An Intra-COVID-19 Assessment of Hand Hygiene Facility, Policy and Staff Compliance in Two Hospitals in Sierra Leone: Is There a Difference between Regional and Capital City Hospitals?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Setting
2.3. Hand Hygiene Facilities Assessment
2.4. Hand Hygiene Compliance
2.5. Hand Hygiene Policy
2.6. Data Analysis
2.7. Ethical Consideration
3. Results
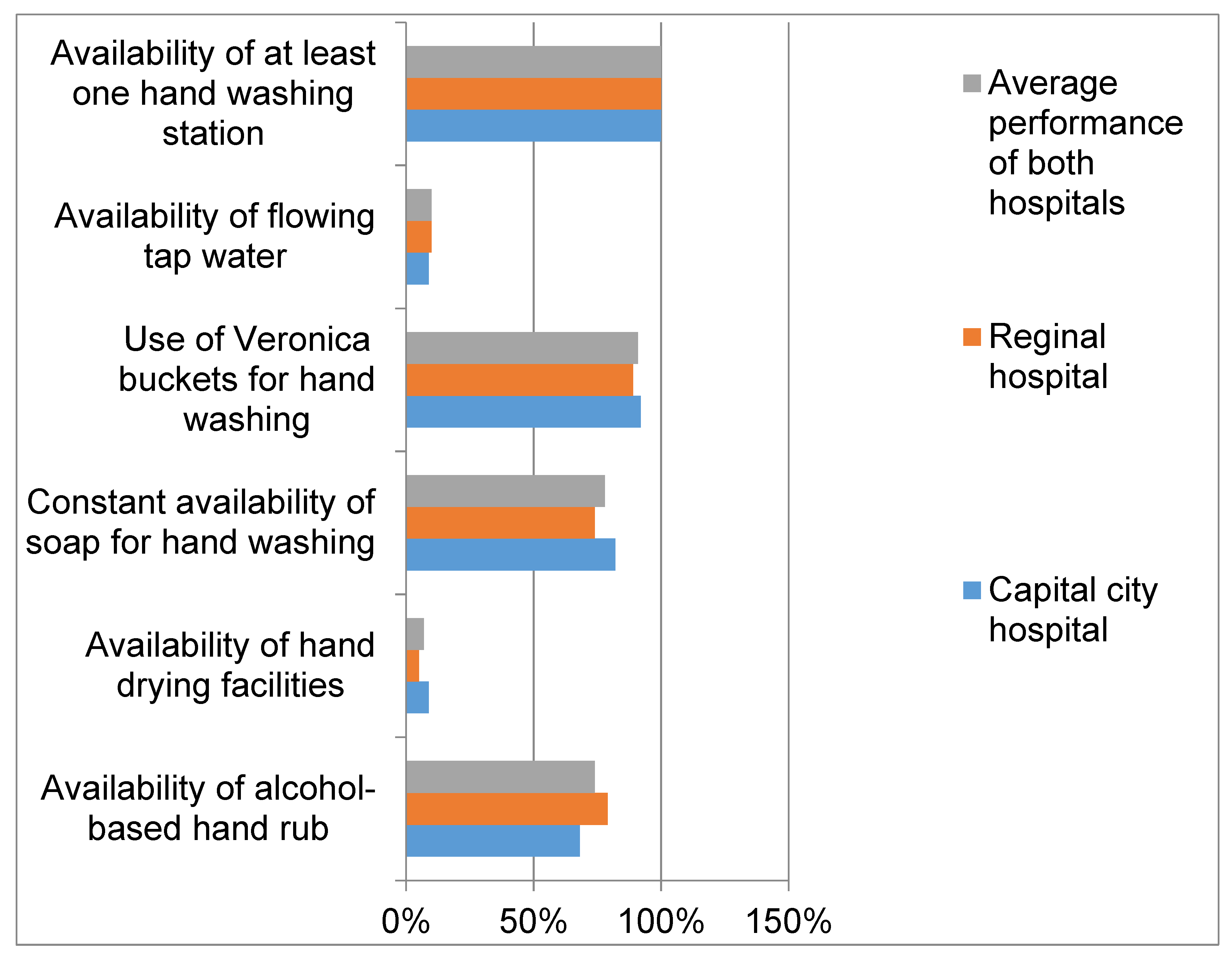
3.1. Hand Hygiene Facilities
3.2. Hand Hygiene Compliance
3.3. Hand Hygiene Levels
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Report on the Burden of Endemic Health Care-Associated Infection Worldwide. 2011. Available online: https://apps.who.int/iris/bitstream/handle/10665/80135/9789241501507_eng.pdf (accessed on 10 July 2021).
