Laser Scanning Confocal Microscopy Was Used to Validate the Presence of Burkholderia pseudomallei or B. mallei in Formalin-Fixed Paraffin Embedded Tissues
Abstract
1. Introduction
2. Materials and Methods
2.1. Bacterial Strains, B. pseudomallei K96243 Antibody, and Human Tissue
2.2. Growth of Bacterial Strains and Antigen Preparation
2.3. Production of Rabbit Polyclonal Antibodies Against B. mallei or B. pseudomallei
2.4. Immunohistochemistry
2.5. Immunofluorescence and Laser Scanning Confocal Microscopy Imaging
3. Results
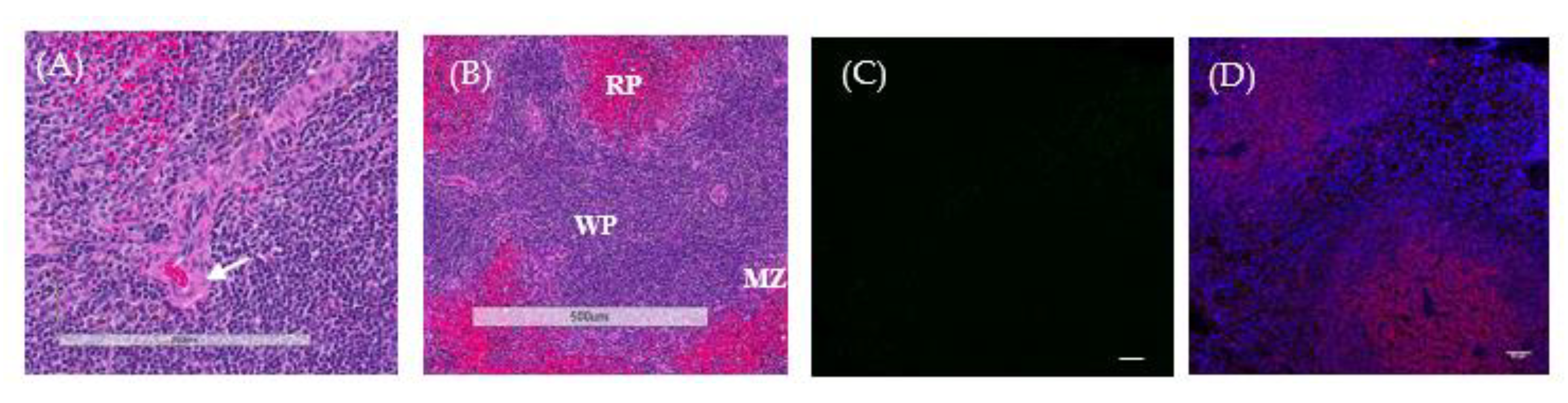
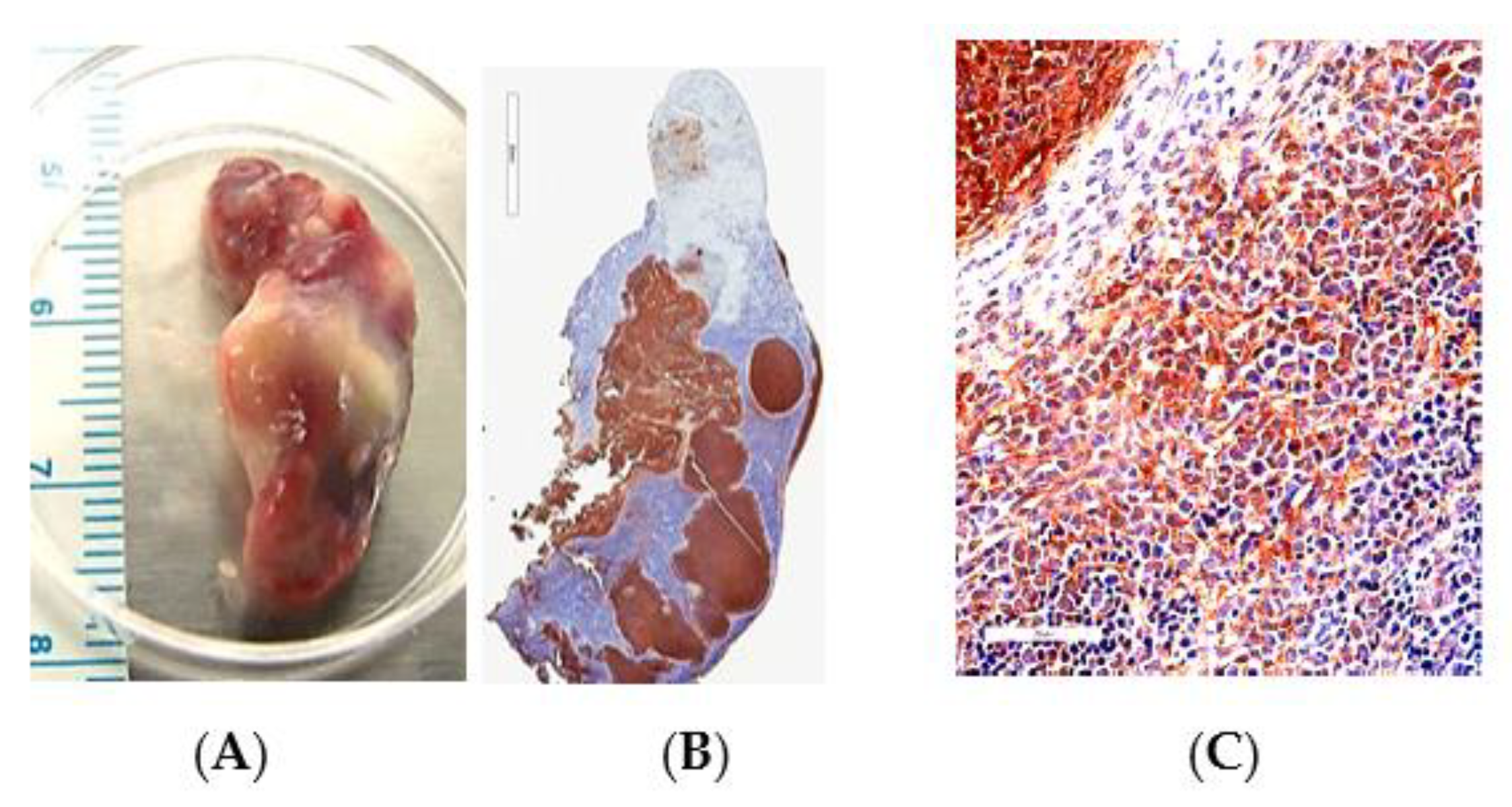
3.1. IHC Analysis of FFPE by Bright Field Microscopy
3.2. LSCM Analysis of FFPE Tissue
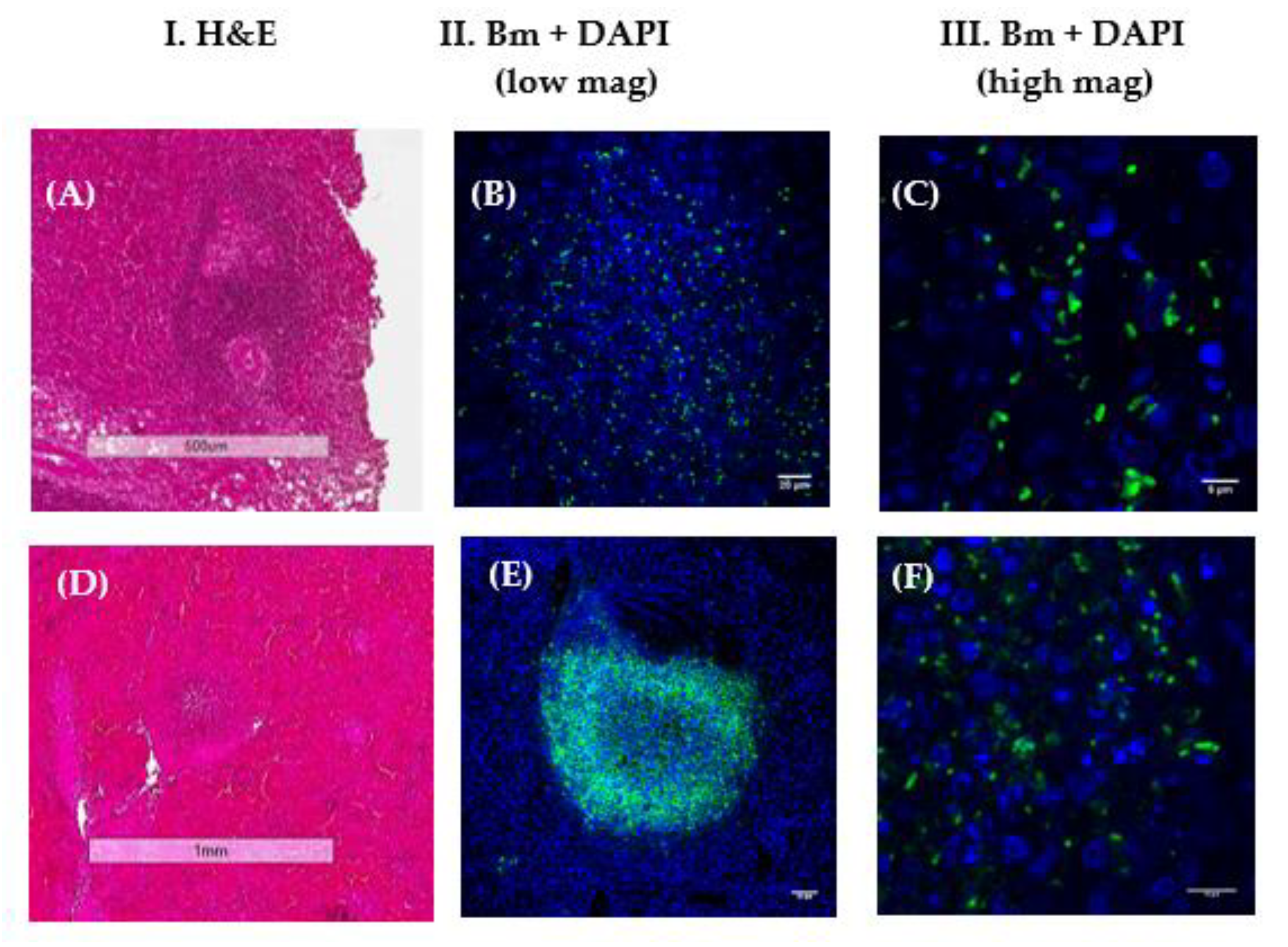
3.2.1. LSCM Analysis of Murine Tissue from Animal Model Studies
3.2.2. LSCM Analysis of Nonhuman Primate (NHP) Tissue
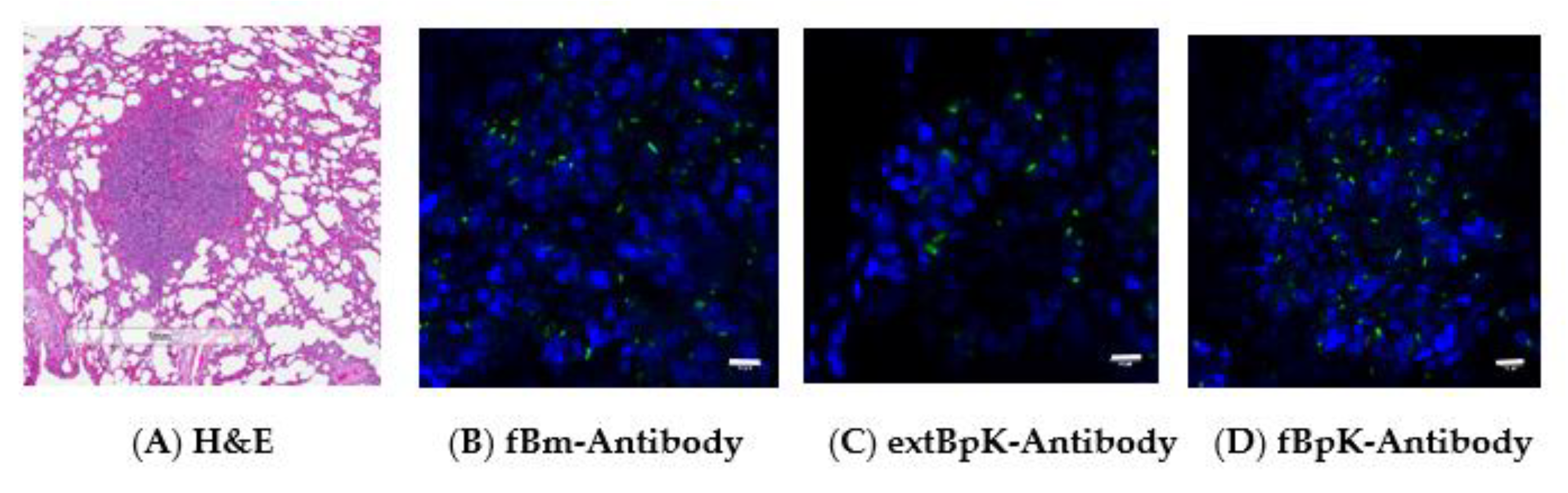
3.2.3. LSCM Analysis of Suspected Human Tissue
3.2.4. Comparison of Polyclonal Antibodies Used to Examine FFPE Tissue by LSCM
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| ELISA Titer a | |||
|---|---|---|---|
| Antigen Used for Antibody Production | Type Antigen b | ||
| IRBpK | fBpK | IRBmFMH | |
| A. | |||
| None (naïve rabbit serum) | 6400 (1.00) | 126 (1.26) | 1008 (1.26) |
| BpK whole-cell extract (extBpK) | 507,968 (1.26) | 806,349 (1.26) | 6,400,000 (1.00) |
| Formalin-treated Bm GB18 (fBm) | 100,794 (1.26) | 320,000 (1.00) | 1,015,937 (1.26) |
| B. | |||
| None (naïve rabbit serum) | 5080 (1.26) | 159 (1.26) | 2016 (1.26) |
| Formalin-treated BpK (fBpK) (no. 1) c | 1,600,000 (1.00) | 6,400,000 (1.00) | 2,560,000 (1.00) |
| Formalin-treated BpK (fBpK) (no. 2) | 1,600,000 (1.00) | 3,200,000 (1.00) | 4,063,747 (1.26) |
References
