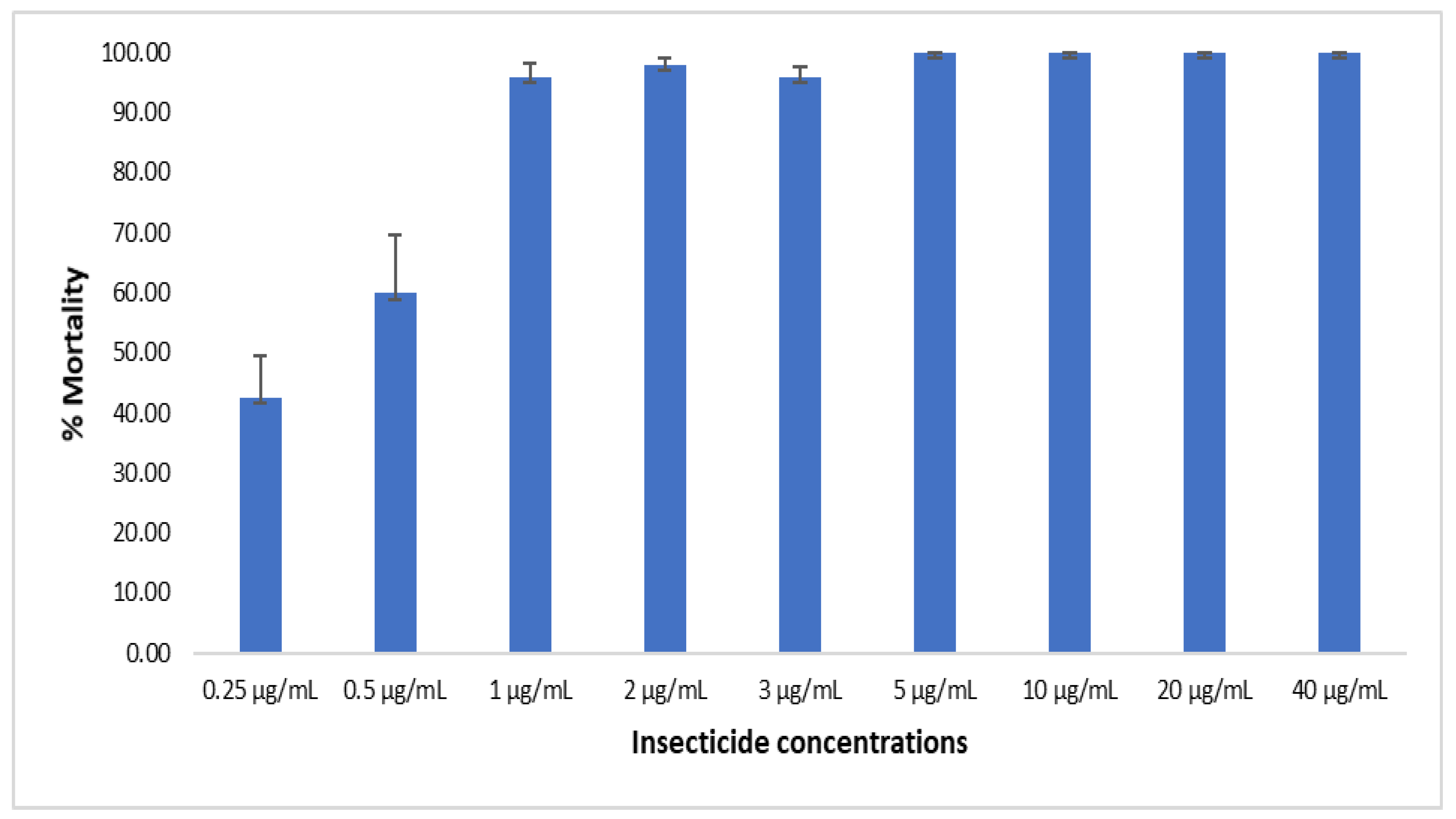
3.5. Establishment of Diagnostic Dose of Imidacloprid and Acetamiprid Using Acetone and Mero as Solvent
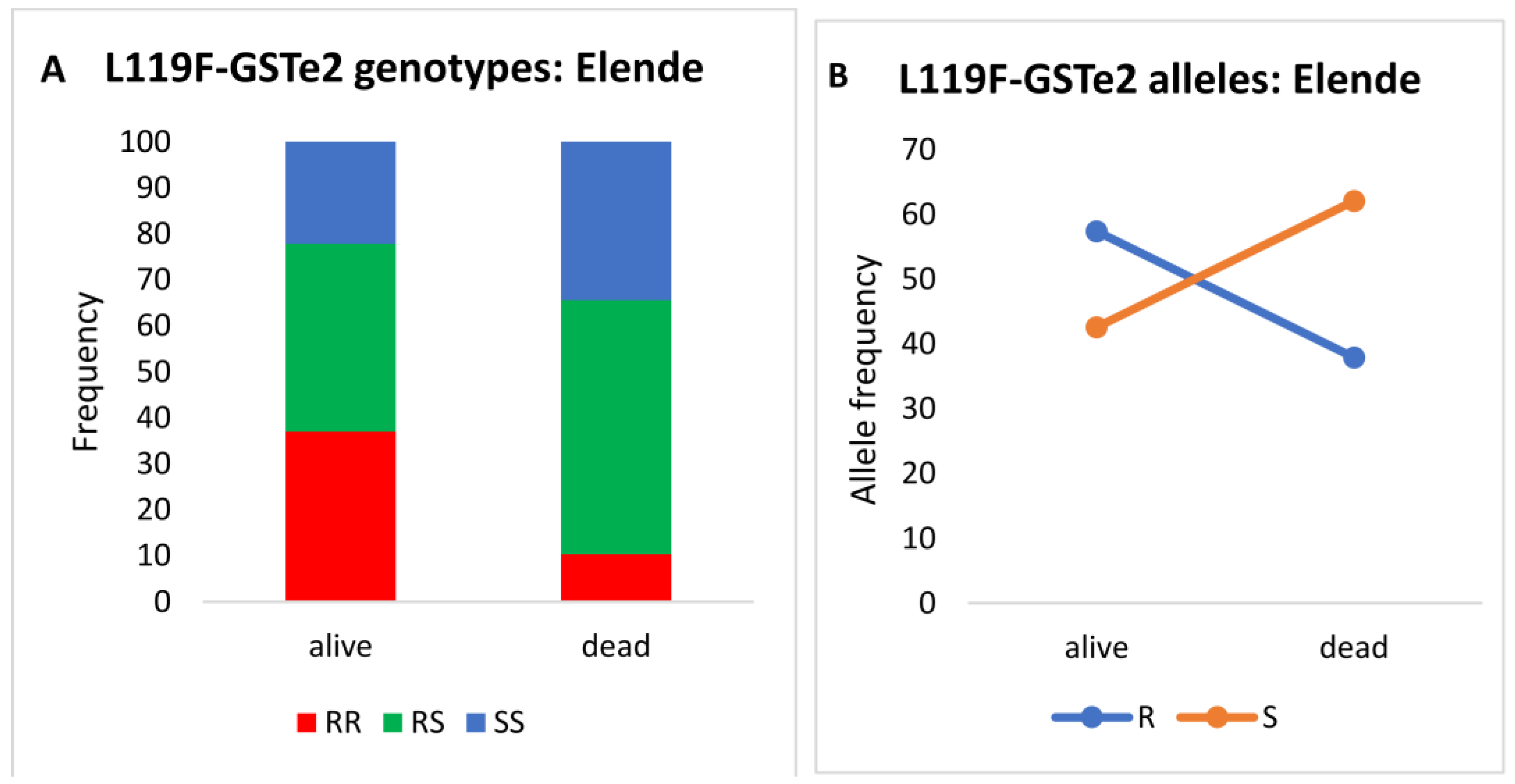
3.6. Assessing Possible Cross-Resistance between Clothianidin and Pyrethroids Using Genotyping of Resistance Markers
4. Discussion
4.1. Contrasting Susceptibility Profiles from the Three Solvents
4.2. Synergist Assays Revealed That Metabolic Enzymes Are Associated with Reduced Susceptibility to Clothianidin in An. funestus
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. World Malaria Report 2022; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Riveron, J.M.; Tchouakui, M.; Mugenzi, L.; Menze, B.D.; Chiang, M.-C.; Wondji, C.S. Insecticide Resistance in malaria vectors: An update at a global scale. In Towards Malaria Elimination-a Leap Forward; IntechOpen: London, UK, 2018. [Google Scholar]
- Hemingway, J.; Beaty, B.J.; Rowland, M.; Scott, T.W.; Sharp, B.L. The Innovative Vector Control Consortium: Improved control of mosquito-borne diseases. Trends Parasitol. 2006, 22, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Denholm, I.; Rowland, M. Tactics for managing pesticide resistance in arthropods: Theory and practice. Annu. Rev. Entomol. 1992, 37, 91–112. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Plan for Insecticide Resistance Management in Malaria Vectors; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Darriet, F.; Robert, V.; Vien, N.T.; Carnevale, P. Evaluation of the Efficacy of Permethrin Impregnated Intact and Perforated Mosquito Nets Against Vectors of Malaria; World Health Organization: Geneva, Switzerland, 1984. [Google Scholar]
- Tseng, L.F.; Chang, W.C.; Ferreira, M.C.; Wu, C.H.; Rampão, H.S.; Lien, J.C. Rapid control of malaria by means of indoor residual spraying of alphacypermethrin in the Democratic Republic of Sao Tome and Principe. Am. J. Trop. Med. Hyg. 2008, 78, 248–250. [Google Scholar] [CrossRef]
- Jeschke, P.; Nauen, R.; Schindler, M.; Elbert, A. Overview of the status and global strategy for neonicotinoids. J. Agric. Food Chem. 2011, 59, 2897–2908. [Google Scholar] [CrossRef] [PubMed]
