COVID-19 Amongst Travelers at Points of Entry in Nepal: Screening, Testing, Diagnosis and Isolation Practices
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
2.2.1. General Setting
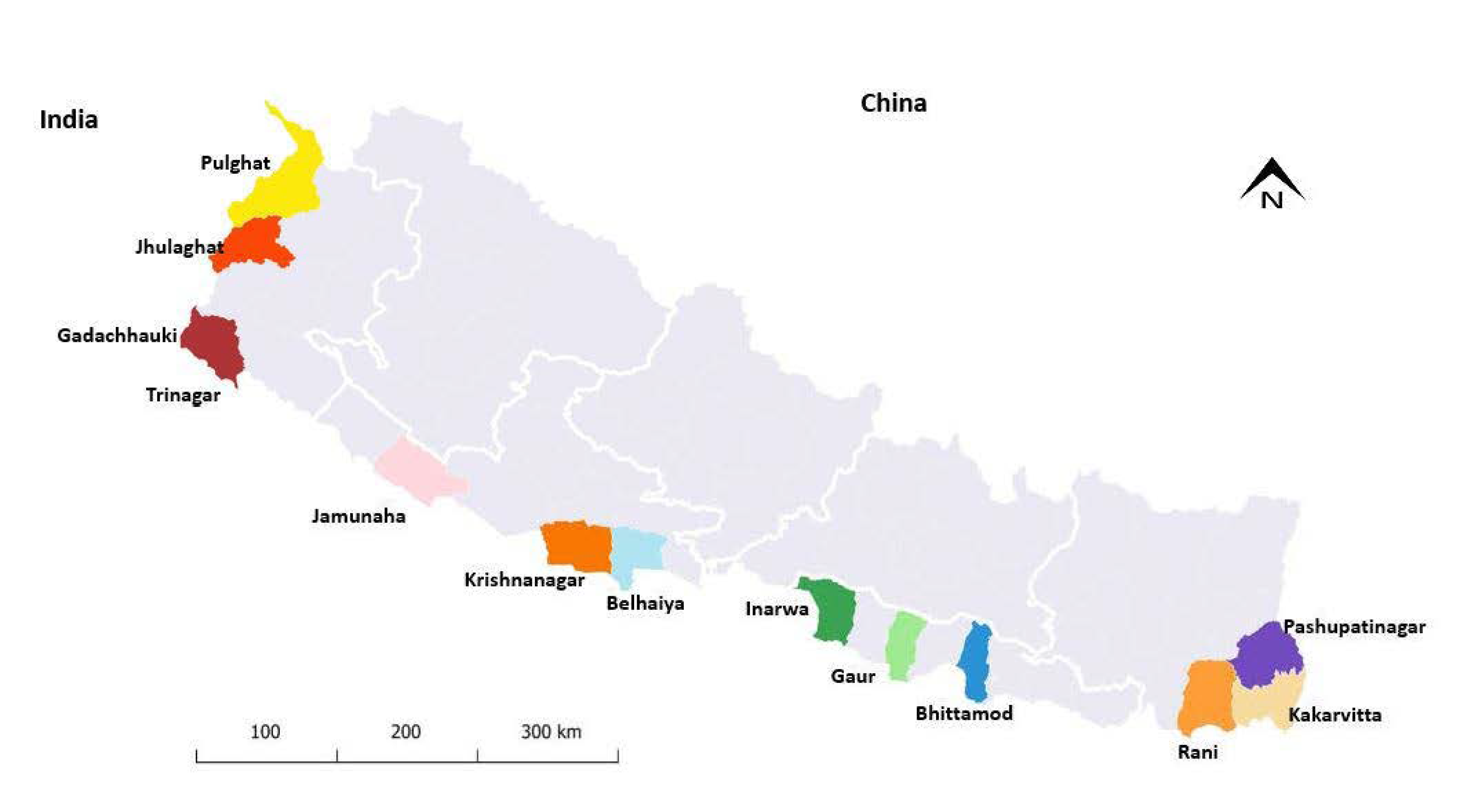
2.2.2. Specific Setting (POE)
2.2.3. Lateral Flow Antigen (LFA) Test
2.2.4. Screening and Testing Procedure and Practice
2.2.5. Isolation Procedure of Positive COVID-19 Patients
2.3. Study Population and Time Period
2.4. Data Variables, Data Sources, Data Collection and Validation
2.5. Analysis and Statistics
3. Results
3.1. Travelers Screened, Tested and Diagnosed at POE during the Study Period
3.2. Trends in Screening, Testing and Diagnosis at POE during the Study Period
3.3. Characteristics of Travelers Testing Positive for COVID-19
3.4. Types of Isolation for Travelers with COVID-19
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Open Access Statement and Disclaimer
References
- World Health Organization. Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 21 September 2021).
