Depriving Out-of-School Children of Deworming Tablets for Soil-Transmitted Helminth Infection in Bangladesh: The Irony of a School-Based Deworming Programme
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Site and Target Population
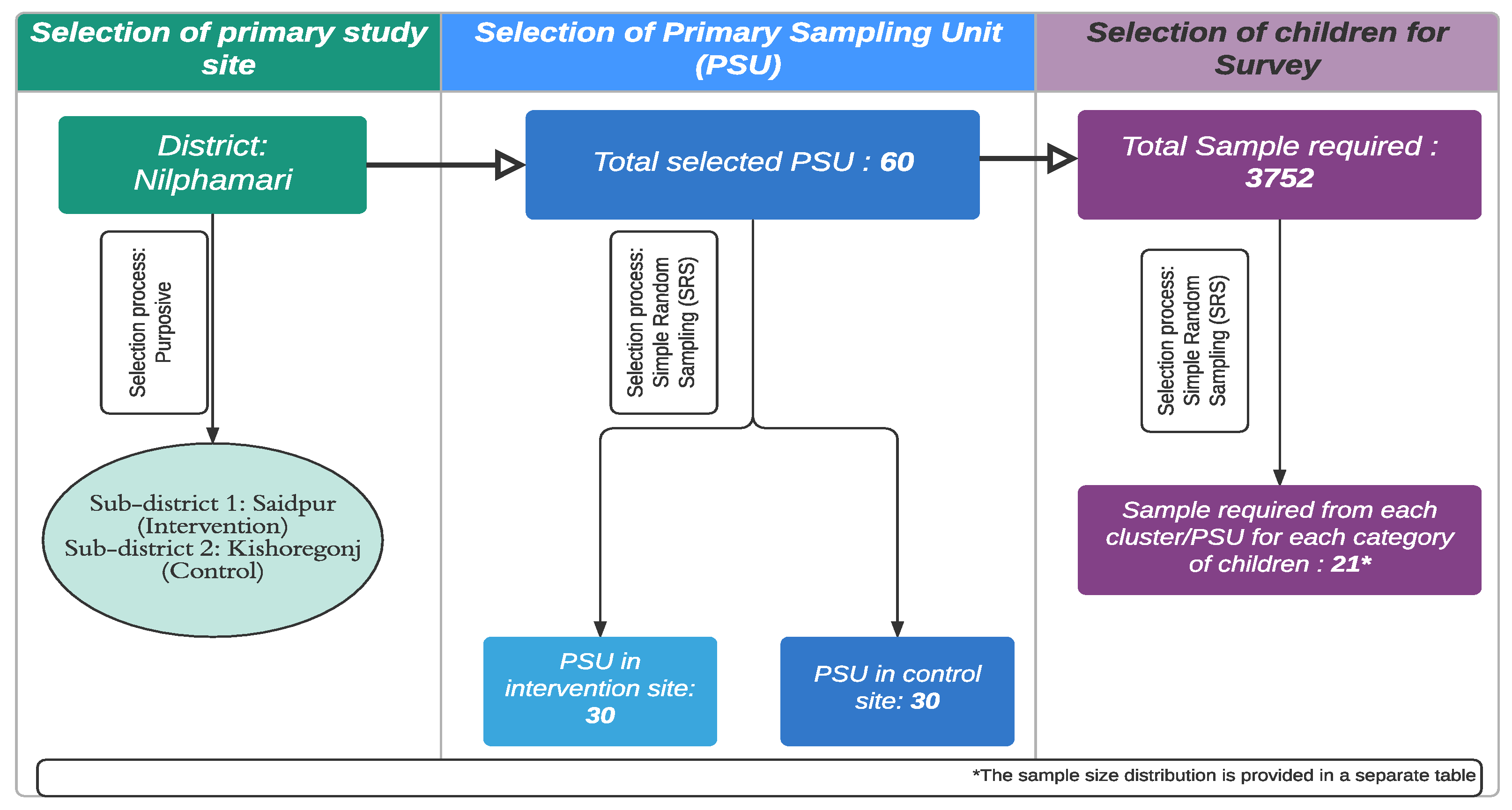
2.3. Sampling Strategy
2.4. Sample Size Calculation
2.5. Data Collection and Analysis
2.6. Ethics Statement and Consent Procedures
3. Results
3.1. Demographic Information of the Target Children and Their Caregivers
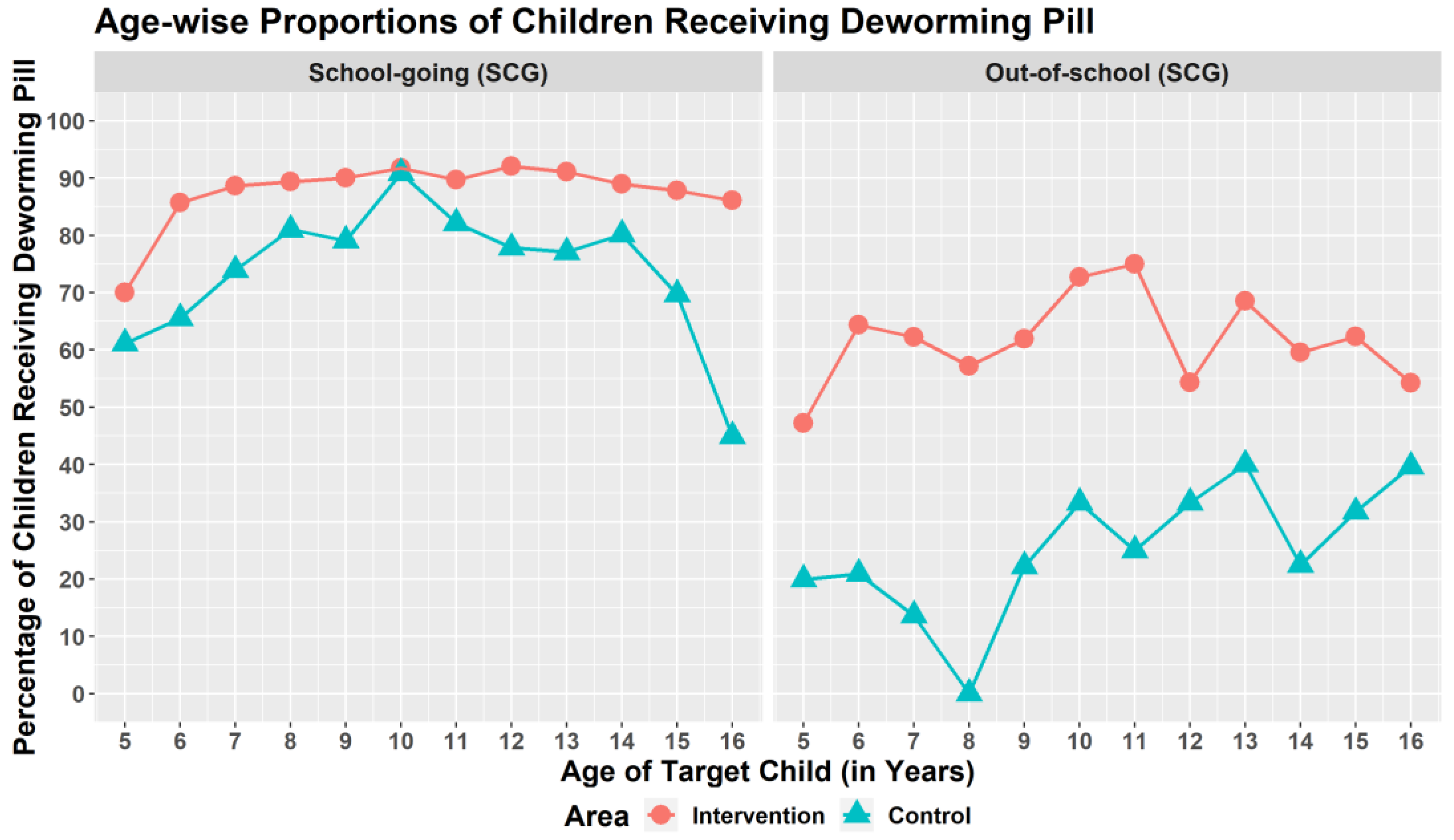
3.2. Self-Reported Deworming Coverage among the SACs
3.3. Knowledge Assessment of the SACs and Their Primary Caregivers
3.4. Assessment of Caregiver’s Knowledge about Deworming Project Activities
3.5. Factors Associated with the Deworming Coverage of the SACs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Kyu, H.H.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1859–1922. Available online: https://linkinghub.elsevier.com/retrieve/pii/S0140673618323353 (accessed on 23 October 2021). [CrossRef] [Green Version]
- Croke, K.; Atun, R. The long run impact of early childhood deworming on numeracy and literacy: Evidence from Uganda. PLoS Negl. Trop. Dis. 2019, 13, e0007085. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahman, M.M. Biannually School Based Deworming by Mebendazole 500mg has Reduced the Worm Load Drastically in Bangladesh. EC Bacteriol. Virol. Res. 2016, 2113, 2113–2114. [Google Scholar] [CrossRef]
- World Health Organization. Guideline: Preventive Chemotherapy to Control Soil-Transmitted Helminth Infections in At-Risk Population Groups. World Health Organization. 2017. Available online: https://apps.who.int/iris/handle/10665/258983 (accessed on 14 November 2021).
