Operational Gaps in Implementing the COVID-19 Case Investigation and Contact Tracing in Madhesh Province of Nepal, May–July 2021
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
2.2.1. General Setting
2.2.2. Specific Setting
2.2.3. The CICT Program
2.3. Study Population and Study Period
2.4. Data Variables and Sources of Data
2.5. Analysis and Statistics
- o
- At least 80% of the cases are investigated within 24 h of reporting.
- o
- 100% of the ‘A forms’ are filled for all cases investigated.
- o
- At least 80% of the contacts are traced and interviewed within 48 h, and 100% of the contacts traced are tested for COVID-19 infection.
- o
- 100% of the ‘B2 forms’ are completed for all contacts traced.
3. Results
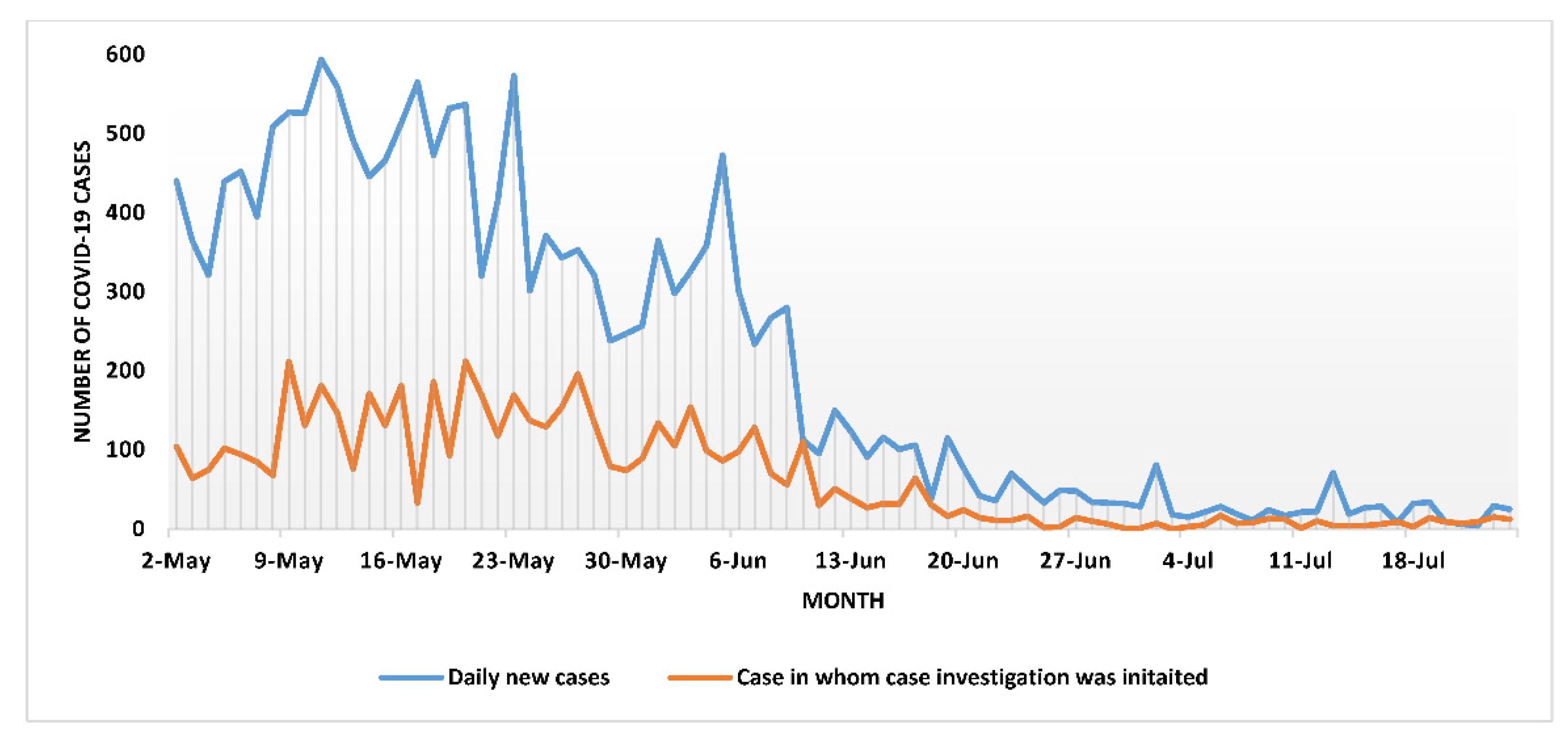
3.1. Case Investigation
3.2. Contact Tracing
3.3. COVID-19 Testing of Contacts
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Disclaimer
References
- Nepal Daily Situation Report of COVID-19 in Nepal. Available online: http://heoc.mohp.gov.np/ (accessed on 22 May 2020).