- Elamathi, N.; Vaishali, V.; Sharma, V.P.; Sreehari, U.; Raghavendra, K. Neonicotinoids in vector control: In silico approach. Asian J. Biomed. Pharm. Sci. 2014, 4, 25–29. [Google Scholar]
- Tomizawa, M.; Casida, J.E. Neonicotinoid insecticide toxicology: Mechanisms of selective action. Annu. Rev. Pharmacol. Toxicol. 2005, 45, 247–268. [Google Scholar] [CrossRef]
- Shah, R.M.; Alam, M.; Ahmad, D.; Waqas, M.; Ali, Q.; Binyamin, M.; Shad, S.A. Toxicity of 25 synthetic insecticides to the field population of Culex quinquefasciatus Say. Parasitol. Res. 2016, 115, 4345–4351. [Google Scholar] [CrossRef]
- Darriet, F.; Chandre, F. Efficacy of six neonicotinoid insecticides alone and in combination with deltamethrin and piperonyl butoxide against pyrethroid-resistant Aedes aegypti and Anopheles gambiae (Diptera: Culicidae). Pest Manag. Sci. 2013, 69, 905–910. [Google Scholar] [CrossRef]
- Tchouakui, M.; Assatse, T.; Mugenzi, L.M.J.; Menze, B.D.; Nguiffo-Nguete, D.; Tchapga, W.; Kayondo, J.; Watsenga, F.; Manzambi, E.Z.; Osae, M.; et al. Comparative study of the effect of solvents on the efficacy of neonicotinoid insecticides against malaria vector populations across Africa. Infect. Dis. Poverty 2022, 11, 23–31. [Google Scholar] [CrossRef]
- Morgan, J.C.; Irving, H.; Okedi, L.M.; Steven, A.; Wondji, C.S. Pyrethroid resistance in an Anopheles funestus population from Uganda. PLoS ONE 2010, 5, e11872. [Google Scholar] [CrossRef]
- Gillies, M.T.; De Meillon, B. The Anophelinae of Africa South of the Sahara (Ethiopian Zoogeographical Region); South African Institute for Medical Research: Johannesburg, South Africa, 1968; p. 343. [Google Scholar]
- Livak, K.J. Organization and mapping of a sequence on the Drosophila melanogaster X and Y chromosomes that is transcribed during spermatogenesis. Genetics 1984, 107, 611–634. [Google Scholar] [CrossRef] [PubMed]
- Koekemoer, L.L.; Kamau, L.; Hunt, R.H.; Coetzee, M. A cocktail polymerase chain reaction assay to identify members of the Anopheles funestus (Diptera: Culicidae) grou. Am. J. Trop. Med. Hyg. 2002, 66, 804–811. [Google Scholar] [CrossRef] [PubMed]
