Contribution of Respiratory Syncytial Virus to Burden of Lower Respiratory Tract Infections: A Global Analysis of 204 Countries and Territories, 1990–2021
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Construction of the ARIMA Model
2.3. Statistical Analysis
3. Results
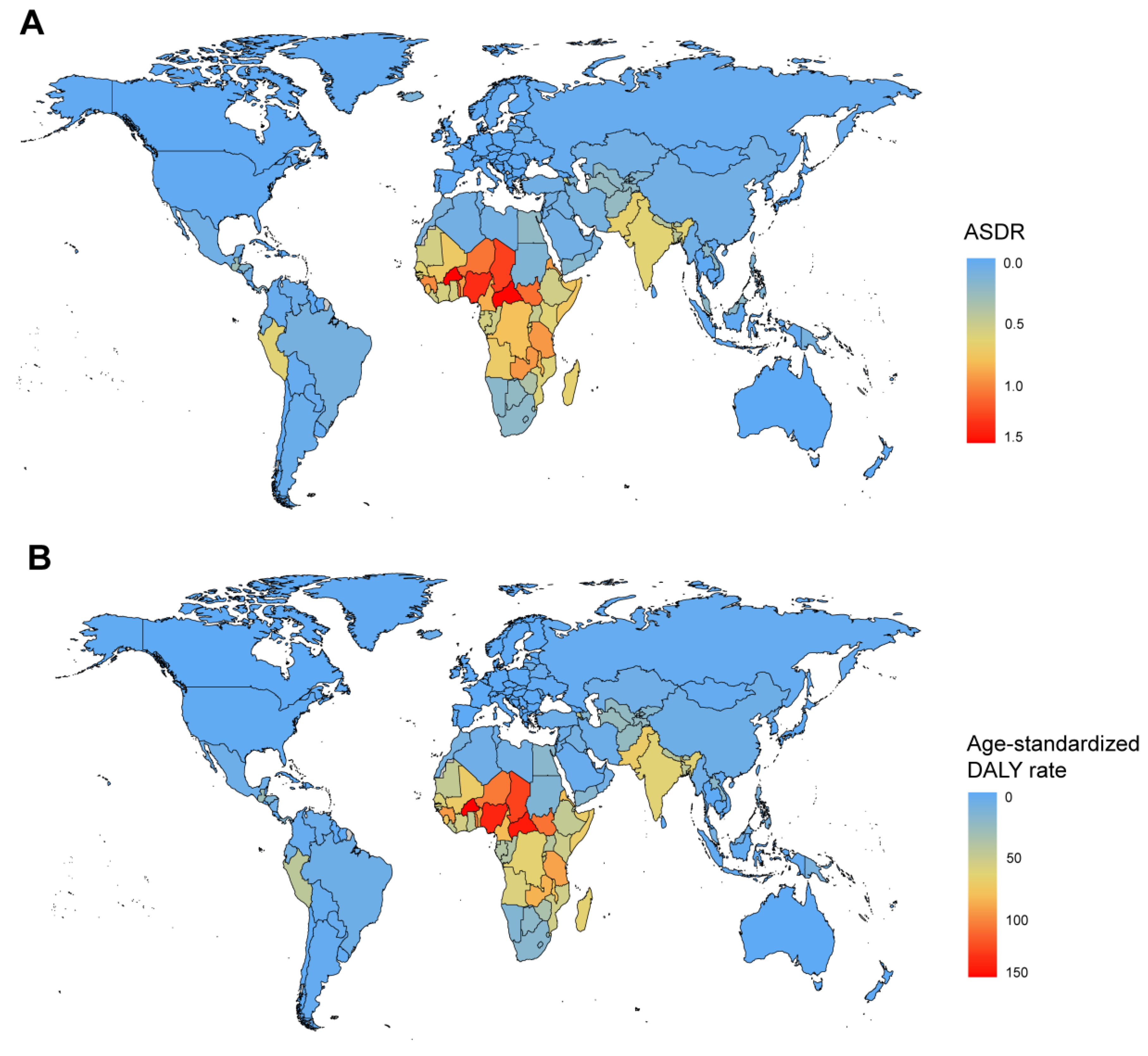
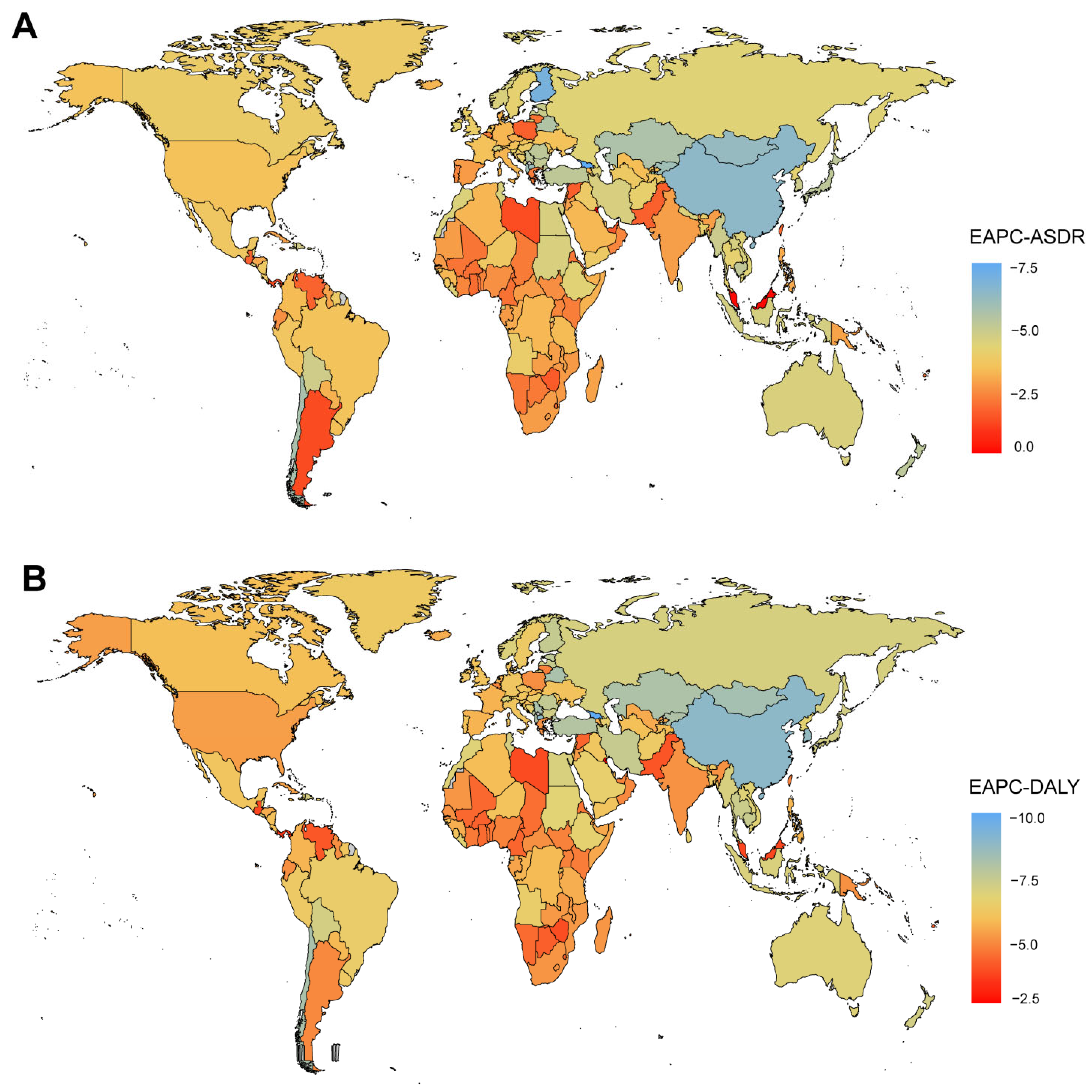
3.1. Death and DALY Burden of Respiratory Syncytial Virus
3.2. Sex and Age Distribution of Deaths and DALYs
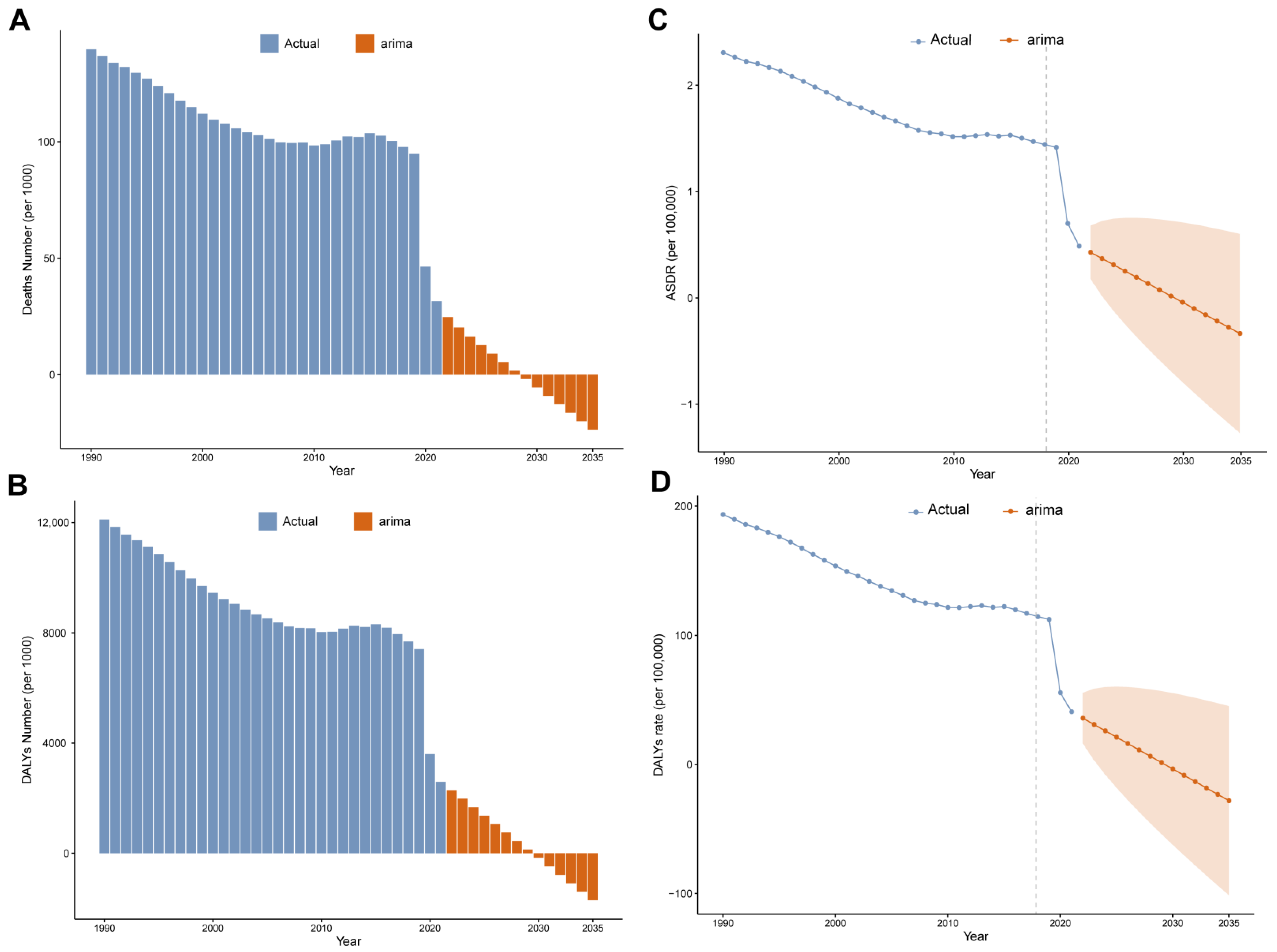
3.3. ARIMA Models Predict Trends in Burden of RSV-Related LRI
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hall, C.B.; Weinberg, G.A.; Iwane, M.K.; Blumkin, A.K.; Edwards, K.M.; Staat, M.A.; Auinger, P.; Griffin, M.R.; Poehling, K.A.; Erdman, D.; et al. The burden of respiratory syncytial virus infection in young children. N. Engl. J. Med. 2009, 360, 588–598. [Google Scholar] [CrossRef] [PubMed]
- Nair, H.; Nokes, D.J.; Gessner, B.D.; Dherani, M.; Madhi, S.A.; Singleton, R.J.; O’Brien, K.L.; Roca, A.; Wright, P.F.; Bruce, N.; et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: A systematic review and meta-analysis. Lancet 2010, 375, 1545–1555. [Google Scholar] [CrossRef] [PubMed]
- Raffaldi, I.; Castagno, E. The Epidemiology of Respiratory Syncytial Virus: New Trends and Future Perspectives. Viruses 2024, 16, 1100. [Google Scholar] [CrossRef] [PubMed]
- Shi, T.; McAllister, D.A.; O’Brien, K.L.; Simoes, E.A.F.; Madhi, S.A.; Gessner, B.D.; Polack, F.P.; Balsells, E.; Acacio, S.; Aguayo, C.; et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in young children in 2015: A systematic review and modelling study. Lancet 2017, 390, 946–958. [Google Scholar] [CrossRef]
- Alfano, F.; Bigoni, T.; Caggiano, F.P.; Papi, A. Respiratory Syncytial Virus Infection in Older Adults: An Update. Drugs Aging 2024, 41, 487–505. [Google Scholar] [CrossRef]
- Karron, R.A.; Singleton, R.J.; Bulkow, L.; Parkinson, A.; Kruse, D.; DeSmet, I.; Indorf, C.; Petersen, K.M.; Leombruno, D.; Hurlburt, D.; et al. Severe respiratory syncytial virus disease in Alaska native children. RSV Alaska Study Group. J. Infect. Dis. 1999, 180, 41–49. [Google Scholar] [CrossRef]
