Clinical Characteristics Associated with Detected Respiratory Microorganism Employing Multiplex Nested PCR in Patients with Presumptive COVID-19 but Negative Molecular Results in Lima, Peru
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Collection and Ethical Aspects
2.3. Processing of Samples and Study Variables
2.4. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ahn, J.G. Epidemiological changes in infectious diseases during the coronavirus disease 2019 pandemic in Korea: A systematic review. Clin. Exp. Pediatr. 2022, 65, 167–171. [Google Scholar] [CrossRef]
- Wong, N.S.; Leung, C.C.; Lee, S.S. Abrupt Subsidence of Seasonal Influenza after COVID-19 Outbreak, Hong Kong, China. Emerg. Infect. Dis. 2020, 26, 2752–2754. [Google Scholar] [CrossRef]
- Chiu, S.S.; Cowling, B.J.; Peiris, J.S.M.; Chan, E.L.Y.; Wong, W.H.S.; Lee, K.P. Effects of Nonpharmaceutical COVID-19 Interventions on Pediatric Hospitalizations for Other Respiratory Virus Infections, Hong Kong. Emerg. Infect. Dis. 2022, 28, 62–68. [Google Scholar] [CrossRef]
- Sakamoto, H.; Ishikane, M.; Ueda, P. Seasonal Influenza Activity During the SARS-CoV-2 Outbreak in Japan. JAMA 2020, 323, 1969–1971. [Google Scholar] [CrossRef]
- Lee, H.H.; Lin, S.H. Effects of COVID-19 Prevention Measures on Other Common Infections, Taiwan. Emerg. Infect. Dis. 2020, 26, 2509–2511. [Google Scholar] [CrossRef]
- Ayouni, I.; Maatoug, J.; Dhouib, W.; Zammit, N.; Fredj, S.B.; Ghammam, R.; Ghannem, H. Effective public health measures to mitigate the spread of COVID-19: A systematic review. BMC Public Health 2021, 21, 1015. [Google Scholar] [CrossRef]
- Masai, A.N.; Akın, L. Practice of COVID-19 preventive measures and risk of acute respiratory infections: A longitudinal study in students from 95 countries. Int. J. Infect. Dis. 2021, 113, 168–174. [Google Scholar] [CrossRef]
- Andryukov, B.G. Six decades of lateral flow immunoassay: From determining metabolic markers to diagnosing COVID-19. AIMS Microbiol. 2020, 6, 280–304. [Google Scholar] [CrossRef]
- Sturgeon, C.M.; Viljoen, A. Analytical error and interference in immunoassay: Minimizing risk. Ann. Clin. Biochem. Int. J. Lab. Med. 2011, 48, 418–432. [Google Scholar] [CrossRef]
- Chiu, Y.T.; Tien, N.; Lin, H.C.; Wei, H.M.; Lai, H.C.; Chen, J.A.; Low, Y.Y.; Lin, H.H.; Hsu, Y.L.; Hwang, K.P. Detection of respiratory pathogens by application of multiplex PCR panel during early period of COVID-19 pandemic in a tertiary hospital in Central Taiwan. J. Microbiol. Immunol. Infect. 2021, in press. [Google Scholar] [CrossRef]
- Hirotsu, Y.; Maejima, M.; Shibusawa, M.; Natori, Y.; Nagakubo, Y.; Hosaka, K.; Sueki, H.; Amemiya, K.; Hayakawa, M.; Mochizuki, H.; et al. Direct comparison of Xpert Xpress, FilmArray Respiratory Panel, Lumipulse antigen test, and RT-qPCR in 165 nasopharyngeal swabs. BMC Infect. Dis. 2022, 22, 221. [Google Scholar] [CrossRef]
- Poritz, M.A.; Blaschke, A.J.; Byington, C.L.; Meyers, L.; Nilsson, K.; Jones, D.E.; Thatcher, S.A.; Robbins, T.; Lingenfelter, B.; Amiott, E.; et al. FilmArray, an Automated Nested Multiplex PCR System for Multi-Pathogen Detection: Development and Application to Respiratory Tract Infection. PLoS ONE 2011, 6, e26047. [Google Scholar] [CrossRef]
- Agca, H.; Akalin, H.; Saglik, I.; Hacimustafaoglu, M.; Celebi, S.; Ener, B. Changing epidemiology of influenza and other respiratory viruses in the first year of COVID-19 pandemic. J. Infect. Public Health 2021, 14, 1186–1190. [Google Scholar] [CrossRef]
- Groves, H.E.; Piché-Renaud, P.P.; Peci, A.; Farrar, D.S.; Buckrell, S.; Bancej, C.; Sevenhuysen, C.; Campigotto, A.; Gubbay, J.B.; Morris, S.K. The impact of the COVID-19 pandemic on influenza, respiratory syncytial virus, and other seasonal respiratory virus circulation in Canada: A population-based study. Lancet Reg. Health-Am. 2021, 1, 100015. Available online: https://www.sciencedirect.com/science/article/pii/S2667193x21000077 (accessed on 6 July 2022).
