An Innovative Public–Private Mix Model for Improving Tuberculosis Care in Vietnam: How Well Are We Doing?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
2.2.1. TB Control Program in Vietnam
2.2.2. PPM Models
2.2.3. PPM Model at HIGH
2.2.4. Recording and Reporting
2.3. Study Population
2.4. Data Variables and Sources
2.5. Analysis and Statistics
2.6. Ethics Approval
3. Results
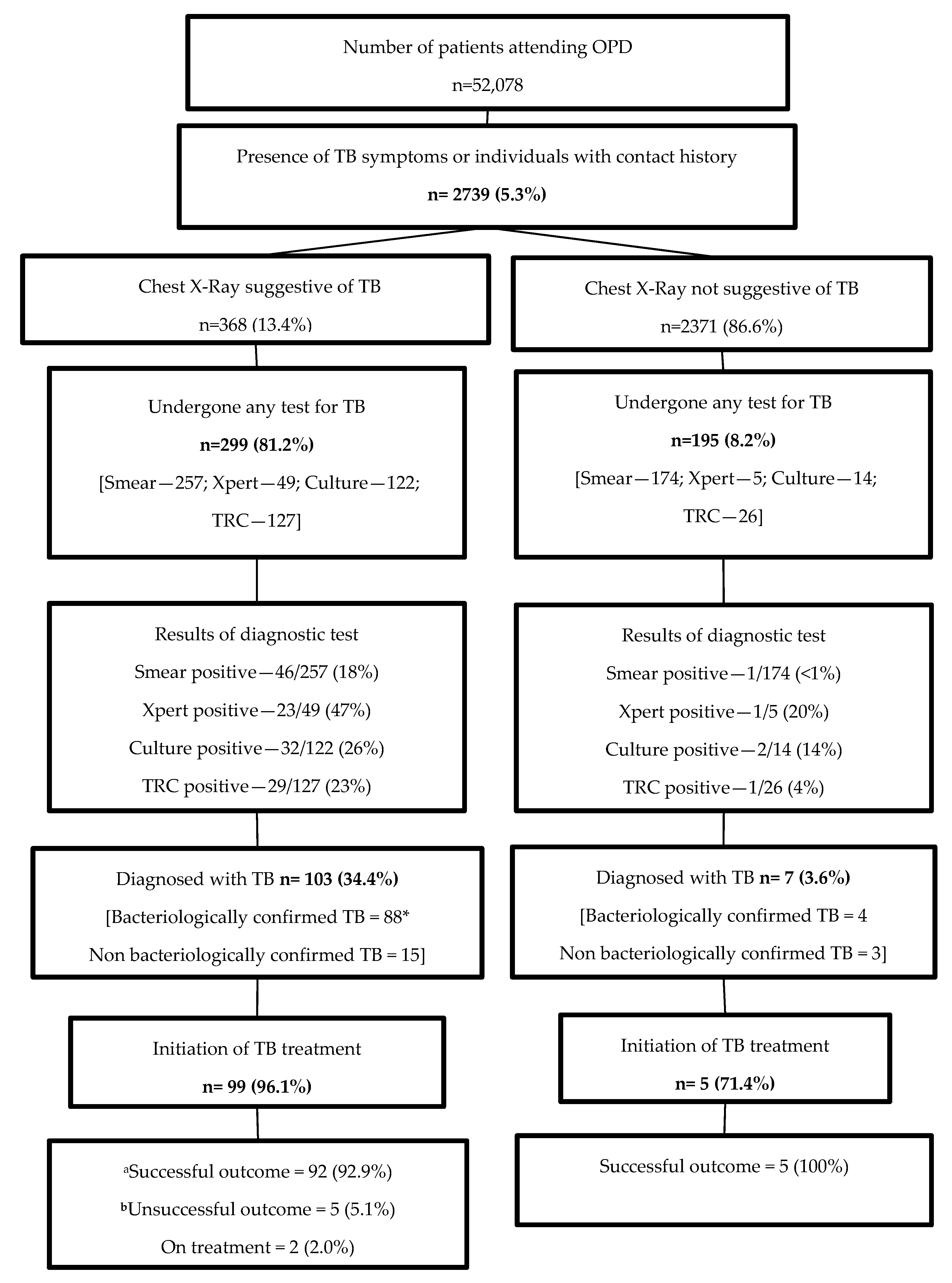
3.1. Cascade of Care
3.2. Factors Associated with ‘Not Getting Tested for TB’
3.3. Factors Associated with TB Diagnosis
3.4. Treatment Outcomes
3.5. Median Delays
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Global Tuberculosis Report. 2019. Available online: https://www.who.int/tb/publications/global_report/en/ (accessed on 18 October 2019).