- Limmathurotsakul, D.; Golding, N.; Dance, D.A.B.; Messina, J.P.; Pigott, D.M.; Moyes, C.L.; Rolim, D.B.; Bertherat, E.; Day, N.P.J.; Peacock, S.J.; et al. Predicted globul distribution of Burkholderia pseudomallei and burden of melioidosis. Nat. Microbiol. 2016, 1, 15008. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.C.; Jacups, S.P.; Gal, D.; Mayo, M.; Currie, B.J. Extreme weather events and environmental contamination are associated with case-clusters of melioidosis in the Northern Territory of Australia. Int. J. Epidemiol. 2005, 35, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Suputtamongkol, Y.; Chaowagul, W.; Chetchotisakd, P.; Lertpatanasuwun, N.; Intaranongpai, S.; Ruchutrakool, T.; Budhsarawong, D.; Mootsikapun, P.; Wuthiekanun, V.; Teerawatasook, N.; et al. Risk factors for melioidosis and bacteremic melioidosis. Clin. Infect. Dis. 1999, 29, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Currie, B.J.; Jacups, S.P.; Cheng, A.C.; Fisher, D.A.; Anstey, N.M.; Huffam, S.E.; Krause, V.L. Melioidosis epidemiology and risk factors from a prospective whole-population study in northern Australia. Trop. Med. Int. Health 2004, 9, 1167–1174. [Google Scholar] [CrossRef]
- Kunnathuparambil, S.G.; Sathar, S.A.; Tank, D.C.; Sreesh, S.; Mukunda, M.; Narayanan, P.; Vinayakumar, K.R. Splenic abscess due to chronic melioidosis in a patient previously misdiagnosed as tuberculosis. Ann. Gastroenterol. 2013, 26, 77–79. [Google Scholar]
- Welkos, S.L.; Klimko, C.P.; Kern, S.J.; Bearss, J.J.; Bozue, J.A.; Bernhards, R.C.; Trevino, S.R.; Waag, D.M.; Amemiya, K.; Worsham, P.L.; et al. Characterization of Burkholderia pseudomallei strains using a murine intraperitoneal infection model and in vitro macrophage assay. PLoS ONE 2015, 10, e0124667. [Google Scholar] [CrossRef]
- Bearss, J.J.; Hunter, M.; Dankmeyer, J.L.; Fritts, K.A.; Klimko, C.P.; Weaver, C.H.; Shoe, J.L.; Quirk, A.V.; Toothman, R.G.; Webster, W.M.; et al. Characterization of pathogenesis of and immune response to Burkholderia pseudomallei K96243 using both inhalational and intraperitoneal infection models in BALB/c and C57BL/6 mice. PLoS ONE 2017, 12, e0172627. [Google Scholar] [CrossRef]
