Polyparasitic Infections: Associated Factors and Effect on the Haemoglobin Level of Children Living in Lambaréné Remote and Surrounding Rural Areas from Gabon—A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Procedures
2.3. Study Population
2.4. Ethical Consideration
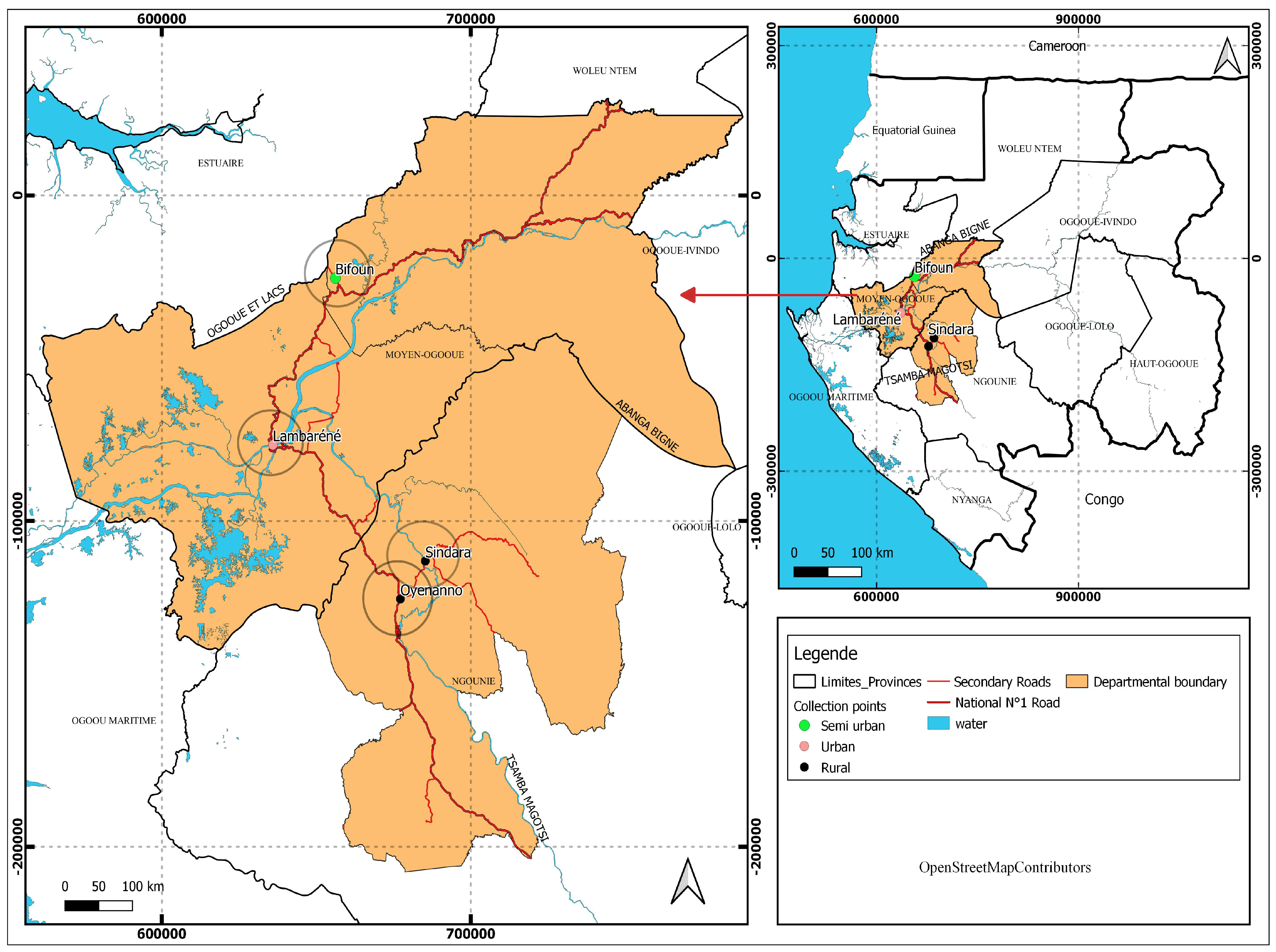
2.5. Study Site and Areas
2.6. Sample Size Calculation
2.7. Participant Recruitment and Sample Collection
2.8. Laboratory Tests
2.8.1. Direct Examination from Stool Sample
2.8.2. Kato–Katz Technique
2.8.3. Coproculture Technique
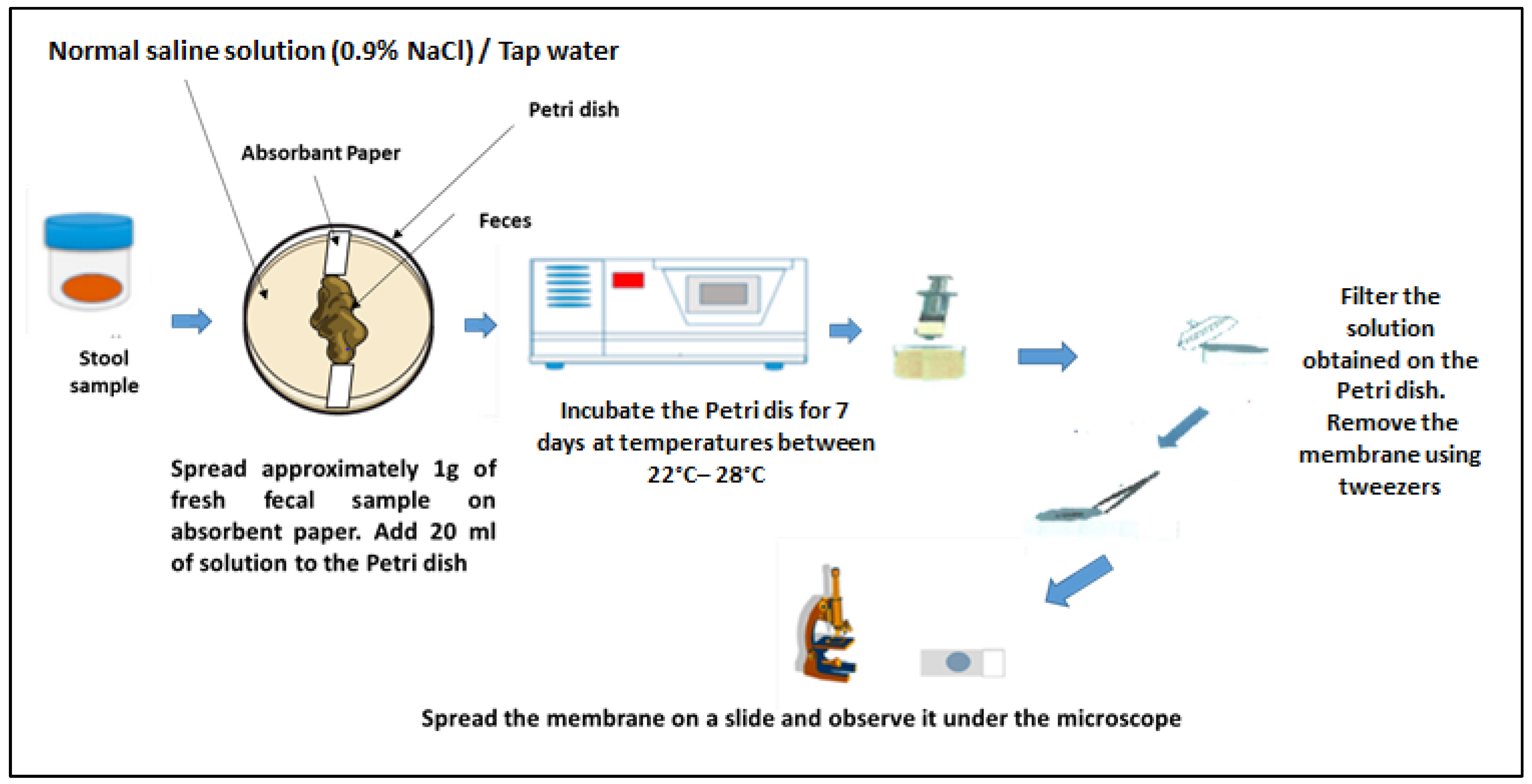
2.8.4. Harada–Mori Culture Technique
2.8.5. Urine Filtration Technique
2.8.6. Blood Sample Examination
2.8.7. Quality Control from Microscopy Results
- Case definition
- We considered any participant to be infected if their slide preparation sample presented at least one form of parasite.
- We considered a polyparasitic infection case to be any participant infected by at least two parasite groups of parasite species (the groups of parasite species considered were STH, IPS, Schistosoma spp., Plasmodium spp., or microfilariae worm species).
