Asymptomatic and Mild SARS-CoV-2 Infections in a Hungarian Outpatient Cohort in the First Year of the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Collection of Blood and Nasopharyngeal Swab Samples
2.2. Questionnaire
2.3. SARS-CoV-2 RT-PCR
2.4. SARS-CoV-2 Culture, Inactivation, and Purification
2.5. Anti-SARS-CoV-2 IgG and IgA Antibody Testing
2.6. Data Analysis
3. Results
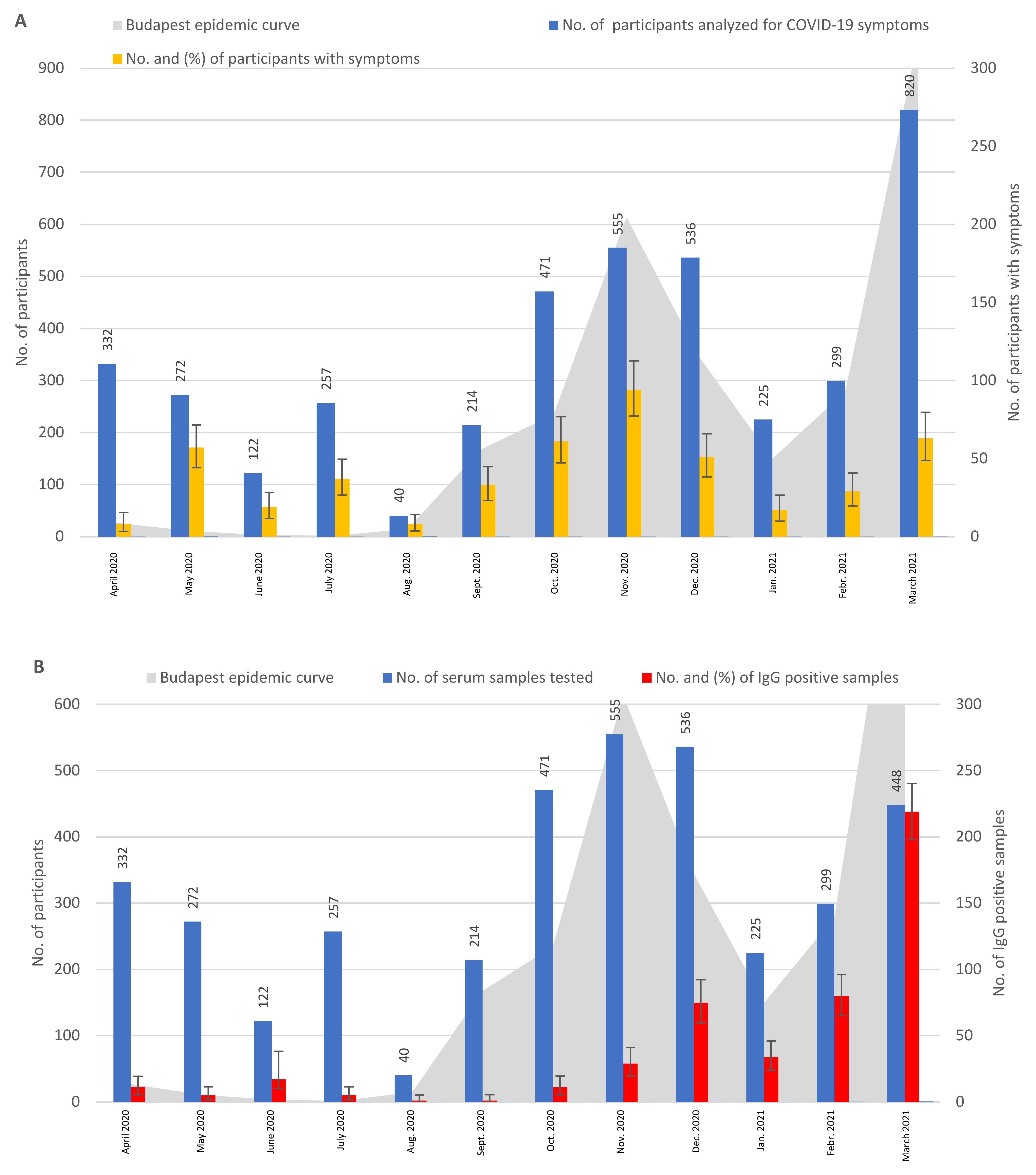