- Benjamin-Chung, J.; Nazneen, A.; Halder, A.K.; Haque, R.; Siddique, A.; Uddin, M.S.; Koporc, K.; Arnold, B.F.; Hubbard, A.E.; Unicomb, L.; et al. The Interaction of Deworming, Improved Sanitation, and Household Flooring with Soil-Transmitted Helminth Infection in Rural Bangladesh. PLoS Negl. Trop. Dis. 2015, 9, e0004256. [Google Scholar] [CrossRef] [Green Version]
- MOHFW. Neglected Tropical Diseases in Bangladesh: Situation Analysis and Gap Analysis. Dhaka, Bangladesh [Internet]. 2011 December. Available online: https://pdf.usaid.gov/pdf_docs/pnady849.pdf (accessed on 23 October 2021).
- Dhakal, S.; Karim, M.J.; Al Kawsar, A.; Irish, J.; Rahman, M.; Tupps, C.; Kabir, A.; Imtiaz, R. Post-intervention epidemiology of STH in Bangladesh: Data to sustain the gains. PLoS Negl. Trop. Dis. 2020, 14, e0008597. Available online: https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0008597 (accessed on 14 November 2021). [CrossRef]
- Control of Neglected Tropical Diseases. Available online: https://www.who.int/teams/control-of-neglected-tropical-diseases (accessed on 14 November 2021).
- Nath, T.C.; Padmawati, R.S.; Murhandarwati, E.H. Barriers and gaps in utilization and coverage of mass drug administration program against soil-transmitted helminth infection in Bangladesh: An implementation research. J. Infect. Public Health 2019, 12, 205–212. Available online: https://pubmed.ncbi.nlm.nih.gov/30385237/ (accessed on 14 November 2021). [CrossRef]
- UNICEF. BANGLADESH EDUCATION FACT SHEETS 2020—UNICEF. 2020. Available online: https://www.google.com/search?client=safari&rls=en&q=BANGLADESH+EDUCATION+FACT+SHEETS+2020+-+UNICEF&ie=UTF-8&oe=UTF-8 (accessed on 5 January 2022).
- FHI: 360. Technical Brief: Assessing Progress in Fighting STHs in Bangladesh|FHI 360. 2013. Available online: https://www.fhi360.org/resource/technical-brief-assessing-progress-fighting-sths-bangladesh (accessed on 14 November 2021).
- Hafiz, I.; Berhan, M.; Keller, A.; Haq, R.; Chesnaye, N.; Koporc, K.; Rahman, M.; Rahman, S.; Mathieu, E. School-based mass distributions of mebendazole to control soil-transmitted helminthiasis in the Munshiganj and Lakshmipur districts of Bangladesh: An evaluation of the treatment monitoring process and knowledge, attitudes, and practices of the population. Acta Trop. 2015, 141, 385–390. Available online: https://pubmed.ncbi.nlm.nih.gov/24370675/ (accessed on 14 November 2021). [CrossRef] [PubMed]
- WHO. Helminth Control in School-Age Children: A Guide for Managers of Control Programmes. 2002. Available online: https://apps.who.int/iris/handle/10665/44671 (accessed on 14 November 2021).
