Involvement of Pore Formation and Osmotic Lysis in the Rapid Killing of Gamma Interferon-Pretreated C166 Endothelial Cells by Rickettsia prowazekii
Abstract
1. Introduction
2. Materials and Methods
2.1. Cultured Cells, IFN-γ, PEGs, Rickettsiae, and Control L929 Cell Preparation
2.1.1. Cultured Cells and IFN-γ
2.1.2. PEGs
2.1.3. Rickettsiae and Control L929 Cell Preparation
2.2. Preparation of Cultures of Untreated and IFN-γ-Pretreated C166 Endothelial Cells, Mock Infection or Infection of the C166 Cells with Rickettsiae, Evaluation of the Infection, and Assessment of Damage to the Endothelial Cells in the Absence or Presence of PEGs
2.2.1. Preparation of Untreated and IFN-γ-Pretreated C166 Endothelial Cells
2.2.2. Mock Infection or Infection of the C166 Cells with Rickettsiae in the Absence or Presence of PEGs
2.2.3. Evaluation of Rickettsial Infection
2.2.4. Assessment of Damage to the Endothelial Cells with Trypan Blue Dye
2.2.5. Evaluation of Damage to the Endothelial Cells in the Absence or Presence of PEGs at Various Times after Mock-Infection or Infection
2.3. Statistical Analyses
3. Results
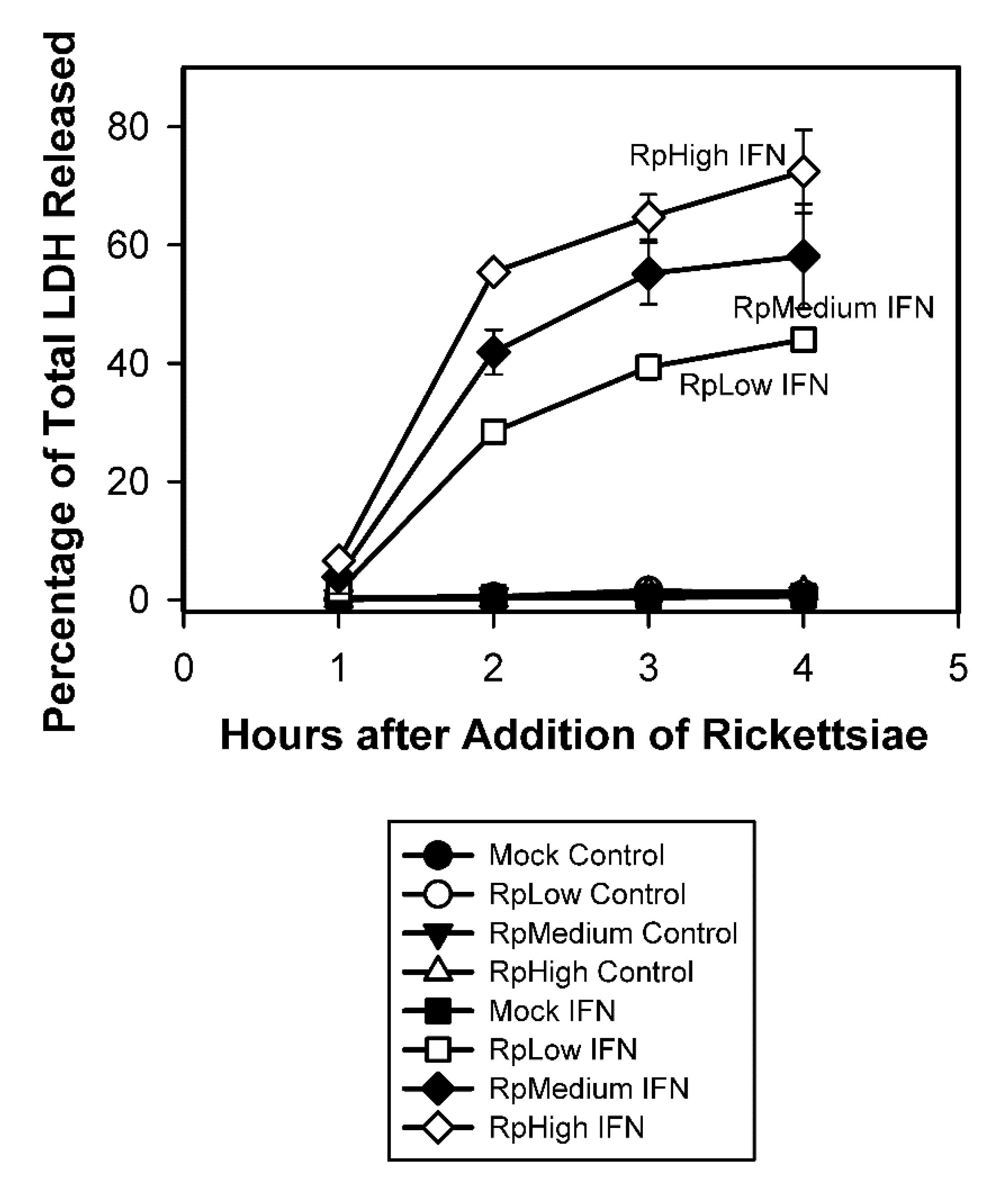
3.1. Substantial Percentages of IFN-γ-Pretreated C166 Endothelial Cells Were Damaged within Four Hours after Addition of R. prowazekii
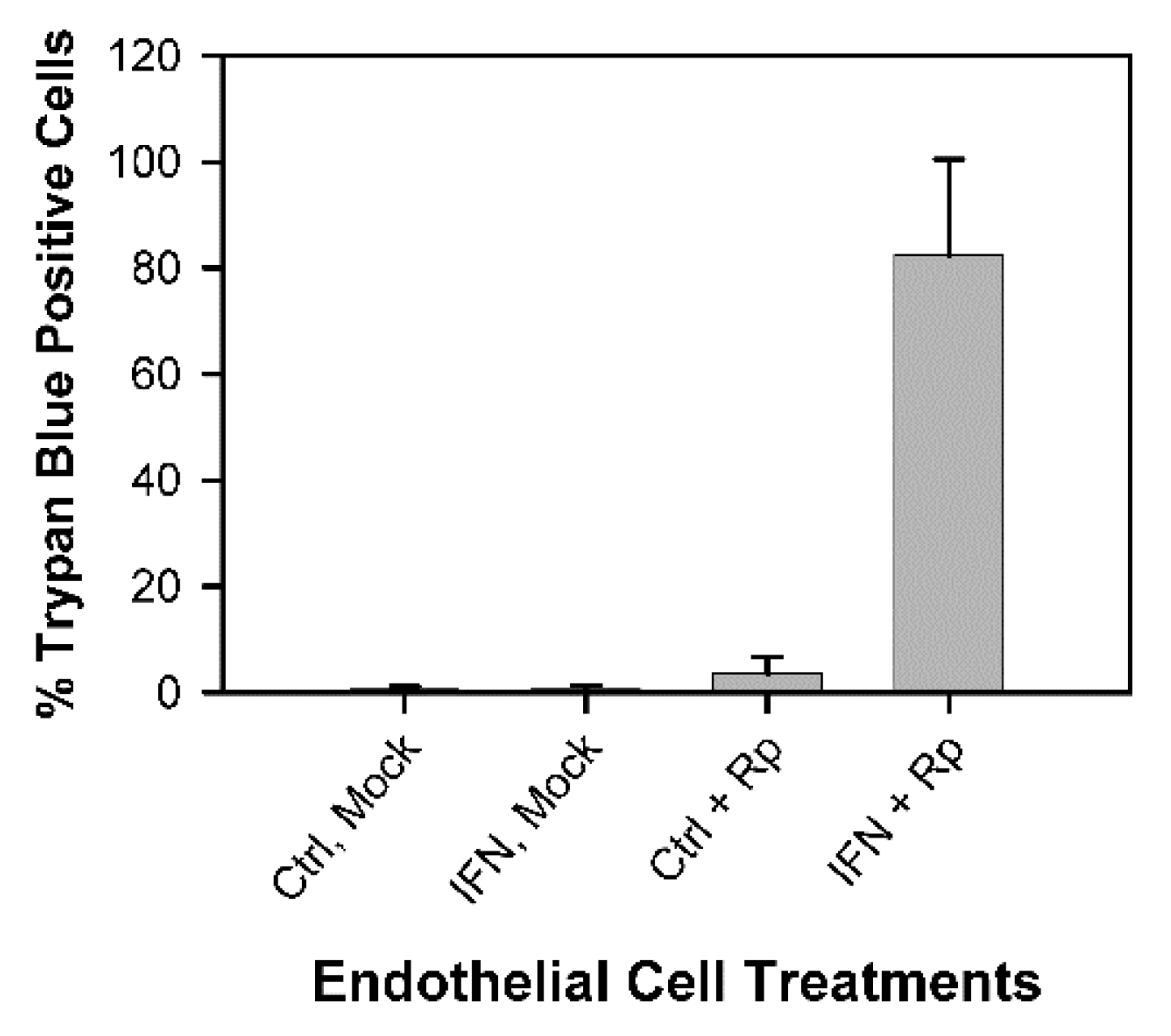
3.1.1. Results of Assessment of Endothelial Cell Damage by Trypan Blue Staining
3.1.2. Results of Assessment of Endothelial Cell Damage by Ethidium Bromide Staining
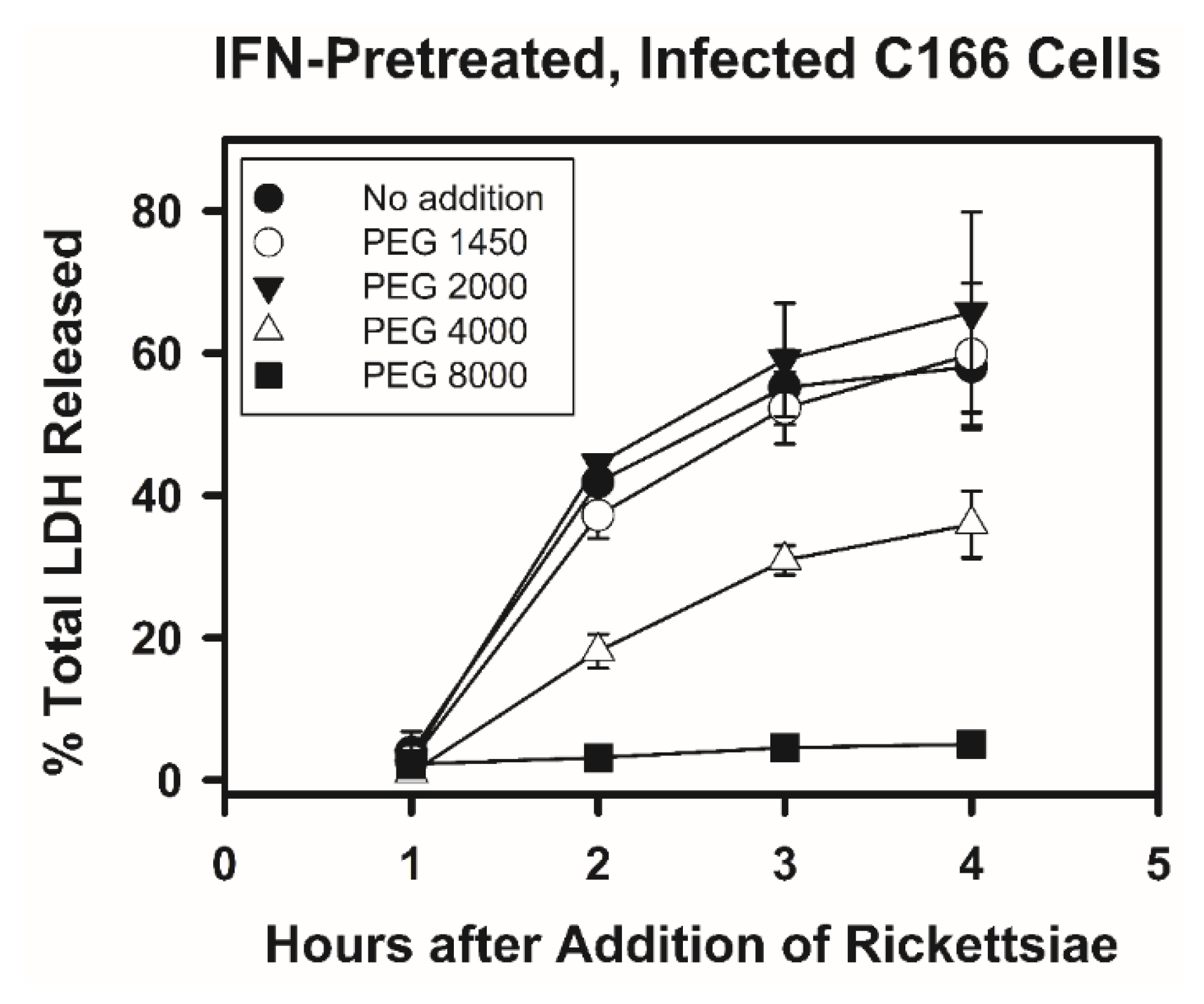
3.2. Effect of Polyethylene Glycols (PEGs) with Various Nominal Average Molecular Weights on the Release of LDH by IFN-γ-Pretreated C166 Endothelial Cells after Infection with R. prowazekii
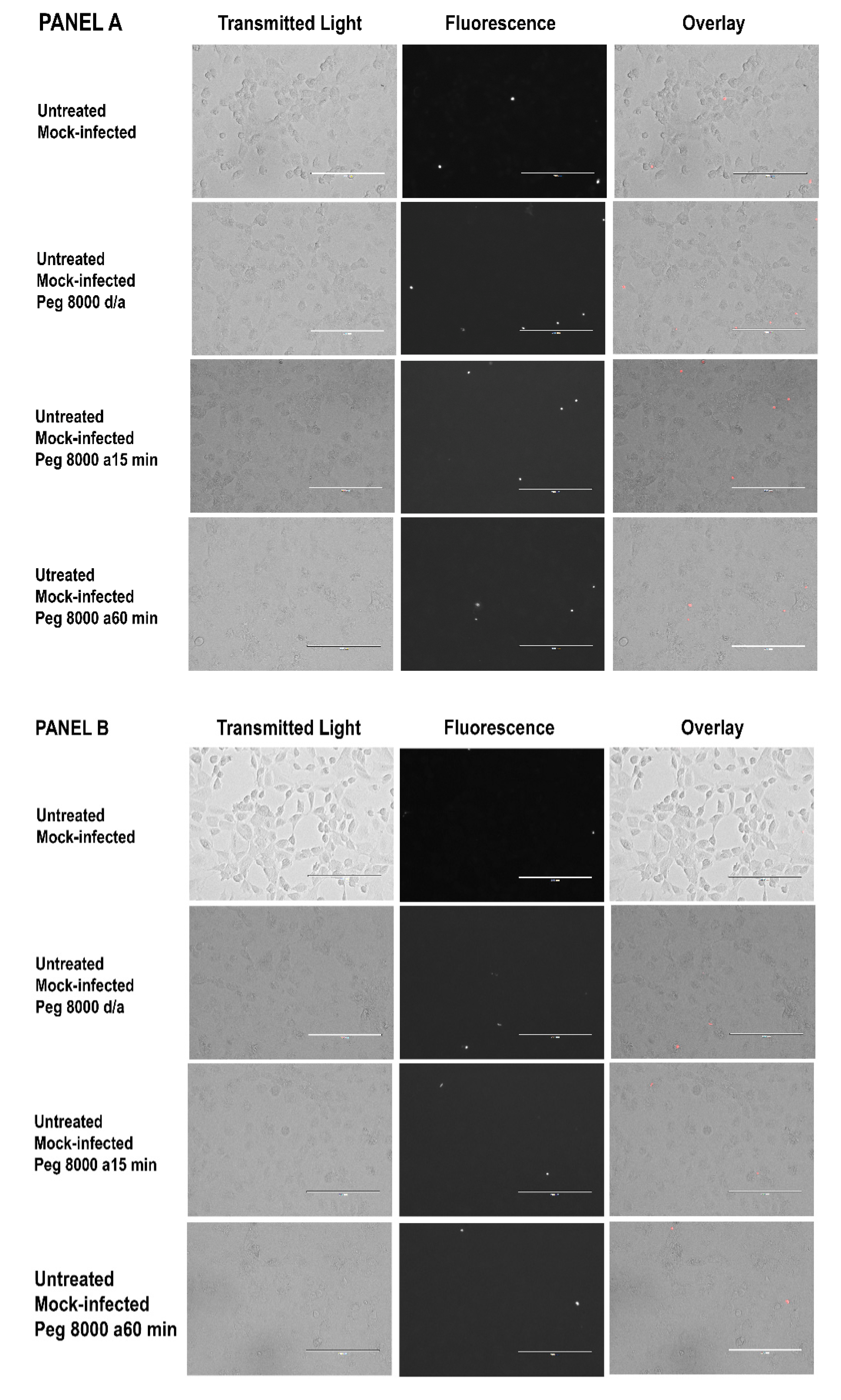
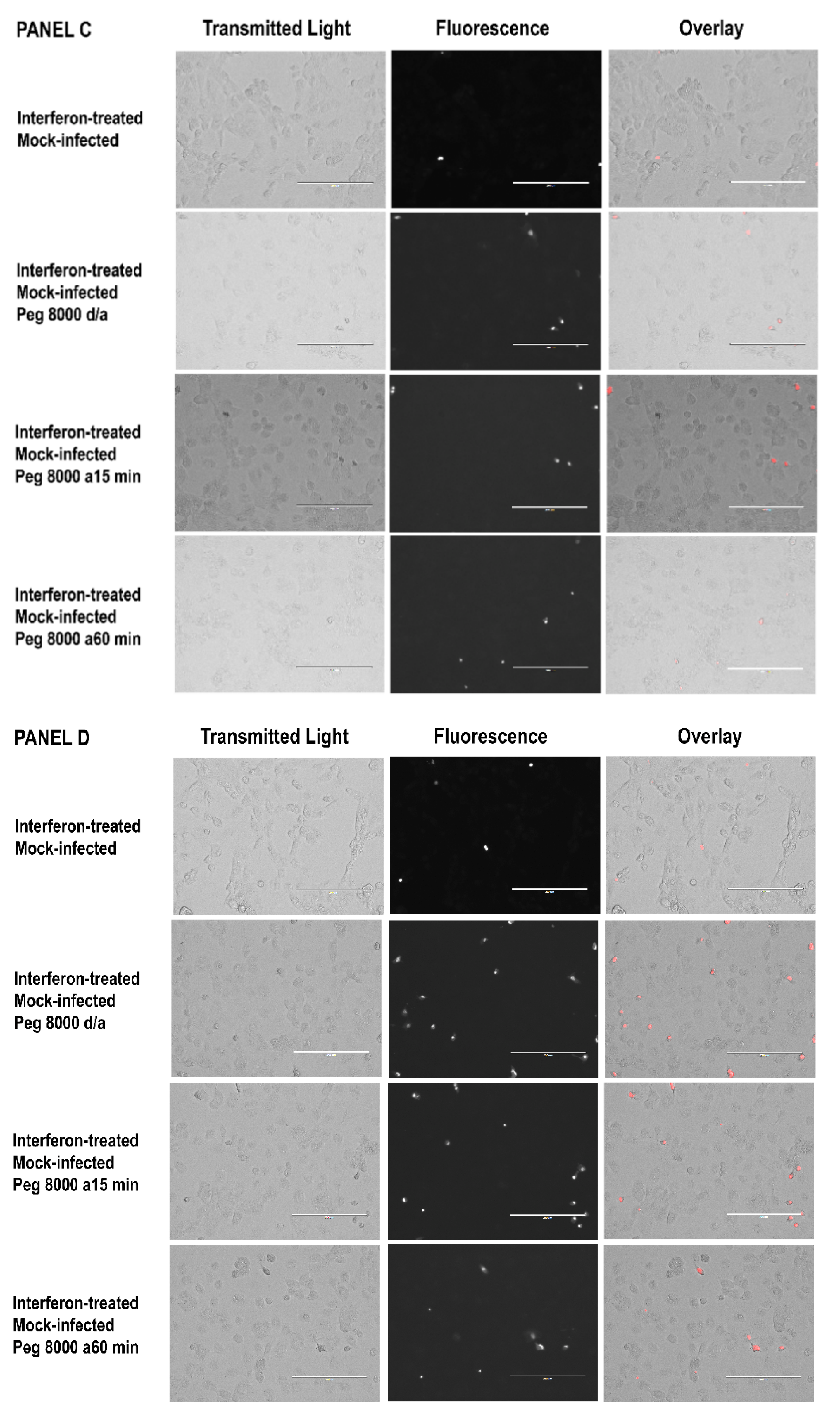
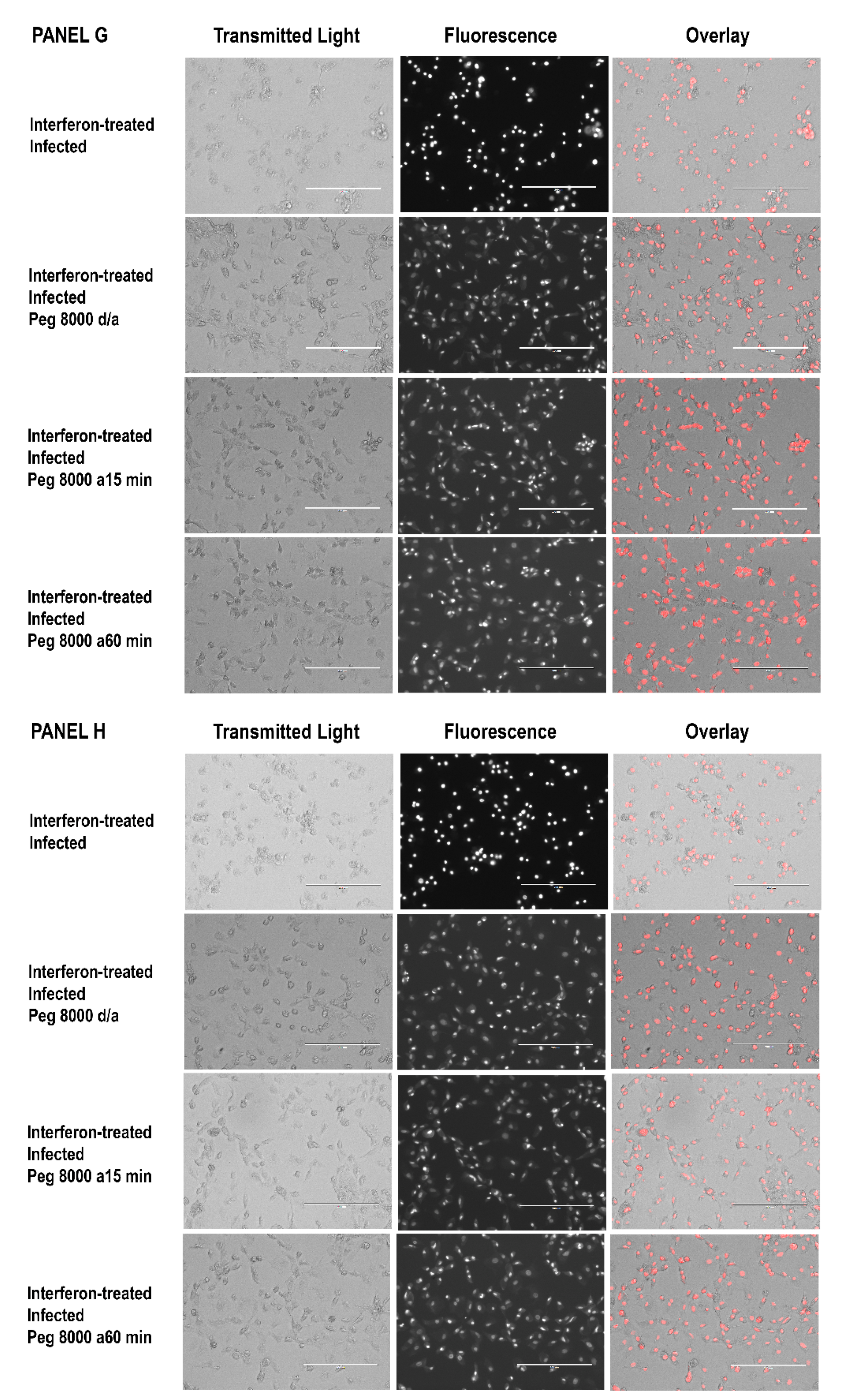
3.3. Inability of PEG 8000 to Prevent the Uptake of Ethidium Bromide by IFN-γ-Pretreated, R. prowazekii-Infected Endothelial Cells
4. Discussion
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fournier, P.-E.; Raoult, D. Rickettsia. In Bergey’s Manual of Systematics of Archaea and Bacteria; Trujillo, M.E., Dedysh, S., DeVos, P., Hedlund, B., Kämpfer, P., Rainey, F.A., Whitman, W.B., Eds.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2019; pp. 1–42. [Google Scholar] [CrossRef]
- Blanton, L.S. The rickettsioses, a practical update. Infect. Dis. Clin. N. Am. 2019, 33, 213–229. [Google Scholar] [CrossRef] [PubMed]