- Kritsotakis, E.I.; Kontopidou, F.; Astrinaki, E.; Roumbelaki, M.; Ioannidou, E.; Gikas, A. Prevalence, incidence burden, and clinical impact of healthcare-associated infections and antimicrobial resistance: A national prevalent cohort study in acute care hospitals in Greece. Infect. Drug Resist. 2017, 10, 317–328. [Google Scholar] [CrossRef] [PubMed]
- Forrester, J.D.; Maggio, P.M.; Tennakoon, L. Cost of Health Care-Associated Infections in the United States. J. Patient Saf. 2021. [Google Scholar] [CrossRef] [PubMed]
- Haque, M.; Sartelli, M.; McKimm, J.; Abu Bakar, M. Health care-associated infections—An overview. Infect. Drug Resist. 2018, 11, 2321–2333. [Google Scholar] [CrossRef]
- Allegranzi, B.; Pittet, D. Role of hand hygiene in healthcare-associated infection prevention. J. Hosp. Infect. 2009, 73, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Hillier, M.D. Using effective hand hygiene practice to prevent and control infection. Nurs. Stand. 2020, 35, 45–50. [Google Scholar] [CrossRef]
- Kirkland, K.B.; Homa, K.A.; Lasky, R.A.; Ptak, J.A.; Taylor, E.A.; Splaine, M.E. Impact of a hospital-wide hand hygiene initiative on healthcare-associated infections: Results of an interrupted time series. BMJ Qual. Saf. 2012, 21, 1019–1026. [Google Scholar] [CrossRef][Green Version]
- Sax, H.; Allegranzi, B.; Chraïti, M.N.; Boyce, J.; Larson, E.; Pittet, D. The World Health Organization hand hygiene observation method. Am. J. Infect. Control. 2009, 37, 827–834. [Google Scholar] [CrossRef]
- Loftus, M.J.; Guitart, C.; Tartari, E.; Stewardson, A.J.; Amer, F.; Bellissimo-Rodrigues, F.; Lee, Y.F.; Mehtar, S.; Sithole, B.L.; Pittet, D. Hand hygiene in low- and middle-income countries. Int. J. Infect. Dis. 2019, 86, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Ataiyero, Y.; Dyson, J.; Graham, M. Barriers to hand hygiene practices among health care workers in sub-Saharan African countries: A narrative review. Am. J. Infect. Control. 2019, 47, 565–573. [Google Scholar] [CrossRef]
- Nwaokenye, J.; Lakoh, S.; Morgan, J. Perceptions of Nigerian healthcare workers towards hand hygiene: A qualitative study. Pan. Afr. Med. J. 2020, 36, 204. [Google Scholar] [CrossRef]
- Tullo, J.E.; Lerea, M.J.; López, P.; Alonso, L. Impacto de la COVID-19 en la prestación de los servicios de salud esenciales en Paraguay [Impact of COVID-19 on the provision of essential health services in Paraguay]. Rev. Panam. Salud. Publica. 2020, 44, e161. [Google Scholar] [CrossRef] [PubMed]
- Lakoh, S.; Jiba, D.F.; Baldeh, M.; Adekanmbi, O.; Barrie, U.; Seisay, A.L.; Deen, G.F.; Salata, R.A.; Yendewa, G.A. Impact of COVID-19 on Tuberculosis Case Detection and Treatment Outcomes in Sierra Leone. Trop. Med. Infect. Dis. 2021, 6, 154. [Google Scholar] [CrossRef]
- Baker, M.A.; Sands, K.E.; Huang, S.S.; Kleinman, K.; Septimus, E.J.; Varma, N.; Blanchard, J.; Poland, R.E.; Coady, M.H.; Yokoe, D.S.; et al. CDC Prevention Epicenters Program. The Impact of COVID-19 on Healthcare-Associated Infections. Clin. Infect. Dis. 2021. [Google Scholar] [CrossRef]
- Sierra Leone Statistics. 2015 Population and Housing Census Summary of Final Results. (1–14 May 2015). 2015. Available online: https://www.statistics.sl/images/StatisticsSL/Documents/final-results_-2015_population_and_housing_census.pdf (accessed on 20 July 2021).