- World Health Organization. The End TB Strategy. Available online: https://www.who.int/tb/strategy/end-tb/en/ (accessed on 14 October 2019).
- Ortblad, K.F.; Lozano, R.; Murray, C.J. An alternative estimation of tuberculosis incidence from 1980 to 2010: Methods from the Global Burden of Disease 2010. Lancet 2013, 381, S104. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Stop TB Partnership. In The Paradigm Shift 2016–2020: Global Plan to End TB; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Chin, D.P.; Hanson, C.L. Finding the Missing Tuberculosis Patients. J. Infect. Dis. 2017, 216, S675–S678. [Google Scholar] [CrossRef]
- Sulis, G.; Pai, M. Missing tuberculosis patients in the private sector: Business as usual will not deliver results. Public Health Action 2017, 7, 80–81. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lönnroth, K.; Uplekar, M.; Arora, V.K.; Juvekar, S.; Lan, N.T.N.; Mwaniki, D.; Pathania, V. Public-private mix for DOTS implementation: What makes it work? Bull World Health Organ 2004, 82, 580–586. [Google Scholar]
- Oanh, T.T.M.; Phượng, H.T.; Phương, N.K.; Tuấn, K.A.; Thủy, N.T.; Mai, V.L.; My, Đ.T. Current Situation Assessment and Recommended Solutions to Strengthen Public Private Partnership in Health Sector; Health Strategy and Policy Institute: Ha Noi, Vietnam, 2011. [Google Scholar]
- Lönnroth, K.; Thuong, L.M.; Lambregts, K.; Quy, H.T.; Diwan, V.K. Private tuberculosis care provision associated with poor treatment outcome: Comparative study of a semi-private lung clinic and the NTP in two urban districts in Ho Chi Minh City, Vietnam. National Tuberculosis Programme. Int. J. Tuberc. Lung. Dis. 2003, 7, 165–171. [Google Scholar] [PubMed]
- Lönnroth, K.; Lambregts, K.; Nhien, D.T.; Quy, H.T.; Diwan, V.K. Private pharmacies and tuberculosis control: A survey of case detection skills and reported anti-tuberculosis drug dispensing in private pharmacies in Ho Chi Minh City, Vietnam. Int. J. Tuberc. Lung. Dis. 2000, 4, 1052–1059. [Google Scholar] [CrossRef] [PubMed]
- Lönnroth, K.; Thuong, L.M.; Linh, P.D.; Diwan, V.K. Delay and discontinuity—A survey of TB patients’ search of a diagnosis in a diversified health care system. Int. J. Tuberc. Lung. Dis. 1999, 3, 992–1000. [Google Scholar] [PubMed]
- Quy, H.T.; Lan, N.T.N.; Lönnroth, K.; Buu, T.N.; Dieu, T.T.N.; Hai, L.T. Public-private mix for improved TB control in Ho Chi Minh City, Vietnam: An assessment of its impact on case detection. Int. J. Tuberc. Lung. Dis. 2003, 7, 464–471. [Google Scholar] [PubMed]
- Quy, H.T.; Lönnroth, K.; Lan, N.T.N.; Buu, T.N. Treatment results among tuberculosis patients treated by private lung specialists involved in a public-private mix project in Vietnam. Int. J. Tuberc. Lung. Dis. 2003, 7, 1139–1146. [Google Scholar] [PubMed]
- The World Bank Vietnam Continues to Reduce Poverty, According to WB Report. Available online: https://www.worldbank.org/en/news/press-release/2018/04/05/vietnam-continues-to-reduce-poverty-according-to-world-bank-report (accessed on 14 October 2019).
- UNITAID. Tuberculosis Diagnostics Technology Lanscape. 2017, pp. 1–90. Available online: https://unitaid.org/assets/2017-Unitaid-TB-Diagnostics-Technology-Landscape.pdf (accessed on 6 November 2019).