- Fongnikin, A.; Houeto, N.; Agbevo, A.; Odjo, A.; Syme, T.; N’guessan, R.; Ngufor, C. Efficacy of Fludora® Fusion (a mixture of deltamethrin and clothianidin) for indoor residual spraying against pyrethroid-resistant malaria vectors: Laboratory and experimental hut evaluation. Parasites Vectors 2020, 13, 466. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Standard Operating Procedure for Testing Insecticide Susceptibility of Adult Mosquitoes in WHO Bottle Bioassays; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Tchouakui, M.; Riveron, J.M.; Djonabaye, D.; Tchapga, W.; Irving, H.; Takam, P.S.; Njiokou, F.; Wondji, C.S. Fitness costs of the glutathione S-transferase epsilon 2 (L119F-GSTe2) mediated metabolic resistance to insecticides in the major African malaria vector Anopheles funestus. Genes 2018, 9, 645. [Google Scholar] [CrossRef]
- Tchouakui, M.; Chiang, M.-C.; Ndo, C.; Kuicheu, C.K.; Amvongo-Adjia, N.; Wondji, M.J.; Tchoupo, M.; Kusimo, M.O.; Riveron, J.M.; Wondji, C.S. A marker of glutathione S-transferase-mediated resistance to insecticides is associated with higher Plasmodium infection in the African malaria vector Anopheles funestus. Sci. Rep. 2019, 9, 5772. [Google Scholar] [CrossRef]
- Ngufor, C.; Fongnikin, A.; Rowland, M.; N’guessan, R. Indoor residual spraying with a mixture of clothianidin (a neonicotinoid insecticide) and deltamethrin provides improved control and long residual activity against pyrethroid resistant Anopheles gambiae sl in Southern Benin. PLoS ONE 2017, 12, e0189575. [Google Scholar] [CrossRef]
- Romero, A.; Anderson, T.D. High levels of resistance in the common bed bug, Cimex lectularius (Hemiptera: Cimicidae), to neonicotinoid insecticides. J. Med. Entomol. 2016, 53, 727–731. [Google Scholar] [CrossRef]
- Dáder, B.; Viñuela, E.; Moreno, A.; Plaza, M.; Garzo, E.; del Estal, P.; Fereres, A. Sulfoxaflor and natural Pyrethrin with Piperonyl Butoxide are effective alternatives to Neonicotinoids against juveniles of Philaenus spumarius, the european vector of Xylella fastidiosa. Insects 2019, 10, 225. [Google Scholar] [CrossRef]
- Mazíková, V.; Sroková, I.; Ebringerová, A. Solvent-free synthesis and properties of carboxymethyl starch fatty acid ester derivatives. Chem. Pap. 2009, 63, 71–76. [Google Scholar] [CrossRef]
