HIV/AIDS Mortality Trends in Lang Son, Vietnam: Insights from a Population-Based Mortality Registration from 2005 to 2018
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
2.2. Data Analysis
3. Results
3.1. HIV/AIDS-Related Mortality
3.2. HIV/AIDS-Related Mortality by Gender
3.3. HIV/AIDS-Related Age-Specific Mortality Rates
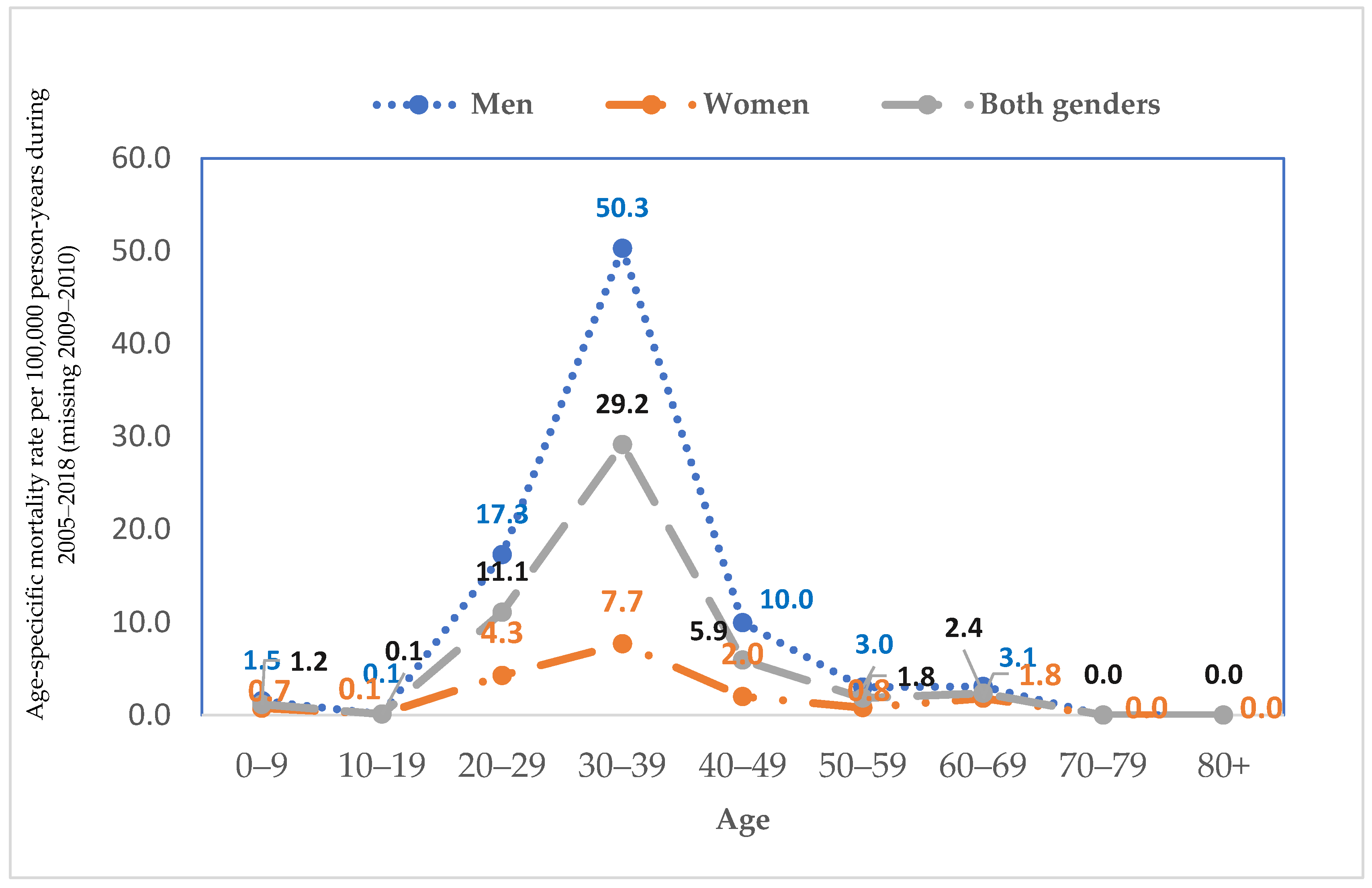
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AIDS | acquired immunodeficiency syndrome. |
| ASRs | age-standardized mortality rates |
| CDC | Center for Disease Control and Prevention |
| CHSs | commune health stations |
| MRR | mortality rate ratios |
| PLWH | people living with HIV |
| WHO | World Health Organization |
References
- UNAIDS. AIDS by the Number. Available online: https://www.unaids.org/en (accessed on 23 May 2024).
