Acute Poisonings at a Regional Referral Hospital in Western Kenya
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Setting and Population
2.3. Statistical Analysis
2.4. Ethical Considerations
3. Results
3.1. Demographic Characteristics of Victims
3.2. Location and Time of Exposure, Referring Facilities, and the Time Taken to Get to the Hospital
3.3. Offending Agents, Routes of Exposure, and Season of Poisoning
3.4. Circumstance and Reasons for Poisoning
3.5. Pre-Hospital First Aid among Victims and Identification of Offending Agents by Emergency Care Personnel
3.6. Admission Status and Outcome of Treatment of Victims at the Intensive Care Unit (ICU)
3.7. Length of Hospital Stay, Status of Treatment, Mortality Causing Offending Agents, and Demographic Features of Victims Who Succumbed to Poisoning
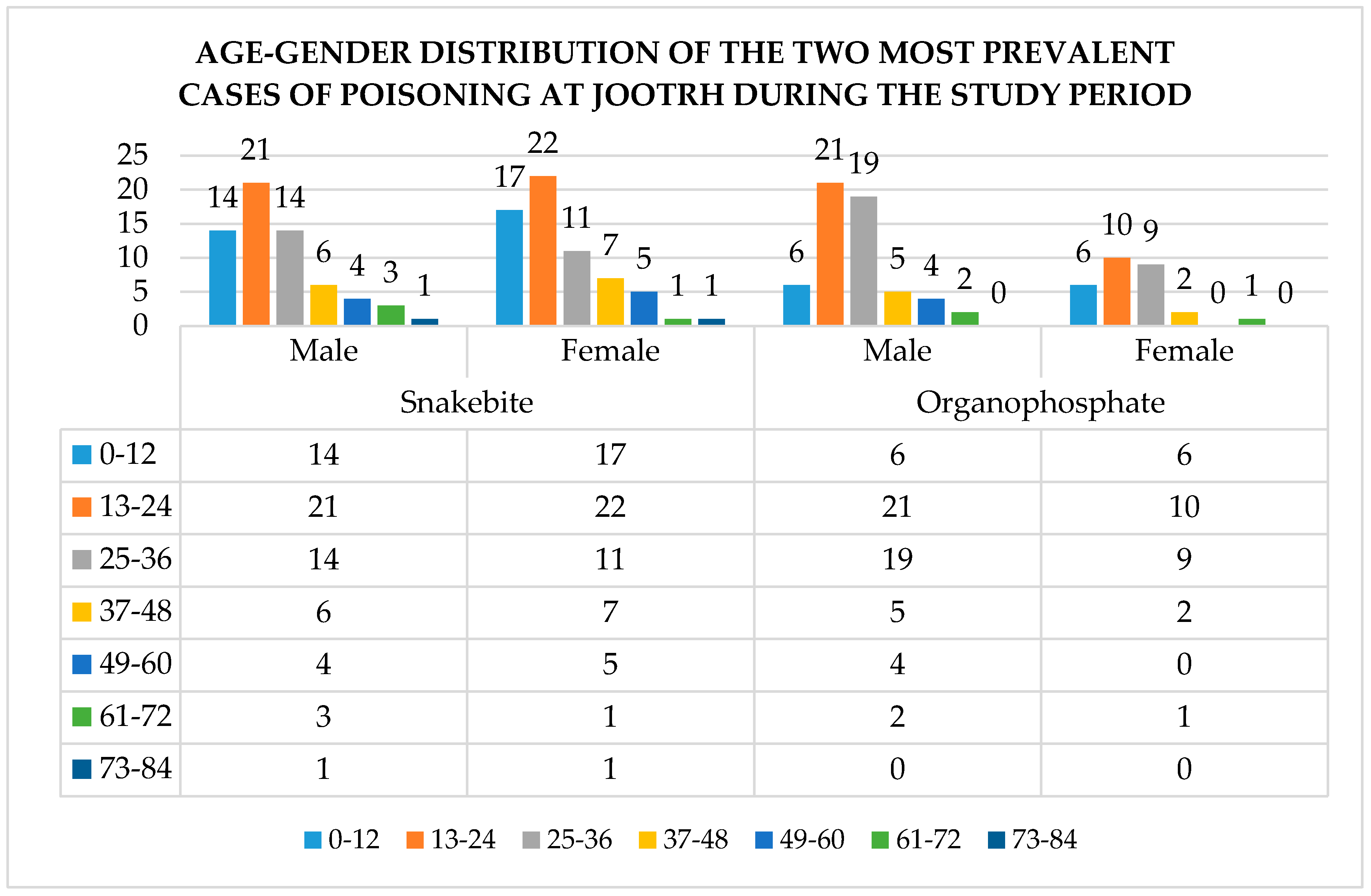
3.8. Treatment of the Two Major Poisons and Effect on the Outcome
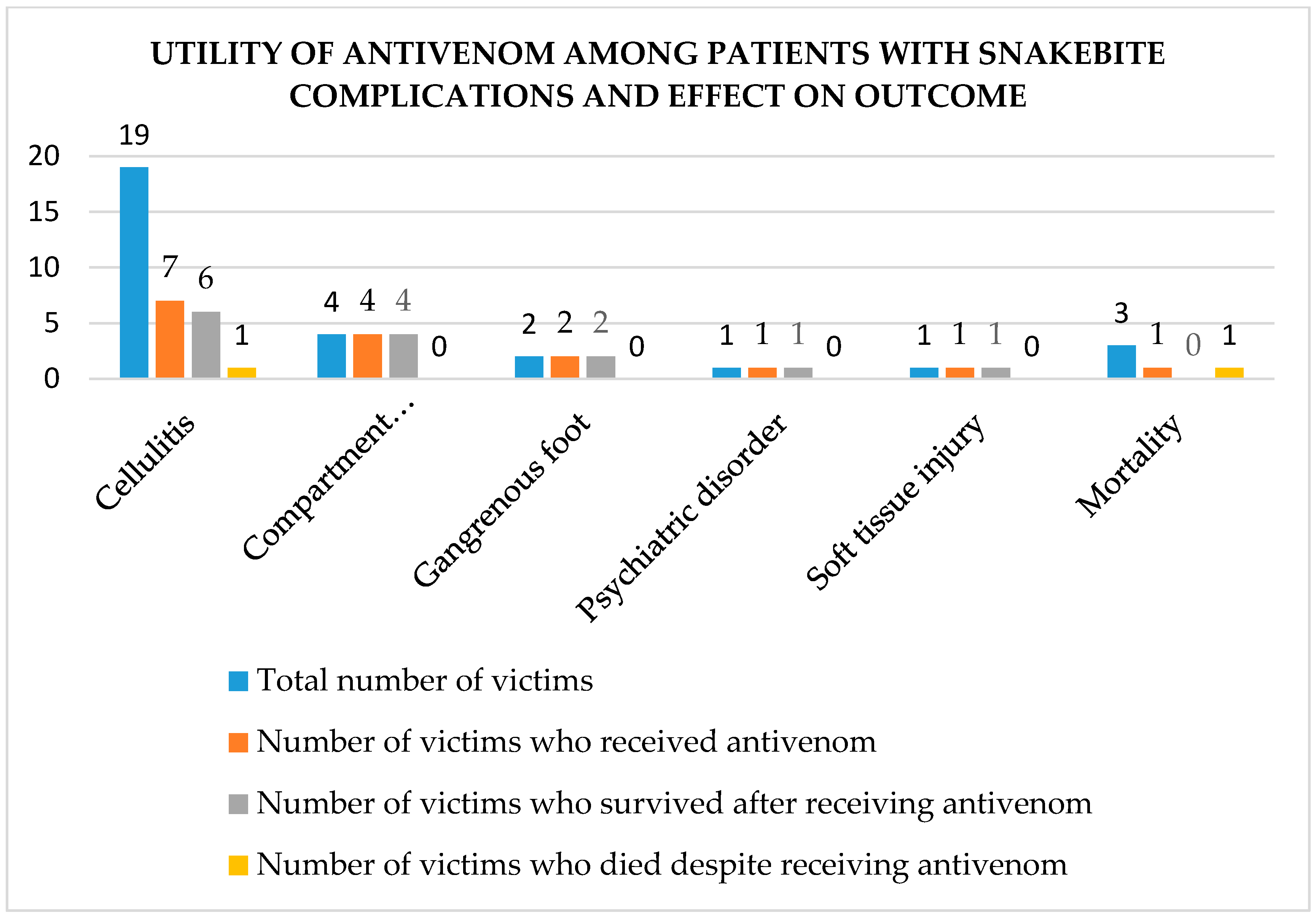
3.8.1. Snakebite
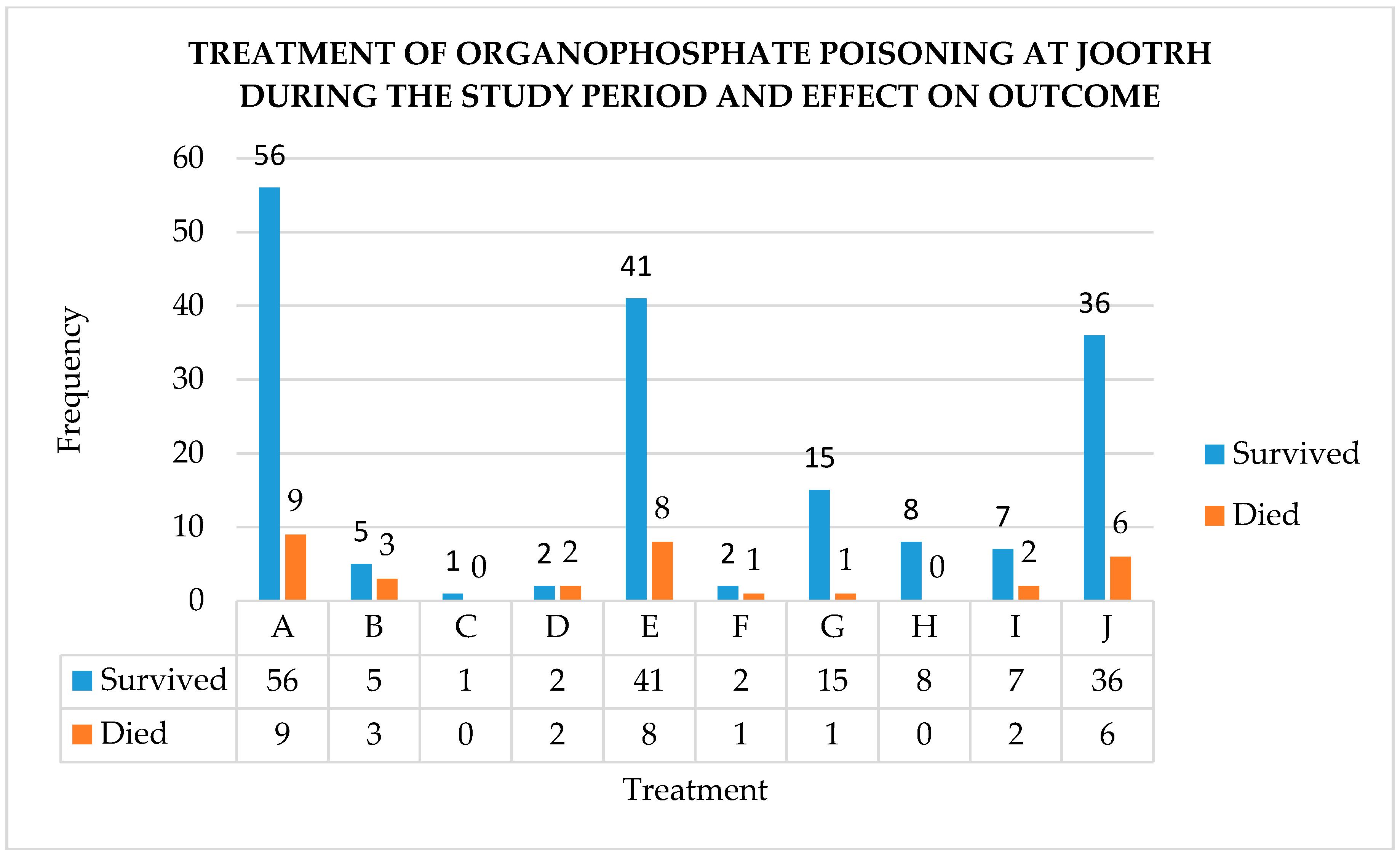
3.8.2. Organophosphates