- Dickens, B.L.; Koo, J.R.; Tao Lim, J.; Sun, H.; Clapham, H.E.; Wilder-Smith, A.; Cook, A.R. Strategies at Points of Entry to Reduce Importation Risk of COVID-19 Cases and Reopen Travel. J. Travel Med. 2020, 27, 1–8. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Technical Considerations for Implementing a Risk-Based Approach to International Travel in the Context of COVID-19. Interim Guidance Annex to: Policy Considerations for Implementing; World Health Organization: Geneva, Switzerland, 2021; pp. 1–14. [Google Scholar]
- World Health Organization. COVID-19 Strategic Preparedness and Response Plan; World Health Organization: Geneva, Switzerland, 2021; p. 14. [Google Scholar]
- Mahmoudinobar, F.; Britton, D.; Montclare, J.K. Protein-Based Lateral Flow Assays for COVID-19 Detection. Protein Eng. Des. Sel. 2021, 34, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Trombetta, B.A.; Kandigian, S.E.; Kitchen, R.R.; Grauwet, K.; Webb, P.K.; Miller, G.A.; Jennings, C.G.; Jain, S.; Miller, S.; Kuo, Y.; et al. Evaluation of Serological Lateral Flow Assays for Severe Acute Respiratory Syndrome Coronavirus-2. BMC Infect. Dis. 2021, 21, 580. [Google Scholar] [CrossRef] [PubMed]
- Peeling, R.W.; Heymann, D.L.; Teo, Y.Y.; Garcia, P.J. Diagnostics for COVID-19: Moving from Pandemic Response to Control. Lancet 2022, 399, 757–768. [Google Scholar] [CrossRef]
- Bastola, A.; Sah, R.; Morales, A.J.R.; Lal, B.K.; Jha, R.; Ojha, H.C.; Shrestha, B.; Chu, D.K.W.; Poon, L.L.M.; Costello, A.; et al. The First 2019 Novel Coronavirus Case in Nepal. Lancet Infect. Dis. 2020, 20, 279–280. [Google Scholar] [CrossRef] [Green Version]
- Epidemiology and Disease Control Division, Nepal. COVID-19 Statistics: Nepal. Available online: https://portal.edcd.gov.np/covid19/ (accessed on 21 March 2022).
- Ministry of Health and Population. Health Sector Response to COVID-19 Pandemic in Nepal; Ministry of Health and Population: Kathmandu, Nepal, 2022; pp. 13–14. [Google Scholar]
- Ministry of Health and Population, Nepal. Corona Virus Disease (COVID-19) Outbreak Updates and Resource Materials, Situation Report 399 and 691. Available online: https://heoc.mohp.gov.np/ (accessed on 3 June 2022).
- Seddon, D. India and Nepal in COVID-19 Crisis Together. Available online: https://www.nepalitimes.com/latest/india-and-nepal-in-Covid-19-crisis-together/ (accessed on 25 September 2020).
- Central Bureau of Statistics. Nepal Population and Housing Census 2011, National Report; Central Bureau of Statistics: Kathmandu, Nepal, 2012. [Google Scholar]
- Ministry of Health and Population. Document on Standards for Health Examination Centre at Entry Point( Land Crossings); Ministry of Health and Population: Kathmandu, Nepal, 2020. [Google Scholar]
- National Public Health Laboratory, Nepal. List of Approved COVID-19 Antigen Kits. Available online: https://nphl.gov.np/covid19/antigen-kits/ (accessed on 23 September 2021).