- Lees, R.; Praulins, G.; Davies, R.; Brown, F.; Parsons, G.; White, A.; Ranson, H.; Small, G.; Malone, D. A testing cascade to identify repurposed insecticides for next-generation vector control tools: Screening a panel of chemistries with novel modes of action against a malaria vector. Gates Open Res. 2019, 3, 1464. [Google Scholar] [CrossRef]
- World Health Organization. Manual for Monitoring Insecticide Resistance in Mosquito Vectors and Selecting Appropriate Interventions; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Mouhamadou, C.S.; De Souza, S.S.; Fodjo, B.K.; Zoh, M.G.; Bli, N.K.; Koudou, B.G. Evidence of insecticide resistance selection in wild Anopheles coluzzii mosquitoes due to agricultural pesticide use. Infect. Dis. Poverty 2019, 8, 64. [Google Scholar] [CrossRef]
- Jin, R.; Mao, K.; Liao, X.; Xu, P.; Li, Z.; Ali, E.; Wan, H.; Li, J. Overexpression of CYP6ER1 associated with clothianidin resistance in Nilaparvata lugens (Stål). Pestic. Biochem. Physiol. 2019, 154, 39–45. [Google Scholar] [CrossRef]
- Zhang, C.; Du, S.; Liu, R.; Dai, W. Overexpression of Multiple Cytochrome P450 Genes Conferring Clothianidin Resistance in Bradysia odoriphaga. J. Agric. Food Chem. 2022, 11, 7636–7643. [Google Scholar] [CrossRef] [PubMed]
- Zoh, M.G.; Bonneville, J.-M.; Tutagata, J.; Laporte, F.; Fodjo, B.K.; Mouhamadou, C.S.; Sadia, C.G.; McBeath, J.; Schmitt, F.; Horstmann, S.; et al. Experimental evolution supports the potential of neonicotinoid-pyrethroid combination for managing insecticide resistance in malaria vectors. Sci. Rep. 2021, 11, 19501. [Google Scholar] [CrossRef] [PubMed]
- Gong, P.; Chen, D.; Wang, C.; Li, M.; Li, X.; Zhang, Y.; Li, X.; Zhu, X. Susceptibility of four species of aphids in wheat to seven insecticides and its relationship to detoxifying enzymes. Front. Physiol. 2021, 11, 1852. [Google Scholar] [CrossRef] [PubMed]
- Puinean, A.M.; Foster, S.P.; Oliphant, L.; Denholm, I.; Field, L.M.; Millar, N.S.; Williamson, M.S.; Bass, C. Amplification of a cytochrome P450 gene is associated with resistance to neonicotinoid insecticides in the aphid Myzus persicae. PLoS Genet. 2010, 6, e1000999. [Google Scholar] [CrossRef] [PubMed]