3.9. Associations between Exposure Factors and Outcome of Poisoning Amongst Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Asawari, R.; Atmaram, P.; Bhagwan, K.; Priti, D.; Kavya, S.; Jabeen, G.A. Toxicological pattern of poisoning in urban hospitals of western India. J. Young Pharm. 2017, 9, 315–320. [Google Scholar] [CrossRef]
- WHO. Poisoning Prevention and Management. 2016. Available online: http://www.who.int/ipcs/poisons/en/ (accessed on 16 February 2018).
- Onsongo, J. Outbreak of aflatoxin poisoning in Kenya. EPI. IDS Bull. 2004, 5, 3–4. [Google Scholar]
- Charters, A.D. Mushroom poisoning in Kenya. J Am. Urolog. Assoc. 1957, 51, 265–270. [Google Scholar] [CrossRef]
- Ogola, J.S.; Mitullah, W.V.; Omulo, M.A. Impact of gold mining on the environment and human health: A case study in the Migori gold belt, Kenya. Environ. Geochem. Health 2002, 24, 141–157. [Google Scholar] [CrossRef]
- Rostrup, M.; Edwards, J.K.; Abukalish, M.; Ezzabi, M.; Some, D.; Ritter, H.; Menge, T.; Abdelrahman, A.; Rootwelt, R.; Janssens, B. The methanol poisoning outbreaks in Libya 2013 and Kenya 2014. PLoS ONE 2016, 11, e0152676. [Google Scholar] [CrossRef] [PubMed]