- Asfaw, M.A.; Hailu, C.; Beyene, T.J. Evaluating Equity and Coverage in Mass Drug Administration for Soil-Transmitted Helminth Infections among School-Age Children in the Hard-to-Reach Setting of Southern Ethiopia. Pediatric Health Med. Ther. 2021, 12, 325–333. Available online: https://pubmed.ncbi.nlm.nih.gov/34267576/ (accessed on 14 November 2021). [CrossRef] [PubMed]
- Hotez, P.J.; Fenwick, A.; Savioli, L.; Molyneux, D.H. Rescuing the bottom billion through control of neglected tropical diseases. Lancet 2009, 373, 1570–1575. Available online: http://www.globalnetwork.org (accessed on 14 November 2021). [CrossRef]
- Rahman, M.R.; Akther, F. Evaluation of the “Cluster Village” Projects: A Case Study on Four Cluster Village Projects of Nilphamari District. In The Jahangirnagar Review, Part II: Social Sciences; Jahangirnagar University: Dhaka, Bangladesh, 2017; Volume XLI, Available online: https://www.researchgate.net/publication/344947976 (accessed on 14 November 2021).
- Creswell, J.W.; Clark, V.L.P. Designing and Conducting Mixed Methods Research, 3rd ed.; Sage Publications: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Demo-Equity Tool. Available online: https://www.equitytool.org/demo/ (accessed on 27 December 2021).
- Weerasooriya, M.V.; Yahathugoda, C.T.; Wickramasinghe, D.; Gunawardena, K.N.; Dharmadasa, R.A.; Vidanapathirana, K.K.; Weerasekara, S.H.; Samarawickrema, W.A. Social mobilisation, drug coverage and compliance and adverse reactions in a Mass Drug Administration (MDA) Programme for the Elimination of Lymphatic Filariasis in Sri Lanka. Filaria J. 2007, 6, 11. Available online: https://pubmed.ncbi.nlm.nih.gov/18005398/ (accessed on 15 November 2021). [CrossRef] [Green Version]
- Fraser, M.; Taleo, G.; Taleo, F.; Yaviong, J.; Amos, M.; Babu, M.; Kalkoa, M. Evaluation of the program to eliminate lymphatic filariasis in Vanuatu following two years of mass drug administration implementation: Results and methodologic approach. Am. J. Trop. Med. Hyg. 2005, 73, 753–758. [Google Scholar] [CrossRef] [PubMed]
- Stolk, W.A.; de Vlas, S.J.; Borsboom, G.J.J.M.; Habbema, J.D.F. LYMFASIM, a simulation model for predicting the impact of lymphatic filariasis control: Quantification for African villages. Parasitology 2008, 135, 1583–1598. Available online: https://pubmed.ncbi.nlm.nih.gov/19006602/ (accessed on 15 November 2021). [CrossRef] [PubMed] [Green Version]
- Gyorkos, T.W.; Maheu-Giroux, M.; Blouin, B.; Casapia, M. Impact of Health Education on Soil-Transmitted Helminth Infections in Schoolchildren of the Peruvian Amazon: A Cluster-Randomized Controlled Trial. PLoS Negl. Trop. Dis. 2013, 7, e2397. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3772033/ (accessed on 15 November 2021). [CrossRef] [PubMed]
- Midzi, N.; Mtapuri-Zinyowera, S.; Mapingure, M.P.; Paul, N.H.; Sangweme, D.; Hlerema, G.; Mutsaka, M.J.; Tongogara, F.; Makware, G.; Chadukura, V.; et al. Knowledge attitudes and practices of grade three primary schoolchildren in relation to schistosomiasis, soil transmitted helminthiasis and malaria in Zimbabwe. BMC Infect. Dis. 2011, 11, 169. Available online: https://bmcinfectdis.biomedcentral.com/articles/10.1186/1471-2334-11-169 (accessed on 15 November 2021). [CrossRef] [PubMed] [Green Version]