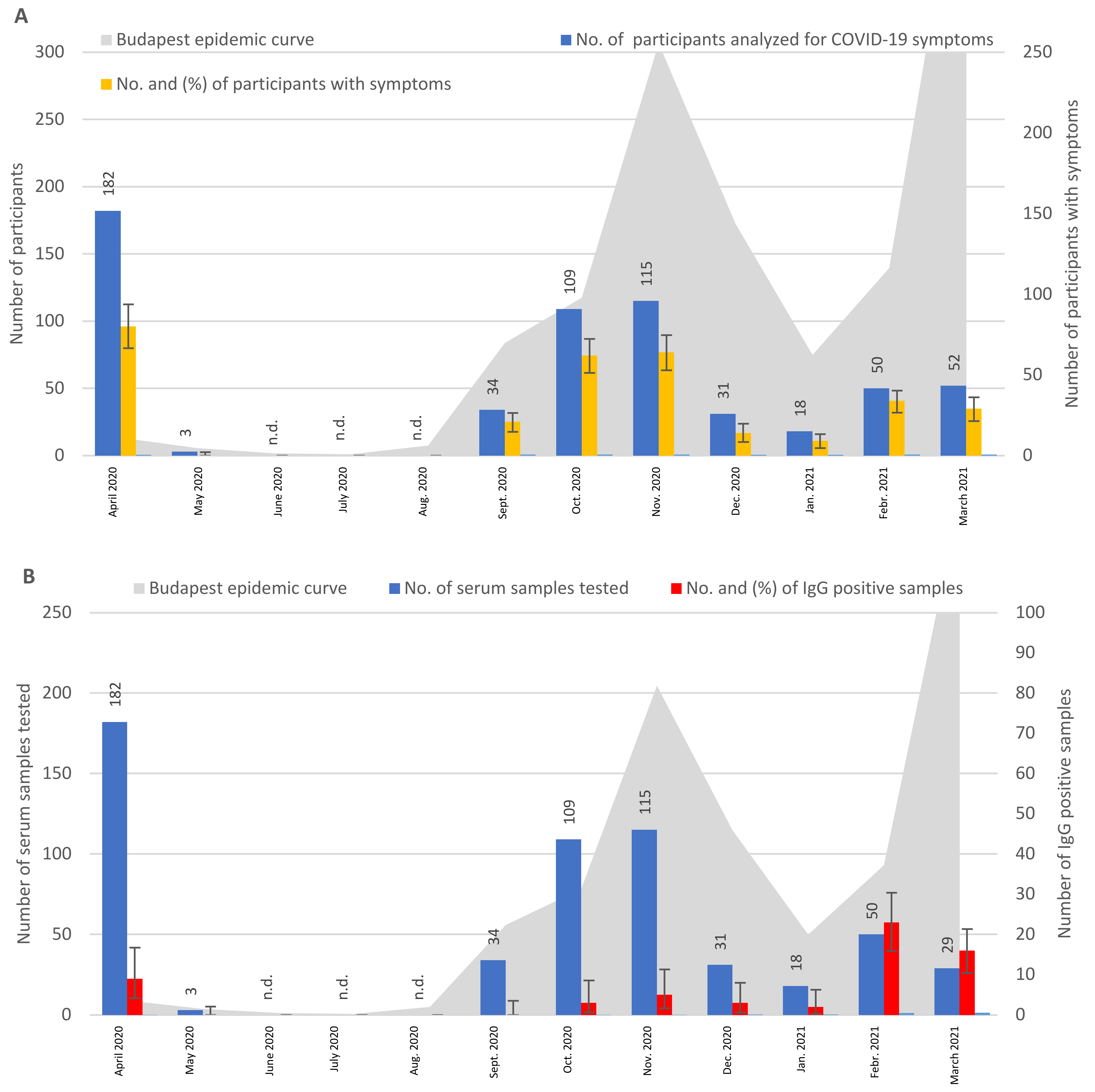
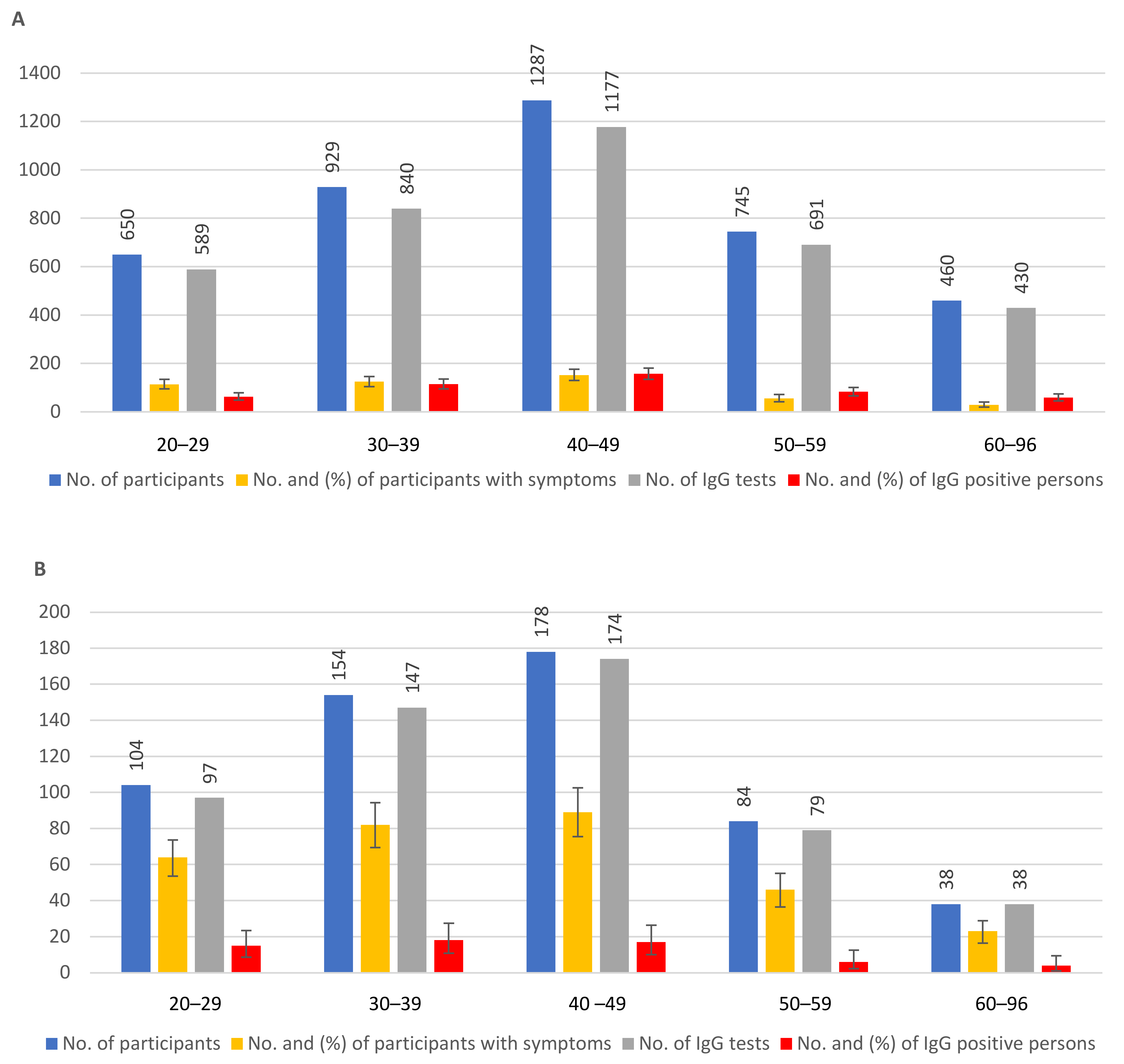
3.1. Clinical Symptoms, Seroprevalence, and RT-PCR Positivity of Participants without Known COVID-19 Contacts
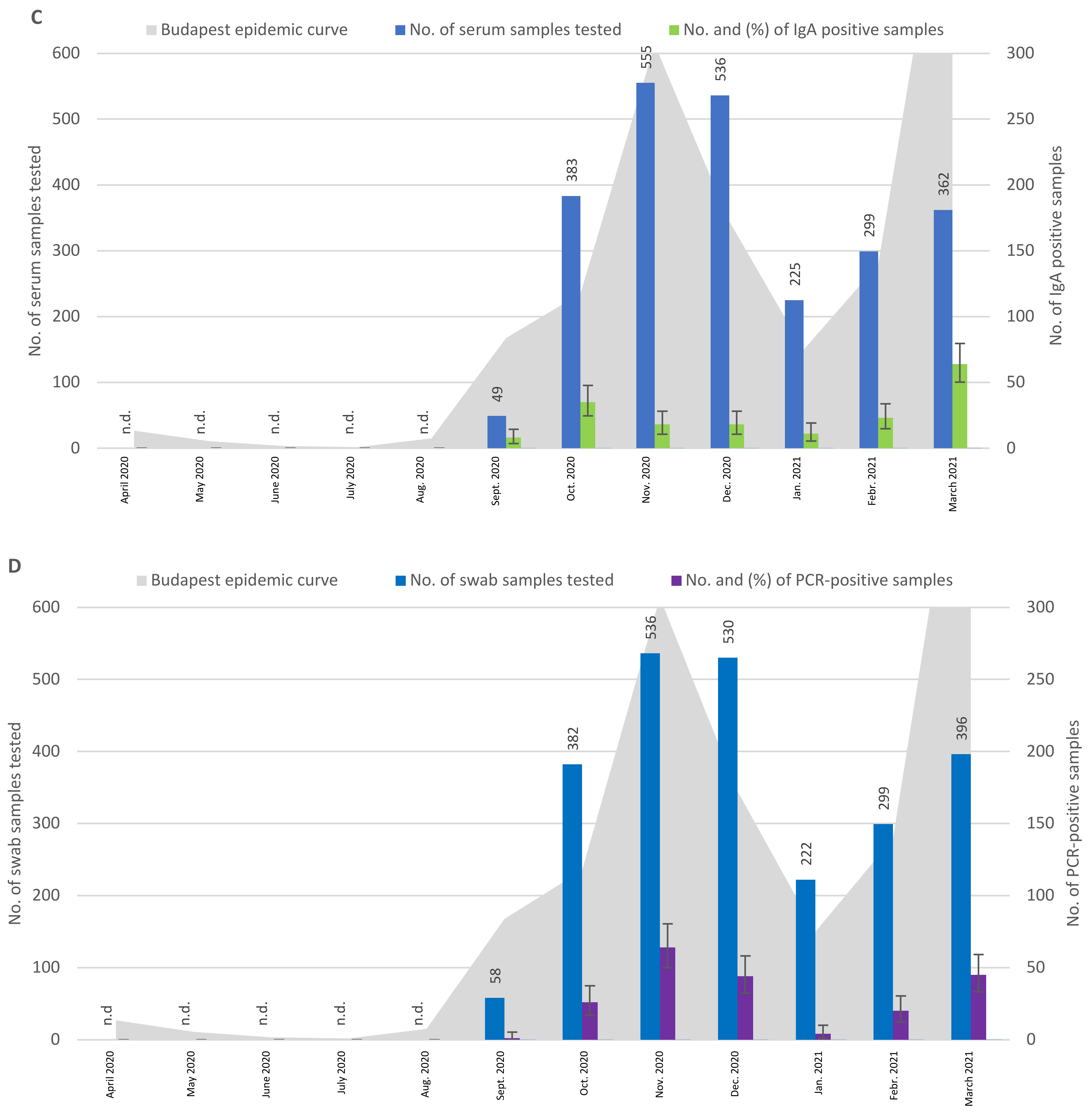
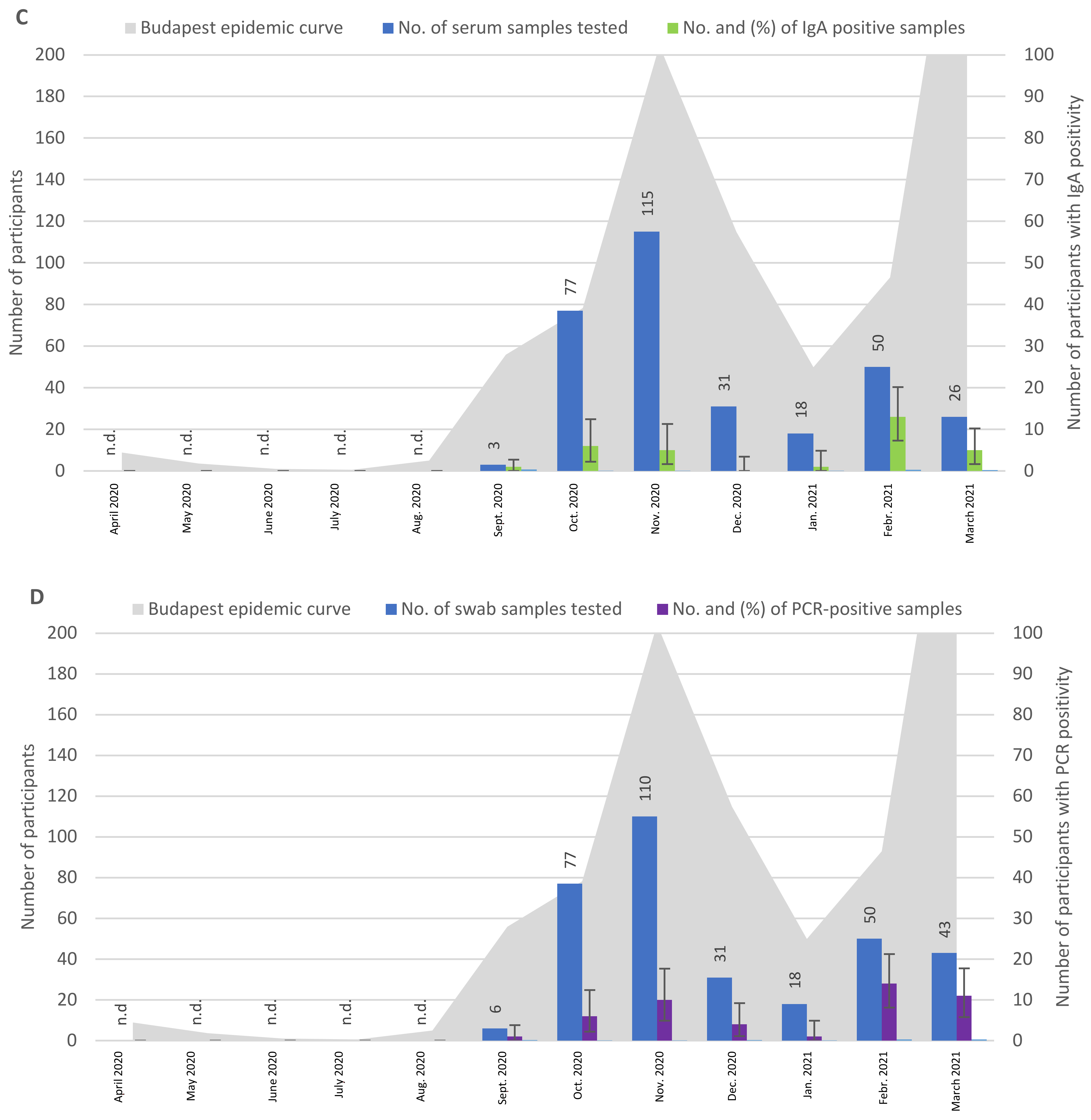
3.2. Symptoms, Seroprevalence, and RT-PCR Positivity of Participants with Known COVID-19 Contacts
3.3. The Relation of IgG and IgA Antibodies in the Participants with or without Previous COVID-19 Contacts
3.4. Coexisting Diseases and COVID-19 Symptoms, in Context with PCR Positivity, in Participants with or without Previous COVID-19 Contacts
3.5. Direct Comparison of PCR Positivity and Symptoms in Participants with or without Previous COVID-19 Contacts
3.6. Repeated Sampling and Testing of 33 Selected Participants: IgG Positivity, PCR Positivity, and Symptoms
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Statement on the Second Meeting of the International Health Regulations. Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-NCoV). 2005. Available online: https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) (accessed on 16 December 2021).
- Word Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19. 11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020 (accessed on 16 December 2021).