- Ohayo-Mitoko, G.J.A. Occupational Pesticide Exposure among Kenyan Agricultural Workers. 1997. Available online: https://library.wur.nl/WebQuery/wurpubs/39730 (accessed on 16 February 2018).
- Mugera, G.M.; Nderito, P. Cestrum poisoning in Kenya livestock. Bull. Epizoot. Dis. Afr. 1968, 11, 501–506. [Google Scholar]
- Krienitz, L.; Ballot, A.; Kotut, K.; Wiegand, C.; Pütz, S.; Metcalf, J.S.; Codd, G.A.; Stephan, P. Contribution of hot spring cyanobacteria to the mysterious deaths of lesser flamingos at Lake Bogoria, Kenya. FEMS Microbiol. Ecol. 2003, 43, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Mbaria, J.M.; Ochodo, C.; Nguta, J.M. Forensic case of lead poisoning from a battery manufacturing company in Nakuru, Kenya. Jpn. J. Vet. Res. 2013, 61, S64–S66. [Google Scholar] [PubMed]
- Jumba, I.O.; Kisia, S.M.; Kock, R. Animal health problems attributed to environmental contamination in Lake Nakuru National Park, Kenya: A case study on heavy metal poisoning in the waterbuck Kobus ellipsiprymnus defassa (Ruppel 1835). Arch. Environ. Contam. Toxicol. 2007, 52, 270–281. [Google Scholar] [CrossRef] [PubMed]
- Otieno, P.O.; Lalah, J.O.; Virani, M.; Jondiko, I.O.; Schramm, K.W. Carbofuran and its toxic metabolites provide forensic evidence for Furadan exposure in vultures (Gyps africanus) in Kenya. Bull. Environ. Contam. Toxicol. 2010, 84, 536–544. [Google Scholar] [CrossRef] [PubMed]
- Kihiko, D. Venomous snake bite injuries at Kitui District Hospital. Ann. Afr. Surg. 2013, 10, 15–20. [Google Scholar]
- Okumu-Ochola, F.O.; Okumu, M.O.; Muchemi, G.M.; Mucunu, J. Epidemiology of snake bites in selected areas of Kenya. Pan Afr. Med. J. 2018, 29, 1–9. [Google Scholar]
- Kahuho, S.K. Drug poisoning in the intensive care unit, Kenyatta National Hospital. East Afr. Med. J. 1980, 57, 490–494. [Google Scholar] [PubMed]
- Guantai, A.N. A Retrospective Study of Childhood Poisoning in Kenya. 1993. Available online: http://erepository.uonbi.ac.ke/handle/11295/17769 (accessed on 16 February 2018).