- Trevino, S.R.; Klimko, C.P.; Reed, M.C.; Aponte-Cuadrado, M.J.; Hunter, M.; Meyer, J.R.; Dankmeyer, J.L.; Biryukov, S.S.; Quirk, A.V.; Fritts, K.A.; et al. Disease progression in mice exposed to low-doses of aerosolized clinical isolates of Burkholderia pseudomallei. PLoS ONE 2018, 13, e0208277. [Google Scholar] [CrossRef]
- Amemiya, K.; Dankmeyer, J.L.; Bearss, J.J.; Zeng, X.; Stonier, S.W.; Soffler, C.; Cote, C.K.; Welkos, S.L.; Fetterer, D.P.; Chance, T.B.; et al. Dysregulation of TNF-α and IFN-γ expression is a common host immune response in a chronically infected mouse model of melioidosis when comparing multiple human strains of Burkholderia pseudomallei. BMC Immunol. 2020, 21, 1–22. [Google Scholar] [CrossRef]
- Steinmetz, I.; Rohde, M.; Brenneke, B. Purification and characterization of an exopolysaccharide of Burkholderia (Pseudomonas) pseudomallei. Infect. Immun. 1995, 63, 3959–3965. [Google Scholar] [CrossRef]
- Anuntagool, N.; Sirisinha, S. Antigenic relatedness between Burkholderia pseudomallei and Burkholderia mallei. Microbiol. Immunol. 2002, 46, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Duval, B.D.; Elrod, M.G.; Gee, J.E.; Chantratita, N.; Tandhavanant, S.; Limmathurotsakul, D.; Hoffmaster, A.R. Short report: Evaluation of a latex agglutination assay for the identification of Burkholderia pseudomallei and Burkholderia mallei. Am. J. Trop. Med. Hyg. 2014, 90, 1043–1046. [Google Scholar] [CrossRef] [PubMed]
- Fritz, D.L.; Vogel, P.; Brown, D.R.; Waag, D.M. The hamster model of intraperitoneal Burkholderia mallei (Glanders). Vet. Pathol. 1999, 36, 276–291. [Google Scholar] [CrossRef] [PubMed]