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development. Department of Economic and Social Affairs. Available online: https://sustainabledevelopment.un.org/post2015/transformingourworld/publication (accessed on 23 May 2024).
- Dombrowski, J.C.; Simoni, J.M.; Katz, D.A.; Golden, M.R. Barriers to HIV Care and Treatment Among Participants in a Public Health HIV Care Relinkage Program. AIDS Patient Care STDS 2015, 29, 279–287. [Google Scholar] [CrossRef]
- Martinez, J.; Harper, G.; Carleton, R.A.; Hosek, S.; Bojan, K.; Clum, G.; Ellen, J. The impact of stigma on medication adherence among HIV-positive adolescent and young adult females and the moderating effects of coping and satisfaction with health care. AIDS Patient Care STDS 2012, 26, 108–115. [Google Scholar] [CrossRef]
- Pellowski, J.A. Barriers to care for rural people living with HIV: A review of domestic research and health care models. J. Assoc. Nurses AIDS Care 2013, 24, 422–437. [Google Scholar] [CrossRef] [PubMed]
- UNAIDS. Country-Viet Nam. 2023. Available online: https://www.unaids.org/en/regionscountries/countries/vietnam (accessed on 15 May 2024).
- Socialist Republic of Vietnam. Contry Report-15 Years Achieving the Viet Nam Millennium Development Goals. 2015. Available online: https://vietnam.un.org/sites/default/files/2019-08/Bao%20cao%20TIENG%20ANH%20-%20MDG%202015_trinh%20TTCP.pdf (accessed on 15 April 2024).
- Hong, T.T.; Phuong Hoa, N.; Walker, S.M.; Hill, P.S.; Rao, C. Completeness and reliability of mortality data in Viet Nam: Implications for the national routine health management information system. PLoS ONE 2018, 13, e0190755. [Google Scholar] [CrossRef] [PubMed]
- Le, N.T.; Nguyen, T.V.; Nguyen, H.T.; Ikeda, S. Mortality due to HIV/AIDS in Viet Nam: Time trend and related socio-economic status in some populations and periods from 2005 to 2014. AIDS Care 2020, 32, 843–849. [Google Scholar] [CrossRef] [PubMed]
- Des Jarlais, D.C.; Johnston, P.; Friedmann, P.; Kling, R.; Liu, W.; Ngu, D.; Chen, Y.; Hoang, T.V.; Donghua, M.; Van, L.K.; et al. Patterns of HIV prevalence among injecting drug users in the cross-border area of Lang Son Province, Vietnam, and Ning Ming County, Guangxi Province, China. BMC Public Health 2005, 5, 89. [Google Scholar] [CrossRef] [PubMed]
- Lang Son People’s Committee. Plan on Ensuring Financial Support for HIV/AIDS Prevention and Control Activities in Lang Son Province for the 2015–2020 Period. 2015. Available online: https://thuvienphapluat.vn/van-ban/Tai-chinh-nha-nuoc/Ke-hoach-75-KH-UBND-2015-bao-dam-tai-chinh-phong-chong-HIVAIDS-Lang-Son-giai-doan-2015-2020-287209.aspx (accessed on 10 May 2024).
- Stevenson, M.; Hung, D.V.; Hoang, T.H.; Mai Anh, L.; Nguyen Thi Hong, T.; Le Tran, N. Evaluation of the Vietnamese A6 Mortality Reporting System: All-Cause Mortality. Asia Pac. J. Public Health 2015, 27, 733–742. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, M.R.; Ngoan le, T.; Hung, D.V.; Huong Tu, N.T.; Mai, A.L.; Ivers, R.Q.; Huong, H.T. Evaluation of the Vietnamese A6 mortality reporting system: Injury as a cause of death. Inj. Prev. 2012, 18, 360–364. [Google Scholar] [CrossRef]
- Ngoan le, T.; Lua, N.T.; Hang, L.T. Cancer mortality pattern in Viet Nam. Asian Pac. J. Cancer Prev. 2007, 8, 535–538. [Google Scholar] [PubMed]
- Cancer Mortality in a Hanoi Population, Viet Nam, 1996-2005. Asian Pac. J. Cancer Prev. 2006, 7, 127–130. Available online: https://journal.waocp.org/article_24441.html (accessed on 10 May 2024).