2.9. Statistical Analysis
3. Results
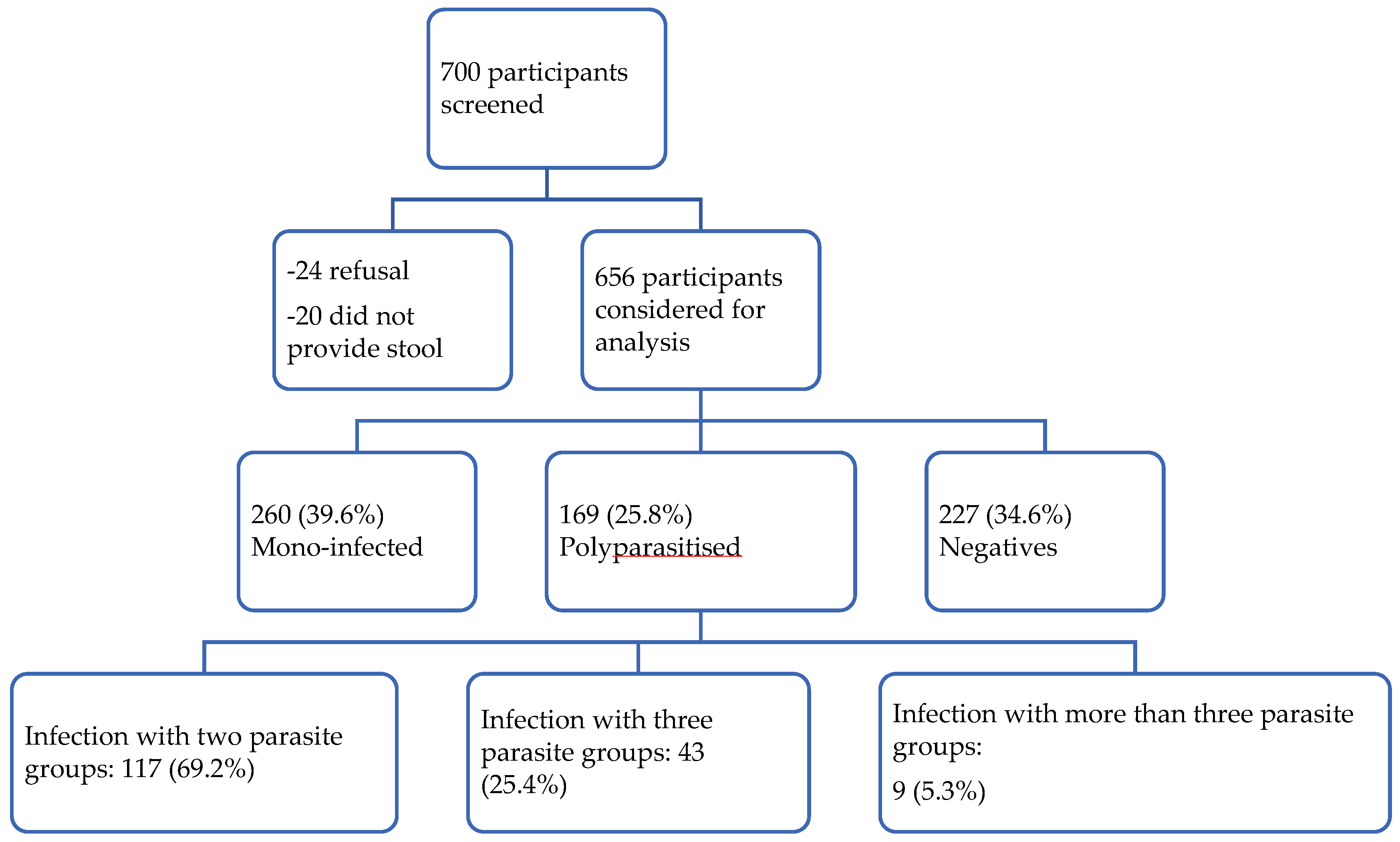
3.1. Characteristics of the Study Population
3.2. The Prevalence of Species Mono-Infection and Polyparasitic Infection
3.3. Factors Associated with Polyparasitic Infection and Its Effect on Haemoglobin Level
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bordes, F.; Morand, S. The Impact of Multiple Infections on Wild Animal Hosts: A Review. Infect. Ecol. Epidemiol. 2011, 1, 7346. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Varikuti, S.; Halsey, G.; Volpedo, G.; Hamza, O.M.; Satoskar, A.R. Host-Directed Therapies for Parasitic Diseases. Future Med. Chem. 2019, 11, 1999–2018. [Google Scholar] [CrossRef] [PubMed]
- Despommier, D.D.; Griffin, D.O.; Gwadz, R.W.; Hotez, P.J.; Knirsch, C. Parasitic Diseases, 6th ed.; Springer: Berlin/Heidelberg, Germany, 2017. [Google Scholar]
- Center for Disease Control and Prevention. What Causes of Parasitic Diseases. Parasites. Available online: https://www.cdc.gov/Parasites/Causes/Index.Html (accessed on 27 November 2024).
- World Health Organization (WHO)—Neglected Tropical Diseases—Global Report on the Neglected Tropical Diseases. Available online: https://www.who.int/Health-Topics/Neglected-Tropical-Diseases (accessed on 30 November 2024).