- Systems for Improved Access to Pharmaceuticals and Services (SIAPS). Infection Control Self-Assessment Tool for Primary Health Care Facilities. Submitted to the US Agency for International Development by the SIAPS) Program. Arlington: Management Sciences for Health. Available online: siapsprogram.org/wp-content/uploads/2013/01/12-137-ICAT-PCH.FINAL_.pdf (accessed on 6 September 2021).
- WHO. Hand Hygiene Technical Reference Manual. 2009. Available online: http://apps.who.int/iris/bitstream/handle/10665/44196/9789241598606_eng.pdf?sequence=1 (accessed on 10 August 2021).
- Public Health Ontario. Hand Hygiene Observation and Analysis Version 1.4; Public Health Ontario: Cambridge, ON, USA, 2009. [Google Scholar]
- Onyedibe, K.I.; Shehu, N.Y.; Pires, D.; Isa, S.E.; Okolo, M.O.; Gomerep, S.S.; Ibrahim, C.; Igbanugo, S.J.; Odesanya, R.U.; Olayinka, A.; et al. Assessment of hand hygiene facilities and staff compliance in a large tertiary health care facility in northern Nigeria: A cross sectional study. Antimicrob. Resist. Infect. Control. 2020, 9, 30. [Google Scholar] [CrossRef]
- WHO. Hand Hygiene Self-Assessment Framework. 2010. Available online: https://www.who.int/gpsc/country_work/hhsa_framework_October_2010.pdf (accessed on 4 August 2021).
- Bonful, H.A.; Addo-Lartey, A.; Aheto, J.M.K.; Ganle, J.K.; Sarfo, B.; Aryeetey, R. Limiting spread of COVID-19 in Ghana: Compliance audit of selected transportation stations in the Greater Accra region of Ghana. PLoS ONE 2020, 15, e0238971. [Google Scholar] [CrossRef]
- Yawson, A.E.; Hesse, A.A. Hand hygiene practices and resources in a teaching hospital in Ghana. J. Infect. Dev. Ctries. 2013, 7, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Lambe, K.A.; Lydon, S.; Madden, C.; Vellinga, A.; Hehir, A.; Walsh, M.; O’Connor, P. Hand Hygiene Compliance in the ICU: A Systematic Review. Crit. Care Med. 2019, 47, 1251–1257. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Sendlhofer, G.; Gombotz, V.; Pregartner, G.; Zierler, R.; Schwarz, C.; Tax, C.; Brunner, G. Hand hygiene compliance in intensive care units: An observational study. Int. J. Nurs. Pract. 2020, 26, e12789. [Google Scholar] [CrossRef]
- Allegranzi, B.; Sax, H.; Pittet, D. Hand hygiene and healthcare system change within multi-modal promotion: A narrative review. J. Hosp. Infect. 2013, 83, S3–S10. [Google Scholar] [CrossRef]
- Głabska, D.; Skolmowska, D.; Guzek, D. Population-based study of the influence of the COVID-19 pandemic on hand hygiene behaviors-polish adolescents’ COVID-19 experience (place-19) study. Sustainability 2020, 12, 4930. [Google Scholar] [CrossRef]