- Gomez, G.B.; Mahé, C.; Chaves, S.S. Uncertain effects of the pandemic on respiratory viruses. Science 2021, 372, 1043–1044. [Google Scholar] [CrossRef]
- FILMARRAY Respiratory Panel. Biomérieux. Available online: https://www.biomerieux-nordic.com/product/filmarray-respiratory-panel (accessed on 30 June 2022).
- Glossary of Influenza (Flu) Terms|CDC. 2019. Available online: https://www.cdc.gov/flu/about/glossary.htm (accessed on 6 July 2022).
- Surveillance Case Definitions for ILI and SARI. Available online: https://www.who.int/teams/global-influenza-programme/surveillance-and-monitoring/case-definitions-for-ili-and-sari (accessed on 6 July 2022).
- Galli, C.; Pellegrinelli, L.; Bubba, L.; Primache, V.; Anselmi, G.; Delbue, S.; Signorini, L.; Binda, S.; Cereda, D.; Gramegna, M.; et al. When the COVID-19 Pandemic Surges during Influenza Season: Lessons Learnt from the Sentinel Laboratory-Based Surveillance of Influenza-Like Illness in Lombardy during the 2019–2020 Season. Viruses 2021, 13, 695. [Google Scholar] [CrossRef]
- Busson, L.; Bartiaux, M.; Brahim, S.; Konopnicki, D.; Dauby, N.; Gérard, M.; De Backer, P.; Van Vaerenbergh, K.; Mahadeb, B.; Mekkaoui, L.; et al. Contribution of the FilmArray Respiratory Panel in the management of adult and pediatric patients attending the emergency room during 2015–2016 influenza epidemics: An interventional study. Int. J. Infect. Dis. 2019, 83, 32–39. [Google Scholar] [CrossRef]
- Tsagarakis, N.J.; Sideri, A.; Makridis, P.; Triantafyllou, A.; Stamoulakatou, A.; Papadogeorgaki, E. Age-related prevalence of common upper respiratory pathogens, based on the application of the FilmArray Respiratory panel in a tertiary hospital in Greece. Medicine 2018, 97, e10903. [Google Scholar] [CrossRef]
- Ciotti, M.; Maurici, M.; Santoro, V.; Coppola, L.; Sarmati, L.; De Carolis, G.; De Filippis, P.; Pica, F. Viruses of Respiratory Tract: An Observational Retrospective Study on Hospitalized Patients in Rome, Italy. Microorganisms 2020, 8, 501. [Google Scholar] [CrossRef]
- Anand, M.; Nimmala, P. Seasonal incidence of respiratory viral infections in Telangana, India: Utility of a multiplex PCR assay to bridge the knowledge gap. Trop. Med. Int. Health 2020, 25, 1503–1509. [Google Scholar] [CrossRef]
- Leber, A.L.; Everhart, K.; Daly, J.A.; Hopper, A.; Harrington, A.; Schreckenberger, P.; McKinley, K.; Jones, M.; Holmberg, K.; Kensinger, B. Multicenter Evaluation of BioFire FilmArray Respiratory Panel 2 for Detection of Viruses and Bacteria in Nasopharyngeal Swab Samples. Clin. Microbiol. 2018, 56, e01945-17. [Google Scholar] [CrossRef] [PubMed]
- Broor, S.; Krishnan, A.; Roy, D.S.; Dhakad, S.; Kaushik, S.; Mir, M.A.; Singh, Y.; Moen, A.; Chadha, M.; Mishra, A.C.; et al. Dynamic Patterns of Circulating Seasonal and Pandemic A(H1N1)pdm09 Influenza Viruses From 2007–2010 in and around Delhi, India. Roberts MG, editor. PLoS ONE 2012, 7, e29129. [Google Scholar] [CrossRef]
- Allan, G.M.; Arroll, B. Prevention and treatment of the common cold: Making sense of the evidence. CMAJ 2014, 186, 190–199. [Google Scholar] [CrossRef]
- Minsa: Aumenta Número de Casos por Influenza A(H3N2) a Nivel Nacional. Available online: https://www.gob.pe/institucion/minsa/noticias/605987-minsa-aumenta-numero-de-casos-por-influenza-a-h3n2-a-nivel-nacional (accessed on 16 June 2022).