- Hotez, P.J.; Fenwick, A.; Savioli, L.; Molyneux, D.H. Rescuing the Bottom Billion through Control of Neglected Tropical Diseases. Lancet 2009, 373, 1570–1575. [Google Scholar] [CrossRef] [PubMed]
- Mengome, M.F.A.; Kono, H.N.; Boulingui, C.M.; M’bondoukwe, N.P.; Ngomo, J.-M.N.; Ditombi, B.M.; Ngondza, P.B.; Bisseye, C.; Mawili-Mboumba, D.P.; Akotet, M.K.B. Prevalence and Sociodemographic Factors Associated With Chronic Intestinal Polyparasitism in Non-Pregnant Adults Living In Urban and Rural Areas of Gabon. Microbiol. Infect. Dis. 2023, 7, 1–7. [Google Scholar] [CrossRef]
- Villamizar, X.; Higuera, A.; Herrera, G.; Vasquez-A, L.R.; Buitron, L.; Muñoz, L.M.; Gonzalez-C, F.E.; Lopez, M.C.; Giraldo, J.C. Molecular and Descriptive Epidemiology of Intestinal Protozoan Parasites of Children and Their Pets in Cauca, Colombia: A Cross-Sectional Study. BMC Infect. Dis. 2019, 19, 190. [Google Scholar] [CrossRef] [PubMed]
- Word Health organization (WHO). World Malaria Report; Word Health Organization: Geneve, Switzerland, 2024. [Google Scholar]
- Lebu, S.; Kibone, W.; Muoghalu, C.C.; Ochaya, S.; Salzberg, A.; Bongomin, F.; Manga, M. Soil-Transmitted Helminths: A Critical Review of the Impact of Co-Infections and Implications for Control and Elimination. PLoS Negl. Trop. Dis. 2023, 17, e0011496. [Google Scholar] [CrossRef]
- Steinmann, P.; Utzinger, J.; Du, Z.-W.; Zhou, X.-N. Chapter 2—Multiparasitism: A Neglected Reality on Global, Regional and Local Scale. Adv. Parasitol. 2024, 73, 21–50. Available online: https://www.sciencedirect.com/science/article/abs/pii/S0065308X10730025 (accessed on 27 June 2025).
- Dejon-Agobé, J.C.; Zinsou, J.F.; Honkpehedji, Y.J.; Ateba-Ngoa, U.; Edoa, J.-R.; Adegbite, B.R.; Mombo-Ngoma, G.; Agnandji, S.T.; Ramharter, M.; Kremsner, P.G.; et al. Schistosoma Haematobium Effects on Plasmodium Falciparum Infection Modified by Soil-Transmitted Helminths in School-Age Children Living in Rural Areas of Gabon. PLoS Negl. Trop. Dis. 2018, 12, e0006663. [Google Scholar] [CrossRef]
- Dejon-Agobé, J.C.; Chassem-Lapue, C.; Nguema-Moure, P.A.; Maloum, M.N.; Lontchi, R.L.; Saidou, M.; Djida, Y.; Edoa, J.R.; Honkpéhèdji, Y.J.; Zinsou, J.F.; et al. Community surveys of the prevalence, distribution, and coinfection of helminth and protozoan infections in semiurban and rural areas of Gabon, Central Africa. PLoS Neglected Trop. Dis. 2025, 19, e0013161. [Google Scholar] [CrossRef]
- Akue, J.P.; Nkoghe, D.; Padilla, C.; Moussavou, G.; Moukana, H.; Mbou, R.A.; Ollomo, B.; Leroy, E.M. Epidemiology of Concomitant Infection Due to Loa Loa and Mansonella Perstans in Gabon. PLoS Negl. Trop. Dis. 2011, 5, e1329. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Honkpéhèdji, Y.J.; Adegbite, B.R.; Zinsou, J.F.; Dejon-Agobé, J.C.; Edoa, J.-R.; Manego, R.Z.; McCall, M.; Ngwese, M.M.; Mougeni, F.L.; Mombo-Ngoma, G.; et al. Association of Low Birth Weight and Polyparasitic Infection during Pregnancy in Lambaréné, Gabon. Trop. Med. Int. Health 2021, 26, 973–981. [Google Scholar] [CrossRef] [PubMed]