- Li, Z.; Jones, C.; Ejigu, G.S.; George, N.; Geller, A.L.; Chang, G.C.; Adamski, A.; Igboh, L.S.; Merrill, R.D.; Ricks, P.; et al. Countries with Delayed COVID-19 Introduction-Characteristics, Drivers, Gaps, and Opportunities. Glob. Health 2021, 17, 28. [Google Scholar] [CrossRef] [PubMed]
- Nepal Health Research Council Rapid Assessment of COVID-19 Related Policy Audit in Nepal. Available online: http://nhrc.gov.np/wp-content/uploads/2021/02/Policy-audit-Report-Final-MD.pdf (accessed on 7 June 2022).
- Piryani, R.M.; Piryani, S.; Shah, J.N. Nepal’s Response to Contain COVID-19 Infection. J. Nepal Health Res. Counc. 2020, 18, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Epidemiology and Disease Control Division A Guide to Early Warning and Reporting System (EWARS). Available online: https://www.edcd.gov.np/resources/download/a-guide-to-ewars-2019 (accessed on 7 June 2022).
- Spencer, K.D.; Chung, C.L.; Stargel, A.; Shultz, A.; Thorpe, P.G. COVID-19 Case Investigation and Contact Tracing Efforts from Health Departments-United States, June 25–July 24, 2020. Morb. Mortal. Wkly. Rep. 2021, 70, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Keeling, M.J.; Hollingsworth, T.D.; Read, J.M. Efficacy of Contact Tracing for the Containment of the 2019 Novel Coronavirus (COVID-19). J. Epidemiol. Community Health 2020, 74, 861–866. [Google Scholar] [CrossRef] [PubMed]
- Center for Disease Control Evaluating Case Investigation and Contact Tracing Success. Available online: https://www.cdc.gov/coronavirus/2019-ncov/php/contact-tracing/contact-tracing-plan/evaluating-success.html (accessed on 7 June 2022).
- Vogt, F.; Kurup, K.K.; Mussleman, P.; Habrun, C.; Crowe, M.; Woodward, A.; Jaramillo-gutierrez, G.; Kaldor, J.; Vong, S.; Vilas, R. Contact Tracing Indicators for COVID-19: Rapid Scoping Review and Conceptual Framework. PLoS ONE 2022, 17, e0264433. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, N.; Bhatt, B.; Gurung, S.; Dahal, S.; Jaishi, A.R.; Neupane, B.; Budhathoki, S.S. Perceptions and Experiences of the Public Regarding the COVID-19 Pandemic in Nepal: A Qualitative Study Using Phenomenological Analysis. BMJ Open 2020, 10, e043312. [Google Scholar] [CrossRef] [PubMed]
- Lash, R.R.; Moonan, P.K.; Byers, B.L.; Bonacci, R.A.; Bonner, K.E.; Donahue, M. COVID-19 Case Investigation and Contact Tracing in the US. JAMA Netw. Open 2021, 4, e2115850. [Google Scholar] [CrossRef] [PubMed]
- Awale, S. Kathmandu Locks Down Again. 2020. Available online: https://www.nepalitimes.com/latest/kathmandu-locks-down-again/ (accessed on 7 June 2022).
- Koetter, P.; Pelton, M.; Gonzalo, J.; Du, P.; Bogale, K.; Buzzelli, L.; Connolly, M.; Katelyn Edel, A.H.; Nicole, R.; Legro, D.M.; et al. Implementation and Process of a COVID-19 Contact Tracing Initiative: Leveraging Health Professional Students to Extend the Workforce During a Pandemic. Am. J. Infect. Control 2020, 48, 1451–1456. [Google Scholar] [CrossRef] [PubMed]
- Kretzschmar, M.E.; Rozhnova, G.; Bootsma, M.C.J.; van Boven, M.; van de Wijgert, B. Impact of Delays on Effectiveness of Contact Tracing Strategies for COVID-19: A Modelling Study. Lancet Public Health 2020, 5, e452–e459. [Google Scholar] [CrossRef]
- Eyawo, O.; Viens, A.M. Lockdowns and Low- and Middle-Income Countries: Building a Feasible, Effective, and Ethical COVID-19 Response Strategy. Glob. Health 2021, 17, 13. [Google Scholar] [CrossRef] [PubMed]