- Szalai, B.; Hercegh, É.; Magyar, N.; Déri, D.; Rózsa, M.; Molnár, Z.; Kuti, D.; Kis, Z.; Szomor, K.; Takács, M.; et al. Detection of the First Appearance of SARS-CoV-2 Virus in Hungary Based on Retrospective Testing of Respiratory Samples. Orv. Hetil. 2020, 161, 1619–1622. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Morales, A.J.; Cardona-Ospina, J.A.; Gutiérrez-Ocampo, E.; Villamizar-Peña, R.; Holguin-Rivera, Y.; Escalera-Antezana, J.P.; Alvarado-Arnez, L.E.; Bonilla-Aldana, D.K.; Franco-Paredes, C.; Henao-Martinez, A.F.; et al. Clinical, Laboratory and Imaging Features of COVID-19: A Systematic Review and Meta-Analysis. Travel Med. Infect. Dis. 2020, 34, 101623. [Google Scholar] [CrossRef]
- Huang, A.T.; Garcia-Carreras, B.; Hitchings, M.D.T.; Yang, B.; Katzelnick, L.C.; Rattigan, S.M.; Borgert, B.A.; Moreno, C.A.; Solomon, B.D.; Trimmer-Smith, L.; et al. A Systematic Review of Antibody Mediated Immunity to Coronaviruses: Kinetics, Correlates of Protection, and Association with Severity. Nat. Commun. 2020, 11, 4704. [Google Scholar] [CrossRef]
- Chen, X.; Chen, Z.; Azman, A.S.; Deng, X.; Sun, R.; Zhao, Z.; Zheng, N.; Chen, X.; Lu, W.; Zhuang, T.; et al. Serological Evidence of Human Infection with SARS-CoV-2: A Systematic Review and Meta-Analysis. Lancet Glob. Health 2021, 9, e598–e609. [Google Scholar] [CrossRef]
- Rostami, A.; Sepidarkish, M.; Leeflang, M.M.G.; Riahi, S.M.; Nourollahpour Shiadeh, M.; Esfandyari, S.; Mokdad, A.H.; Hotez, P.J.; Gasser, R.B. SARS-CoV-2 Seroprevalence Worldwide: A Systematic Review and Meta-Analysis. Clin. Microbiol. Infect. 2021, 27, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Azami, M.; Moradi, Y.; Moradkhani, A.; Aghaei, A. SARS-CoV-2 seroprevalence around the world: An updated systematic review and meta-analysis. Eur. J. Med. Res. 2022, 27, 81. [Google Scholar] [CrossRef]
- Emmenegger, M.; De Cecco, E.; Lamparter, D.; Jacquat, R.P.B.; Riou, J.; Menges, D.; Ballouz, T.; Ebner, D.; Schneider, M.M.; Morales, I.C.; et al. Continuous population-level monitoring of SARS-CoV-2 seroprevalence in a large European metropolitan region. iScience 2023, 26, 05928. [Google Scholar] [CrossRef]
- Ma, Y.; Deng, J.; Liu, Q.; Du, M.; Liu, M.; Liu, J. Long-Term Consequences of Asymptomatic SARS-CoV-2 Infection: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public. Health 2023, 20, 1613. [Google Scholar] [CrossRef] [PubMed]
- Nagy, É.; Golopencza, P.; Barcs, I.; Ludwig, E. Comparison of COVID-19 Severity and Mortality Rates in the First Four Epidemic Waves in Hungary in a Single-Center Study with Special Regard to Critically Ill Patients in an Intensive Care Unit. Trop. Med. Infect. Dis. 2023, 8, 153. [Google Scholar] [CrossRef] [PubMed]
- Long, Q.X.; Liu, B.Z.; Deng, H.J.; Wu, G.C.; Deng, K.; Chen, Y.K.; Liao, P.; Qiu, J.F.; Lin, Y.; Cai, X.F.; et al. Antibody Responses to SARS-CoV-2 in Patients with COVID-19. Nat. Med. 2020, 26, 845–848. [Google Scholar] [CrossRef]
- Kim, G.U.; Kim, M.J.; Ra, S.H.; Lee, J.; Bae, S.; Jung, J.; Kim, S.H. Clinical Characteristics of Asymptomatic and Symptomatic Patients with Mild COVID-19. Clin. Microbiol. Infect. 2020, 26, 948.e1–948.e3. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Su, Y.Y.; Zhi, S.S.; Huang, J.; Zhuang, C.L.; Bai, W.Z.; Wan, Y.; Meng, X.R.; Zhang, L.; Zhou, Y.B.; et al. Virus Shedding Dynamics in Asymptomatic and Mildly Symptomatic Patients Infected with SARS-CoV-2. Clin. Microbiol. Infect. 2020, 26, 1556.e1–1556.e6. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Jin, C.; Zhang, L.; Kong, D.; Hu, K.; Xuan, M.; Liu, Q.; Li, S.; Zhang, K.; Xue, Y. Clinical characteristics and risk factors analysis of viral shedding time in mildly symptomatic and asymptomatic patients with SARS-CoV-2 Omicron variant infection in Shanghai. Front. Public. Health 2023, 10, 1073387. [Google Scholar] [CrossRef] [PubMed]
- Gao, W.; Lv, J.; Pang, Y.; Li, L.M. Role of asymptomatic and pre-symptomatic infections in covid-19 pandemic. BMJ 2021, 375, n2342. [Google Scholar] [CrossRef]
- World Health Organization. Unity Studies: Early Investigation Protocols. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/early-investigations (accessed on 16 December 2021).
- World Health Organization. Living Guidance for Clinical Management of COVID-19. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2 (accessed on 12 January 2022).
- World Health Organization. Population-Based Age-Stratified Seroepidemiological Investigation Protocol for COVID-19 Virus Infection. Available online: https://apps.who.int/iris/handle/10665/331656 (accessed on 17 March 2020).