- Nguema-Moure, P.A.; Nzamba, M.M.; Manouana, G.P.; Laclong, L.R.-A.; Mirabau, M.N.; Edoa, J.R.; Zinsou, J.F.; Meulah, B.; Mahmoudou, S.; Mirna, N.E.; et al. A Randomized Assessors-Blind Clinical Trial to Evaluate the Safety and the Efficacy of Albendazole Alone and in Combination with Mebendazole or Pyrantel for the Treatment of Trichuris Trichiura Infection in School-Aged Children in Lambaréné and Surroundings. Antimicrob. Agents Chemother. 2024, 68, e01211-23. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dejon-Agobé, J.C.; Honkpehedji, Y.J.; Zinsou, J.F.; Edoa, J.R.; Adégbitè, B.R.; Mangaboula, A.; Agnandji, S.T.; Mombo-Ngoma, G.; Ramharter, M.; Kremsner, P.G.; et al. Epidemiology of Schistosomiasis and Soil-Transmitted Helminth Coinfections among Schoolchildren Living in Lambaréné, Gabon. Am. J. Trop. Med. Hyg. 2020, 103, 325–333. [Google Scholar] [CrossRef] [PubMed]
- Ngwese, M.M.; Manouana, G.P.; Nguema-Moure, P.A.; Ramharter, M.; Esen, M.; Adégnika, A.A. Diagnostic Techniques of Soil-Transmitted Helminths: Impact on Control Measures. Trop. Med. Infect. Dis. 2020, 5, 93. [Google Scholar] [CrossRef]
- Nguema-Moure, P.A.; Dejon-Agobé, J.C.; Laclong Lontchi, R.-A.; Manouana, G.P.; Nzamba Maloum, M.; Meulah, B.; Manfoumbi Mabicka, D.C.; Nzame Ngome, M.E.; Kremsner, P.G.; Adegnika, A.A. Effect of Anthelmintic Treatment on the Agreement Between Real-Time Polymerase Chain Reaction (RT-PCR) and Kato–Katz Microscopic Technique in the Diagnosis of Soil-Transmitted Helminth Infections. Parasitologia 2024, 4, 345–357. [Google Scholar] [CrossRef]
- Chessbrough, M. Distric Laboratory Practices in Tropical Countries, 2nd ed.; Cambridge University Press: Cambridge, UK, 2006. [Google Scholar] [CrossRef]
- Meulah, B.; Oyibo, P.; Hoekstra, P.T.; Nguema-Moure, P.A.; Maloum, M.N.; Laclong-Lontchi, R.A.; Honkpehedji, Y.J.; Bengtson, M.; Hokke, C.; Corstjens, P.L.A.M.; et al. Validation of Artificial Intelligence-Based Digital Microscopy for Automated Detection of Schistosoma Haematobium Eggs in Urine in Gabon. PLoS Negl. Trop. Dis. 2024, 18, e0011967. [Google Scholar] [CrossRef]
- Mischlinger, J.; Pitzinger, P.; Veletzky, L.; Groger, M.; Zoleko-Manego, R.; Adegnika, A.A.; Agnandji, S.T.; Lell, B.; Kremsner, P.G.; Mombo-Ngoma, G.; et al. Validity and Reliability of Methods to Microscopically Detect and Quantify Malaria Parasitaemia. Trop. Med. Int. Health 2018, 23, 980–991. [Google Scholar] [CrossRef]
- Parkouda, S.; Saidou, M.; Bisseye, C. Microfilariae Prevalence and Its Association with Anemia Among First-Time Blood Donors in Lambaréné, Gabon. Balk. Med. J. 2024, 41, 139–143. [Google Scholar] [CrossRef]
- Eyayu, T.; Kiros, T.; Workineh, L.; Sema, M.; Damtie, S.; Hailemichael, W.; Dejen, E.; Tiruneh, T. Prevalence of Intestinal Parasitic Infections and Associated Factors among Patients Attending at Sanja Primary Hospital, Northwest Ethiopia: An Institutional-Based Cross-Sectional Study. PLoS ONE 2021, 16, e0247075. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aschale, A.; Adane, M.; Getachew, M.; Faris, K.; Gebretsadik, D.; Sisay, T.; Dewau, R.; Chanie, M.G.; Muche, A.; Zerga, A.A.; et al. Water, Sanitation, and Hygiene Conditions and Prevalence of Intestinal Parasitosis among Primary School Children in Dessie City, Ethiopia. PLoS ONE 2021, 16, e0245463. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Odoemene, S.N.; Oluwole, A.S.; Mogaji, H.O.; Adegbola, M.V.; Omitola, O.O.; Bayegun, A.A.; Ojo, D.A.; Sam-Wobo, S.O.; Ekpo, U.F. Polyparasitism with Malaria and Intestinal Parasite Infections among Infants and Preschool-Aged Children in Egbedore, Osun State, Nigeria. J. Parasitol. Res. 2020, 2020, 8810148. [Google Scholar] [CrossRef] [PubMed]