- Du, Y.; Yan, R.; Wu, X.; Zhang, X.; Chen, C.; Jiang, D.; Yang, M.; Cao, K.; Chen, M.; You, Y.; et al. Global burden and trends of respiratory syncytial virus infection across different age groups from 1990 to 2019: A systematic analysis of the Global Burden of Disease 2019 Study. Int. J. Infect. Dis. 2023, 135, 70–76. [Google Scholar] [CrossRef]
- Díez-Domingo, J.; Pérez-Yarza, E.G.; Melero, J.A.; Sánchez-Luna, M.; Aguilar, M.D.; Blasco, A.J.; Alfaro, N.; Lázaro, P. Social, economic, and health impact of the respiratory syncytial virus: A systematic search. BMC Infect. Dis. 2014, 14, 544. [Google Scholar] [CrossRef]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Divarathne, M.V.M.; Ahamed, R.R.; Noordeen, F. The Impact of RSV-Associated Respiratory Disease on Children in Asia. J. Pediatr. Infect. Dis. 2019, 14, 79–88. [Google Scholar] [CrossRef]
- Thompson, W.W.; Shay, D.K.; Weintraub, E.; Brammer, L.; Bridges, C.B.; Cox, N.J.; Fukuda, K. Influenza-associated hospitalizations in the United States. JAMA 2004, 292, 1333–1340. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, X.; Blau, D.M.; Caballero, M.T.; Feikin, D.R.; Gill, C.J.; Madhi, S.A.; Omer, S.B.; Simões, E.A.F.; Campbell, H.; et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in children younger than 5 years in 2019: A systematic analysis. Lancet 2022, 399, 2047–2064. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease Cancer Collaboration. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: A systematic analysis for the global burden of disease study. JAMA Oncol. 2017, 3, 524–548. [Google Scholar] [CrossRef]
- Wu, M.; Wu, Q.; Liu, D.; Zu, W.; Zhang, D.; Chen, L. The global burden of lower respiratory infections attributable to respiratory syncytial virus in 204 countries and territories, 1990–2019: Findings from the Global Burden of Disease Study 2019. Intern. Emerg. Med. 2024, 19, 59–70. [Google Scholar] [CrossRef]
- Chartrand, C.; Tremblay, N.; Renaud, C.; Papenburg, J. Diagnostic Accuracy of Rapid Antigen Detection Tests for Respiratory Syncytial Virus Infection: Systematic Review and Meta-analysis. J. Clin. Microbiol. 2015, 53, 3738–3749. [Google Scholar] [CrossRef]