- Kilpatrick, C.; Tartari, E.; Gayet-Ageron, A.; Storr, J.; Tomczyk, S.; Allegranzi, B.; Pittet, D. Global hand hygiene improvement progress: Two surveys using the WHO Hand Hygiene Self-Assessment Framework. J. Hosp. Infect. 2018, 100, 202–206. [Google Scholar] [CrossRef] [PubMed]

| Cadre/Bed Capacity/Units | Total | Regional Hospital | Capital City Hospital | |||
|---|---|---|---|---|---|---|
| Freq. | % | Freq. | % | Freq. | % | |
| Bed capacity | 388 | 100.0 | 207 | 100.0 | 181 | 100.0 |
| Units/wards/department | 41 | 100.0 | 19 | 100.0 | 22 | 100.0 |
| Number of healthcare workers | 803 | 100 | 351 | 100 | 452 | 100 |
| Nurses | 546 | 68.1 | 252 | 71.8 | 294 | 67.9 |
| Doctors | 22 | 2.7 | 8 | 2.3 | 14 | 3.2 |
| Community health officers | 20 | 2.5 | 7 | 2 | 13 | 0.3 |
| Pharmacy personnel | 44 | 5.5 | 8 | 2.3 | 36 | 8.3 |
| Laboratory personnel | 46 | 5.7 | 21 | 6 | 25 | 5.8 |
| Radiographers | 6 | 0.7 | 4 | 1.1 | 2 | 0.5 |
| Others | 119 | 14.8 | 51 | 14.5 | 68 | 15.7 |
| Unit/Ward/Department of the Hospital | Capital City Hospital | Regional Hospital | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Frq. | Hand Washing Stations | Water Always Available | Hand Operated Tap in the Wash Stations | Use of Liquid Soap | Soap Always Available | Multiple Use Cloth for Hand Drying | Disposable Paper Towel | Frq. | Hand Washing Stations | Water Always Available | Hand Operated Tap Buckets in the Wash Stations | Use of Plain Liquid Soap | Soap Always Available | Multiple Use Cloth for Hand Drying | Disposable Paper Towel | |
| Triage | 1 | 8 | Yes | Sink | Yes | Yes | No | No | 1 | 4 | Yes | Yes | Yes | Yes | No | No |
| Laboratories | 1 | 5 | Yes | Sink | Yes | Yes | No | Yes | 1 | 1 | No | No | No | No | No | No |
| Accident and Emergency | 1 | 2 | Yes | Yes | Yes | Yes | No | No | 1 | 1 | Yes | Yes | Yes | Yes | No | No |
| ICU | 1 | 5 | Yes | Yes | No | Yes | No | No | 1 | 1 | Yes | Yes | Yes | Yes | No | No |
| Operating main theatre | 1 | 1 | Yes | Yes | Yes | Yes | No | No | 1 | 2 | Yes | No | Yes | Yes | No | No |
| Maternity theatre | NA | NA | NA | NA | NA | NA | NA | NA | 1 | 2 | No | No | Yes | Yes | No | Yes |
| Mortuary | 1 | 2 | Yes | Yes | Yes | Yes | No | No | 1 | 1 | Yes | No | No | Yes | No | No |
| Pharmacy | 1 | 1 | Yes | Yes | Yes | Yes | No | No | 1 | 1 | Yes | Sink | Yes | No | No | No |
| Physiotherapy unit | 1 | 2 | Yes | Yes | Yes | Yes | No | No | NA | NA | NA | NA | NA | NA | NA | NA |
| SCBU | NA | NA | NA | NA | NA | NA | NA | NA | 1 | 5 | Yes | Yes | Yes | Yes | No | No |
| Male medical ward | 2 | 2 | Yes | Yes | Yes | Yes | No | No | 1 | 2 | Yes | Yes | Yes | Yes | No | No |
| Female medical ward | 1 | 2 | No | Yes | No | No | No | No | 1 | 1 | Yes | Yes | Yes | Yes | No | No |
| Male surgical ward | 2 | 2 | No | Yes | Yes | No | No | No | 1 | 2 | Yes | Yes | Yes | Yes | No | No |