- Finianos, M.; Issa, R.; Curran, M.D.; Afif, C.; Rajab, M.; Irani, J.; Hakimeh, N.; Naous, A.; Hajj, M.J.; Hajj, P.; et al. Etiology, seasonality, and clinical characterization of viral respiratory infections among hospitalized children in Beirut, Lebanon: Molecular Viral Epidemiology of Respiratory Viruses in Lebanon. J. Med. Virol. 2016, 88, 1874–1881. [Google Scholar] [CrossRef]
- O’Grady, K.F.; Grimwood, K.; Sloots, T.P.; Whiley, D.M.; Acworth, J.P.; Phillips, N.; Goyal, V.; Chang, A.B. Prevalence, codetection and seasonal distribution of upper airway viruses and bacteria in children with acute respiratory illnesses with cough as a symptom. Clin. Microbiol. Infect. 2016, 22, 527–534. [Google Scholar] [CrossRef]
- Adam, K.; Pangesti, K.N.A.; Setiawaty, V. Multiple Viral Infection Detected from Influenza-Like Illness Cases in Indonesia. BioMed Res. Int. 2017, 2017, 9541619. [Google Scholar] [CrossRef]
- Yang, S.; Li, H.; Tang, Y.; Yu, F.; Ma, C.; Zhang, H.; Pang, L.; Zhao, H.; Wang, L. Multiplex Tests for Respiratory Tract Infections: The Direct Utility of the FilmArray Respiratory Panel in Emergency Department. Can. Respir. J. 2020, 2020, 6014563. [Google Scholar] [CrossRef]
- Serigstad, S.; Markussen, D.; Grewal, H.M.S.; Ebbesen, M.; Kommedal, Ø.; Heggelund, L.; van Werkhoven, C.H.; Faurholt-Jepsen, D.; Clark, T.W.; Ritz, C.; et al. Rapid syndromic PCR testing in patients with respiratory tract infections reduces time to results and improves microbial yield. Sci. Rep. 2022, 12, 326. [Google Scholar] [CrossRef]
- Barlam, T.F.; Cosgrove, S.E.; Abbo, L.M.; Macdougall, C.; Schuetz, A.N.; Septimus, E.J.; Srinivasan, A.; Dellit, T.H.; Falck-Ytter, Y.T.; Fishman, N.O.; et al. Implementing an Antibiotic Stewardship Program: Guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin. Infect. Dis. 2016, 62, e51–e77. [Google Scholar] [CrossRef]
- Green, D.A.; Hitoaliaj, L.; Kotansky, B.; Campbell, S.M.; Peaper, D.R. Clinical Utility of On-Demand Multiplex Respiratory Pathogen Testing among Adult Outpatients. J. Clin. Microbiol. 2016, 54, 2950. [Google Scholar] [CrossRef]