- Baer, A.; Kehn-Hall, K. Viral concentration determination through plaque assays: Using traditional and novel overlay systems. J. Vis. Exp. 2014, 93, e52065. [Google Scholar] [CrossRef]
- Rockstroh, A.; Wolf, J.; Fertey, J.; Kalbitz, S.; Schroth, S.; Lübbert, C.; Ulbert, S.; Borte, S. Correlation of Humoral Immune Responses to Different SARS-CoV-2 Antigens with Virus Neutralizing Antibodies and Symptomatic Severity in a German COVID-19 Cohort. Emerg. Microbes. Infect. 2021, 10, 774–781. [Google Scholar] [CrossRef]
- Ma, H.; Zeng, W.; He, H.; Zhao, D.; Jiang, D.; Zhou, P.; Cheng, L.; Li, Y.; Ma, X.; Jin, T. Serum IgA, IgM, and IgG Responses in COVID-19. Cell. Mol. Immunol. 2020, 17, 773–775. [Google Scholar] [CrossRef]
- Zervou, F.N.; Louie, P.; Stachel, A.; Zacharioudakis, I.M.; Ortiz-Mendez, Y.; Thomas, K.; Aguero-Rosenfeld, M.E. SARS-CoV-2 Antibodies: IgA Correlates with Severity of Disease in Early COVID-19 Infection. J. Med. Virol. 2021, 93, 5409–5415. [Google Scholar] [CrossRef]
- Oroszi, B.; Horváth, J.K.; Túri, G.; Krisztalovics, K.; Röst, G. The Role of Epidemiological Surveillance and Mathematical Forecasting in Preventing and Mitigating Pandemic Waves—What Has Been Accomplished and What Should Be Achieved. Sci. Secur. 2021, 2, 38–53. (In Hungarian) [Google Scholar] [CrossRef]
- Röst, G.; Bartha, F.A.; Bogya, N.; Boldog, P.; Dénes, A.; Ferenci, T.; Horváth, K.J.; Juhász, A.; Nagy, C.; Tekeli, T.; et al. Early Phase of the COVID-19 Outbreak in Hungary and Post-Lockdown Scenarios. Viruses 2020, 12, 708. [Google Scholar] [CrossRef]
- Uzzoli, A.; Kovács, S.; Páger, B.; Szabó, T. Regional Inequalities in the Waves of the COVID-19 Pandemic in Hungary. Terul. Stat. 2021, 61, 291–319. [Google Scholar] [CrossRef]
- Koronavírus. Available online: https://koronavirus.gov.hu/ (accessed on 16 December 2021).
- Ye, Q.; Zhang, T.; Lu, D. Potential false-positive reasons for SARS-CoV-2 antibody testing and its solution. J. Med. Virol. 2021, 93, 4242–4246. [Google Scholar] [CrossRef]
- World Health Organization. Final WHO SARS-CoV-2 Serology Test Kit Evaluation Results. Available online: hhttps://www.who.int/publications/m/item/final-who-sars-cov-2-serology-test-kit-evaluation-results (accessed on 21 July 2022).
- Amendola, A.; Bianchi, S.; Gori, M.; Colzani, D.; Canuti, M.; Borghi, E.; Raviglione, M.C.; Zuccotti, G.V.; Tanzi, E. Evidence of SARS-CoV-2 RNA in an Oropharyngeal Swab Specimen, Milan, Italy, Early December 2019. Emerg. Infect. Dis. 2021, 27, 648–650. [Google Scholar] [CrossRef]
- La Rosa, G.; Mancini, P.; Bonanno Ferraro, G.; Veneri, C.; Iaconelli, M.; Bonadonna, L.; Lucentini, L.; Suffredini, E. SARS-CoV-2 Has Been Circulating in Northern Italy since December 2019: Evidence from Environmental Monitoring. Sci. Total. Environ. 2021, 750, 141711. [Google Scholar] [CrossRef] [PubMed]
- Trombetta, C.M.; Marchi, S.; Viviani, S.; Manenti, A.; Casa, E.; Dapporto, F.; Remarque, E.J.; Bollati, V.; Manini, I.; Lazzeri, G.; et al. A serological investigation in Southern Italy: Was SARS-CoV-2 circulating in late 2019? Hum. Vaccin. Immunother. 2022, 18, 2047582. [Google Scholar] [CrossRef] [PubMed]
- Merkely, B.; Szabó, A.J.; Kosztin, A.; Berényi, E.; Sebestyén, A.; Lengyel, C.; Merkely, G.; Karády, J.; Várkonyi, I.; Papp, C.; et al. Novel Coronavirus Epidemic in the Hungarian Population, a Cross-Sectional Nationwide Survey to Support the Exit Policy in Hungary. Geroscience 2020, 42, 1063–1074. [Google Scholar] [CrossRef]
- Omori, R.; Matsuyama, R.; Nakata, Y. The Age Distribution of Mortality from Novel Coronavirus Disease (COVID-19) Suggests No Large Difference of Susceptibility by Age. Sci. Rep. 2020, 10, 16642. [Google Scholar] [CrossRef]
- Axfors, C.; Pezzullo, A.M.; Contopoulos-Ioannidis, D.G.; Apostolatos, A.; Ioannidis, J.P. Differential COVID-19 infection rates in children, adults, and elderly: Systematic review and meta-analysis of 38 pre-vaccination national seroprevalence studies. J. Glob. Health 2023, 13, 06004. [Google Scholar] [CrossRef]
- Zsichla, L.; Müller, V. Risk Factors of Severe COVID-19: A Review of Host, Viral and Environmental Factors. Viruses 2023, 15, 175. [Google Scholar] [CrossRef]
- Rosenberg, E.S.; Dufort, E.M.; Blog, D.S.; Hall, E.W.; Hoefer, D.; Backenson, B.P.; Muse, A.T.; Kirkwood, J.N.; St George, K.; Holtgrave, D.R.; et al. COVID-19 Testing, Epidemic Features, Hospital Outcomes, and Household Prevalence, New York State—March 2020. Clin. Infect. Dis. 2020, 71, 1953–1959. [Google Scholar] [CrossRef]
- Boehmer, T.K.; DeVies, J.; Caruso, E.; van Santen, K.L.; Tang, S.; Black, C.L.; Hartnett, K.P.; Kite-Powell, A.; Dietz, S.; Lozier, M.; et al. Changing Age Distribution of the COVID-19 Pandemic—United States, May–August 2020. MMWR Morb. Mort. Wkl. Rep. 2020, 69, 1404–1409. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Rapid Risk Assessment: Coronavirus Disease 2019 (COVID-19) in the EU/EEA and the UK—Eleventh Update: Resurgence of Cases. Available online: https://www.ecdc.europa.eu/?url=https%3A%2F%2Fwww.ecdc.europa.eu%2Fen%2Fpublications-data%2Frapid-risk-assessment-coronavirus-disease-2019-covid-19-eueea-and-uk-eleventh (accessed on 10 August 2020).