- Amemiya, K.; Bush, G.V.; DeShazer, D.; Waag, D.M. Nonviable Burkholderia mallei induces a mixed Th1- and Th2-like cytokine response in BALB/c mice. Infect. Immun. 2002, 70, 2319–2325. [Google Scholar] [CrossRef] [PubMed]
- Jonkman, J.; Brown, C.M. Any way you slice it-a comparison of confocal microscopy techniques. J. Biomol. Tech. 2015, 26, 54–65. [Google Scholar] [CrossRef]
- Wong, K.T.; Vadivelu, J.; Puthucheary, S.D.; Tan, K.L. An immunohistochemical method for the diagnosis of melioidosis. Pathology 1996, 28, 188–191. [Google Scholar] [CrossRef]
- Glaros, T.G.; Blancett, C.D.; Bell, T.M.; Natesan, M.; Ulrich, R.G. Serum biomarkers of Burkholderia mallei infection elucidated by proteomic imaging of skin and lung abscesses. Clin. Proteom. 2015, 12, 7. [Google Scholar] [CrossRef]
- Hagen, R.M.; Frickmann, H.; Elschner, M.; Melzer, F.; Neubauer, H.; Gauthier, Y.P.; Racz, P.; Poppert, S. Rapid identification of Burkholderia pseudomallei and Burkholderia mallei by fluorescence in situ hybridization (FISH) from culture and paraffin-embedded tissue samples. Int. J. Med. Microbiol. 2011, 301, 585–590. [Google Scholar] [CrossRef]
- Eu, L.C.; Ong, K.C.; Hiu, J.; Vadivelu, J.; Nathan, S.; Wong, K.T. In situ hybridization to detect and identify Burkholderia pseudomallei in human melioidosis. Mod. Pathol. 2014, 27, 657–664. [Google Scholar] [CrossRef][Green Version]
- Hagen, R.M.; Gauthier, Y.P.; Sprague, L.D.; Vidal, D.R.; Zysk, G.; Finke, E.-J.; Neubauer, H. Strategies for PCR based detection of Burkholderia pseudomallei DNA in paraffin was embedded tissues. J. Clin. Pathol. Mol. Pathol. 2002, 55, 398–400. [Google Scholar] [CrossRef]
- Obersteller, S.; Neubauer, H.; Hagen, R.M.; Frickmann, H. Comparison of five commercial nucleic acid extraction kits for the PCR-based detection of Burkholderia pseudomallei DNA in formalin-fixed, paraffin-embedded tissues. Eur. J. Microbiol. Immunol. 