- Ferrani, S.; Prazuck, T.; Béchet, S.; Lesne, F.; Cohen, R.; Levy, C. Diagnostic accuracy of a rapid antigen triple test (SARS-CoV-2, respiratory syncytial virus, and influenza) using anterior nasal swabs versus multiplex RT-PCR in children in an emergency department. Infect. Dis. Now. 2023, 53, 104769. [Google Scholar] [CrossRef]
- El-Atawi, K.; De Luca, D.; Ramanathan, R.; Luna, M.S.; Alsaedi, S.; Wahab, M.G.A.; Hamdi, M.; Saleh, M. Efficacy and Safety of Palivizumab as a Prophylaxis for Respiratory Syncytial Virus (RSV) Disease: An Updated Systemic Review and Meta-Analysis. Cureus 2023, 15, e51375. [Google Scholar] [CrossRef]
- Cichero, E.; Calautti, A.; Francesconi, V.; Tonelli, M.; Schenone, S.; Fossa, P. Probing In Silico the Benzimidazole Privileged Scaffold for the Development of Drug-like Anti-RSV Agents. Pharmaceuticals 2021, 14, 1307. [Google Scholar] [CrossRef]
- Cox, R.; Plemper, R.K. Structure-guided design of small-molecule therapeutics against RSV disease. Expert. Opin. Drug Discov. 2016, 11, 543–556. [Google Scholar] [CrossRef]
- Chirikov, V.; Botteman, M.; Simões, E.A.F. The Long-Term Healthcare Utilization and Economic Burden of RSV Infection in Children ≤5 Years in Japan: Propensity Score Matched Cohort Study. Clin. Outcomes Res. 2022, 14, 699–714. [Google Scholar] [CrossRef]
- Clark, J.; Kochovska, S.; Currow, D.C. Burden of respiratory problems in low-income and middle-income countries. Curr. Opin. Support. Palliat. Care 2022, 16, 210–215. [Google Scholar] [CrossRef] [PubMed]
- GBD 2019 Chronic Respiratory Diseases Collaborators. Global burden of chronic respiratory diseases and risk factors, 1990–2019: An update from the Global Burden of Disease Study 2019. eClinicalMedicine 2023, 59, 101936. [Google Scholar] [CrossRef] [PubMed]
- Meghji, J.; Mortimer, K.; Agusti, A.; Allwood, B.W.; Asher, I.; Bateman, E.D.; Bissell, K.; Bolton, C.E.; Bush, A.; Celli, B.; et al. Improving lung health in low-income and middle-income countries: From challenges to solutions. Lancet 2021, 397, 928–940. [Google Scholar] [CrossRef] [PubMed]
- Du, Z.; Pandey, A.; Moghadas, S.M.; Bai, Y.; Wang, L.; Matrajt, L.; Singer, B.H.; Galvani, A.P. Impact of RSVpreF vaccination on reducing the burden of respiratory syncytial virus in infants and older adults. Nat. Med. 2025, 31, 647–652. [Google Scholar] [CrossRef]