- Ministry of Health and Population. Health Standard for Isolation of COVID-19 Cases; Ministry of Health and Population: Kathmandu, Nepal, 2020. [Google Scholar]
- Lokossou, V.K.; Usman, A.B.; Sombie, I.; Paraiso, M.N.; Balogun, M.S.; Umeokonkwo, C.D.; Gatua, J.; Wagai, J.; Ouendo, E.M.; Nguku, P. COVID-19 Pandemic in Economic Community of West African States (Ecowas) Region: Implication for Capacity Strengthening at Point of Entry. Pan Afr. Med. J. 2021, 39. [Google Scholar] [CrossRef] [PubMed]
- Meesit, A.; Kaewla, W.; Wiwanikit, V. Forgotten Problems in Land Border Crossings. Ann. Trop. Med. Public Health. 2016, 9, 130. [Google Scholar] [CrossRef]
- Rooij, D.D.; Belfroid, E.; Hadjichristodoulou, C.; Mouchtouri, V.A.; Raab, J.; Timen, A. Assessing Training Needs in Infectious Disease Management at Major Ports, Airports and Ground-Crossings in Europe. BMC Public Health 2021, 21, 1013. [Google Scholar] [CrossRef] [PubMed]
- Klinger, C.; Burns, J.; Movsisyan, A.; Biallas, R.; Norris, S.L.; Rabe, J.E.; Stratil, J.M.; Voss, S.; Wabnitz, K.; Rehfuess, E.A.; et al. Unintended Health and Societal Consequences of International Travel Measures during the COVID-19 Pandemic: A Scoping Review. J. Travel Med. 2021, 28, taab123. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases from the Chinese Center for Disease Control and Prevention. JAMA J. Am. Med. Assoc. 2020, 323, 1239–1242. [Google Scholar] [CrossRef] [PubMed]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; Cohen, S.L.; et al. Presenting Characteristics, Comorbidities, and Outcomes among 5700 Patients Hospitalized with COVID-19 in the New York City Area. JAMA J. Am. Med. Assoc. 2020, 323, 2052–2059. [Google Scholar] [CrossRef] [PubMed]
- Koh, H.K.; Geller, A.C.; Vanderweele, T.J. Deaths from COVID-19. JAMA J. Am. Med. Assoc. 2021, 325, 133–134. [Google Scholar] [CrossRef] [PubMed]
- Elm, E.V.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [Green Version]
- Wirawan, I.M.A.; Sutarsa, I.N.; Astuti, P.A.S. Healthy Tourism Initiative in the Age of COVID-19 in Indonesia. Asian Pac. J. Trop. Med. 2021, 14, 381–382. [Google Scholar] [CrossRef]
- Yamano, T.; Pradhananga, M.; Schipani, S.; Samson, J.N.G.; Quiao, L.; Leuangkhamsing, S.; Maddawin, A. The Impact of COVID-19 on Tourism Enterprises in the Lao People’s Democratic Republic: An initial Assessment; Asian Development Bank: Mandaluyong, Philippines, 2020. [Google Scholar]
- Abbas, J.; Mubeen, R.; Iorember, P.T.; Raza, S.; Mamirkulova, G. Exploring the Impact of COVID-19 on Tourism: Transformational Potential and Implications for a Sustainable Recovery of the Travel and Leisure Industry. Curr. Res. Behav. Sci. 2021, 2, 100033. [Google Scholar] [CrossRef]


| Designated POE | Screened n | Tested n (%) | COVID-19 Positive n (%) | ||
|---|---|---|---|---|---|
| Total | 337,338 | 69,886 | (21) | 3907 | (6) |
| Belahiya | 25,595 | 5467 | (19) | 124 | (2) |
| Gaddachauki | 39,571 | 15,611 | (40) | 116 | (1) |
| Gaur | 3385 | 602 | (18) | 13 | (2) |
| Inarwa | 12,981 | 3628 | (28) | 368 | (10) |
| Jamunaha | 132,378 | 9642 | (7) | 366 | (4) |
| Jhulaghat | 1820 | 1799 | (99) | 107 | (6) |
| Kakarbhitta | 24,135 | 2864 | (12) | 129 | (5) |
| Krishnanagar | 19,572 | 946 | (5) | 128 | (14) |
| Pashupatinagar | 1528 | 75 | (5) | 2 | (3) |
| Pulghat | 973 | 466 | (48) | 1 | (<1) |
| Rani | 2450 | 969 | (40) | 86 | (9) |
| Trinagar | 66,927 | 27,817 | (42) | 2467 | (9) |
| Bhittamod | 2023 | 0 | (0) | - | - |