2016, 6, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Gauthier, Y.P.; Hagen, R.M.; Brochier, G.S.; Neubauer, H.; Splettstoesser, W.D.; Finke, E.-J.; Vidal, D.R. Study on the pathophysiology of experimental Burkholderia pseudomallei infection in mice. FEMS Immunol. Med. Microbiol. 2001, 30, 53–63. [Google Scholar] [CrossRef]
- Vadivelu, J.; Vellasamy, K.M.; Thimma, J.; Mariappan, V.; Kang, W.-T.; Choh, L.-C.; Shankar, E.M.; Wong, K.T. Survival and intra-nuclear trafficking of Burkholderia pseudomallei: Strategies of evasion from immune surveillance? PLoS Negl. Trop. Dis. 2017, 11, e0005241. [Google Scholar] [CrossRef] [PubMed]
- Bozue, J.A.; Chaudhury, S.; Amemiya, K.; Chua, J.; Cote, C.K.; Toothman, R.G.; Dankmeyer, J.L.; Klimko, C.P.; Wilhelmsen, C.L.; Raymond, J.W.; et al. Phenotypic characterization of a novel virulence-factor deletion strain of Burkholderia mallei that provides partial protection against inhalational glanders in mice. Front. Cell. Infect. Microbiol. 2016, 6, 21. [Google Scholar] [CrossRef] [PubMed]
- Chua, J.; Senft, J.L.; Lockett, S.J.; Brett, P.J.; Burtnick, M.N.; DeShazer, D.; Friedlander, A.M. pH alkalinization by chloroquine suppresses pathogenic Burkholderia type 6 secretion system 1 and multinucleated giant cells. Infect. Immun. 2017, 85. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Fang, Y.; Zhu, P.; Ren, C.-Y.; Chen, H.; Gu, J.; Jia, Y.-P.; Wang, K.; Tong, W.-D.; Zhang, W.-J.; et al. Burkholderia pseudomallei survival in lung epithelial cells benefits from miRNA-mediated suppression of ATG10. Autophagy 2015, 11, 1293–1307. [Google Scholar]
- Saikh, K.U.; Dankmeyer, J.L.; Zeng, X.; Ulrich, R.G.; Amemiya, K. An increase in intracellular p62/NBR1 and persistence of Burkholderia mallei and B. pseudomallei in infected mice linked to autophagy deficiency. Immun. Inflamm. Dis. 2019, 7, 7–21. [Google Scholar] [CrossRef]