- Lewis, D. Why Many Countries Failed at COVID Contact-Tracing--but Some Got It Right. Nature 2020, 588, 384–387. [Google Scholar] [CrossRef] [PubMed]

| Districts | Reported Cumulative Cases | Average Daily Caseload (Range) | Case Investigation Initiated within 24 h * % (95% CI) | Case Investigation Completed % (95% CI) ** |
|---|---|---|---|---|
| Overall (Madhesh Province) | 17,943 | 213 (5–605) | 30.3 (29.6–31.0) | 18.2 (17.7–18.8) |
| Dhanusha | 5307 | 63 (0–218) | 40.6 (39.2–41.9) | 34.1 (32.8–35.4) |
| Mahottari | 2566 | 30 (0–112) | 50.0 (48.1–52.0) | 12.8 (11.6–14.2) |
| Parsa | 2400 | 29 (0–163) | 20.8 (19.1–22.4) | 4.5 (3.8–5.4) |
| Bara | 1952 | 23 (0–236) | 12.6 (11.2–14.2) | 4.2 (3.4–5.2) |
| Saptari | 1888 | 11 (0–119) | 18.4 (16.6–20.2) | 9.1 (7.8–10.4) |
| Siraha | 1580 | 19 (0–92) | 9.5 (8.1–11.0) | 9.2 (7.8–10.7) |
| Rautahat | 1277 | 15 (0–93) | 44.4 (41.6–47.1) | 40.2 (37.5–42.9) |
| Sarlahi | 973 | 12 (0–73) | 20.3 (17.9–23.1) | 11.8 (9.8–14.0) |
| Districts | Contacts Identified | Average Contacts Per 10 Cases Investigated | Average Daily Contact Load | Contacts Tested % (95% CI) | Positivity Rate among Contacts Tested % (95% CI) | Contact Assessments Completed * % (95% CI) |
|---|---|---|---|---|---|---|
| Overall (Province 2) | 6067 | 3 | 73 | 40 (38.7–41.2) | 64 (62.7–65.2) | 14 (13.1–14.9) |
| Dhanusha | 2592 | 5 | 31 | 19 (17.4–20.5) | 50 (48.0–51.9) | 7 (6.0–7.9) |
| Mahottari | 466 | 2 | 6 | 100 | 59 (54.5–63.4) | 14 (10.9–17.1) |
| Parsa # | 1200 | 5 | 14 | 38 (35.2–40.7) | 100 | 9 (7.3–10.6) |
| Bara | 382 | 2 | 5 | 36 (31.9–40.8) | 27 (22.5–31.4) | 0 |
| Saptari $ | 364 | 2 | 4 | - | - | 33 (28.1–37.8) |
| Siraha | 137 | 1 | 2 | 16 (9.8–22.1) | 73 (65.5–80.4) | 39 (30.8–47.1) |
| Rautahat | 794 | 7 | 10 | 16 (13.4–18.5) | 91 (89.0–92.9) | 24 (21.0–26.9) |
| Sarlahi | 132 | 1 | 2 | 54 (45.5–62.5) | 45 (36.5–53.4) | 97 (94.0–99.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thakur, N.; Vogt, F.; Satyanarayana, S.; Nair, D.; Garu, K.; Subedee, K.C.; Mandal, S.K.; Pokhrel, A.; Gautam, D.; Paudel, K.P. Operational Gaps in Implementing the COVID-19 Case Investigation and Contact Tracing in Madhesh Province of Nepal, May–July 2021. Trop. Med. Infect. Dis. 2022, 7, 98. https://doi.org/10.3390/tropicalmed7060098
Thakur N, Vogt F, Satyanarayana S, Nair D, Garu K, Subedee KC, Mandal SK, Pokhrel A, Gautam D, Paudel KP. Operational Gaps in Implementing the COVID-19 Case Investigation and Contact Tracing in Madhesh Province of Nepal, May–July 2021. Tropical Medicine and Infectious Disease. 2022; 7(6):98. https://doi.org/10.3390/tropicalmed7060098
Chicago/Turabian StyleThakur, Nishant, Florian Vogt, Srinath Satyanarayana, Divya Nair, Krishna Garu, Koshal Chandra Subedee, Shrawan Kumar Mandal, Amrit Pokhrel, Dipendra Gautam, and Krishna Prasad Paudel. 2022. "Operational Gaps in Implementing the COVID-19 Case Investigation and Contact Tracing in Madhesh Province of Nepal, May–July 2021" Tropical Medicine and Infectious Disease 7, no. 6: 98. https://doi.org/10.3390/tropicalmed7060098
APA StyleThakur, N., Vogt, F., Satyanarayana, S., Nair, D., Garu, K., Subedee, K. C., Mandal, S. K., Pokhrel, A., Gautam, D., & Paudel, K. P. (2022). Operational Gaps in Implementing the COVID-19 Case Investigation and Contact Tracing in Madhesh Province of Nepal, May–July 2021. Tropical Medicine and Infectious Disease, 7(6), 98. https://doi.org/10.3390/tropicalmed7060098