- Lee, B.R.; Hassan, F.; Jackson, M.A.; Selvarangan, R. Impact of multiplex molecular assay turn-around-time on antibiotic utilization and clinical management of hospitalized children with acute respiratory tract infections. J. Clin. Virol. 2019, 110, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Echavarría, M.; Marcone, D.N.; Querci, M.; Seoane, A.; Ypas, M.; Videla, C.; O’Farrell, C.; Vidaurreta, S.; Ekstrom, J.; Carballal, G. Clinical impact of rapid molecular detection of respiratory pathogens in patients with acute respiratory infection. J. Clin. Virol. 2018, 108, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Chertow, D.S.; Memoli, M.J. Bacterial coinfection in influenza: A grand rounds review. JAMA 2013, 309, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Hishiki, H.; Ishiwada, N.; Fukasawa, C.; Abe, K.; Hoshino, T.; Aizawa, J.; Ishikawa, N. Incidence of bacterial coinfection with respiratory syncytial virus bronchopulmonary infection in pediatric inpatients. J. Infect. Chemother. 2011, 17, 87–90. [Google Scholar] [CrossRef] [PubMed]
- Lansbury, L.; Lim, B.; Baskaran, V.; Lim, W.S. Co-infections in people with COVID-19: A systematic review and meta-analysis. J. Infect. 2020, 81, 266–275. [Google Scholar] [CrossRef] [PubMed]
- Morris, A.C.; Kohler, K.; De Corte, T.; Ercole, A.; De Grooth, H.-J.; Elbers, P.W.G.; Povoa, P.; Morais, R.; Koulenti, D.; Jog, S.; et al. Co-infection and ICU-acquired infection in COIVD-19 ICU patients: A secondary analysis of the UNITE-COVID data set. Crit. Care 2022, 26, 236. [Google Scholar] [CrossRef]
- Cultrera, R.; Barozzi, A.; Libanore, M.; Marangoni, E.; Pora, R.; Quarta, B.; Spadaro, S.; Ragazzi, R.; Marra, A.; Segala, D.; et al. Co-Infections in Critically Ill Patients with or without COVID-19: A Comparison of Clinical Microbial Culture Findings. Int. J. Environ. Res. Public Health 2021, 18, 4358. [Google Scholar] [CrossRef]
- Copaja-Corzo, C.; Hueda-Zavaleta, M.; Benites-Zapata, V.A.; Rodriguez-Morales, A.J. Antibiotic use and fatal outcomes among critically ill patients with covid-19 in Tacna, Peru. Antibiotics 2021, 10, 959. [Google Scholar] [CrossRef]
- Nateghian, A.; Gouya, M.M.; Nabavi, M.; Soltani, H.; Mousavi, S.V.; Agah, E.; Erfani, H.; Parchami, P.; Dadras, M.; Robinson, J.L. Demographic, clinical, and virological characteristics of patients with a laboratory-confirmed diagnosis of influenza during three consecutive seasons, 2015/2016–2017/18, in the Islamic Republic of Iran. J. Clin. Virol. 2020, 124, 104281. [Google Scholar] [CrossRef]