- Mbakaya, C.F.L.; Ohayo-Mitoko, G.J.; Ngowi, V.A.; Mbabazi, R.; Simwa, J.M.; Maeda, D.N.; Stephens, J.; Hakuza, H. The status of pesticide usage in East Africa. Afr. J. Health Sci. 1994, 1, 37–41. [Google Scholar] [PubMed]
- Nyamu, D.G.; Maitai, C.K.; Mecca, L.W.; Mwangangi, E.M. Trends of acute poisoning cases occurring at the Kenyatta National Hospital, Nairobi, Kenya. East Cent. Afr. J. Pharm. Sci. 2012, 15, 29–34. [Google Scholar]
- Lang, T.; Thuo, N.; Akech, S. Accidental paraffin poisoning in Kenyan children. Trop. Med. Inter. Health 2008, 13, 845–847. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bundotich, J.K.; Gichuhi, M.M. Acute poisoning in the Rift Valley Provincial General Hospital, Nakuru, Kenya: January to June 2012. S. Afr. Fam. Pract. 2015, 57, 214–218. [Google Scholar] [CrossRef]
- County Statistics—Kenya National Bureau of Statistics. Available online: https://www.knbs.or.ke/county-statistics/ (accessed on 30 January 2018).
- Jaramogi Oginga Oginga Teaching and Referral Hospital. Available online: http://ameca.org.uk/directory/listing/jaramogi-oginga-odinga-teaching-and-referral-hospital (accessed on 8 February 2018).
- Boyd, J.J.; Agazzi, G.; Svajda, D.; Morgan, A.J.; Ferrandis, S.; Norris, R.L. Venomous snakebite in mountainous terrain: Prevention and management. Wilder. Environ. Med. 2007, 18, 190–202. [Google Scholar] [CrossRef] [PubMed]
- Jailkhani, S.M.K.; Naik, J.D.; Thakur, M.S.; Langare, S.D.; Pandey, V.O. Retrospective analysis of poisoning cases admitted in a tertiary care hospital. Int. J. Recent Trends Sci. Technol. 2014, 10, 365–368. [Google Scholar]
- Snakes. Available online: http://www.bio-ken.com/index.php/reptiles-and-amphibians/snakes (accessed on 1 February 2018).