- Orish, V.N.; Ofori-Amoah, J.; Amegan-Aho, K.H.; Osei-Yeboah, J.; Lokpo, S.Y.; Osisiogu, E.U.; Agordoh, P.D.; Adzaku, F.K. Prevalence of Polyparasitic Infection Among Primary School Children in the Volta Region of Ghana. Open Forum Infect. Dis. 2019, 6, ofz153. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sumbele, I.U.N.; Otia, O.V.; Bopda, O.S.M.; Ebai, C.B.; Kimbi, H.K.; Nkuo-Akenji, T. Polyparasitism with Schistosoma Haematobium, Plasmodium and Soil-Transmitted Helminths in School-Aged Children in Muyuka, Cameroon, Following Implementation of Control Measures: A Cross Sectional Study. Infect. Dis. Poverty 2021, 10, 14. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hürlimann, E.; Yapi, R.B.; Houngbedji, C.A.; Schmidlin, T.; Kouadio, B.A.; Silué, K.D.; Ouattara, M.; N’Goran, E.K.; Utzinger, J.; Raso, G. The Epidemiology of Polyparasitism and Implications for Morbidity in Two Rural Communities of Côte d’Ivoire. Parasites Vectors 2014, 7, 81. [Google Scholar] [CrossRef] [PubMed]
- Kono, H.N.; Mengome, M.F.A.; Ngondza, B.P.; Matotou, R.H.S.; Akomezoghe, L.N.; Ekomi, B.; Ditombi, B.C.M.; Lengongo, J.V.K.; Ngomo, J.M.N.; M’Bondoukwé, N.P.; et al. C-Reactive Protein and High-Sensitivity C-Reactive Protein Levels in Asymptomatic Intestinal Parasite Carriers from Urban and Rural Areas of Gabon. PLoS Negl. Trop. Dis. 2024, 18, e0011282. [Google Scholar] [CrossRef]
- M’bondoukw, N.P.; Kendjo, E.; Mawili-Mboumba, D.P.; Koumba, L.J.V.; Mbouoronde, C.O.; Nkoghe, D.; Touré, F.; Bouyou-Akotet, M.K. Prevalence of and Risk Factors for Malaria, Filariasis, and Intestinal Parasites as Single Infections or Co-Infections in Different Settlements of Gabon, Central Africa. Infect. Dis. Poverty 2018, 7, 6, Erratum in Infect. Dis. Poverty 2018, 7, 38. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- M’bondoukwé, P.N.; Mawili-Mboumba, D.P.; Manga, M.F.; Kombila, M.; Akotet, M.K.B. Prevalence of Soil-Transmitted Helminths and Intestinal Protozoa in Shanty Towns of Libreville, Gabon. Int. J. Trop. Dis. Health 2016, 20, 1–9. [Google Scholar] [CrossRef]
- Atabati, H.; Kassiri, H.; Shamloo, E.; Akbari, M.; Atamaleki, A.; Sahlabadi, F.; Linh, N.T.T.; Rostami, A.; Fakhri, Y.; Khaneghah, A.M. The Association between the Lack of Safe Drinking Water and Sanitation Facilities with Intestinal Entamoeba Spp Infection Risk: A Systematic Review and Meta-Analysis. PLoS ONE. 2020, 15, e0237102. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bustinduy, A.L.; Parraga, I.M.; Thomas, C.L.; Mungai, P.L.; Mutuku, F.; Muchiri, E.M.; Kitron, U.; King, C.H. Impact of Polyparasitic Infections on Anaemia and Undernutrition among Kenyan Children Living in a Schistosoma Haematobium-Endemic Area. Am. J. Trop. Med. Hyg. 2013, 88, 433–440. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Anemia—World Health Organization (WHO). Available online: https://www.who.int/health-topics/anaemia#tab=tab_1 (accessed on 1 February 2025).
| Characteristic | Frequency (%) | [95% CI] |
|---|---|---|
| Age group (years) | ||
| 2 to 5 | 238 (36.3%) | [32.7–40.3] |
| 6 to 10 | 249 (38.0%) | [34.3–41.7] |
| 11 to 17 | 169 (25.8%) | [25.8–29.2] |
| Areas | ||
| Lambaréné (semi-urban) | 59 (9.0%) | [7.0–11.5] |
| Sur. areas LBN (Ogooué et Lacs) | 369 (56.3%) | [52.4–60.0] |
| Remote areas LBN (Tsamba-Magotsi) | 227 (34.6%) | [31.0–38.3] |