- Chow, A.; Aung, A.H.; Tin, G.; Ooi, C.K. Performance of WHO and CDC influenza-like illness (ILI) case definitions in detecting influenza in the tropics. Int. J. Infect. Dis. 2020, 101, 370–371. [Google Scholar] [CrossRef]
- Winther, B. Rhinovirus Infections in the Upper Airway. Proc. Am. Thorac. Soc. 2011, 8, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Lo, D.; Kennedy, J.L.; Kurten, R.C.; Panettieri, R.A.; Koziol-White, C.J. Modulation of airway hyperresponsiveness by rhinovirus exposure. Respir. Res. 2018, 19, 208. [Google Scholar] [CrossRef] [PubMed]
- Ng, K.T.; Oong, X.Y.; Lim, S.H.; Chook, J.B.; Takebe, Y.; Chan, Y.F.; Chan, K.G.; Hanafi, N.S.; Pang, Y.K.; Kamarulzaman, A.; et al. Viral Load and Sequence Analysis Reveal the Symptom Severity, Diversity, and Transmission Clusters of Rhinovirus Infections. Clin. Infect. Dis. 2018, 67, 261–268. [Google Scholar] [CrossRef] [PubMed]
| Variable | (n = 342) |
|---|---|
| Age (years) 1 | 33.39 (19.70–47.17) |
| ≤5 years (%) | 18 (5.26) |
| 6–17 years (%) | 61 (17.84) |
| 18–59 years (%) | 221 (64.62) |
| ≥60 years (%) | 42 (12.28) |
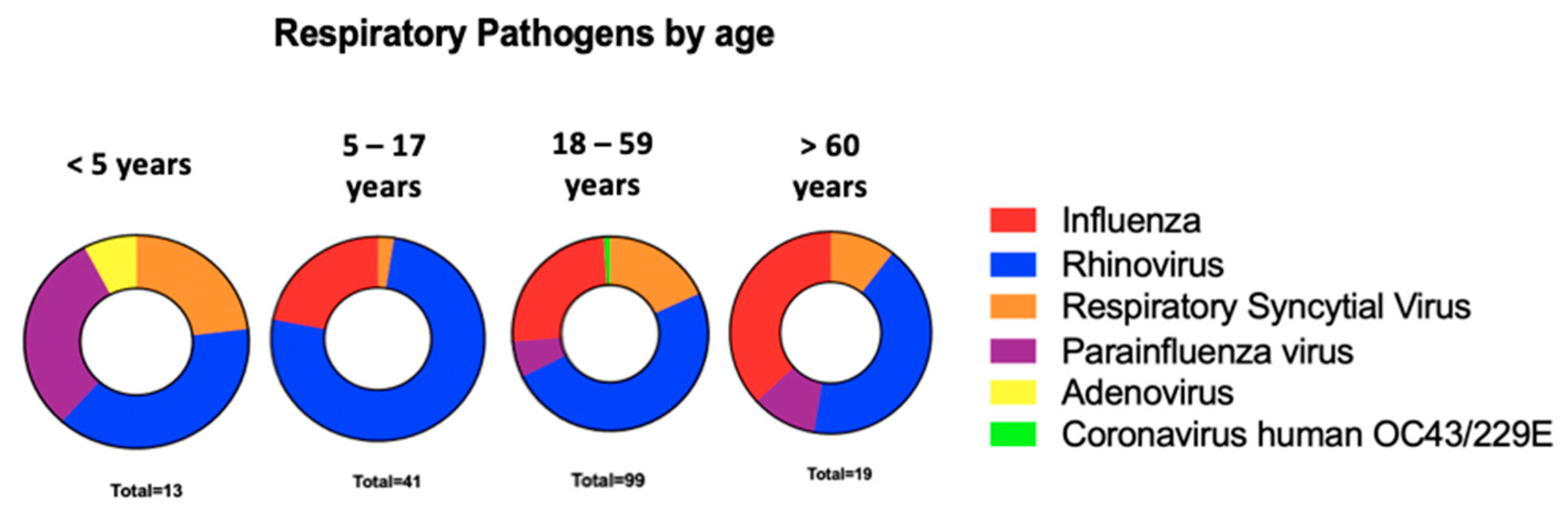
| Positivity by age categorized | |
| ≤5 years (%) | 12 (66.67) |
| 6–17 years (%) | 41 (67.21) |
| 18–59 years (%) | 99 (44.79) |
| ≥60 years (%) | 19 (45.23) |
| Sex | |
| Female (%) | 196 (57.31) |
| Male (%) | 146 (42.69) |
| Days of symptoms 1 | 2 (1–3) |
| Comorbidities | |
| Pregnancy (%) | 5 (1.46) |
| Cardiopathy (%) | 8 (2.34) |
| Diabetes (%) | 5 (1.46) |
| Chronic kidney disease (%) | 2 (0.58) |
| Chronic pulmonary disease (%) | 3 (0.88) |
| Cancer (%) | 1 (0.29) |
| Clinical characteristics | |
| Fever (%) | 137 (40.06) |
| General discomfort (%) | 148 (43.27) |
| Cough (%) | 200 (58.48) |
| Sore throat (%) | 240 (70.18) |
| Respiratory distress (%) | 45 (13.16) |
| Nasal congestion (%) | 193 (56.43) |
| Diarrhea (%) | 34 (9.94) |
| Nausea (%) | 23 (6.73) |
| Headache (%) | 62 (18.13) |
| Irritation (%) | 5 (1.46) |
| Myalgias (%) | 41 (11.99) |
| Abdominal pain (%) | 11 (3.22) |
| Thorax pain (%) | 15 (4.39) |
| Arthralgias (%) | 8 (2.34) |