- Mazigo, H.D.; Waihenya, R.; Mkoji, G.M.; Zinga, M.; Ambrose, E.E.; Jahanpour, O.F.; Bahemana, E.; Mnyone, L.L.; Kweka, E.J.; Lwambo, N.J. Intestinal schistosomiasis: Prevalence, knowledge, attitude and practices among school children in an endemic area of north western tanzania. J. Rural. Trop. Public Health 2010, 9, 53–60. [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. Parenting Matters: Supporting Parents of Children Ages 0–8; The National Academies Press: Washington, DC, USA, 2016. [Google Scholar] [CrossRef]
- Albonico, M.; Montresor, A.; Crompton, D.W.T.; Savioli, L. Intervention for the control of Soil-transmitted helminthiasis in the community. Adv. Parasitol. 2006, 61, 311. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5633078/ (accessed on 15 November 2021). [PubMed] [Green Version]
- Curtale, F.; Pokhrel, R.P.; Tilden, R.L.; Higashi, G. Intestinal helminths and xerophthalmia in Nepal. A case-control study. J. Trop. Pediatrics 1995, 41, 334–337. Available online: https://pubmed.ncbi.nlm.nih.gov/8606439/ (accessed on 15 November 2021). [CrossRef] [PubMed]
- Khanal, P.; Walgate, R. Nepal deworming programme ready to go worldwide. Bull. World Health Organ. 2002, 80, 423–424. [Google Scholar] [PubMed]
- Babu, B.V.; Babu, G.R. Coverage of, and compliance with, mass drug administration under the programme to eliminate lymphatic filariasis in India: A systematic review. Trans. R. Soc. Trop. Med. Hyg. 2014, 108, 538–549. Available online: https://pubmed.ncbi.nlm.nih.gov/24728444/ (accessed on 15 November 2021). [CrossRef] [PubMed]
| OSCs | SGCs | |||||
|---|---|---|---|---|---|---|
| Selected Study Sites | Saidpur (Intervention) | Kishoregonj (Control) | Saidpur (Intervention) | Kishoregonj (Control) | ||
| Age Strata | 5–16 years | 5–11 years and 12–16 years | ||||
| Number of PSUs | 30 | |||||
| Required Sample Size/Age Group | 617 | 617 | 631 | 628 | 631 | 628 |
| Interviews Conducted | 613 | 598 | 617 | 623 | 623 | 623 |
| Responses | ||||
|---|---|---|---|---|
| Variables | Intervention (N = 1853) | Control (N = 1844) | ||
| SGC (n = 1240) | OSC (n = 613) | SGC (n = 1246) | OSC (n = 598) | |
| Mean Age of the Target Children | ||||
| Mean Age, in years (±SD) | 11 (3.1) | 11 (4.1) | 11 (3.1) | 9 (4.4) |
| Gender of targeted SAC | ||||
| Female | 664 (53.6) | 221 (36.1) | 665 (53.4) | 220 (36.8) |
| Male | 576 (46.5) | 392 (63.9) | 581 (46.6) | 378 (63.2) |
| Mean Age Primary Caregivers * | ||||
| Mean Age, in years (±SD) | 35 (8.2) | 36 (9.4) | 36 (9.2) | 35 (9.9) |
| Gender Primary Caregivers * | ||||
| Female | 1042 (88.2) | 510 (89.3) | 1047 (87.8) | 485 (86.30 |
| Male | 139 (11.8) | 61 (10.7) | 146 (12.2) | 77 (13.7) |
| Relationship of the OSCs to their Primary Caregivers * | ||||
| Parents | 1088 (92.1) | 505 (88.4) | 1060 (88.9) | 490 (87.2) |