- Esposito, S.; Raya, B.A.; Baraldi, E.; Flanagan, K.; Torres, F.M.; Tsolia, M.; Zielen, S. RSV Prevention in All Infants: Which Is the Most Preferable Strategy? Front. Immunol. 2022, 13, 880368. [Google Scholar] [CrossRef]
- Gong, X.; Luo, E.; Fan, L.; Zhang, W.; Yang, Y.; Du, Y.; Yang, X.; Xing, S. Clinical research on RSV prevention in children and pregnant women: Progress and perspectives. Front. Immunol. 2023, 14, 1329426. [Google Scholar] [CrossRef]
- Shi, T.; Denouel, A.; Tietjen, A.K.; Campbell, I.; Moran, E.; Li, X.; Campbell, H.; Demont, C.; Nyawanda, B.O.; Chu, H.; et al. Global Disease Burden Estimates of Respiratory Syncytial Virus-Associated Acute Respiratory Infection in Older Adults in 2015: A Systematic Review and Meta-Analysis. J. Infect. Dis. 2020, 222, S577–S583. [Google Scholar] [CrossRef]
- Bents, S.J.; Viboud, C.; Grenfell, B.T.; Hogan, A.B.; Tempia, S.; von Gottberg, A.; Moyes, J.; Walaza, S.; Hansen, C.; Cohen, C.; et al. Modeling the impact of COVID-19 nonpharmaceutical interventions on respiratory syncytial virus transmission in South Africa. Influenza Other Respir. Viruses 2023, 17, e13229. [Google Scholar] [CrossRef]
- Al-Jwadi, R.F.; Mills, E.H.A.; Torp-Pedersen, C.; Andersen, M.P.; Jørgensen, I.M. Consequences of COVID-19-related lockdowns and reopenings on emergency hospitalizations in pediatric patients in Denmark during 2020-2021. Eur. J. Pediatr. 2023, 182, 285–293. [Google Scholar] [CrossRef]
- Angelova, A.; Atanasova, M.; Ketev, K.; Halil, Z.; Paskaleva, I.; Lengerova, G.; Dimcheva, T.; Korsun, N.; Murdjeva, M. Severe SARS-CoV-2 and respiratory syncytial virus co-infection in two children. Folia Med. 2023, 65, 495–499. [Google Scholar] [CrossRef]




| Deaths Cases (95% CI) | ASDR (95% CI) | 1990–2021 EAPCs (95%CI) | |||
|---|---|---|---|---|---|
| 1990 | 2021 | 1990 | 2021 | ||
| Global | 139,762 (123,666–158,110) | 31,525 (23,348–41,871) | 2.31 (2.05–2.60) | 0.49 (0.36–0.65) | −2.62 (−3.33 to −1.91) |
| SDI | |||||
| High SDI | 3391 (3102–3628) | 290 (211–396) | 0.38 (0.35–0.41) | 0.02 (0.01–0.03) | −3.19 (−4.84 to −1.51) |
| High-middle SDI | 10,300 (9268–11,698) | 626 (467–841) | 1.16 (1.05–1.32) | 0.06 (0.05–0.08) | −5.24 (−6.30 to −4.16) |