| Influenza-like Illness by WHO (%) | 81 (23.68) |
| Influenza-like Illness by CDC (%) | 116 (33.92) |
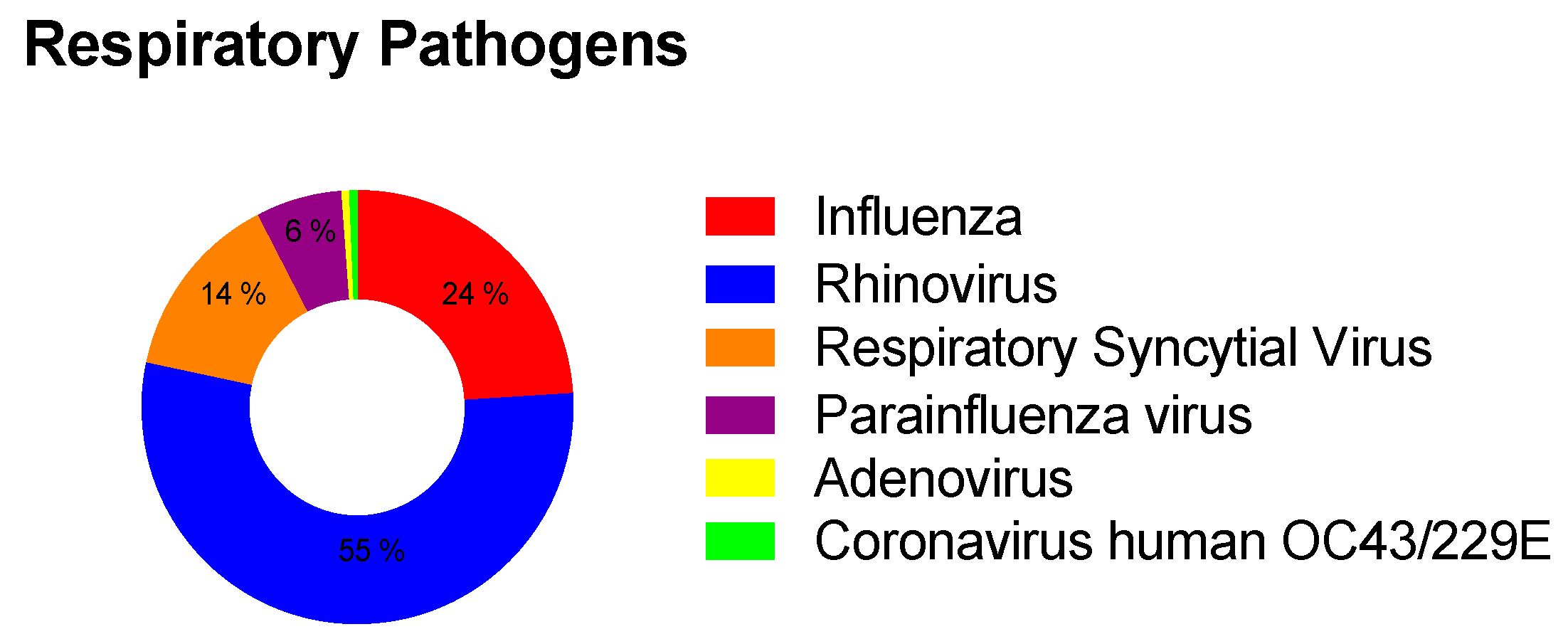
| Pathogens detected (%) | 171 (50.00) |
| Rhinovirus (%) | 93 (54.38) |
| Influenza A/B (%) | 41 (23.98) |
| A(H3N2) | 39 (95.12) |
| Respiratory Syncytial Virus (%) | 24 (14.04) |
| Parainfluenza (%) | 11 (6.42) |
| Adenovirus (%) | 1 (0.58) |
| Human Coronavirus OC43 | 1 (0.58) |
| Human Coronavirus 229E | 1 (0.58) |
| Co-infections (Influenza/Rhinovirus) | 5 (2.92) |
| Variable | Rhinovirus (n = 89) | Influenza (n = 41) | RSV (n = 22) | p-Value |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age (years) * | 25.67 (9.69–35.28) | 32.87 (21.24–44.19) | 35.41 (23.69–45.27) | 0.028 a |
| <5 years (%) | 5 (5.61) | 0 (0.0) | 3 (13.63) | 0.022 b |
| 6–17 years (%) | 30 (33.70) | 9 (21.95) | 1 (4.55) | |
| 18–59 years (%) | 47 (52.80) | 25 (60.98) | 16 (72.72) | |
| >60 years (%) | 7 (7.89) | 7 (17.07) | 2 (9.10) | |
| Sex | 0.272 b | |||
| Female | 54 (60.68) | 20 (48.78) | 10 (45.45) | |
| Male | 35 (39.32) | 21 (51.22) | 12 (54.55) | |
| Days of symptoms before sampling * | 2 (1–3) | 3 (2–4) | 2.5 (2–4) | 0.028 a |
| Comorbidities | ||||
| Pregnancy (%) | 0 (0.0) | 1 (2.43) | 0 (0.0) | 0.999 c |
| Cardiopathy (%) | 0 (0.0) | 3 (7.31) | 0 (0.0) | 0.038 c |
| Diabetes (%) | 0 (0.0) | 0 (0.0) | 1 (4.54) | 0.145 c |
| Chronic kidney disease (%) | 1 (1.12) | 0 (0.0) | 0 (0.0) | 0.999 c |
| Chronic pulmonary disease (%) | 1 (1.12) | 0 (0.0) | 0 (0.0) | 0.999 c |
| Clinical characteristics | ||||
| Fever (%) | 32 (35.95) | 21 (51.21) | 7 (31.81) | 0.186 b |
| General malaise (%) | 43 (48.31) | 17 (41.46) | 9 (40.90) | 0.691 b |
| Cough (%) | 65 (73.03) | 31 (75.60) | 16 (72.72) | 0.947 b |
| Sore throat (%) | 70 (78.65) | 32 (78.04) | 19 (86.36) | 0.694 b |
| Respiratory distress (%) | 7 (7.86) | 8 (19.51) | 5 (22.27) | 0.067 c |
| Nasal congestion (%) | 67 (75.28) | 24 (58.53) | 17 (77.27) | 0.129 b |
| Diarrhea (%) | 9 (10.11) | 5 (12.19) | 3 (13.63) | 0.816 c |
| Nausea (%) | 4 (4.49) | 3 (7.31) | 2 (9.10) | 0.568 c |
| Headache (%) | 16 (17.97) | 5 (12.19) | 6 (27.27) | 0.307 c |
| Irritation (%) | 1 (1.12) | 2 (4.87) | 1 (4.55) | 0.236 c |
| Myalgias (%) | 8 (8.98) | 6 (14.63) | 4 (18.18) | 0.324 c |