| Characteristics of COVID-19 Patients | n | (%) | |
|---|---|---|---|
| Total | 3907 | ||
| Socio-demographic characteristics | |||
| Age in years | 1–5 | 21 | (1) |
| 6–14 | 91 | (2) | |
| 15–29 | 2014 | (52) | |
| 30–44 | 1192 | (30) | |
| 45–59 | 438 | (11) | |
| 60 and above | 151 | (4) | |
| Gender | Male | 3331 | (85) |
| Female | 576 | (15) | |
| Occupation | Unemployed | 37 | (1) |
| Employed | 129 | (3) | |
| Migrant worker | 3100 | (79) | |
| Health worker | 50 | (1) | |
| Security person | 28 | (1) | |
| Student | 255 | (7) | |
| Business/Trade | 13 | (<1) | |
| Others * | 20 | (1) | |
| Not recorded | 275 | (7) | |
| Nationality | Nepalese | 3749 | (96) |
| Indian | 158 | (4) | |
| Clinical characteristics | |||
| Symptoms | Cough/Sore throat | 214 | (6) |
| Fever | 3693 | (95) | |
| Other COVID-19 symptoms * | 72 | (2) | |
| Points of Entry | Total Number Diagnosed with COVID-19 | Home-Based Isolation n (%) | Community-Based Isolation n (%) | Hospital-Based Isolation n (%) | Returned to INDIA n (%) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Total | 3907 | 1261 | (32) | 2501 | (64) | 65 | (2) | 80 | (2) |
| Belahiya | 124 | 117 | (94) | 7 | (6) | 0 | (0) | 0 | (0) |
| Gaddachauki | 116 | 3 | (3) | 113 | (97) | 0 | (0) | 0 | (0) |
| Gaur | 13 | 0 | (0) | 13 | (100) | 0 | (0) | 0 | (0) |
| Inarwa | 368 | 271 | (74) | 15 | (4) | 2 | (1) | 80 | (21) |
| Jamunaha | 366 | 164 | (45) | 151 | (41) | 51 | (14) | 0 | (0) |
| Jhulaghat | 107 | 46 | (43) | 60 | (56) | 1 | (1) | 0 | (0) |
| Kakarbhitta | 129 | 126 | (98) | 0 | (0) | 3 | (2) | 0 | (0) |
| Krishnanagar | 128 | 120 | (94) | 0 | (0) | 8 | (6.3) | 0 | (0) |
| Pashupatinagar | 2 | 0 | (0) | 2 | (100) | 0 | (0) | 0 | (0) |
| Pulghat | 1 | 0 | (0) | 1 | (100) | 0 | (0) | 0 | (0) |
| Rani | 86 | 86 | (100) | 0 | (0) | 0 | (0) | 0 | (0) |
| Trinagar | 2467 | 328 | (13) | 2139 | (87) | 0 | (0) | 0 | (0) |
| Bhittamod | 0 | 0 | (0) | 0 | (0) | 0 | (0) | 0 | (0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Subedee, K.C.; Paudel, K.P.; Khogali, M.; Pokhrel, A.; Chinnakali, P.; Thakur, N.; Timsina, D.; Gautam, R.; Rahman, A.; Mandal, S.K.; et al. COVID-19 Amongst Travelers at Points of Entry in Nepal: Screening, Testing, Diagnosis and Isolation Practices. Trop. Med. Infect. Dis. 2022, 7, 99. https://doi.org/10.3390/tropicalmed7060099
Subedee KC, Paudel KP, Khogali M, Pokhrel A, Chinnakali P, Thakur N, Timsina D, Gautam R, Rahman A, Mandal SK, et al. COVID-19 Amongst Travelers at Points of Entry in Nepal: Screening, Testing, Diagnosis and Isolation Practices. Tropical Medicine and Infectious Disease. 2022; 7(6):99. https://doi.org/10.3390/tropicalmed7060099
Chicago/Turabian StyleSubedee, Koshal Chandra, Krishna Prasad Paudel, Mohammed Khogali, Amrit Pokhrel, Palanivel Chinnakali, Nishant Thakur, Deepak Timsina, Rabin Gautam, Anisur Rahman, Shrawan Kumar Mandal, and et al. 2022. "COVID-19 Amongst Travelers at Points of Entry in Nepal: Screening, Testing, Diagnosis and Isolation Practices" Tropical Medicine and Infectious Disease 7, no. 6: 99. https://doi.org/10.3390/tropicalmed7060099
APA StyleSubedee, K. C., Paudel, K. P., Khogali, M., Pokhrel, A., Chinnakali, P., Thakur, N., Timsina, D., Gautam, R., Rahman, A., Mandal, S. K., Adhikari, M. D., & Harries, A. D. (2022). COVID-19 Amongst Travelers at Points of Entry in Nepal: Screening, Testing, Diagnosis and Isolation Practices. Tropical Medicine and Infectious Disease, 7(6), 99. https://doi.org/10.3390/tropicalmed7060099