- Chugh, S.N.; Aggarwal, N.; Dabla, S.; Chhabra, B. Comparative evaluation of atropine alone and atropine with pralidoxime (PAM) in the management of organophosphorus poisoning. J. Indian Acad. Clin. Med. 2005, 6, 33–37. [Google Scholar]
- Eyer, P.; Buckley, N. Pralidoxime for organophosphate poisoning. Lancet 2006, 368, 2110–2111. [Google Scholar] [CrossRef] [Green Version]
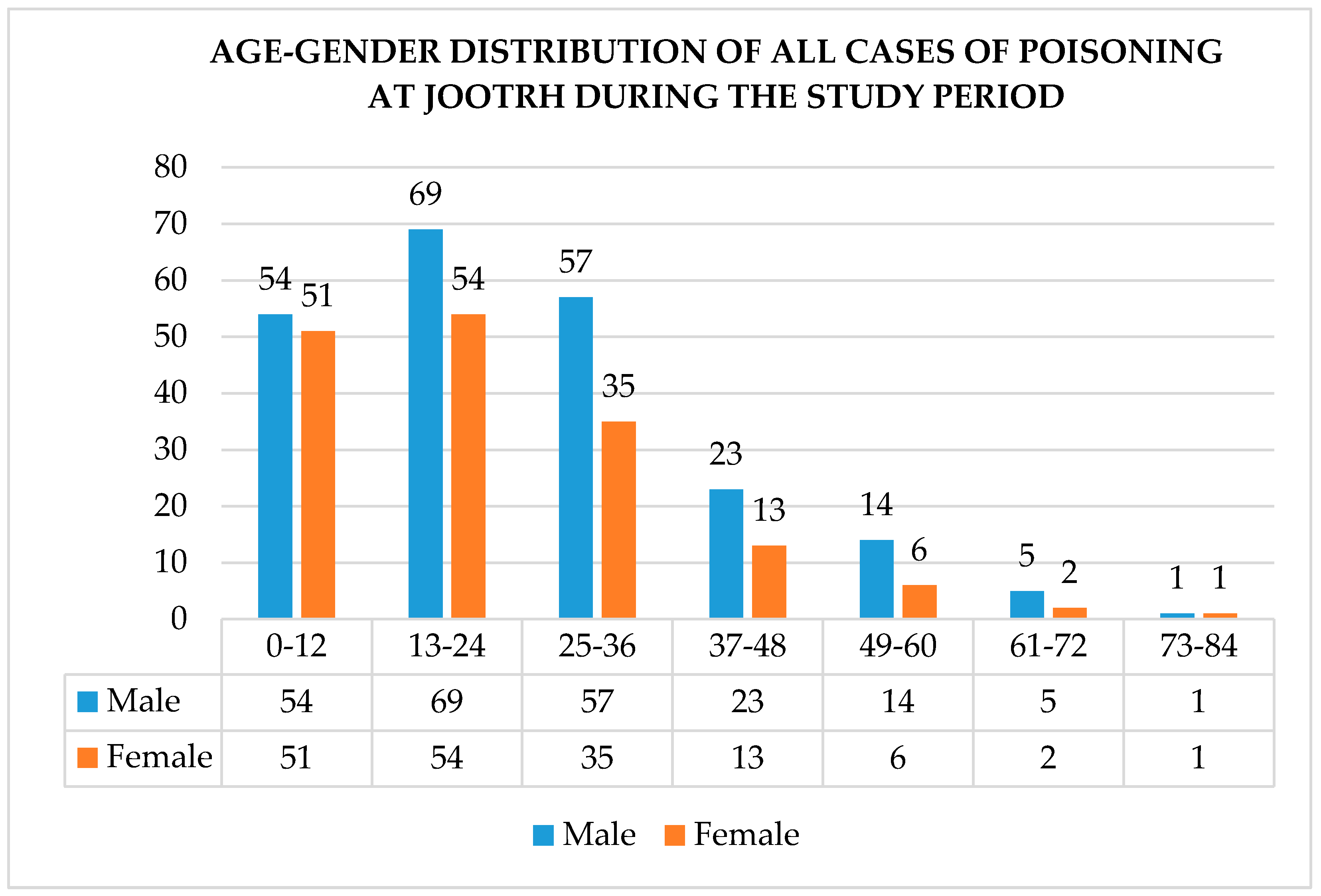
| Demographic Factor | n = 385 |
|---|---|
| Gender | |
| Male | 223 (57.9%) |
| Female | 162 (42.1%) |
| Age | |
| 0–12 | 105 (27.3%) |
| 13–24 | 123 (31.9%) |
| 25–36 | 92 (23.9%) |
| 37–48 | 36 (9.4%) |
| 49–60 | 20 (5.2%) |
| 61–72 | 7 (1.8%) |
| 73–84 | 2 (0.5%) |
| Marital status | |
| Married | 139 (36.1%) |
| Child | 117 (30.4%) |
| Single | 90 (23.4%) |
| Unknown | 29 (7.5%) |
| Divorcees, widows, widowers | 10 (2.6%) |
| Occupation | |
| Self-employed | 107 (27.8%) |
| Students | 89 (23.1%) |
| Child | 77 (20.0%) |
| Unemployed | 39 (10.1%) |
| Formally employed | 33 (8.6%) |
| Casual laborers | 11 (2.9%) |
| Unknown | 29 (7.5%) |
| Variable | Frequency (n = 385) |
|---|---|
| County | |
| Kisumu | 323 (83.9%) |
| Siaya | 28 (7.3%) |
| Vihiga | 11 (2.9%) |
| Homabay | 8 (2.1%) |
| Nandi | 7 (1.8%) |
| Other a | 8 (2.1%) |
| Sub-county * | |
| Kisumu East | 190 (58.8%) |
| Nyando | 43 (13.3%) |
| Kisumu West | 39 (12.1%) |
| Nyakach | 18 (5.6%) |
| Kisumu Central | 15 (4.6%) |
| Seme | 11 (3.4%) |
| Muhoroni | 7 (2.2%) |
| Referring facilities | |
| Public hospitals | 74 (81.3%) |
| Private hospitals | 11 (12.1%) |
| Mission hospitals | 6 (6.6%) |
| Time of exposure | |
| 0600–1159 | 49 (12.7%) |
| 1200–1759 | 60 (15.6%) |
| 1800–2359 | 91 (23.6%) |
| 0000–0559 | 20 (5.2%) |
| No data | 165 (42.9%) |
| Time to hospital | |
| <1 h | 10 (2.6%) |
| 1–4 h | 91 (23.6%) |
| 4–8 h | 49 (12.7%) |
| 8–12 h | 19 (4.9%) |
| 12–16 h | 8 (2.1%) |
| 16–20 h | 8 (2.1%) |
| 20–24 h | 19 (4.9%) |
| >24 h | 5 (1.3%) |
| Unknown | 176 (45.7%) |
| Variable | Frequency (n = 385) |
|---|---|
| Offending agents | |