- Salje, J. Cells within cells: Rickettsiales and the obligate intracellular bacterial lifestyle. Nat. Rev. Microbiol. 2021, 19, 375–390. [Google Scholar] [CrossRef] [PubMed]
- McGinn, J.; Lamason, R.L. The enigmatic biology of rickettsiae: Recent advances, open questions and outlook. Pathog. Dis. 2021, 79, ftab019. [Google Scholar] [CrossRef] [PubMed]
- Voss, O.H.; Rahman, M.S. Rickettsia-host interaction: Strategies of intracytosolic host colonization. Pathog. Dis. 2021, 79, ftab015. [Google Scholar] [CrossRef] [PubMed]
- Salje, J.; Weitzel, T.; Newton, P.N.; Varghese, G.M.; Day, N. Rickettsial infections: A blind spot in our view of neglected tropical diseases. PLoS Negl. Trop. Dis. 2021, 15, e0009353. [Google Scholar] [CrossRef] [PubMed]
- Bechah, Y.; Capo, C.; Mege, J.-L.; Raoult, D. Epidemic typhus. Lancet Infect. Dis. 2008, 8, 417–426. [Google Scholar] [CrossRef]
- Angelakis, E.; Bechah, Y.; Raoult, D. The history of epidemic typhus. Microbiol. Spectr. 2016, 4, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Bechah, Y.; Capo, C.; Mege, J.-L.; Raoult, D. Rickettsial diseases: From rickettsia-arthropod relationships to pathophysiology and animal models. Future Microbiol. 2008, 3, 223–236. [Google Scholar] [CrossRef]
- Sahni, S.K.; Rydkina, E. Host cell interactions with pathogenic Rickettsia species. Future Microbiol. 2009, 4, 323–339. [Google Scholar] [CrossRef] [PubMed]
- Dumler, J.S. Clinical disease: Current treatment and new challenges. In Intracellular Pathogens II, Rickettsiales; Palmer, G.H., Azad, A.F., Eds.; ASM Press: Washington, DC, USA, 2012; pp. 1–39. [Google Scholar]
- Walker, D.H.; Ismail, N. Emerging and re-emerging rickettsioses: Endothelial cell infection and early disease events. Nat. Rev. Microbiol. 2008, 6, 375–386. [Google Scholar] [CrossRef] [PubMed]
- Sahni, S.K.; Narra, H.P.; Sahni, A.; Walker, D.H. Recent molecular insights into rickettsial pathogenesis and immunity. Future Microbiol. 2013, 8, 1265–1288. [Google Scholar] [CrossRef] [PubMed]
- Narra, H.P.; Sahni, A.; Walker, D.H.; Sahni, S.K. Recent research milestones in the pathogenesis of human rickettsioses and opportunities ahead. Future Microbiol. 2020, 15, 753–765. [Google Scholar] [CrossRef] [PubMed]
- Sahni, A.; Fang, R.; Sahni, S.; Walker, D.H. Pathogenesis of rickettsial diseases: Pathogenic and immune mechanisms of an endotheliotropic infection. Annu. Rev. Pathol. 2019, 14, 127–152. [Google Scholar] [CrossRef]