- Erokhina, M.V.; Lepekha, L.N.; Voronezhskaya, E.E.; Nezlin, L.P.; Avdienko, V.G.; Ergeshov, A.E. Application of laser scanning confocal microscopy for the visualization of M. tuberculosis in lung tissue samples with weak Ziehl-Neelsen staining. J. Clin. Med. 2019, 8, 1185. [Google Scholar] [CrossRef]
- Jones, S.M.; Ellis, J.F.; Russell, P.; Griffin, K.F.; Oyston, P.C.F. Passive protection against Burkholderia pseudomallei infection in mice by monoclonal antibodies against capsular polysaccharide, lipopolysaccharide or proteins. J. Med. Microbiol. 2002, 51, 1055–1062. [Google Scholar] [CrossRef]
- Trevino, S.R.; Permenter, A.R.; England, M.J.; Parthasarathy, N.; Gibbs, P.H.; Waag, D.M.; Chanh, T.C. Monoclonal antibodies passively protect BALB/c mice against Burkholderia mallei aerosol challenge. Infect. Immun. 2006, 74, 1958–1961. [Google Scholar] [CrossRef]



| Figure No. | Strain/Species a | Exposure to Bp or Bm Strain | Amount of Exposure (CFU) b | Route of Infection | Tissue | Time Post-Infection (Days) | CFU/g Tissue | Source of Tissue |
|---|---|---|---|---|---|---|---|---|
| 2 | C57BL/6 | Bp 22 | 127 | Aerosol | Spleen | 47 | na d | This ref |
| 3 | BALB/c | Bp K96243 | 3.0 × 104 | IPc | Dorsalthoracic | 22 | na | [7] |
| 3 | BALB/c | Bp K96243 | 5.0 | Aerosol | Spleen | 15 | na | [7] |
| 3 | BALB/c | Bp K96243 | 3.0 × 104 | IP | Lumbar | 22 | na | [7] |
| 3 | BALB/c | Bp K96243 | 5.0 | Aerosol | Lung | 19 | na | [7] |
| 3 | C57BL/6 | Bp K96243 | 18.0 | Aerosol | Liver | 28 | na | [7] |
| 4 | AGM | Bp HBPUB10134a | 319 | Nose only | Lung | 13 | 158,489 | This Ref |
| 4 | AGM | Bp HBPUB10134a | 319 | Nose only | Spleen | 13 | 5,011,872 | This Ref |
| 4 | AGM | Bp HBPUB10134a | 420 | Nose only | Lung | 5 | 1,584,893 | This Ref |
| 4 | Rhesus | Bp HBPUB10134a | 286 | Nose only | Lung | 13 | 15,848,931 | This Ref |
| 4 | Rhesus | Bp HBPUB10134a | 531 | Nose only | Lung | 42 | 0 | This Ref |