| Middle SDI | 40,684 (36,610–45,407) | 3563 (2585–4721) | 2.13 (1.93–2.37) | 0.21 (0.15–0.28) | −4.10 (−4.98 to −3.21) |
| Low-middle SDI | 49,350 (42,974–56,450) | 11,772 (7763–16,625) | 2.84 (2.49–3.25) | 0.66 (0.43–0.93) | −2.38 (−3.10 to −1.64) |
| Low SDI | 35,948 (29,715–42,705) | 15,264 (10,766–20,495) | 3.85 (3.20–4.55) | 1.01 (0.72–1.34) | −2.39 (−2.99 to −1.79) |
| Central Europe, eastern Europe, and central Asia | |||||
| Central Asia | 4344 (4034–4707) | 222 (118–365) | 4.64 (4.31–5.02) | 0.23 (0.12–0.38) | −3.98 (−5.37 to −2.57) |
| Central Europe | 841 (795–883) | 9 (2–22) | 0.92 (0.87–0.96) | 0.01 (0.00–0.01) | −4.54 (−7.04 to −1.98) |
| Eastern Europe | 1073 (1017–1134) | 68 (29–130) | 0.68 (0.64–0.72) | 0.04 (0.02–0.07) | −4.18 (−5.48 to −2.86) |
| High income region | |||||
| High-income Asia Pacific | 757 (681–817) | 2 (0–12) | 0.50 (0.45–0.54) | 0.00 (0.00–0.00) | −5.77 (−9.62 to −1.75) |
| High-income North America | 967 (870–1042) | 113 (55–205) | 0.30 (0.27–0.32) | 0.02 (0.01–0.04) | −3.23 (−4.60 to −1.85) |
| Western Europe | 1292 (1159–1399) | 97 (62–143) | 0.27 (0.25–0.29) | 0.01 (0.01–0.01) | −3.16 (−5.10 to −1.17) |
| Australasia | 42 (39–46) | 0 (0–1) | 0.23 (0.22–0.25) | 0.00 (0.00–0.00) | −5.04 (−8.35 to −1.61) |
| Latin America and Caribbean | |||||
| Andean Latin America | 1404 (1225–1590) | 284 (106–464) | 2.77 (2.43–3.12) | 0.48 (0.18–0.79) | −3.12 (−4.26 to −1.96) |
| Caribbean | 613 (516–733) | 2 (0–11) | 1.54 (1.31–1.82) | 0.01 (0.00–0.03) | −3.75 (−6.99 to −0.39) |
| Southern Latin America | 277 (262–291) | 32 (13–61) | 0.59 (0.55–0.62) | 0.04 (0.02–0.08) | −1.51 (−3.69–0.72) |
| Tropical Latin America | 2064 (1841–2295) | 263 (78–586) | 1.37 (1.23–1.51) | 0.12 (0.04–0.28) | −3.22 (−4.53 to −1.89) |
| Central Latin America | 2779 (2571–3032) | 212 (142–305) | 1.29 (1.20–1.39) | 0.10 (0.07–0.15) | −2.46 (−3.82 to −1.08) |
| North Africa and Middle East | |||||
| North Africa and Middle East | 10,774 (9198–13,390) | 1039 (560–1796) | 2.17 (1.85–2.67) | 0.20 (0.11–0.34) | −3.86 (−4.46 to −3.25) |
| South Asia | |||||
| South Asia | 41,103 (34,240–48,132) | 11,561 (5798–18,693) | 2.64 (2.21–3.08) | 0.77 (0.39–1.25) | −2.20 (−2.69 to −1.71) |