| Abdominal pain (%) | 1 (1.12) | 0 (0.0) | 0 (0.0) | 0.999 c |
| Thorax pain (%) | 2 (2.24) | 2 (4.87) | 11 (50.00) | 0.533 c |
| Arthralgias (%) | 0 (0.0) | 1 (0.50) | 1 (0.50) | 0.170 c |
| Influenza-like illness by WHO | 24 (26.97) | 17 (41.46) | 6 (27.27) | 0.232 b |
| Influenza-like illness by CDC | 31 (34.82) | 20 (48.78) | 7 (31.82) | 0.253 b |
| Variable | Influenza | Rhinovirus | Respiratory Syncytial Virus | |||
|---|---|---|---|---|---|---|
| cPR (95% CI) | p-Value | cPR (95% CI) | p-Value | cPR (95% CI) | p-Value | |
| Age | 1.006 (0.991–1.020) | 0.409 | 0.980 (0.970–0.990) | <0.001 | 1.000 (0.983–1.017) | 0.994 |
| Cardiopathy | 3.296 (1.281–8.477) | 0.013 | 0.971 (0.272–3.091) | 0.890 | - | - |
| Fever | 1.571 (0.885–2.788) | 0.123 | 0.862 (0.599–1.239) | 0.424 | 0.616 (0.262–1.448) | 0.267 |
| General discomfort | 0.928 (0.517–1.665) | 0.803 | 1.177 (0.832–1.665) | 0.357 | 1.109 (0.510–2.407) | 0.793 |
| Cough | 2.201 (1.114–4.346) | 0.023 | 1.931 (1.287–2.896) | <0.001 | 1.420 (0.624–3.231) | 0.403 |
| Sore throat | 1.511 (0.747–3.053) | 0.250 | 1.655 (1.057–2.591) | 0.028 | 2.975 (0.905–9.769) | 0.072 |
| Nasal congestion | 1.089 (0.607–1.954) | 0.773 | 2.219 (1.468–3.354) | <0.001 | 2.933 (1.119–7.685) | 0.029 |
| Influenza-like illness by WHO | 2.282 (1.290–4.035) | 0.005 | 1.184 (0.805–1.741) | 0.389 | 1.074 (0.440–2.618) | 0.875 |
| Influenza-like illness by CDC | 1.855 (1.048–3.283) | 0.034 | 1.071 (0.746–1.538) | 0.708 | 0.802 (0.342–1.881) | 0.612 |
| Variables | Influenza | Rhinovirus | Respiratory Syncytial Virus | |||
|---|---|---|---|---|---|---|
| aPR (95% CI) | p-Value | aPR (95% CI) | p-Value | aPR (95% CI) | p-Value | |
| Age | 1.007 (0.992–1.023) | 0.335 | 0.983 (0.973–0.993) | 0.002 | 1.005 (0.987–1.024) | 0.545 |
| Cardiopathy | 3.007 (0.992–1.023) | 0.074 | - | - | - | - |
| General malaise | 0.028 (0.425–1.511) | 0.496 | 1.042 (0.742–1.462) | 0.812 | 0.833 (0.391–1.774) | 0.669 |
| Sore throat | 1.684 (0.829–3.423) | 0.149 | 1.256 (0.791–1.993) | 0.333 | 2.376 (0.715–7.893) | 0.157 |
| Nasal congestion | 0.979 (0.515–1.858) | 0.949 | 1.840 (1.169–2.897) | 0.008 | 2.591 (1.010–6.645) | 0.048 |
| Influenza-like illness by WHO | 2.331 (1.298–4.183) | 0.005 | 0.917 (0.628–1.339) | 0.655 | 0.911 (0.382–2.170) | 0.835 |