- Lei, X.; Liu, Q.; Escobar, E.; Philogene, J.; Zhu, H.; Wang, Y.; Tang, S. Public–private mix for tuberculosis care and control: A systematic review. Int. J. Infect. Dis. 2015, 34, 20–32. [Google Scholar] [CrossRef] [PubMed]
- Khan, B.J.; Kumar, A.M.V.; Stewart, A.; Khan, N.M.; Selvaraj, K.; Fatima, R.; Samad, Z. Alarming rates of attrition among tuberculosis patients in public-private facilities in Lahore, Pakistan. Public Health Action 2017, 7, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Lal, S.S.; Sahu, S.; Wares, F.; Lönnroth, K.; Chauhan, L.S.; Uplekar, M. Intensified scale-up of public-private mix: A systems approach to tuberculosis care and control in India. Int. J. Tuberc. Lung. Dis. 2011, 15, 97–104. [Google Scholar] [PubMed]
- Chengsorn, N.; Bloss, E.; Anekvorapong, R.; Anuwatnonthakate, A.; Wattanaamornkiat, W.; Komsakorn, S.; Moolphate, S.; Limsomboon, P.; Kaewsa-ard, S.; Nateniyom, S.; et al. Tuberculosis services and treatment outcomes in private and public health care facilities in Thailand, 2004–2006. Int. J. Tuberc. Lung. Dis. 2009, 13, 888–894. [Google Scholar] [PubMed]
- Thet Lwin, Z.M.; Sahu, S.K.; Owiti, P.; Chinnakali, P.; Majumdar, S.S. Public-private mix for tuberculosis care and control in Myanmar: A strategy to scale up? Public Health Action 2017, 7, 15–20. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Khan, A.J.; Khowaja, S.; Khan, F.S.; Qazi, F.; Lotia, I.; Habib, A.; Mohammed, S.; Khan, U.; Amanullah, F.; Hussain, H.; et al. Engaging the private sector to increase tuberculosis case detection: An impact evaluation study. Lancet Infect. Dis. 2012, 12, 608–616. [Google Scholar] [CrossRef]
- Creswell, J.; Khowaja, S.; Codlin, A.; Hashmi, R.; Rasheed, E.; Khan, M.; Durab, I.; Mergenthaler, C.; Hussain, O.; Khan, F.; et al. An evaluation of systematic tuberculosis screening at private facilities in Karachi, Pakistan. PLoS ONE 2014, 9, e93858. [Google Scholar] [CrossRef] [PubMed]
- Van’t Hoog, A.H.; Onozaki, I.; Lonnroth, K. Choosing algorithms for TB screening: A modelling study to compare yield, predictive value and diagnostic burden. BMC Infect. Dis. 2014, 14, 532. [Google Scholar] [CrossRef] [PubMed]
- Hoa, N.B.; Sy, D.N.; Nhung, N.V.; Tiemersma, E.W.; Borgdorff, M.W.; Cobelens, F.G.J. National survey of tuberculosis prevalence in Viet Nam. Bull World Health Organ 2010, 88, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.K.A.; Dewan, P.K.; Nair, P.K.J.; Frieden, T.R.; Sahu, S.; Wares, F.; Laserson, K.; Wells, C.; Granich, R.; Chauhan, L.S. Improved tuberculosis case detection through public-private partnership and laboratory-based surveillance, Kannur District, Kerala, India, 2001–2002. Int. J. Tuberc. Lung. Dis. 2005, 9, 870–876. [Google Scholar] [PubMed]
| Characteristic | Number | (%) |
|---|---|---|
| Total | 2739 | (100.0) |
| Age group (years) | ||
| 15-44 | 1170 | (42.7) |
| 45-64 | 1084 | (39.6) |
| ≥ 65 | 485 | (17.7) |
| Gender | ||
| Male | 1372 | (50.1) |
| Female | 1367 | (49.9) |
| Self-reported HIV status | ||
| Negative | 596 | (21.8) |
| Positive | 4 | (0.1) |