| Female surgical ward | 2 | 2 | Yes | Yes | No | Yes | No | No | 1 | 1 | Yes | Yes | Yes | Yes | No | No |
| Dental | 1 | 1 | Yes | Yes | Yes | Yes | No | No | 0 | 0 | NA | NA | NA | NA | NA | NA |
| IDPC/MDR-TB ward | 1 | 10 | Yes | No | Yes | Yes | No | Yes | 1 | 6 | Yes | Yes | Yes | Yes | No | Yes |
| Ophthalmology | 1 | 1 | Yes | Yes | Yes | Yes | No | No | 1 | 2 | Yes | Yes | Yes | Yes | No | No |
| Maternity unit | 1 | 4 | Yes | Yes | No | Yes | No | No | 1 | 6 | Yes | Sink | Yes | Yes | No | No |
| Public health | 1 | 1 | Yes | Yes | Yes | Yes | No | No | 0 | 0 | NA | NA | NA | NA | NA | NA |
| Research | 1 | 2 | Yes | Yes | No | Yes | No | No | 0 | 0 | NA | NA | NA | NA | NA | NA |
| Paediatric ward | 1 | 2 | No | Yes | Yes | No | No | No | 1 | 4 | Yes | Yes | Yes | No | No | No |
| Under five | 1 | 2 | Yes | No | Yes | Yes | No | No | 0 | 0 | No | No | No | No | No | No |
| Observation ward | NA | NA | NA | NA | NA | NA | NA | NA | 1 | 1 | Yes | Yes | Yes | Yes | No | No |
| X-ray department | NA | NA | NA | NA | NA | NA | NA | NA | 1 | 2 | No | Yes | Yes | No | Yes | No |
| IDCU | 1 | 1 | Yes | Yes | Yes | Yes | No | Yes | NA | NA | NA | NA | NA | NA | NA | NA |
| Parameter | Total N (%) | Capital City Hospital N (%) | Regional Hospital N (%) |
|---|---|---|---|
| Total opportunities | 2198 (100%) | 1279 (58.2%) | 919 (42.8%) |
| Ward | |||
| Medical | 353 (16.1) | 232 (18.1) | 121 (13.2) |
| Surgical | 440 (20.0) | 291 (22.8) | 149 (16.2) |
| Paediatric | 393 (17.9) | 216 (16.9) | 177 (19.3) |
| Maternity | 424 (19.3) | 198 (15.5) | 226 (24.6) |
| A & E | 360 (16.4) | 194 (15.2) | 166 (18.1) |
| Others | 228 (10.4) | 148 (11.6) | 80 (8.7) |
| Healthcare workers | |||
| Doctor | 250 (11.4) | 140 (10.9) | 110 (12.0) |
| Nurse | 1535 (69.8) | 1101 (86.1) | 434 (47.2) |
| Others | 413 (18.8) | 38 (3.0) | 375 (40.8) |
| Indication | |||
| Before touching a patient | 649 (29.5) | 315 (24.6) | 334 (36.3) |
| Before aseptic procedure | 256 (11.7) | 164 (12.8) | 92 (10.0) |
| After exposure to body fluid | 221 (10.1) | 155 (12.1) | 66 (7.2) |
| After touching a patient | 579 (26.3) | 304 (23.8) | 275 (29.9) |
| After touching patient surroundings | 493 (22.4) | 341 (26.7) | 152 (15.5) |
| Hand hygiene compliance | |||
| No | 1790 (81.4) | 1062 (83.0) | 728 (79.2) |
| Yes | 408 (18.6) | 217 (17.0) | 191 (20.8) |
| Parameter | Compliance | Crude Odds Ratio (C.I) | p | Adjusted Odds Ratio (C. I) | p | |
|---|---|---|---|---|---|---|
| Yes (%) 408 (18.6) | No (%) 1790 (81.4) | |||||
| Hospital | ||||||
| Capital city | 217 (17.0) | 1062 (83.0) | 1 | - | 1 | - |
| Regional | 191 (20.8) | 728 (79.2) | 1.28 (1.03–1.59) | 0.023 | 1.66 (1.24–2.23) | 0.001 |
| Wards | ||||||
| Medical | 75 (21.3) | 278 (78.7) | 1 | - | 1 | - |