- Gambrill, M.R.; Wisseman, C.L., Jr. Mechanisms of immunity in typhus infections. II. Multiplication of typhus rickettsiae in human macrophage cell cultures in the nonimmune system: Influence of virulence of rickettsial strains and of chloramphenicol. Infect. Immun. 1973, 8, 519–527. [Google Scholar] [CrossRef]
- Turco, J.; Winkler, H.H. Differentiation between virulent and avirulent strains of Rickettsia prowazekii by macrophage-like cell lines. Infect. Immun. 1982, 35, 783–791. [Google Scholar] [CrossRef] [PubMed]
- Kristof, M.N.; Allen, P.E.; Yutzy, L.D.; Thibodaux, B.; Paddock, C.D.; Martinez, J.J. Significant growth by Rickettsia species within human macrophage-like cells is a phenotype correlated with the ability to cause disease in mammals. Pathogens 2021, 10, 228. [Google Scholar] [CrossRef]
- Turco, J.; Winkler, H.H. Effect of mouse lymphokines and cloned mouse interferon-γ on the interaction of Rickettsia prowazekii with mouse macrophage-like RAW264.7 cells. Infect. Immun. 1984, 45, 303–308. [Google Scholar] [CrossRef]
- Turco, J.; Winkler, H.H. Interactions between Rickettsia prowazekii and cultured host cells: Alterations induced by gamma interferon. In Interferon and Nonviral Pathogens; Byrne, G.I., Turco, J., Eds.; Marcel Dekker, Inc.: New York, NY, USA, 1988; pp. 95–115. [Google Scholar]
- Turco, J.; Winkler, H.H. Cytokines influencing infections by Rickettsia species. In Rickettsial Infection and Immunity; Anderson, B., Friedman, H., Bendinelli, M., Eds.; Plenum Publishing Corp.: New York, NY, USA, 1997; pp. 29–52. [Google Scholar]
- Turco, J.; Winkler, H.H. Role of the nitric oxide synthase pathway in the inhibition of growth of interferon-sensitive and interferon-resistant Rickettsia prowazekii strains in L929 cells treated with tumor necrosis factor alpha and gamma interferon. Infect. Immun. 1993, 61, 4317–4325. [Google Scholar] [CrossRef] [PubMed]
- Turco, J.; Winkler, H.H. Relationship of tumor necrosis factor alpha, the nitric oxide synthase pathway, and lipopolysaccharide to the killing of gamma interferon-treated macrophagelike RAW264.7 cells by Rickettsia prowazekii. Infect. Immun. 1994, 62, 2568–2574. [Google Scholar] [CrossRef]
- Turco, J.; Liu, H.; Gottlieb, S.F.; Winkler, H.H. Nitric oxide-mediated inhibition of the ability of Rickettsia prowazekii to infect mouse fibroblasts and mouse macrophagelike cells. Infect. Immun. 1998, 66, 558–566. [Google Scholar] [CrossRef]