| Southeast Asia, east Asia, and Oceania | |||||
| East Asia | 25,950 (22,337–30,046) | 908 (513–1516) | 2.34 (2.02–2.70) | 0.10 (0.06–0.16) | −7.31 (−8.16 to −6.45) |
| Oceania | 305 (247–380) | 23 (11–43) | 3.05 (2.50–3.76) | 0.12 (0.06–0.22) | −2.00 (−4.03–0.07) |
| Southeast Asia | 11,749 (10,245–13,843) | 398 (259–584) | 2.09 (1.83–2.44) | 0.07 (0.05–0.11) | −3.93 (−5.53 to −2.31) |
| Sub-Saharan Africa | |||||
| Central Sub-Saharan Africa | 3460 (2530–4456) | 1537 (729–2437) | 3.31 (2.48–4.17) | 0.98 (0.48–1.50) | −3.06 (−3.36 to −2.77) |
| Eastern Sub-Saharan Africa | 11,960 (9743–14,547) | 4505 (2917–6559) | 3.31 (2.73–3.96) | 0.85 (0.57–1.23) | −2.79 (−3.45 to −2.13) |
| Southern Sub-Saharan Africa | 1479 (1295–1693) | 245 (98–490) | 2.15 (1.90–2.44) | 0.33 (0.13–0.67) | −1.50 (−3.34–0.37) |
| Western Sub-Saharan Africa | 16,519 (13,585–19,646) | 9996 (5877–14,968) | 4.47 (3.68–5.30) | 1.34 (0.80–2.00) | −1.80 (−2.41 to −1.20) |
| DALYs (95% CI) | Age-Standardized DALY Rate (95% CI) | 1990–2021 EAPCs (95%CI) | |||
|---|---|---|---|---|---|
| 1990 | 2021 | 1990 | 2021 | ||
| Global | 12,105,847 (10,665,949–13,740,784) | 2,591,507 (1,902,003–3,468,792) | 193.49 (170.61–219.46) | 40.82 (29.91–54.59) | −2.77 (−3.44 to −2.09) |
| SDI | |||||
| High SDI | 122,762 (115,754–130,626) | 7790 (5622–10,838) | 17.16 (16.12–18.35) | 0.89 (0.63–1.23) | −3.38 (−4.85 to −1.88) |
| High-middle SDI | 866,214 (774,684–990,312) | 28,413 (21,346–37,666) | 96.90 (86.68–110.78) | 3.84 (2.85–5.13) | −6.34 (−7.34 to −5.33) |
| Middle SDI | 3,563,942 (3,200,439–3,987,783) | 251,513 (179,101–340,161) | 180.15 (161.94–201.38) | 15.34 (10.88–20.86) | −4.54 (−5.41 to −3.67) |
| Low-middle SDI | 4,368,503 (3,799,151–5,000,857) | 982,202 (651,937–1,386,106) | 244.40 (212.81–279.98) | 52.79 (35.00–74.55) | −2.58 (−3.31 to −1.84) |
| Low SDI | 3,177,072 (2,621,925–3,775,665) | 1,321,025 (932,144–1,775,047) | 326.85 (269.73–389.51) | 80.35 (56.66–107.90) | −2.56 (−3.17 to −1.95) |
| Central Europe, eastern Europe, and central Asia | |||||
| Central Asia | 386,572 (358,853–418,955) | 19,064 (9879–31,308) | 410.33 (381.01–444.66) | 19.29 (10.02–31.67) | −4.10 (−5.50 to −2.68) |