| Other Caregivers | 93 (7.9) | 66 (11.6) | 133 (11.1) | 72 (12.8) |
| Wealth status # | ||||
| Poorest | 7 (0.6) | 17 (3.0) | 29 (2.4) | 23 (4.1) |
| Poor | 118 (10.0) | 100 (17.5) | 471 (39.5) | 264 (47.0) |
| Middle | 195 (16.5) | 122 (21.4) | 343 (28.8) | 166 (29.5) |
| Rich | 512 (43.4) | 236 (41.3) | 296 (24.8) | 88 (15.7) |
| Richest | 349 (29.6) | 96 (16.8) | 54 (4.5) | 21 (3.7) |
| SACs (N = 3697) | Caregivers (N = 3507) | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Intervention | Control | Intervention | Control | ||||
| SGC, n = 1240 | OSC, n = 613 | SGC, n = 1246 | OSC, n = 598 | SGC, n = 1181 | OSC, n = 571 | SGC, n = 1193 | OSC, n = 562 | |
| Importance and reason for taking the deworming pill | ||||||||
| Taking the deworming pill is necessary | 970 (78.2) | 374 (61.0) | 964 (77.4) | 344 (57.5) | 1147 (97.1) | 518 (90.7) | 1088 (91.2) | 481 (85.6) |
| Taking the deworming pill will keep them from getting the worm | 916 (73.9) | 330 (53.8) | 843 (67.7) | 291 (48.7) | 1120 (94.8) | 507 (88.8) | 1023 (85.8) | 446 (79.4) |
| Not taking the pill will make them feel sick | 985 (79.4) | 374 (61.0) | 947 (76.0) | 331 (55.4) | 1102 (93.3) | 510 (89.3) | 1067 (89.4) | 485 (86.3) |
| Knowledge about STH infection-related symptoms | ||||||||
| Knows bloating is a symptom | 606 (48.9) | 236 (38.5) | 573 (46.0) | 221 (37.0) | 824 (69.8) | 386 (67.6) | 848 (71.1) | 380 (67.6) |
| Knows vomiting is a symptom | 449 (36.2) | 173 (28.2) | 361 (29.0) | 130 (21.7) | 649 (55.0) | 302 (52.9) | 550 (46.1) | 235 (41.8) |
| Knows lack of appetite is a symptom | 178 (14.4) | 66 (10.8) | 155 (12.4) | 50 (8.4) | 285 (24.1) | 120 (21.0) | 231 (19.4) | 95 (16.9) |
| Knows indigestion is a symptom | 356 (28.7) | 144 (23.5) | 303 (24.3) | 110 (18.4) | 576 (48.8) | 299 (52.4) | 534 (44.8) | 204 (36.3) |
| Knows spitting frequently is a symptom | 364 (29.4) | 133 (21.7) | 384 (30.8) | 141 (23.6) | 529 (44.8) | 251 (44.0) | 562 (47.1) | 230 (40.9) |
| Knows itching in the anus is a symptom | 149 (12) | 60 (9.8) | 194 (15.6) | 80 (13.4) | 300 (25.4) | 125 (21.9) | 356 (29.8) | 157 (27.9) |
| Knows the type of illness caused by STH infection | ||||||||
| Knows it causes malnutrition | 330 (26.6) | 125 (20.4) | 296 (23.8) | 132 (22.1) | 551 (46.7) | 235 (41.2) | 489 (41) | 215 (38.3) |
| Knows it causes anaemia | 135 (10.9) | 52 (8.5) | 148 (11.9) | 57 (9.5) | 235 (19.9) | 95 (16.6) | 224 (18.8) | 95 (16.9) |
| Knows it causes indigestion | 236 (19.0) | 98 (16.0) | 208 (16.7) | 70 (11.7) | 325 (27.5) | 137 (24.0) | 305 (25.6) | 141 (25.1) |
| Knows it causes diarrhoea | 269 (21.7) | 106 (17.3) | 270 (21.7) | 111 (18.6) | 399 (33.8) | 170 (29.8) | 387 (32.4) | 163 (29.0) |
| Knows the pathways of STH transmission | ||||||||
| Eating with dirty hands | 633 (51.0) | 224 (36.5) | 555 (44.5) | 200 (33.4) | 810 (68.6) | 393 (68.8) | 758 (63.5) | 318 (56.6) |
| Not washing hands after defecation | 570 (46.0) | 184 (30.0) | 465 (37.3) | 156 (26.1) | 740 (62.7) | 336 (58.8) | 653 (54.7) | 288 (51.2) |