- Feng, H.-M.; Popov, V.L.; Walker, D.H. Depletion of gamma interferon and tumor necrosis factor alpha in mice with Rickettsia conorii-infected endothelium: Impairment of rickettsicidal nitric oxide production resulting in fatal, overwhelming rickettsial disease. Infect. Immun. 1994, 62, 1952–1960. [Google Scholar] [CrossRef]
- Walker, D.H.; Popov, V.L.; Feng, H.-M. Establishment of a novel endothelial target mouse model of a typhus group rickettsiosis: Evidence for critical roles for gamma interferon and CD8 T lymphocytes. Lab. Investig. 2000, 80, 1361–1372. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Burke, T.P.; Engström, P.; Tran, C.J.; Langohr, I.M.; Glasner, D.R.; Espinosa, D.A.; Harris, E.; Welch, M.D. Interferon receptor-deficient mice are susceptible to eschar-associated rickettsiosis. eLife 2021, 10, e67029. [Google Scholar] [CrossRef] [PubMed]
- Galluzzi, L.; Vitale, I.; Aaronson, S.A.; Abrams, J.M.; Adam, D.; Agostinis, P.; Alnemri, E.; Altucci, L.; Amelio, I.; Andrews, D.W.; et al. Molecular mechanisms of cell death: Recommendations of the nomenclature committee on cell death. Cell Death Differ. 2018, 25, 486–541. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.-M.; Li, Z.-X.; Lin, R.-H.; Shan, J.-Q.; Yu, Q.-W.; Wang, R.-X.; Liao, L.-S.; Yan, W.-T.; Wang, Z.; Shang, L.; et al. Guidelines for regulated cell death assays: A systematic summary, a categorical comparison, a prospective. Front. Cell Dev. Biol. 2021, 9, 634690. [Google Scholar] [CrossRef] [PubMed]
- D’Arcy, M.S. Cell death: A review of the major forms of apoptosis, necrosis and autophagy. Cell Biol. Int. 2019, 43, 582–592. [Google Scholar] [CrossRef]
- Loterio, R.K.; Zamboni, D.S.; Newton, H.J. Keeping the host alive—Lessons from obligate intracelllular bacterial pathogens. Pathog. Dis. 2021, 79, ftab052. [Google Scholar] [CrossRef] [PubMed]
- Romo, R.R. Cell death as part of innate immunity: Cause or consequence? Immunology 2021, 163, 399–415. [Google Scholar] [CrossRef] [PubMed]
- Imre, G. The involvement of regulated cell death forms in modulating bacterial and viral pathogenesis. Int. Rev. Cell Mol. Biol. 2020, 353, 211–253. [Google Scholar] [CrossRef]
- Song, H.; Yang, B.; Li, Y.; Qian, A.; Kang, Y.; Shan, X. Focus on the mechanisms and functions of pyroptosis, inflammasomes, and inflammatory caspases in infectious diseases. Oxid. Med. Cell. Longev. 2022, 2022, 2501279. [Google Scholar] [CrossRef]