| Central Europe | 64,501 (60,872–67,975) | 302 (102–665) | 73.73 (69.47–77.82) | 0.36 (0.13–0.76) | −5.54 (−8.07 to −2.94) |
| Eastern Europe | 89,677 (84,819–95,109) | 3395 (1479–6437) | 58.39 (55.12–61.98) | 2.55 (1.09–4.89) | −5.07 (−6.33 to −3.79) |
| High income region | |||||
| High-income Asia Pacific | 21,608 (19,934–23,193) | 32 (3–167) | 16.94 (15.45–18.46) | 0.01 (0.00–0.06) | −6.13 (−9.95 to −2.15) |
| High-income North America | 31,180 (29,641–32,616) | 3149 (1488–5682) | 11.83 (11.28–12.35) | 0.96 (0.45–1.74) | −2.74 (−4.14 to −1.33) |
| Western Europe | 33,033 (31,404–34,542) | 1547 (974–2258) | 10.08 (9.71–10.45) | 0.28 (0.18–0.41) | −3.64 (−5.55 to −1.69) |
| Australasia | 1841 (1718–1974) | 11 (2–25) | 11.12 (10.34–11.99) | 0.04 (0.01–0.09) | −5.31 (−8.68 to −1.81) |
| Latin America and Caribbean | |||||
| Andean Latin America | 121,704 (106,006–138,172) | 16,774 (6358–28,740) | 225.47 (196.65–255.68) | 27.78 (10.53–47.55) | −3.82 (−5.01 to −2.61) |
| Caribbean | 51,753 (43,055–62,437) | 161 (46–808) | 123.00 (102.62–147.91) | 0.41 (0.12–2.06) | −3.94 (−7.17 to −0.59) |
| Southern Latin America | 19,127 (18,027–20,171) | 919 (398–1779) | 38.14 (35.97–40.18) | 1.67 (0.74–3.26) | −3.19 (−5.33 to −1.00) |
| Tropical Latin America | 175,597 (156,002–196,127) | 12,370 (3599–27,803) | 109.81 (97.68–122.46) | 6.58 (1.93–14.88) | −4.42 (−5.80 to −3.01) |
| Central Latin America | 240,956 (222,737–263,718) | 15,563 (10,261–22,529) | 104.04 (96.20–113.67) | 7.93 (5.23–11.48) | −2.68 (−4.05 to −1.30) |
| North Africa and Middle East | |||||
| North Africa and Middle East | 953,149 (813,177–1,186,437) | 79,031 (40,379–138,867) | 185.69 (158.49–230.93) | 13.74 (7.08–24.08) | −4.37 (−5.00 to −3.74) |
| South Asia | |||||
| South Asia | 3,645,872 (3,031,824–4,273,297) | 959,423 (484,294–1,553,206) | 228.41 (190.32–267.49) | 63.00 (31.79–102.03) | −2.36 (−2.86 to −1.85) |
| Southeast Asia, east Asia, and Oceania | |||||
| East Asia | 2,268,332 (1,947,322–2,627,318) | 45,581 (25,630–76,212) | 198.61 (170.68–229.97) | 6.68 (3.69–11.12) | −8.14 (−8.98 to −7.30) |
| Oceania | 27,062 (21,928–33,795) | 2105 (1010–3884) | 259.24 (210.30–322.38) | 10.51 (5.05–19.34) | −1.99 (−4.02–0.09) |