| Snake poison | 127 (33%) |
| Organophosphates a | 85 (22.1%) |
| Kerosene/paraffin | 29 (7.5%) |
| OTC b and prescription drugs c | 19 (4.9%) |
| Amitraz | 18 (4.7%) |
| Food | 16 (4.2%) |
| Ethanol | 15 (3.9%) |
| Corrosive chemicals | 15 (3.9%) |
| Herbal medicine | 9 (2.3%) |
| Rodenticides | 8 (2.1%) |
| Insect repellant | 8 (2.1%) |
| Others d | 19 (4.9%) |
| Route of exposure | |
| Oral/ingestion | 239 (62.1%) |
| Inoculation | 131 (34.0%) |
| Mucocutaneous | 9 (2.3%) |
| Inhalation | 5 (1.3%) |
| Unknown | 1 (0.3%) |
| Season of poisoning | |
| Long rainy season | 172 (44.7%) |
| Short rainy season | 74 (19.2%) |
| Cool dry season | 78 (20.3%) |
| Hot dry season | 61 (15.8%) |
| Variable | Frequency (n = 385) |
|---|---|
| Circumstance | |
| Accidental | 242 (62.9%) |
| Suicidal | 122 (31.7%) |
| Homicidal | 17 (4.4%) |
| Suicidal and homicidal | 1 (0.3%) |
| Unknown | 3 (0.8%) |
| Reasons for poisoning | |
| Accidentally bitten by snakes | 127 (33.0%) |
| Domestic quarrels | 68 (17.7%) |
| Parental negligence | 44 (11.4%) |
| Poor food handling/preparation | 17 (4.4%) |
| Alcohol misuse | 14 (3.6%) |
| Psychiatric disorders | 12 (3.1%) |
| Love affairs | 11 (2.9%) |
| Curiosity | 7 (1.8%) |
| Traditional beliefs | 5 (1.3%) |
| Unemployment | 4 (1.0%) |
| Unknown | 51 (13.2%) |
| Others a | 25 (6.5%) |
| Variable | Frequency (n = 385) |
|---|---|
| First aid measure | |
| Tying a tourniquet | 10 (2.6%) |
| Use of herbal medicine | 10 (2.6%) |
| Use of milk | 7 (1.8%) |
| Use of raw eggs | 7 (1.8%) |
| Use of both raw eggs and milk | 4 (1.0%) |
| Incisions | 2 (0.5%) |
| Torniquet, incisions, and herbal medicine | 2 (0.5%) |
| Incisions and herbal medicine | 2 (0.5%) |
| None | 323 (84%) |
| Others a | 18 (4.7%) |
| Mode of identifying offending agents | |
| Container | 104 (27.0%) |
| The color of the offending animal | 83 (21.6%) |
| Odor only | 14 (3.6%) |
| Container and odor | 8 (2.1%) |
| History from informant | 11 (2.9%) |
| Identification of the food source | 12 (3.1%) |
| Fang marks | 12 (3.1%) |