| Not washing hands before eating food | 319 (25.7) | 111 (18.1) | 263 (21.1) | 85 (14.2) | 424 (35.9) | 176 (30.8) | 389 (32.6) | 148 (26.3) |
| Drinking contaminated water | 93 (7.5) | 28 (4.6) | 75 (6.0) | 21 (3.5) | 122 (10.3) | 42 (7.4) | 92 (7.7) | 37 (6.6) |
| Not wearing shoes | 541 (43.6) | 178 (29.0) | 480 (38.5) | 178 (29.8) | 698 (59.1) | 304 (53.2) | 631 (52.9) | 284 (50.5) |
| Open defecation | 50 (4.0) | 22 (3.6) | 79 (6.3) | 20 (3.3) | 75 (6.4) | 38 (6.7) | 122 (10.2) | 54 (9.6) |
| Variables | Intervention, SCG | Intervention, OSC | Control, SCG | Control, OSC |
|---|---|---|---|---|
| n = 1181 | n = 571 | n = 1193 | n = 562 | |
| Sources that informed caregivers about the importance of the deworming pill | ||||
| Community worker from BRAC | 579 (49.0) | 326 (57.1) | 228 (19.1) | 107 (19.0) |
| Teacher of their child | 313 (26.5) | 31 (5.4) | 272 (22.8) | 49 (8.7) |
| Medical Doctors | 123 (10.4) | 60 (10.5) | 137 (11.5) | 73 (13.0) |
| Through Visual aids/Miking | 91 (7.7) | 30 (5.3) | 83 (7.0) | 27 (4.8) |
| Types of sensitization activity seen before the deworming campaign in the area | ||||
| Miking | 402 (34.0) | 197 (34.5) | 65 (5.4) | 21 (3.7) |
| Household visit by community workers | 278 (23.5) | 161 (28.2) | 29 (2.4) | 14 (2.5) |
| Courtyard meeting with women | 152 (12.9) | 78 (13.7) | 25 (2.1) | 11 (2.0) |
| Courtyard meeting with adolescent girls | 16 (1.4) | 8 (1.4) | - | - |
| Courtyard/Outdoor meeting with men | 23 (1.9) | 4 (0.7) | - | 1 (0.2) |
| In-school programs with children | 38 (3.2) | 4 (0.7) | 7 (0.6) | - |
| Cable TV message | 11 (0.9) | 4 (0.7) | 5 (0.4) | 2 (0.4) |
| Knowledge about the workers seen engaged in household visits in the area | ||||
| Community worker from BRAC | 398 (33.7) | 203 (35.6) | 49 (4.1) | 15 (2.7) |
| Community worker from government | 145 (12.3) | 49 (8.6) | 71 (6.0) | 23 (4.1) |
| Variables | Intervention | Control | ||
|---|---|---|---|---|
| Adjusted Odds Ratio or, AOR (95% Confidence Interval) | p-Value | Adjusted Odds Ratio or, AOR (95% Confidence Interval) | p-Value | |
| Child not going to school | 0.18 (0.14–0.25) | 0.000 *** | 0.12 (0.09–0.15) | 0.000 *** |
| Child’s gender is female | 1.24 (0.93–1.64) | 0.139 | 0.91 (0.72–1.16) | 0.447 |
| Caregiver’s gender is female | 1.07 (0.70–1.64) | 0.743 | 1.37 (0.97–1.94) | 0.073 * |
| Household belongs to 2nd/poor wealth quintal | 0.82 (0.28–2.37) | 0.714 | 0.95 (0.47–1.93) | 0.895 |
| Household belongs to 3rd/middle wealth quintal | 0.67 (0.24–1.90) | 0.453 | 1.12 (0.55–2.30) | 0.751 |
| Household belongs to 4th/rich wealth quintal | 0.75 (0.27–2.08) | 0.579 | 0.90 (0.43–1.86) | 0.77 |
| Household belongs to 5th/richest wealth quintal | 0.84 (0.29–2.42) | 0.751 | 0.96 (0.39–2.37) | 0.923 |
| The child knows taking the deworming pill is important | 0.92 (0.53–1.59) | 0.77 | 1.89 (1.21–2.96) | 0.005 *** |
| Child knows taking the deworming pill will prevent them from harm | 1.62 (0.92–2.87) | 0.095 * | 0.64 (0.40–1.02) | 0.059 * |