| Southeast Asia | 1,030,723 (898,445–1,218,338) | 27,229 (17,728–40,560) | 177.34 (154.64–209.25) | 4.89 (3.20–7.28) | −4.56 (−6.18 to −2.91) |
| Sub-Saharan Africa | |||||
| Central Sub-Saharan Africa | 305,071 (222,276–393,719) | 128,479 (59,859–204,950) | 272.16 (199.13–350.26) | 65.72 (31.33–103.94) | −3.62 (−3.96 to −3.28) |
| Eastern Sub-Saharan Africa | 1,053,436 (856,319–1,285,137) | 384,101 (246,486–559,266) | 272.46 (221.83–331.61) | 62.48 (40.51–90.90) | −3.08 (−3.76 to −2.40) |
| Southern Sub-Saharan Africa | 127,066 (110,619–146,145) | 19,442 (7745–39,009) | 172.02 (150.42–197.12) | 24.96 (9.96–50.12) | −1.68 (−3.51–0.18) |
| Western Sub-Saharan Africa | 1,457,578 (1,198,455–1,733,011) | 872,819 (513,360–1,305,845) | 379.38 (309.14–452.76) | 108.55 (63.85–162.60) | −1.94 (−2.55 to −1.32) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Z.; Zhang, Q.; Li, J.; Xie, N.; Zheng, Q.; Lai, Y.; Zhang, X. Contribution of Respiratory Syncytial Virus to Burden of Lower Respiratory Tract Infections: A Global Analysis of 204 Countries and Territories, 1990–2021. Trop. Med. Infect. Dis. 2025, 10, 223. https://doi.org/10.3390/tropicalmed10080223
Chen Z, Zhang Q, Li J, Xie N, Zheng Q, Lai Y, Zhang X. Contribution of Respiratory Syncytial Virus to Burden of Lower Respiratory Tract Infections: A Global Analysis of 204 Countries and Territories, 1990–2021. Tropical Medicine and Infectious Disease. 2025; 10(8):223. https://doi.org/10.3390/tropicalmed10080223
Chicago/Turabian StyleChen, Zhiwei, Qiu Zhang, Junrong Li, Naihong Xie, Qingmei Zheng, Youzhen Lai, and Xiaoyang Zhang. 2025. "Contribution of Respiratory Syncytial Virus to Burden of Lower Respiratory Tract Infections: A Global Analysis of 204 Countries and Territories, 1990–2021" Tropical Medicine and Infectious Disease 10, no. 8: 223. https://doi.org/10.3390/tropicalmed10080223
APA StyleChen, Z., Zhang, Q., Li, J., Xie, N., Zheng, Q., Lai, Y., & Zhang, X. (2025). Contribution of Respiratory Syncytial Virus to Burden of Lower Respiratory Tract Infections: A Global Analysis of 204 Countries and Territories, 1990–2021. Tropical Medicine and Infectious Disease, 10(8), 223. https://doi.org/10.3390/tropicalmed10080223