| None | 134 (34.8%) |
| Others b | 7 (1.8%) |
| Variable | Frequency |
|---|---|
| Clinical presentation (n = 385) | |
| Neurological a and gastrointestinal b | 80 (20.8%) |
| Neurological a only | 71 (18.4%) |
| Neurological a and swelling | 53 (13.8%) |
| Gastrointestinal b only | 53 (13.8%) |
| Neurological a, gastrointestinal b, and cardiopulmonary c | 28 (7.3%) |
| Neurological a and cardiopulmonary c | 26 (6.8%) |
| Swelling only | 14 (3.6%) |
| Neurological a and bleeding | 13 (3.4%) |
| Neurological a, swelling, and bleeding | 12 (3.1%) |
| Asymptomatic | 4 (1.0%) |
| Others | 31 (13.8%) |
| Laboratory evaluation (n = 110) | |
| RBS only | 28 (25.5%) |
| FHG, serum electrolytes, and BUN | 17 (15.5%) |
| FHG, serum electrolytes, and Scr | 9 (8.2%) |
| FHG, serum electrolytes, and LFTs | 7 (6.4%) |
| FHG only | 7 (6.4%) |
| Abdominal ultrasound | 4 (3.6%) |
| FHG and serum electrolytes | 4 (3.6%) |
| Others x | 34 (30.9%) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okumu, M.O.; Patel, M.N.; Bhogayata, F.R.; Olweny, I.A.; Ochola, F.O.; Onono, J.O. Acute Poisonings at a Regional Referral Hospital in Western Kenya. Trop. Med. Infect. Dis. 2018, 3, 96. https://doi.org/10.3390/tropicalmed3030096
Okumu MO, Patel MN, Bhogayata FR, Olweny IA, Ochola FO, Onono JO. Acute Poisonings at a Regional Referral Hospital in Western Kenya. Tropical Medicine and Infectious Disease. 2018; 3(3):96. https://doi.org/10.3390/tropicalmed3030096
Chicago/Turabian StyleOkumu, Mitchel Otieno, Minal Naran Patel, Foram Rajnkant Bhogayata, Irene Awuor Olweny, Francis Okumu Ochola, and Joshua Orungo Onono. 2018. "Acute Poisonings at a Regional Referral Hospital in Western Kenya" Tropical Medicine and Infectious Disease 3, no. 3: 96. https://doi.org/10.3390/tropicalmed3030096
APA StyleOkumu, M. O., Patel, M. N., Bhogayata, F. R., Olweny, I. A., Ochola, F. O., & Onono, J. O. (2018). Acute Poisonings at a Regional Referral Hospital in Western Kenya. Tropical Medicine and Infectious Disease, 3(3), 96. https://doi.org/10.3390/tropicalmed3030096