| Child knows not taking the pill will make them fall sick | 1.59 (1.11–2.28) | 0.011 ** | 1.78 (1.26–2.50) | 0.001 *** |
| Child knows precise date of the last pill distribution | 2.49 (0.92–6.75) | 0.074 * | 1.68 (0.90–3.16) | 0.106 |
| Caregiver knows taking the deworming pill is important | 0.99 (0.40–2.46) | 0.987 | 1.56 (0.91–2.69) | 0.107 |
| Caregiver knows taking the deworming pill will prevent harm for their child | 0.67 (0.39–1.12) | 0.127 | 1.51 (1.00–2.27) | 0.048 ** |
| Caregiver knows not taking the pill will make the child fall sick | 4.63 (2.32–9.25) | 0.000 *** | 5.68 (2.48–12.99) | 0.000 *** |
| Caregiver knows the precise date of last pill distribution | 2.57 (1.53–4.32) | 0.000 *** | 4.12 (1.53–11.13) | 0.005 *** |
| Caregivers learned about deworming sessions from BRAC community workers | 2.07 (1.49–2.88) | 0.000 *** | 1.65 (1.19–2.28) | 0.003 *** |
| Caregivers learned about deworming sessions from visual aid/miking | 1.37 (0.73–2.56) | 0.323 | 0.93 (0.57–1.52) | 0.782 |
| Caregivers saw sensitization activity-courtyard meeting with women | 0.80 (0.49–1.32) | 0.382 | 1.58 (0.57–4.38) | 0.383 |
| Caregivers saw sensitization activity-miking | 1.33 (0.92–1.92) | 0.131 | 2.77 (1.41–5.44) | 0.003 *** |
| Caregivers saw sensitization activity-household visit by community workers | 1.09 (0.72–1.65) | 0.697 | 0.24 (0.11–0.53) | 0.000 *** |
| Caregivers saw community workers from the government going door-to-door | 2.42 (1.37–4.25) | 0.002 *** | 2.08 (1.14–3.79) | 0.017 ** |
| Caregivers saw community workers from BRAC going door-to-door | 1.79 (1.23–2.59) | 0.002 *** | 1.95 (0.91–4.19) | 0.085 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saha, A.; Chowdhury, S.; Goswami, E.T.; Gop, K.; Alam, A.; Rahman, A.; Sarker, M. Depriving Out-of-School Children of Deworming Tablets for Soil-Transmitted Helminth Infection in Bangladesh: The Irony of a School-Based Deworming Programme. Trop. Med. Infect. Dis. 2022, 7, 35. https://doi.org/10.3390/tropicalmed7030035
Saha A, Chowdhury S, Goswami ET, Gop K, Alam A, Rahman A, Sarker M. Depriving Out-of-School Children of Deworming Tablets for Soil-Transmitted Helminth Infection in Bangladesh: The Irony of a School-Based Deworming Programme. Tropical Medicine and Infectious Disease. 2022; 7(3):35. https://doi.org/10.3390/tropicalmed7030035
Chicago/Turabian StyleSaha, Avijit, Srizan Chowdhury, Edwin Theophilus Goswami, Konica Gop, Ariful Alam, Asadur Rahman, and Malabika Sarker. 2022. "Depriving Out-of-School Children of Deworming Tablets for Soil-Transmitted Helminth Infection in Bangladesh: The Irony of a School-Based Deworming Programme" Tropical Medicine and Infectious Disease 7, no. 3: 35. https://doi.org/10.3390/tropicalmed7030035
APA StyleSaha, A., Chowdhury, S., Goswami, E. T., Gop, K., Alam, A., Rahman, A., & Sarker, M. (2022). Depriving Out-of-School Children of Deworming Tablets for Soil-Transmitted Helminth Infection in Bangladesh: The Irony of a School-Based Deworming Programme. Tropical Medicine and Infectious Disease, 7(3), 35. https://doi.org/10.3390/tropicalmed7030035