| Surgical | 63 (14.3) | 377 (85.7) | 0.62 (0.43–0.89) | 0.011 | 0.49 (0.32–0.76) | 0.001 |
| Paediatric | 56 (14.3) | 337 (85.7) | 0.61 (0.42–0.90) | 0.013 | 0.46 (0.30–0.72) | 0.001 |
| Maternity | 91 (21.5) | 333 (78.5) | 1.01 (0.72–1.43) | 0.942 | 0.83 (0.55–1.25) | 0.382 |
| A & E | 45 (12.5) | 315 (87.5) | 0.53 (0.35–0.79) | 0.002 | 0.46 (0.29–0.73) | 0.001 |
| Others | 78 (34.2) | 150 (65.8) | 1.93 (1.33–2.80) | 0.001 | 2.10 (1.35–3.28) | 0.001 |
| Healthcare workers | ||||||
| Doctors | 63 (25.2) | 187 (74.8) | 1 | - | 1 | - |
| Nurses | 269 (17.5) | 1266 (82.5) | 0.63 (0.46–0.86) | 0.004 | 0.63 (0.43–0.93) | 0.019 |
| Others | 76 (18.4) | 337 (81.6) | 0.67 (0.46–0.98) | 0.038 | 0.59 (0.37–0.95) | 0.031 |
| Indications | ||||||
| HM 1 | 38 (5.9) | 611 (94.1) | 1 | - | 1 | |
| HM 2 | 5 (1.9) | 251 (98.1) | 0.32 (0.12–0.82) | 0.018 | 0.39 (0.15–1.01) | 0.051 |
| HM 3 | 129 (58.4) | 92 (41.6) | 22.5 (14.8–34.4) | <0.001 | 34.0 (21.5–53.6) | <0.001 |
| HM 4 | 203 (35.1) | 376 (64.9) | 8.7 (6.0–12.6) | <0.001 | 9.95 (6.8–14.6) | <0.001 |
| HM 5 | 33 (6.7) | 460 (93.3) | 1.15 (0.71–1.87) | 0.561 | 1.41 (0.86–2.30) | 0.175 |
| Parameters | Capital City Hospital (N = 1279) | Regional Hospital (N = 919) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Compliance | OR (C.I) | p | aOR (C.I) | p | Compliance | OR (C.I) | p | aOR (C.I) | p | |||
| Yes (%) 217 (17) | No (%) 1062 (83) | Yes (%) 191 (20.8) | No (%) 728 (79.2) | |||||||||
| Wards | ||||||||||||
| Medical | 48 (20.7) | 184 (79.3) | 1 | - | 1 | - | 27 (22.3) | 94 (77.7) | 1 | - | - | - |
| Surgical | 34 (11.7) | 257 (88.3) | 0.51 (0.31–0.82) | 0.005 | 0.58 (0.32–1.05) | 0.072 | 29 (19.5) | 120 (80.5) | 0.84 (0.47–1.52) | 0.566 | - | - |
| Paediatric | 21 (9.7) | 195 (90.3) | 0.41 (0.24–0.72) | 0.002 | 0.36 (0.19–0.68) | 0.002 | 35 (19.8) | 142 (80.2) | 0.86 (0.49–1.51) | 0.596 | - | - |
| Maternity | 40 (20.2) | 158 (79.8) | 0.97 (0.61–1.55) | 0.901 | 1.30 (0.71–2.38) | 0.393 | 51 (22.6) | 175 (77.4) | 1.01 (0.60–1.72) | 0.975 | - | - |
| A & E | 15 (7.7) | 179 (92.3) | 0.32 (0.17–0.59) | <0.001 | 0.30 (0.15–0.61) | 0.001 | 30 (18.1) | 136 (81.9) | 0.77 (0.43–1.38) | 0.374 | - | - |
| Others | 59 (39.9) | 89 (60.1) | 2.5 (1.6–4.0) | <0.001 | 5.7 (3.0–10.9) | <0.001 | 19 (23.8) | 61 (76.2) | 1.08 (0.56–2.12) | 0.813 | - | - |
| Healthcare workers | ||||||||||||
| Doctors | 43 (30.7) | 97 (69.3) | 1 | - | 1 | - | 20 (18.2) | 90 (81.8) | 1 | - | 1 | - |
| Nurses | 166 (15.1) | 935 (84.9) | 0.40 (0.27–0.59) | <0.001 | 0.24 (0.14–0.44) | <0.001 | 103 (23.7) | 331 (76.3) | 1.4 (0.82–2.39) | 0.215 | 1.3 (0.7–2.4) | 0.376 |
| Others | 8 (21.1) | 30 (78.9) | 0.60 (0.25–1.42) | 0.246 | 0.59 (0.20–1.76) | 0.345 | 68 (18.1) | 307 (81.9) | 0.99 (0.57–1.73) | 0.991 | 0.7 (0.4–1.4) | 0.363 |