| Unknown | 2139 | (78.1) |
| Self-reported diabetes | ||
| No | 1699 | (62.0) |
| Yes | 161 | (5.9) |
| Unknown | 879 | (32.1) |
| Presenting symptoms | ||
| Cough (any duration) * | 2240 | (81.8) |
| Chest pain and dyspnea | 1926 | (70.3) |
| Fever | 418 | (15.3) |
| Fatigue | 1521 | (55.5) |
| Sweating at night | 51 | (1.9) |
| Unexplained weight loss | 133 | (4.9) |
| History of contact of TB | 34 | (1.2) |
| Characteristic | Total | Not Tested for TB# | RR | (95%CI) | aRR | (95%CI) | |
|---|---|---|---|---|---|---|---|
| n | (%) | ||||||
| Total | 368 | 69 | (18.7) | - | - | ||
| Age (years) | |||||||
| 15–44 | 138 | 27 | (19.6) | 0.89 | (0.52–1.51) | 1.06 | (0.97–1.08) |
| 45–64 | 148 | 24 | (16.2) | 0.74 | (0.43–1.28) | 1.01 | (0.96–1.07) |
| 65 and above | 82 | 18 | (21.9) | 1 | 1 | ||
| Gender | |||||||
| Male | 203 | 30 | (14.8) | 1 | 1 | ||
| Female | 165 | 39 | (23.6) | 1.60 | (1.04–2.46) | 1.02 | (0.99–1.06) |
| Self-reported HIV status | |||||||
| Negative | 195 | 24 | (12.3) | - | - | ||
| Positive | 1 | 0 | (0.0) | - | - | ||
| Unknown | 172 | 45 | (25.2) | - | - | ||
| Self-reported diabetes | |||||||
| No | 280 | 49 | (17.5) | 0.72 | (0.39–1.34) | 1.03 | (0.94–1.13) |
| Yes | 37 | 9 | (24.3) | 1 | 1 | ||
| Unknown | 51 | 11 | (21.6) | 0.89 | (0.41–1.92) | 1.17 | (1.06–1.28) |
| Cough | |||||||
| No | 68 | 20 | (29.4) | 1.80 | (1.15–2.82) | 1.07 | (1.02–1.28) |
| Present | 300 | 49 | (16.3) | 1 | 1 | ||
| Fever | |||||||
| No | 267 | 59 | (22.1) | 2.23 | (1.19–4.19) | 1.20 | (1.12–1.29) |
| Present | 101 | 10 | (9.9) | 1 | 1 | ||
| Chest pain and dyspnea | |||||||
| No | 128 | 23 | (18.0) | 0.94 | (0.60–1.47) | 0.99 | (0.96–1.04) |
| Present | 240 | 46 | (19.2) | 1 | 1 | ||
| Fatigue | |||||||
| No | 159 | 38 | (23.9) | 1.61 | (1.05–2.47) | 0.95 | (0.91–0.98) |
| Present | 209 | 31 | (14.8) | 1 | 1 | ||
| Night sweat | |||||||
| No | 343 | 68 | (19.8) | 4.96 | (0.72–34.21) | 1.37 | (1.08–1.77) |
| Present | 25 | 1 | (4.0) | 1 | 1 | ||
| Weight loss * | |||||||
| No | 311 | 65 | (20.9) | 2.93 | (1.11–7.71) | 1.38 | (1.20–1.62) |
| Present | 56 | 4 | (7.1) | 1 | 1 | ||
| Contact history of TB | |||||||
| No | 355 | 67 | (18.8) | 1.23 | (0.34–4.47) | 1.31 | (1.01–1.71) |
| Present | 13 | 2 | (15.4) | 1 | 1 | ||
| Characteristic | Number Tested | Confirmed TB# | RR | (95%CI) | aRR | (95%CI) | |
|---|---|---|---|---|---|---|---|
| n | (%) | ||||||
| Total | 494 | 110 | (22.3) | - | - | ||
| Age (years) | |||||||
| 15–44 | 191 | 45 | (23.6) | 1.32 | (0.81–2.16) | 1.59 | (0.93–2.72) |
| 45–64 | 202 | 47 | (23.3) | 1.31 | (0.80–2.13) | 1.33 | (0.80–2.21) |
| 65 and above | 101 | 18 | (17.8) | 1 | 1 | ||
| Gender | |||||||
| Male | 267 | 63 | (23.6) | 1.14 | (0.82–1.59) | 1.01 | (0.73–1.39) |
| Female | 227 | 47 | (20.7) | 1 | 1 | ||
| Self-reported HIV status | |||||||
| Negative | 218 | 70 | (32.1) | - | - | ||
| Positive | 2 | 0 | (0.0) | - | - | ||
| Unknown | 274 | 40 | (14.6) | - | - | ||
| Self-reported diabetes | |||||||
| No | 375 | 83 | (22.1) | 1 | 1 | ||
| Yes | 40 | 16 | (40.0) | 1.81 | (1.18–2.76) | 2.13 | (1.31–3.48) |