| Influenza-like illness by CDC | 1.892 (1.051–3.409) | 0.034 | 0.858 (0.604–1.219) | 0.394 | 0.717 (0.304–1.691) | 0.448 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez de la Torre Pretell, J.C.; Hueda-Zavaleta, M.; Cáceres-DelAguila, J.A.; Barletta-Carrillo, C.; Copaja-Corzo, C.; Poccorpachi, M.d.P.S.; Delgado, M.S.V.; Sanchez, G.M.M.L.; Benites-Zapata, V.A. Clinical Characteristics Associated with Detected Respiratory Microorganism Employing Multiplex Nested PCR in Patients with Presumptive COVID-19 but Negative Molecular Results in Lima, Peru. Trop. Med. Infect. Dis. 2022, 7, 340. https://doi.org/10.3390/tropicalmed7110340
Gómez de la Torre Pretell JC, Hueda-Zavaleta M, Cáceres-DelAguila JA, Barletta-Carrillo C, Copaja-Corzo C, Poccorpachi MdPS, Delgado MSV, Sanchez GMML, Benites-Zapata VA. Clinical Characteristics Associated with Detected Respiratory Microorganism Employing Multiplex Nested PCR in Patients with Presumptive COVID-19 but Negative Molecular Results in Lima, Peru. Tropical Medicine and Infectious Disease. 2022; 7(11):340. https://doi.org/10.3390/tropicalmed7110340
Chicago/Turabian StyleGómez de la Torre Pretell, Juan Carlos, Miguel Hueda-Zavaleta, José Alonso Cáceres-DelAguila, Claudia Barletta-Carrillo, Cesar Copaja-Corzo, Maria del Pilar Suarez Poccorpachi, María Soledad Vega Delgado, Gloria Maria Magdalena Levano Sanchez, and Vicente A. Benites-Zapata. 2022. "Clinical Characteristics Associated with Detected Respiratory Microorganism Employing Multiplex Nested PCR in Patients with Presumptive COVID-19 but Negative Molecular Results in Lima, Peru" Tropical Medicine and Infectious Disease 7, no. 11: 340. https://doi.org/10.3390/tropicalmed7110340
APA StyleGómez de la Torre Pretell, J. C., Hueda-Zavaleta, M., Cáceres-DelAguila, J. A., Barletta-Carrillo, C., Copaja-Corzo, C., Poccorpachi, M. d. P. S., Delgado, M. S. V., Sanchez, G. M. M. L., & Benites-Zapata, V. A. (2022). Clinical Characteristics Associated with Detected Respiratory Microorganism Employing Multiplex Nested PCR in Patients with Presumptive COVID-19 but Negative Molecular Results in Lima, Peru. Tropical Medicine and Infectious Disease, 7(11), 340. https://doi.org/10.3390/tropicalmed7110340