| Parasite Species (n = 656) | Prevalence (%) | [IC 95%] | Parasite Count |
|---|---|---|---|
| Any STH | 280 (42.7) | [39.0–46.4] | - |
| Trichiurus trichiurus | 213 (32.5) | [29.0–36.1] | 1513 EPG |
| Ascaris lumbricoides | 144 (21.9) | [18.9–25.3] | 43825 EPG |
| Strongyloides stercoralis | 64 (9.8) | [7.5–12.4] | 12 Larvae |
| Hookworms | 62 (9.5) | [7.4–11.9] | 372 EPG |
| Schistosoma haematobium | 131 (19.9) | [34.7–45.3] | 136 eggs/10 mL |
| Any blood filaria species | 49 (7.5) | [7.5–9.40] | - |
| Mansonella perstans | 32 (4.9) | [3.2–6.8] | 5 P/mL |
| Loa loa | 17 (2.6) | [1.4–3.8] | 6 P/mL |
| Blood protozoa (P. falciparum) | 65 (9.9) | [7.6–12.2] | 1582 P/µL |
| Any intestinal protozoa species | 140 (21.3%) | [18.2–24.4] | - |
| Blastocystis hominis | 36 (5.5%) | [4.0–7.5] | - |
| Giardia duodenalis | 29 (4.4%) | [3.0–6.2] | - |
| Entamoeba coli | 25 (3.8%) | [2.4–5.3] | - |
| Iodamoeba bütschlii | 16 (2.4%) | [1.5–3.9] | - |
| Endolimax nana | 18 (2.7%) | [1.7–4.3] | - |
| Entamoeba histolytica/dispar/hartmanni | 16 (2.4%) | [1.5–3.9] | - |
| Polyparasitic Infection | Bivariable Analysis | Multivariable Analysis | ||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | No n = 487 | Yes n = 169 | OR | 95% CI | p-Value | OR | 95% CI | p-Value |
| Age (years) | 7.0 (4.0, 10.0) 1 | 8.0 (5.0, 11.0) 1 | 1.02 | 0.97, 1.06 | 0.45 | 1.05 | 0.93, 1.19 | 0.4 |
| Sex | ||||||||
| F | 236 (73%) | 89 (27%) | — | — | — | — | ||
| M | 251 (76%) | 80 (24%) | 0.85 | 0.59, 1.20 | 0.35 | 0.85 | 0.58, 1.26 | 0.4 |
| Areas | ||||||||
| Lambaréné | 30 (51%) | 29 (49%) | — | — | — | — | ||
| Remote areas LBN (Tsamba-Magotsi) | 132 (58%) | 96 (42%) | 0.75 | 0.42, 1.34 | 0.33 | 0.75 | 0.29, 1.98 | 0.6 |
| Sur. North and Sud LBN (Ogooué et Lacs) | 325 (88%) | 44 (12%) | 0.14 | 0.08, 0.25 | <0.001 | 0.22 | 0.09, 0.55 | 0.001 * |
| Washing hands before meals | ||||||||
| Often | 26 (70%) | 11 (30%) | — | — | — | — | ||
| Rarely | 76 (78%) | 21 (22%) | 0.65 | 0.28, 1.57 | 0.33 | 1.06 | 0.34, 3.36 | >0.9 |
| Sometimes | 385 (74%) | 137 (26%) | 0.84 | 0.41, 1.82 | 0.64 | 0.89 | 0.35, 2.31 | 0.8 |
| Water source | ||||||||
| Tap water | 98 (84%) | 19 (16%) | — | — | — | — | ||
| Mixed | 285 (84%) | 56 (16%) | 1.01 | 0.58, 1.83 | 0.96 | 0.83 | 0.43, 1.68 | 0.6 |
| River | 104 (53%) | 94 (47%) | 4.66 | 2.70, 8.39 | <0.001 | 2.09 | 1.06, 4.25 | 0.038 * |
| House type | ||||||||
| Cement brick | 14 (47%) | 16 (53%) | — | — | — | — | ||
| Planck house | 473 (76%) | 153 (24%) | 0.28 | 0.13, 0.59 | <0.001 | 0.59 | 0.20, 1.73 | 0.3 |
| Barefoot walking | ||||||||
| Often | 218 (74%) | 77 (26%) | — | — | — | — | ||
| Rarely | 58 (79%) | 15 (21%) | 0.73 | 0.38, 1.34 | 0.33 | 0.57 | 0.14, 2.29 | 0.4 |
| Sometimes | 211 (73%) | 77 (27%) | 1.03 | 0.71, 1.49 | 0.86 | 1.65 | 0.77, 3.53 | 0.2 |
| Sanitation | ||||||||
| WC or Latrine | 332 (81%) | 77 (19%) | — | — | — | — | ||
| Non-conventional | 155 (63%) | 92 (37%) | 2.56 | 1.79, 3.67 | <0.001 | 2.00 | 1.25, 3.22 | 0.004 * |
| Bivariable Analysis | Multivariable Analysis | |||||
|---|---|---|---|---|---|---|
| Characteristic | β | [95% CI] | p-Value | β | [95% CI] | p-Value |
| Polyparasitic infection | ||||||
| No | Ref | — | — | — | ||
| Yes | −0.48 | [−0.92–−0.04] | 0.03 * | −0.60 | [−1.1–−0.12] | 0.01 * |
| Sex | ||||||
| F | Ref | — | — | — | ||