- Londingkene, J.A.; Trisyono, Y.A.; Witjaksono; Martono, E. Resistance to imidacloprid and effect of three synergists on the resistance level of brown planthopper. In AIP Conference Proceedings; AIP Publishing LLC: Melville, NY, USA, 2016. [Google Scholar]
- Ma, Z.; Li, J.; Zhang, Y.; Shan, C.; Gao, X. Inheritance mode and mechanisms of resistance to imidacloprid in the house fly Musca domestica (Diptera: Muscidae) from China. PLoS ONE 2017, 12, e0189343. [Google Scholar] [CrossRef]

| Genotypes | L119F-GSTe2 and Clothianidin Resistance | |
|---|---|---|
| Odds-Ratio | p-Value | |
| RR vs. SS | 5.55 | p < 0.0001 ** |
| RR vs. RS | 4.84 | p < 0.0001 ** |
| RS vs. SS | 1.14 | p = 0.6891 |
| R vs. S | 2.2 | p = 0.0058 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Assatse, T.; Tchouakui, M.; Mugenzi, L.; Menze, B.; Nguiffo-Nguete, D.; Tchapga, W.; Kekeunou, S.; Wondji, C.S. Anopheles funestus Populations across Africa Are Broadly Susceptible to Neonicotinoids but with Signals of Possible Cross-Resistance from the GSTe2 Gene. Trop. Med. Infect. Dis. 2023, 8, 244. https://doi.org/10.3390/tropicalmed8050244
Assatse T, Tchouakui M, Mugenzi L, Menze B, Nguiffo-Nguete D, Tchapga W, Kekeunou S, Wondji CS. Anopheles funestus Populations across Africa Are Broadly Susceptible to Neonicotinoids but with Signals of Possible Cross-Resistance from the GSTe2 Gene. Tropical Medicine and Infectious Disease. 2023; 8(5):244. https://doi.org/10.3390/tropicalmed8050244
Chicago/Turabian StyleAssatse, Tatiane, Magellan Tchouakui, Leon Mugenzi, Benjamin Menze, Daniel Nguiffo-Nguete, Williams Tchapga, Sevilor Kekeunou, and Charles S. Wondji. 2023. "Anopheles funestus Populations across Africa Are Broadly Susceptible to Neonicotinoids but with Signals of Possible Cross-Resistance from the GSTe2 Gene" Tropical Medicine and Infectious Disease 8, no. 5: 244. https://doi.org/10.3390/tropicalmed8050244
APA StyleAssatse, T., Tchouakui, M., Mugenzi, L., Menze, B., Nguiffo-Nguete, D., Tchapga, W., Kekeunou, S., & Wondji, C. S. (2023). Anopheles funestus Populations across Africa Are Broadly Susceptible to Neonicotinoids but with Signals of Possible Cross-Resistance from the GSTe2 Gene. Tropical Medicine and Infectious Disease, 8(5), 244. https://doi.org/10.3390/tropicalmed8050244







