3.2. Traumatic Events Reported by TB Patients
Pain and discomfort, and anxiety and/or depression were the dominant traumatic events reported among the 439 participants surveyed, with 46.5 and 36.9% of participants reporting either a moderate or serious level of impairment, respectively (
Table 3).
In the univariate analysis, the following variables of household size, disease localization, TB diagnostic, distance to treatment site and the frequency of appointments for drug supply (in days) were significantly associated with stress; the following were significantly associated with anxiety/depression: level of education, household size, distance to treatment site, and the frequency of appointments for drug supply (in days); age, household number size and whether or not antiretroviral treatments were significantly associated with pain/discomfort; age and distance to treatment site were significantly associated with self care; age, level of education, disease localization, treatment history, the frequency of appointments for drug supply (in days) and duration of treatment were significantly associated with usual activities and age, household size, disease localization and the frequency of appointments for drug supply (in days) were significantly associated with mobility (
Table S1 in Supplementary Material).
The multivariate analysis identified numerous associations between the domains and the following socio-demographic and clinical variables. Difficulties performing usual activities were positively and significantly associated with elderly participants (OR = 5.42; 95% CI: 1.57–22.2;
p < 0.05) and patients with drug-resistant TB (OR = 27.7; 95% CI: 6.02–132;
p < 0.005). Those siginficantly less likely to report difficulites with perfoming usual activities included previously-treated patients (OR = 0.02, CI: 0.00–0.011), HIV-negative patients (OR = 0.52; 95% CI: 0.32–0.87; <0.05) and those who had been on treatment for more than 90 days (OR = 0.56; 95% CI: 0.32–0.98;
p < 0.05) (
Table 4).
For a one unit increase in the household size, the odds of reporting pain and discomfort was 1.05 times greater (OR = 1.05; CI: 1.00–1.11,
p < 0.05), and patients who were clinically diagnosed were 93% more likely to have pain and discomfort than those diagnosed bacteriologically (OR = 1.93,CI: 1.06–3.54,
p = 0.031), while patients whose frequency of appointments for drug supply was between 15 and 30 days were 66% less likely to have pain/discomfort than those whose frequency of appointments for drug supply was within 14 days (OR = 0.34,CI: 0.16–0.67,
p = 0.003) (
Table 5).
For anxiety, we found that an increase in one unit in the household size was associated with a higher likelihood of reporting anxiety (OR = 1.08, CI: 1.03–1.14,
p = 0.02), as was distance between patients’ residence to DTCs (OR = 1.03, CI: 1.01–1.05,
p < 0.001), while non TB/HIV coinfected patients were 55% less likely to experience anxiety than those coinfected (OR = 0.45, CI: 0.29–0.71,
p = 0.02;
Table 6).
For a one unit increase in the household size, the odds of reporting stress were 1.08 times greater (OR = 1.08, CI: 1.03, 1.14,
p = 0.002). Non-co-infected TB patients were 55% less likely to be stressed than co-infected ones (OR = 0.45, CI: 0.29–0.71,
p < 0.001). For an increase of one unit in the distance from patients’ residence to DTCs, the odds of anxiety were 1.03 times greater (OR = 1.03, CI: 1.01–1.05,
p < 0.001). Similarly, patients whose frequency of appointments for drug supply was between 15 and 30 days were 65% less likely to be stressed than those whose frequency of appointments for drug supply was ≤14 days (OR = 0.35, CI: 0.14–0.75,
p = 0.011). Likewise, patients whose frequency of appointments for drug supply was >30 days were 99.94% less likely to experience stress than those whose frequency of appointments for drug supply was ≤14 days (OR = 0.06, CI: 0.00, 0.30,
p = 0.007; (
Table 7).