| M | −0.21 | [−0.65–0.24] | 0.36 | −0.40 | [−0.86–0.07] | 0.09 |
| Age (years) | −0.04 | [−0.11–0.02] | 0.16 | −0.01 | [−0.18–0.16] | 0.92 |
| Areas | ||||||
| Lambaréné | Ref | — | — | — | ||
| Remote areas LBN (Tsamba-Magotsi) | 0.62 | [−1.3–2.5] | 0.52 | 2.4 | [−0.27–5.1] | 0.07 |
| Sur. areas LBN (Ogooué et Lacs) | 0.21 | [−1.7–2.1] | 0.83 | 1.9 | [−0.86–4.6] | 0.18 |
| Washing hands before meals | ||||||
| Often | Ref | — | — | — | ||
| Rarely | 1.3 | [−0.41–2.9] | 0.14 | 1.1 | [−1.1–3.3] | 0.32 |
| Sometimes | 0.93 | [−0.64–2.5] | 0.24 | 0.94 | [−0.91–2.8] | 0.32 |
| Water source | ||||||
| Tap water | Ref | — | — | — | ||
| Mixed | 0.73 | [−0.10–1.6] | 0.08 | 0.60 | [−0.32–1.5] | 0.20 |
| River | 0.39 | [−0.45–1.2] | 0.36 | 0.22 | [−0.84–1.3] | 0.68 |
| House type | ||||||
| Cement brick | Ref | — | — | — | ||
| Planck house | −1.1 | [−3.8–1.6] | 0.43 | −4.1 | [−7.9–−0.34] | 0.03 * |
| Barefoot walking | ||||||
| Often | Ref | — | — | — | ||
| Rarely | −0.29 | [−1.1–0.46] | 0.44 | 0.21 | [−1.4–1.9] | 0.80 |
| Sometimes | −0.39 | [−0.87–0.08] | 0.11 | 0.02 | [−0.85–0.89] | 0.97 |
| Sanitation | ||||||
| WC or Latrine | Ref | — | — | — | ||
| Non-conventional | 0.23 | [−0.22–0.68] | 0.32 | 0.12 | [−0.40–0.65] | 0.64 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguema-Moure, P.A.; Adegbite, B.R.; Nzamba Maloum, M.; Dejon-Agobé, J.-C.; Laclong Lontchi, R.-A.; Honkpehedji, Y.J.; Manfoumbi Mabicka, D.-C.; Chassem-Lapue, C.; Sole, P.W.; Ogoula, S.; et al. Polyparasitic Infections: Associated Factors and Effect on the Haemoglobin Level of Children Living in Lambaréné Remote and Surrounding Rural Areas from Gabon—A Cross-Sectional Study. Trop. Med. Infect. Dis. 2025, 10, 218. https://doi.org/10.3390/tropicalmed10080218
Nguema-Moure PA, Adegbite BR, Nzamba Maloum M, Dejon-Agobé J-C, Laclong Lontchi R-A, Honkpehedji YJ, Manfoumbi Mabicka D-C, Chassem-Lapue C, Sole PW, Ogoula S, et al. Polyparasitic Infections: Associated Factors and Effect on the Haemoglobin Level of Children Living in Lambaréné Remote and Surrounding Rural Areas from Gabon—A Cross-Sectional Study. Tropical Medicine and Infectious Disease. 2025; 10(8):218. https://doi.org/10.3390/tropicalmed10080218
Chicago/Turabian StyleNguema-Moure, Paul Alvyn, Bayode Romeo Adegbite, Moustapha Nzamba Maloum, Jean-Claude Dejon-Agobé, Roméo-Aimé Laclong Lontchi, Yabo Josiane Honkpehedji, Danny-Carrel Manfoumbi Mabicka, Christian Chassem-Lapue, Pavel Warry Sole, Stephane Ogoula, and et al. 2025. "Polyparasitic Infections: Associated Factors and Effect on the Haemoglobin Level of Children Living in Lambaréné Remote and Surrounding Rural Areas from Gabon—A Cross-Sectional Study" Tropical Medicine and Infectious Disease 10, no. 8: 218. https://doi.org/10.3390/tropicalmed10080218
APA StyleNguema-Moure, P. A., Adegbite, B. R., Nzamba Maloum, M., Dejon-Agobé, J.-C., Laclong Lontchi, R.-A., Honkpehedji, Y. J., Manfoumbi Mabicka, D.-C., Chassem-Lapue, C., Sole, P. W., Ogoula, S., M’Baidigium, F. B., Mouloungui-Mavoungou, J., Ramharter, M., Gottfried Kremsner, P., & Adegnika, A. A. (2025). Polyparasitic Infections: Associated Factors and Effect on the Haemoglobin Level of Children Living in Lambaréné Remote and Surrounding Rural Areas from Gabon—A Cross-Sectional Study. Tropical Medicine and Infectious Disease, 10(8), 218. https://doi.org/10.3390/tropicalmed10080218