- Tummers, B.; Green, D.R. The evolution of regulated cell death pathways in animals and their evasion by pathogens. Physiol. Rev. 2022, 102, 411–454. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, I.; Rayamajhi, M.; Miao, E.A. Programmed cell death as a defence against infection. Nat. Rev. Immunol. 2017, 17, 151–164. [Google Scholar] [CrossRef]
- Joshi, S.G.; Francis, C.W.; Silverman, D.J.; Sahni, S.K. Nuclear factor κB protects against host cell apoptosis during Rickettsia rickettsii infection by inhibiting activation of apical and effector caspases and maintaining mitochondrial integrity. Infect. Immun. 2003, 71, 4127–4136. [Google Scholar] [CrossRef] [PubMed]
- Joshi, S.G.; Francis, C.W.; Silverman, D.J.; Sahni, S.K. NF-κB activation suppresses host cell apoptosis during Rickettsia rickettsii infection via regulatory effects on intracellular localization or levels of apoptogenic and anti-apoptotic proteins. FEMS Microbiol. Lett. 2004, 234, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Burke, T.P.; Engström, P.; Chavez, R.A.; Fonbuena, J.A.; Vance, R.E.; Welch, M.D. Inflammasome-mediated antagonism of type I interferon enhances Rickettsia pathogenesis. Nat. Microbiol. 2020, 5, 688–696. [Google Scholar] [CrossRef] [PubMed]
- Voss, O.H.; Cobb, J.; Gaytan, H.; Diaz, N.R.; Sanchez, R.; DeTolla, L.; Rahman, M.S.; Azad, A.F. Pathogenic, but not non-pathogenic, Rickettsia spp. evade inflammasome-dependent IL-1 responses to establish an intracytosolic replication niche. mBio 2022, 13, e02918-21. [Google Scholar] [CrossRef] [PubMed]
- Engström, P.; Burke, T.P.; Mitchell, G.; Ingabire, N.; Mark, K.G.; Golovkine, G.; Iavarone, A.T.; Rape, M.; Cox, J.S.; Welch, M.D. Evasion of autophagy mediated by Rickettsia surface protein OmpB is critical for virulence. Nat. Microbiol. 2019, 4, 2538–2551. [Google Scholar] [CrossRef] [PubMed]
- Engström, P.; Burke, T.P.; Tran, C.J.; Iavarone, A.T.; Welch, M.D. Lysine methylation shields an intracellular pathogen from ubiquitylation and autophagy. Sci. Adv. 2021, 7, eabg2517. [Google Scholar] [CrossRef]
- Bechelli, J.; Smalley, C.; Milhano, N.; Walker, D.H.; Fang, R. Rickettsia massiliae and Rickettsia conorii Israeli spotted fever strain differentially regulate endothelial cell responses. PLoS ONE 2015, 10, e0138830. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Flores-Romero, H.; Ros, U.; Garcia-Saez, A.J. Pore formation in regulated cell death. EMBO J. 2020, 39, e105753. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chen, X.; Gueydan, C.; Han, J. Plasma membrane changes during programmed cell deaths. Cell Res. 2018, 28, 9–21. [Google Scholar] [CrossRef]