3.3. Qualitative Findings
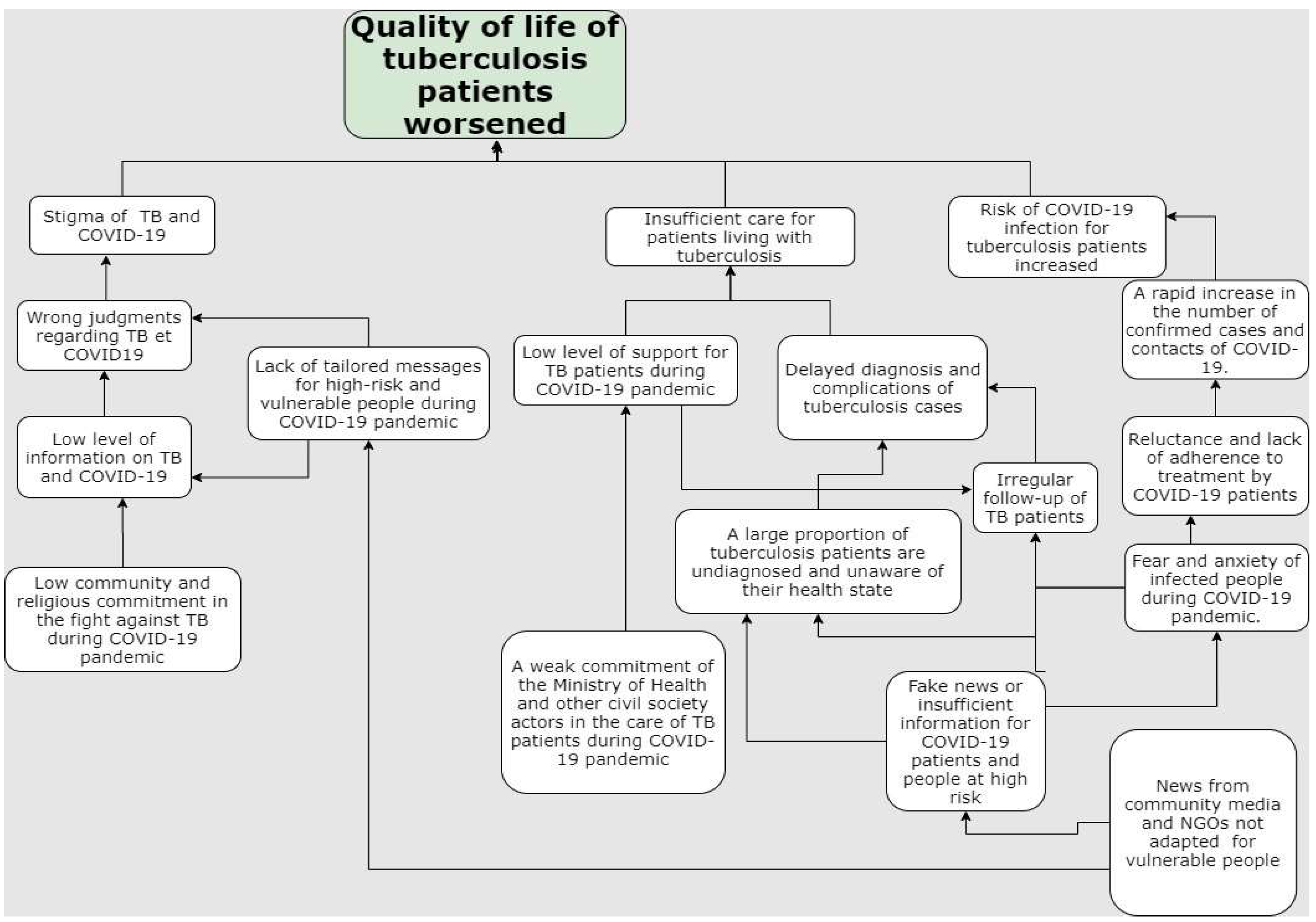
In total, 36 TB patients, including 15 women, were interviewed about their perceptions regarding the COVID-19 pandemic. Thematic analysis was used to identify the following three predominate themes, and six sub-themes that emerged from the quantitative data.
Theme 1. Social and psychological aspect.
Sub-theme. TB patients’ perception about the stigma related to COVID-19.