| Indications | ||||||||||||
| HM 1 | 3 (0.9) | 312 (99.1) | 1 | - | 1 | - | 35 (10.5) | 299 (89.5) | 1 | - | 1 | - |
| HM 2 | 1 (0.6) | 163 (99.4) | 0.64 (0.06–6.18) | 0.698 | 1.0 (0.1–9.9) | 0.998 | 4 (4.3) | 88 (95.7) | 0.39 (0.13–1.12) | 0.081 | 0.4 (0.1–1.1) | 0.070 |
| HM 3 | 71 (45.8) | 84 (54.2) | 87 (27–286) | <0.001 | 243 (68–862) | <0.001 | 58 (87.9) | 8 (12.1) | 61.9 (27.3 –140.3) | <0.001 | 66 (29–152) | <0.001 |
| HM 4 | 117 (38.5) | 187 (61.5) | 65 (20–207) | <0.001 | 125 (36–423) | <0.001 | 86 (31.3) | 189 (68.7) | 3.9 (2.52–6.0) | <0.001 | 3.9 (2.5–6.0) | <0.001 |
| HM 5 | 25 (7.3) | 316 (92.7) | 8.2 (2.5–27.5) | 0.001 | 13 (4–47) | <0.001 | 8 (5.3) | 144 (94.7) | 0.47 (0.21–1.05) | 0.066 | 0.5 (0.2–1.0) | 0.060 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lakoh, S.; Firima, E.; Williams, C.E.E.; Conteh, S.K.; Jalloh, M.B.; Sheku, M.G.; Adekanmbi, O.; Sevalie, S.; Kamara, S.A.; Kamara, M.A.S.; et al. An Intra-COVID-19 Assessment of Hand Hygiene Facility, Policy and Staff Compliance in Two Hospitals in Sierra Leone: Is There a Difference between Regional and Capital City Hospitals? Trop. Med. Infect. Dis. 2021, 6, 204. https://doi.org/10.3390/tropicalmed6040204
Lakoh S, Firima E, Williams CEE, Conteh SK, Jalloh MB, Sheku MG, Adekanmbi O, Sevalie S, Kamara SA, Kamara MAS, et al. An Intra-COVID-19 Assessment of Hand Hygiene Facility, Policy and Staff Compliance in Two Hospitals in Sierra Leone: Is There a Difference between Regional and Capital City Hospitals? Tropical Medicine and Infectious Disease. 2021; 6(4):204. https://doi.org/10.3390/tropicalmed6040204
Chicago/Turabian StyleLakoh, Sulaiman, Emmanuel Firima, Christine Ellen Elleanor Williams, Sarah K. Conteh, Mohamed Boie Jalloh, Mohamed Gbeshay Sheku, Olukemi Adekanmbi, Stephen Sevalie, Sylvia Adama Kamara, Mohamed Akmed Salim Kamara, and et al. 2021. "An Intra-COVID-19 Assessment of Hand Hygiene Facility, Policy and Staff Compliance in Two Hospitals in Sierra Leone: Is There a Difference between Regional and Capital City Hospitals?" Tropical Medicine and Infectious Disease 6, no. 4: 204. https://doi.org/10.3390/tropicalmed6040204
APA StyleLakoh, S., Firima, E., Williams, C. E. E., Conteh, S. K., Jalloh, M. B., Sheku, M. G., Adekanmbi, O., Sevalie, S., Kamara, S. A., Kamara, M. A. S., Barrie, U., Kamara, G. N., Yi, L., Guo, X., Haffner, C., Kamara, M. N., Jiba, D. F., Namanaga, E. S., Maruta, A., ... Russell, J. B. W. (2021). An Intra-COVID-19 Assessment of Hand Hygiene Facility, Policy and Staff Compliance in Two Hospitals in Sierra Leone: Is There a Difference between Regional and Capital City Hospitals? Tropical Medicine and Infectious Disease, 6(4), 204. https://doi.org/10.3390/tropicalmed6040204