- Newton, K.; Dixit, V.M.; Kayagaki, N. Dying cells fan the flames of inflammation. Science 2021, 374, 1076–1080. [Google Scholar] [CrossRef] [PubMed]
- Verma, P.; Gandhi, S.; Lata, K.; Chattopadhyay, K. Pore-forming toxins in infection and immunity. Biochem. Soc. Trans. 2021, 49, 455–465. [Google Scholar] [CrossRef]
- Peraro, M.D.; Van der Goot, F.G. Pore-forming toxins: Ancient, but never really out of fashion. Nat. Rev. Microbiol. 2016, 14, 77–92. [Google Scholar] [CrossRef] [PubMed]
- Ulhuq, F.R.; Giuseppina, M. Bacterial pore-forming toxins. Microbiology 2022, 168, 001154. [Google Scholar] [CrossRef] [PubMed]
- Lobo, A.L.; Welch, R.A. Identification and assay of RTX family of cytolysins. In Methods in Enzymology, Bacterial Pathogenesis, Part A, Identification and Regulation of Virulence Factors; Clark, V.L., Bavoil, P.M., Eds.; Academic Press: San Diego, CA, USA, 1994; Volume 235, pp. 667–678. [Google Scholar]
- Viboud, G.I.; Bliska, J.B. Measurement of pore formation by contact-dependent Type III protein secretion systems. In Methods in Enzymology, Bacterial Pathogenesis, Part C, Identification, Regulation and Function of Virulence Factors; Clark, V., Bavoil, P., Eds.; Academic Press: Cambridge, MA, USA, 2002; Volume 358, pp. 345–350. [Google Scholar]
- Pei, J.; Turse, J.E.; Wu, Q.; Ficht, T.A. Brucella abortus rough mutants induce macrophage oncosis that requires bacterial protein synthesis and direct interaction with the macrophage. Infect. Immun. 2006, 74, 2667–2675. [Google Scholar] [CrossRef] [PubMed]
- Fink, S.L.; Cookson, B.T. Caspase-1-dependent pore formation during pyroptosis leads to osmotic lysis of infected host macrophages. Cell. Microbiol. 2006, 8, 1812–1825. [Google Scholar] [CrossRef]
- Sun, G.W.; Lu, J.; Pervaiz, S.; Cao, W.P.; Gan, Y.-H. Caspase-1 dependent macrophage death induced by Burkholderia pseudomallei. Cell. Microbiol. 2005, 7, 1447–1458. [Google Scholar] [CrossRef]
- Turco, J.; Winkler, H.H. Inhibition of the growth of Rickettsia prowazekii in cultured fibroblasts by lymphokines. J. Exp. Med. 1983, 157, 974–986. [Google Scholar] [CrossRef]
- Vernon, K.H.; Turco, J. Viability of Rickettsia prowazekii after rickettsia-mediated killing of gamma interferon-pretreated, macrophage-like RAW264.7 cells. Ga. J. Sci. 2016, 74, 9. Available online: https://digitalcommons.gaacademy.org/gjs/vol74/iss2/9/ (accessed on 23 July 2022).