- Wölfel, R.; Corman, V.M.; Guggemos, W.; Seilmaier, M.; Zange, S.; Müller, M.A.; Niemeyer, D.; Jones, T.C.; Vollmar, P.; Rothe, C.; et al. Virological Assessment of Hospitalized Patients with COVID-2019. Nature 2020, 581, 465–469, Erratum in Nature 2020, 588, E35. [Google Scholar] [CrossRef]
- Kellam, P.; Barclay, W. The Dynamics of Humoral Immune Responses Following SARS-CoV-2 Infection and the Potential for Reinfection. J. Gen. Vir. 2020, 101, 791–797. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Yan, L.M.; Wan, L.; Xiang, T.X.; Le, A.; Liu, J.M.; Peiris, M.; Poon, L.L.M.; Zhang, W. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect. Dis. 2020, 20, 656–657. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062, Erratum in Lancet 2020, 395, 1038. [Google Scholar] [CrossRef]
- Wellinghausen, N.; Plonné, D.; Voss, M.; Ivanova, R.; Frodl, R.; Deininger, S. SARS-CoV-2-IgG Response Is Different in COVID-19 Outpatients and Asymptomatic Contact Persons. J. Clin. Vir. 2020, 130, 104542. [Google Scholar] [CrossRef] [PubMed]
- Zhou, R.; Li, F.; Chen, F.; Liu, H.; Zheng, J.; Lei, C.; Wu, X. Viral Dynamics in Asymptomatic Patients with COVID-19. Int. J. Infect. Dis. 2020, 96, 288–290. [Google Scholar] [CrossRef]
- Arevalo-Rodriguez, I.; Buitrago-Garcia, D.; Simancas-Racines, D.; Zambrano-Achig, P.; del Campo, R.; Ciapponi, A.; Sued, O.; Martinez-García, L.; Rutjes, A.W.; Low, N.; et al. False-Negative Results of Initial RT-PCR Assays for COVID-19: A Systematic Review. PLoS ONE 2020, 15, e0242958. [Google Scholar] [CrossRef]
- Wikramaratna, P.S.; Paton, R.S.; Ghafari, M.; Lourenço, J. Estimating the false-negative test probability of SARS-CoV-2 by RT-PCR. Eurosurveillance 2020, 25, 2000568. [Google Scholar] [CrossRef]
- Wikramaratna, P.S.; Paton, R.S.; Ghafari, M.; Lourenço, J. Prolonged persistence of SARS-CoV-2 RNA in body fluids. Emerg. Infect. Dis. 2020, 26, 1834–1838. [Google Scholar]
- Meyerowitz, E.A.; Richterman, A.; Bogoch, I.I.; Low, N.; Cevik, M. Towards an Accurate and Systematic Characterisation of Persistently Asymptomatic Infection with SARS-CoV-2. Lancet Infect. Dis. 2021, 21, e163–e169. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zheng, K.; Gao, W.; Lv, J.; Yu, C.; Wang, L.; Wang, Z.; Wang, B.; Liao, C.; Li, L. Asymptomatic and pre-symptomatic infection in Coronavirus Disease 2019 pandemic. Med. Rev. 2022, 2, 66–88. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total No. of Tested People | Time Period | No. of People with Positive RT-PCR-Results | Percentage of Positive People (95% CI) |
|---|---|---|---|---|
| Symptoms | 1023 of 1023 | April 2020–August 2020 | 129 | 12.6 (10.64–14.80) |
| IgG antibodies | 1023 of 1023 | April 2020–August 2020 | 39 | 3.8 (2.72–5.17) |
| Symptoms | 3120 of 3120 | September 2020–March 2021 | 348 | 11.1 (10.07–12.31) |
| IgG antibodies | 2748 of 3120 | September 2020–March 2021 | 449 | 16.3 (14.98–17.78) |
| IgA antibodies | 2409 of 3120 | September 2020–March 2021 | 177 | 7.3 (6.34–8.46) |
| Viral RNA | 2423 of 3120 | September 2020–March 2021 | 204 | 8.4 (7.34–9.6) |
| Symptoms | 4143 of 4143 | April 2020–March 2021 | 477 | 11.5 (10.56–12.52) |
| IgG antibodies | 3771 of 4143 | April 2020–March 2021 | 488 | 12.9 (11.89–14.05) |
| Characteristics | Total No. of Tested People | Time Period | No. of People with Positive RT-PCR-Results | Percentage of Positive People (95% CI) |
|---|---|---|---|---|
| Symptoms | 185 of 185 | April 2020–May 2020 | 80 | 43.2 (35.99–50.71) |
| IgG antibodies | 185 of 185 | April 2020–May 2020 | 9 | 4.9 (2.25–9.03) |
| Symptoms | 409 of 409 | September 2020–March 2021 | 233 | 57.0 (52.01–61.82) |
| IgG antibodies | 386 of 409 | September 2020–March 2021 | 52 | 13.5 (10.23–17.29 |
| IgA antibodies | 320 of 409 | September 2020–March 2021 | 31 | 9.7 (6.68–13.47) |
| Viral RNA | 335 of 409 | September 2020–March 2021 | 47 | 14.0 (10.46–18.16) |