| Unknown | 79 | 11 | (13.9) | 0.63 | (0.35–1.12) | 0.78 | (0.44–1.39) |
| Cough | |||||||
| No | 66 | 10 | (15.1) | 1 | 1 | ||
| Present | 428 | 100 | (23.4) | 1.54 | (0.85–2.80) | 1.42 | (0.82–2.46) |
| Fever | |||||||
| No | 355 | 69 | (19.4) | 1 | 1 | ||
| Present | 139 | 41 | (29.5) | 1.52 | (1.08–2.13) | 1.32 | (0.95–1.83) |
| Chest pain and dyspnea | |||||||
| No | 162 | 44 | (27.2) | 1 | 1 | ||
| Present | 332 | 66 | (19.9) | 0.73 | (0.53–1.02) | 0.78 | (0.56–1.08) |
| Fatigue | |||||||
| No | 224 | 40 | (17.9) | 1 | 1 | ||
| Present | 270 | 70 | (25.9) | 1.45 | (1.03–2.05) | 1.18 | (0.82–1.69) |
| Night sweat | |||||||
| No | 469 | 100 | (21.3) | 1 | 1 | ||
| Present | 25 | 10 | (40.0) | 1.88 | (1.12–3.13) | 1.31 | (0.76–2.25) |
| Weight loss * | |||||||
| No | 433 | 83 | (19.2) | 1 | 1 | ||
| Present | 60 | 27 | (45.0) | 2.35 | (1.67–3.30) | 2.06 | (1.44–2.96) |
| Contact history of TB | |||||||
| No | 480 | 105 | (21.9) | 1 | 1 | ||
| Present | 14 | 5 | (35.7) | 1.63 | (0.79–3.36) | 1.51 | (0.75–3.04) |
| Treatment Outcomes | N | (%) |
|---|---|---|
| Total | 104 | (100) |
| Cured | 58 | (55.8) |
| Treatment completed | 39 | (37.5) |
| Died | 2 | (1.9) |
| Lost to follow-up | 3 | (2.9) |
| On treatment * | 2 | (1.9) |
| Duration | Number Eligible | Number (%) with Valid Dates | Median Days | (IQR) |
|---|---|---|---|---|
| From visiting the HIGH to receiving the TB diagnosis test | 494 | 487 (99) | 0 | (0–1) |
| From TB diagnosis to initiation of treatment | 103 | 99 (93) | 6 | (1–17) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Do Thu, T.; Kumar, A.M.V.; Ramaswamy, G.; Htun, T.; Le Van, H.; Nguyen Quang Vo, L.; Thi Thu Dong, T.; Codlin, A.; Forse, R.; Crewsell, J.; et al. An Innovative Public–Private Mix Model for Improving Tuberculosis Care in Vietnam: How Well Are We Doing? Trop. Med. Infect. Dis. 2020, 5, 26. https://doi.org/10.3390/tropicalmed5010026
Do Thu T, Kumar AMV, Ramaswamy G, Htun T, Le Van H, Nguyen Quang Vo L, Thi Thu Dong T, Codlin A, Forse R, Crewsell J, et al. An Innovative Public–Private Mix Model for Improving Tuberculosis Care in Vietnam: How Well Are We Doing? Tropical Medicine and Infectious Disease. 2020; 5(1):26. https://doi.org/10.3390/tropicalmed5010026
Chicago/Turabian StyleDo Thu, Thuong, Ajay M. V. Kumar, Gomathi Ramaswamy, Thurain Htun, Hoi Le Van, Luan Nguyen Quang Vo, Thuy Thi Thu Dong, Andrew Codlin, Rachel Forse, Jacob Crewsell, and et al. 2020. "An Innovative Public–Private Mix Model for Improving Tuberculosis Care in Vietnam: How Well Are We Doing?" Tropical Medicine and Infectious Disease 5, no. 1: 26. https://doi.org/10.3390/tropicalmed5010026
APA StyleDo Thu, T., Kumar, A. M. V., Ramaswamy, G., Htun, T., Le Van, H., Nguyen Quang Vo, L., Thi Thu Dong, T., Codlin, A., Forse, R., Crewsell, J., Nguyen Thanh, H., Nguyen Viet, H., Bui Van, H., Nguyen Binh, H., & Nguyen Viet, N. (2020). An Innovative Public–Private Mix Model for Improving Tuberculosis Care in Vietnam: How Well Are We Doing? Tropical Medicine and Infectious Disease, 5(1), 26. https://doi.org/10.3390/tropicalmed5010026