- Wisseman, C.L., Jr.; Waddell, A.D.; Walsh, W.T. In vitro studies of the action of antibiotics on Rickettsia prowazeki by two basic methods of cell culture. J. Infect. Dis. 1974, 130, 564–574. [Google Scholar] [CrossRef] [PubMed]
- Giménez, D.F. Staining rickettsiae in yolk-sac cultures. Stain Technol. 1964, 39, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Berestovsky, G.N.; Ternovsky, V.I.; Kataev, A.A. Through pore diameter in the cell wall of Chara coralline. J. Exp. Bot. 2001, 52, 1173–1177. [Google Scholar] [CrossRef]
- Turco, J.; Keysary, A.; Winkler, H.H. Interferon-γ and rickettsia-induced killing of macrophage-like cells is inhibited by antirickettsial antibodies and does not require the respiratory burst. J. Interferon Res. 1989, 9, 615–629. [Google Scholar] [CrossRef]
- Winkler, H.H.; Day, L.; Daugherty, R.; Turco, J. Effect of gamma interferon on phospholipid hydrolysis and fatty acid incorporation in L929 cells infected with Rickettsia prowazekii. Infect. Immun. 1993, 61, 3412–3415. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zhao, Y.; Zhang, P.; Li, Y.; Yang, Y.; Yang, Y.; Zhu, J.; Song, X.; Jiang, G.; Fan, J. Hemorrhagic shock primes for lung vascular endothelial cell pyroptosis: Role in pulmonary inflammation following LPS. Cell Death Dis. 2016, 7, e2363. [Google Scholar] [CrossRef]
- Cheng, K.T.; Xiong, S.; Ye, Z.; Hong, Z.; Di, A.; Tsang, K.M.; Gao, X.; An, S.; Mittal, M.; Vogel, S.M.; et al. Caspase-11-mediated endothelial pyroptosis underlies endotoxemia-induced lung injury. J. Clin. Investig. 2017, 127, 4124–4135. [Google Scholar] [CrossRef]
- Pei, J.; Wu, Q.; Kahl-McDonagh, M.; Ficht, T.A. Cytotoxicity in macrophages infected with rough Brucella mutants is type IV secretion system dependent. Infect. Immun. 2008, 76, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Rupper, A.C.; Cardelli, J.A. Induction of guanylate binding protein 5 by gamma interferon increases susceptibility to Salmonella enterica Serovar Typhimurium-induced pyroptosis in RAW 264.7 cells. Infect. Immun. 2008, 76, 2304–2315. [Google Scholar] [CrossRef] [PubMed]
- Hao, Q.; Shetty, S.; Tucker, T.A.; Idell, S.; Tang, H. Interferon-γ preferentially promotes necroptosis of lung epithelial cells by upregulating MLKL. Cells 2022, 11, 563. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, J.J.; Kaur, S.J.; Rahman, M.S.; Rennoll-Bankert, K.; Sears, K.T.; Beier-Sexton, M.; Azad, A.F. Secretome of obligate intracellular Rickettsia. FEMS Microbiol. Rev. 2015, 39, 47–80. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, J.J.; Phan, I.Q.; Driscoll, T.P.; Guillotte, M.L.; Lehman, S.S.; Rennoll-Bankert, K.E.; Subramanian, S.; Beier-Sexton, M.; Myler, P.J.; Rahman, M.S.; et al. The Rickettsia type IV secretion system: Unrealized complexity mired by gene family expansion. Pathog. Dis. 2016, 74, ftw058. [Google Scholar] [CrossRef]
- Housley, N.A.; Winkler, H.H.; Audia, J.P. The Rickettsia prowazekii Exo U homologue possesses phospholipase A1 (PLA1), PLA2, and lyso-PLA2 activities and can function in the absence of any eukaryotic cofactors in vitro. J. Bacteriol. 2011, 193, 4634–4642. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.S.; Ammerman, N.C.; Sears, K.T.; Ceraul, S.M.; Azad, A.F. Functional characterization of a phospholipase A2 homolog from Rickettsia typhi. J. Bacteriol. 2010, 192, 3294–3303. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.S.; Gillespie, J.J.; Kaur, S.J.; Sears, K.T.; Ceraul, S.M.; Beier-Sexton, M.; Azad, A.F. Rickettsia typhi possesses phospholipase A2 enzymes that are involved in infection of host cells. PLoS Pathog. 2013, 9, e1003399. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hardy, K.S.; Tuckey, A.N.; Renema, P.; Patel, M.; Al-Mehdi, A.-B.; Spadafora, D.; Schlumpf, C.A.; Barrington, R.A.; Alexeyev, M.F.; Stevens, T.; et al. ExoU induces lung endothelial cell damage and activates pro-inflammatory caspase-1 during Pseudomonas aeruginosa infection. Toxins 2022, 14, 152. [Google Scholar] [CrossRef] [PubMed]