| 5 | Human | B. mallei | Unknown | Unknown | Spleen | Unknown | Unknown | Unknown |
| 6 | AGM | B. mallei | 2.10 × 107 | Head only | Lung | 14 | Unknown | This Ref |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amemiya, K.; Zeng, X.; Bearss, J.J.; Cote, C.K.; Soffler, C.; Bernhards, R.C.; Dankmeyer, J.L.; Ribot, W.J.; Trevino, S.R.; Welkos, S.L.; et al. Laser Scanning Confocal Microscopy Was Used to Validate the Presence of Burkholderia pseudomallei or B. mallei in Formalin-Fixed Paraffin Embedded Tissues. Trop. Med. Infect. Dis. 2020, 5, 65. https://doi.org/10.3390/tropicalmed5020065
Amemiya K, Zeng X, Bearss JJ, Cote CK, Soffler C, Bernhards RC, Dankmeyer JL, Ribot WJ, Trevino SR, Welkos SL, et al. Laser Scanning Confocal Microscopy Was Used to Validate the Presence of Burkholderia pseudomallei or B. mallei in Formalin-Fixed Paraffin Embedded Tissues. Tropical Medicine and Infectious Disease. 2020; 5(2):65. https://doi.org/10.3390/tropicalmed5020065
Chicago/Turabian StyleAmemiya, Kei, Xiankun Zeng, Jeremy J. Bearss, Christopher K. Cote, Carl Soffler, Robert C. Bernhards, Jennifer L. Dankmeyer, Wilson J. Ribot, Sylvia R. Trevino, Susan L. Welkos, and et al. 2020. "Laser Scanning Confocal Microscopy Was Used to Validate the Presence of Burkholderia pseudomallei or B. mallei in Formalin-Fixed Paraffin Embedded Tissues" Tropical Medicine and Infectious Disease 5, no. 2: 65. https://doi.org/10.3390/tropicalmed5020065
APA StyleAmemiya, K., Zeng, X., Bearss, J. J., Cote, C. K., Soffler, C., Bernhards, R. C., Dankmeyer, J. L., Ribot, W. J., Trevino, S. R., Welkos, S. L., Worsham, P. L., & Waag, D. M. (2020). Laser Scanning Confocal Microscopy Was Used to Validate the Presence of Burkholderia pseudomallei or B. mallei in Formalin-Fixed Paraffin Embedded Tissues. Tropical Medicine and Infectious Disease, 5(2), 65. https://doi.org/10.3390/tropicalmed5020065