Different opinions were expressed regarding the social and psychological impact of COVID-19. A commonly expressed concern was related to stigma, with the majority of participants accepting that stigma is commonly experienced by TB patients, and who also felt that the COVID-19 pandemic has increased the amount of stigma towards people with symptoms that may be suggestive of COVID-19. As one participant noted, “Once you cough or sneeze, people distance themselves from you; then you feel bad… they think you have COVID-19 if you cough once or twice. For those who do not know that you have TB, they are going to think that you have COVID-19 because we do not overthink TB now”. One participant shared how some people, without any knowledge on this person’s health status, do not even hesitate to walk away from them with a contemptuous gaze; other TB patients who were interviewed revealed how this practice has become more obvious during the COVID-19 pandemic, with people assuming symptoms such as coughs are an indication of COVID-19, rather than TB, demonstrated by the following statement: “… ‘It’s so clear to me because my husband doesn’t allow me to come near him since he learned that COVID-19 also causes coughs. Usually, I did everything with him. But now, everything has changed, he no longer approaches me like before coronavirus pandemic, we no longer talk too much, and even now we eat separately, you see…”.
Sub-theme. Description of the health status of TB patients during COVID-19 pandemic.
The majority of participants (n = 25) believed that their overall health conditions were better before the start of the COVID-19 pandemic. Some participants reported little hope for a full recovery of their health, due to the difficulties they faced in accessing effective TB treatment during the pandemic and the increasingly difficult living conditions under COVID-19, such as challenges with accessing food, demonstrated by the following statement: “Mentally, I feel like garbage; all I’m worried about right now is how to get my health back. I don’t feel well right now, you see that by yourself! Due to food problems I barely earn, it’s just filling my stomach. Currently, it’s not okay, and sometimes I don’t have transport to get to the centre or sometimes even if you leave you are told that the centre is out of medication. I have lost a lot of weight at the moment. I lost much hope despite the encouragement of the doctors”.
Theme 2. Economic aspects.
Sub-theme. Financial situation of TB patients during the COVID-19 pandemic.
Respondants highlighted how the cessation of certain activities during the COVID-19 pandemic directly and/or indirectly affected their financial conditions, which created challenges for accessing TB services and maintaining their treatment as this participant, who earns money to support their family through artistic activities, noted in the following statement: “…. Financially it [the situation during COVID-19] is not good. There are no events, and as I am an artist, this is where I earn money to feed my family and pay for transportation to the [treatment] centre. But as there is currently no event, even finding transport to get to the treatment centre is a problem because transport is expensive, sometimes we do not come on the date that the doctors tell us to come, because we don’t have transportation. You see, it’s not easy”.
Sub-theme. Diet of TB patients during the COVID-19 pandemic.
TB patients revealed during their interviews that their health condition had deteriorated significantly during COVID-19 due to the lack of an appropriate diet. They noted how they were no longer able to comply with the diet recommended by their doctors, as this participant noted in the following statement: “I cannot eat all of the foods my doctor recommends. I eat with difficulty, and for example, with this difficult situation, I only eat rice. I have diabetes, and my doctor has advised me to limit my intake a bit. But I have to consume it because that’s what I earn”.
Theme 3. Perceptions on government actions during the COVID-19 pandemic.
Sub-theme. Restrictive measures.
According to our participants, the Guinean population’s life depends on their daily economic activities; therefore, the restrictive measures imposed by the Government to limit the spread of COVID-19 were largely regarded as drastic and thought to cause more harm than good, as shown by the following statement: “These measures of the state are salutary, but which is not without consequences for some, you knew it as well as me sir… these measures make life difficult by blocking the activities of people, and you know here what we see, that’s what we eat. Guineans eat from day to day, so these measures increase their suffering”.
Sub-theme. Mitigation measures.
Unanimously, respondents believed that the Government should financially help its people, especially those who were sick, poor, children or elderly, demonstrated by the following statement: “I thank the state for what is already done the price of fuel at the pump, this leads to a reduction in the prices of necessities (rice, sugar …), and, therefore facilitates access to food by the population. But some do not benefit from it and others do not even know about it. But when the price drops, everyone will feel this impact on their living condition”. Likewise, some believed that special attention should be paid to TB patients given the additional burdens created by their illness, as shown by the following statement: “Yes, the state should help its population, especially patients like us tuberculosis patients who are rejected by our bosses for fear of being infected ……”.