| Symptoms | 594 of 594 | April 2020–March 2021 | 313 | 52.6 (48.59–56.77) |
| IgG antibodies | 571 of 594 | April 2020–March 2021 | 61 | 10.6 (8.27–13.51) |
| Symptoms * | PCR-Positive Participants | % | PCR-Negative Participants | % | p-Value |
|---|---|---|---|---|---|
| n = 204 | n = 2219 | ||||
| cough | 40 | 19.6 | 68 | 3.1 | <0.001 |
| fatigue | 33 | 16.2 | 98 | 4.4 | <0.001 |
| headache | 33 | 16.2 | 125 | 5.6 | <0.001 |
| sore throat | 27 | 13.2 | 80 | 3.6 | <0.001 |
| rhinitis | 24 | 11.8 | 84 | 3.8 | <0.001 |
| chills | 21 | 10.3 | 32 | 1.4 | <0.001 |
| myalgia | 23 | 11.3 | 38 | 1.7 | <0.001 |
| anosmia | 15 | 7.4 | 19 | 0.9 | <0.001 |
| dysgeusia | 15 | 7.4 | 19 | 0.9 | <0.001 |
| fever | 14 | 6.9 | 19 | 0.9 | <0.001 |
| chest pain | 7 | 3.4 | 22 | 1.0 | 0.002 |
| gastrointestinal symptoms | 6 | 2.9 | 13 | 0.6 | <0.001 |
| shortness of breath | 3 | 1.5 | 13 | 0.6 | 0.135 |
| Symptoms * | PCR-Positive Participants | PCR-Negative Participants | |||
|---|---|---|---|---|---|
| n = 47 | % | n = 288 | % | p-Value | |
| sore throat | 22 | 46.8 | 59 | 20.5 | <0.001 |
| cough | 20 | 42.6 | 41 | 14.2 | <0.001 |
| fatigue | 23 | 48.9 | 57 | 19.8 | <0.001 |
| rhinitis | 20 | 42.6 | 57 | 19.8 | 0.001 |
| headache | 20 | 42.6 | 101 | 35.1 | 0.322 |
| myalgia | 26 | 55.3 | 22 | 7.6 | <0.001 |
| anosmia | 11 | 23.4 | 9 | 3.1 | <0.001 |
| dysgeusia | 11 | 23.4 | 9 | 3.1 | <0.001 |
| chills | 12 | 25.5 | 20 | 6.9 | <0.001 |
| fever | 10 | 21.3 | 9 | 3.1 | <0.001 |
| chest pain | 5 | 10.6 | 8 | 2.8 | 0.010 |
| shortness of breath | 5 | 10.6 | 15 | 5.2 | 0.145 |
| gastrointestinal symptoms | 0 | 0.0 | 19 | 6.6 | 0.070 |
| Groups | No. of PCR-Positive People | No. and Percentage PCR-Positive People with Symptoms | No. and Percentage of PCR-Positive People without Symptoms |
|---|---|---|---|
| Participants without COVID-19 contact | 204 | 53 (26.0) *,+ | 151 (74.0) + |
| Participants with COVID-19 contact | 47 | 36 (76.6) *,× | 11 (23.4) × |
| Participants | PCR-Positive | IgG-Positive | IgG-Negative |
|---|---|---|---|
| 10 with symptoms | 4 (1 of 3–4 samples was positive) | 2 | 2 |
| 6 (more than 1 of 3–4 samples were positive) | 2 | 4 | |
| 23 without symptoms | 8 (1 of 3–4 samples was positive) | 3 | 5 |
| 12 (more than 1 of 3–4 samples were positive) | 1 | 11 | |
| 3 (intermittent positive and negative samples) | 1 | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jankovics, I.; Müller, C.; Gönczöl, É.; Visontai, I.; Varga, I.; Lőrincz, M.; Kuti, D.; Hasitz, Á.; Malik, P.; Ursu, K.; et al. Asymptomatic and Mild SARS-CoV-2 Infections in a Hungarian Outpatient Cohort in the First Year of the COVID-19 Pandemic. Trop. Med. Infect. Dis. 2023, 8, 204. https://doi.org/10.3390/tropicalmed8040204
Jankovics I, Müller C, Gönczöl É, Visontai I, Varga I, Lőrincz M, Kuti D, Hasitz Á, Malik P, Ursu K, et al. Asymptomatic and Mild SARS-CoV-2 Infections in a Hungarian Outpatient Cohort in the First Year of the COVID-19 Pandemic. Tropical Medicine and Infectious Disease. 2023; 8(4):204. https://doi.org/10.3390/tropicalmed8040204
Chicago/Turabian StyleJankovics, István, Cecília Müller, Éva Gönczöl, Ildikó Visontai, István Varga, Márta Lőrincz, Dávid Kuti, Ágnes Hasitz, Péter Malik, Krisztina Ursu, and et al. 2023. "Asymptomatic and Mild SARS-CoV-2 Infections in a Hungarian Outpatient Cohort in the First Year of the COVID-19 Pandemic" Tropical Medicine and Infectious Disease 8, no. 4: 204. https://doi.org/10.3390/tropicalmed8040204
APA StyleJankovics, I., Müller, C., Gönczöl, É., Visontai, I., Varga, I., Lőrincz, M., Kuti, D., Hasitz, Á., Malik, P., Ursu, K., Bányász, B., Sarkadi, J., & Dénes, B. (2023). Asymptomatic and Mild SARS-CoV-2 Infections in a Hungarian Outpatient Cohort in the First Year of the COVID-19 Pandemic. Tropical Medicine and Infectious Disease, 8(4), 204. https://doi.org/10.3390/tropicalmed8040204