| Treatment b | Infection c | Addition d | % Total LDH Released at the following Time after Infection or Mock Infection | ||||
|---|---|---|---|---|---|---|---|
| Removed e | 1 h | 2 h | 3 h | 4 h | |||
| Untreated | Mock | No addition | — | 0.2 ± 0.2 (10) | 0.4 ± 0.4 (6) | 0.4 ± 0.6 (16) | 0.7 ± 0.5 (15) |
| PEG 1450 | — | 0.0 ± 0.0 (2) | 0.0 ± 0.0 (2) | 0.0 ± 0.0 (2) | 0.2 ± 0.2 (2) | ||
| PEG 2000 | — | 0.0 ± 0.0 (2) | 0.0 ± 0.0 (2) | 0.0 ± 0.0 (2) | 0.4 ± 0.4 (4) | ||
| PEG 4000 | — | 1.3 ± 1.5 (6) | 1.7 ± 0.9 (6) | 1.5 ± 1.0 (6) | 1.2 ± 1.0 (8) | ||
| PEG 4000 A-1 h | — | — | 0.5 ± 0.0 (2) | 0.4 ± 0.0 (2) | 0.4 ± 0.1 (2) | ||
| PEG 8000 | — | 2.2 ± 0.6 (2) | 1.7 ± 0.4 (2) | 1.8 ± 0.5 (14) | 2.1 ± 0.7 (12) | ||
| PEG 8000 A-0.25 h | 0.4 ± 0.1 (2) | — | — | 1.2 ± 0.1 (2) | 1.5 ± 0.1 (4) | ||
| PEG 8000 A-1 h | — | — | — | — | 1.7 ± 0.2 (4) | ||
| Interferon | Mock | No addition | — | 0.4 ± 0.5 (10) | 0.4 ± 0.7 (6) | 0.6 ± 0.6 (16) | 0.7 ± 0.6 (15) |
| PEG 1450 | — | 0.0 ± 0.0 (2) | 0.0 ± 0.0 (2) | 0.0 ± 0.0 (2) | 0.0 ± 0.0 (2) | ||
| PEG 2000 | — | 0.0 ± 0.0 (2) | 0.0 ± 0.0 (2) | 0.0 ± 0.0 (2) | 0.5 ± 0.7 (4) | ||
| PEG 4000 | — | 1.2 ± 1.6 (6) | 2.1 ± 1.7 (6) | 4.1 ± 1.1 (6) | 4.8 ± 2.5 (7) | ||
| PEG 4000 A-1 h | — | — | 0.3 ± 0.0 (2) | 0.6 ± 0.1 (2) | 0.6 ± 0.1 (2) | ||
| PEG 8000 | — | 2.3 ± 0.4 (4) | 2.3 ± 0.3 (4) | 2.0 ± 0.5 (16) | 2.7 ± 1.2 (14) | ||
| PEG 8000 A-0.25 h | 0.7 ± 0.5 (2) | — | — | 1.6 ± 0.1 (2) | 1.5 ± 0.2 (2) | ||
| PEG 8000 A-1 h | — | — | — | — | 1.6 ± 0.3 (4) | ||
| Untreated | Rp | No addition | — | 0.3 ± 0.4 (11) | 0.6 ± 0.4 (6) | 0.6 ± 0.7 (16) | 0.8 ± 0.4 (13) |
| PEG 1450 | — | 0.0 ± 0.0 (2) | 0.0 ± 0.0 (2) | 0.0 ± 0.0 (2) | 0.0 ± 0.0 (2) | ||
| PEG 2000 | — | 0.0 ± 0.0 (2) | 0.3 ± 0.4 (2) | 0.3 ± 0.4 (2) | 0.0 ± 0.0 (2) | ||
| PEG 4000 | — | 0.8 ± 1.0 (5) | 1.2 ± 1.1 (5) | 1.6 ± 1.2 (5) | 1.6 ± 1.1 (5) | ||
| PEG 4000 A-1 h | — | — | 0.4 ± 0.0 (2) | 0.3 ± 0.2 (2) | 0.3 ± 0.2 (2) | ||
| PEG 8000 | — | 1.7 ± 0.2 (2) | 2.8 ± 0.4 (2) | 1.7 ± 0.5 (14) | 2.6 ± 1.0 (12) | ||
| PEG 8000 A-0.25 h | 0.5 ± 0.2 (3) | — | — | 1.3 ± 0.1 (2) | 1.5 ± 0.2 (3) | ||
| PEG 8000 A-1 h | — | — | — | — | 1.5 ± 0.2 (3) | ||
| Interferon | Rp | No addition | — | 3.9 ± 2.9 (11) | 41.9 ± 3.8 (6) | 55.2 ± 5.2 (16) | 58.1 ± 8.8 (13) |
| PEG 1450 | — | 2.7 ± 1.1 (4) | 37.2 ± 3.2 (4) | 52.3 ± 5.0 (4) | 59.8 ± 10.0 (4) | ||
| PEG 2000 | — | 2.9 ± 2.0 (4) | 44.5 ± 0.9 (4) | 59.1 ± 8.0 (4) | 65.7 ± 14.1 (4) | ||
| PEG 4000 | — | 1.0 ± 1.2 (6) | 18.1 ± 2.4 (6) | 30.9 ± 2.1 (6) | 35.9 ± 4.7 (6) | ||
| PEG 4000 A-1 h | — | — | 16.9 ± 2.1 (2) | 23.5 ± 2.7 (2) | 26.0 ± 3.4 (2) | ||
| PEG 8000 | — | 2.3 ± 0.4 (4) | 3.2 ± 0.8 (4) | 4.6 ± 1.0 (16) | 5.3 ± 1.7 (15) | ||
| PEG 8000 A-0.25 h | 0.5 ± 0.2 (3) | — | — | 4.8 ± 0.8 (2) | 2.8 ± 0.2 (3) | ||
| PEG 8000 A-1 h | — | — | — | — | 3.0 ± 0.2 (3) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Turco, J. Involvement of Pore Formation and Osmotic Lysis in the Rapid Killing of Gamma Interferon-Pretreated C166 Endothelial Cells by Rickettsia prowazekii. Trop. Med. Infect. Dis. 2022, 7, 163. https://doi.org/10.3390/tropicalmed7080163
Turco J. Involvement of Pore Formation and Osmotic Lysis in the Rapid Killing of Gamma Interferon-Pretreated C166 Endothelial Cells by Rickettsia prowazekii. Tropical Medicine and Infectious Disease. 2022; 7(8):163. https://doi.org/10.3390/tropicalmed7080163
Chicago/Turabian StyleTurco, Jenifer. 2022. "Involvement of Pore Formation and Osmotic Lysis in the Rapid Killing of Gamma Interferon-Pretreated C166 Endothelial Cells by Rickettsia prowazekii" Tropical Medicine and Infectious Disease 7, no. 8: 163. https://doi.org/10.3390/tropicalmed7080163
APA StyleTurco, J. (2022). Involvement of Pore Formation and Osmotic Lysis in the Rapid Killing of Gamma Interferon-Pretreated C166 Endothelial Cells by Rickettsia prowazekii. Tropical Medicine and Infectious Disease, 7(8), 163. https://doi.org/10.3390/tropicalmed7080163