- Ahmad, O.B.; Boschi Pinto, C.; Lopez, A.D. Age Standardization of Rates: A New WHO Standard; GPE Discussion Paper Series: No 31; World Health Organization: Geneva, Switzerland, 2001; pp. 10–12. [Google Scholar]
- Aldaz, P.; Moreno-Iribas, C.; Egüés, N.; Irisarri, F.; Floristan, Y.; Sola-Boneta, J.; Martínez-Artola, V.; Sagredo, M.; Castilla, J. Mortality by causes in HIV-infected adults: Comparison with the general population. BMC Public Health 2011, 11, 300. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Wu, Z.; McGoogan, J.M.; Shi, C.X.; Li, A.; Dou, Z.; Ma, Y.; Qin, Q.; Brookmeyer, R.; Detels, R.; et al. Immediate Antiretroviral Therapy Decreases Mortality Among Patients With High CD4 Counts in China: A Nationwide, Retrospective Cohort Study. Clin. Infect. Dis. 2018, 66, 727–734. [Google Scholar] [CrossRef]
- Trickey, A.; McGinnis, K.; Gill, M.J.; Abgrall, S.; Berenguer, J.; Wyen, C.; Hessamfar, M.; Reiss, P.; Kusejko, K.; Silverberg, M.J.; et al. Longitudinal trends in causes of death among adults with HIV on antiretroviral therapy in Europe and North America from 1996 to 2020: A collaboration of cohort studies. Lancet HIV 2024, 11, e176–e185. [Google Scholar] [CrossRef] [PubMed]
- Ashraf, H.; Nadeem, A.; Ashfaq, H.; Fatima, T.; Ahmed, S.; Nadeem, Z.A.; Saleh, A. Disparities in mortality trends of adults with HIV in the USA: A comprehensive examination across 2 decades. Medicine 2024, 103, e38570. [Google Scholar] [CrossRef] [PubMed]
- Coelho, L.; Grinsztejn, B.; Castilho, J.L.; De Boni, R.; Quintana, M.S.; Campos, D.P.; Ribeiro, S.R.; Pacheco, A.G.; Veloso, V.G.; Luz, P.M. Mortality in HIV-infected women, heterosexual men, and men who have sex with men in Rio de Janeiro, Brazil: An observational cohort study. Lancet HIV 2016, 3, e490–e498. [Google Scholar] [CrossRef]
- Gao, D.; Zou, Z.; Dong, B.; Zhang, W.; Chen, T.; Cui, W.; Ma, Y. Secular trends in HIV/AIDS mortality in China from 1990 to 2016: Gender disparities. PLoS ONE 2019, 14, e0219689. [Google Scholar] [CrossRef] [PubMed]
- Gheibi, Z.; Dianatinasab, M.; Haghparast, A.; Mirzazadeh, A.; Fararouei, M. Gender difference in all-cause mortality of people living with HIV in Iran: Findings from a 20-year cohort study. HIV Med. 2020, 21, 659–667. [Google Scholar] [CrossRef] [PubMed]
- Girum, T.; Wasie, A.; Lentiro, K.; Muktar, E.; Shumbej, T.; Difer, M.; Shegaze, M.; Worku, A. Gender disparity in epidemiological trend of HIV/AIDS infection and treatment in Ethiopia. Arch. Public Health 2018, 76, 51. [Google Scholar] [CrossRef]
- Frank, T.D.; Carter, A.; Jahagirdar, D.; Biehl, M.H.; Douwes-Schultz, D.; Larson, S.L.; Arora, M.; Dwyer-Lindgren, L.; Steuben, K.M.; Abbastabar, H.; et al. Global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2017, and forecasts to 2030, for 195 countries and territories: A systematic analysis for the Global Burden of Diseases, Injuries, and Risk Factors Study 2017. Lancet HIV 2019, 6, e831–e859. [Google Scholar] [CrossRef] [PubMed]
- Orza, L.; Bass, E.; Bell, E.; Crone, E.T.; Damji, N.; Dilmitis, S.; Tremlett, L.; Aidarus, N.; Stevenson, J.; Bensaid, S.; et al. In Women’s Eyes: Key Barriers to Women’s Access to HIV Treatment and a Rights-Based Approach to their Sustained Well-Being. Health Hum. Rights 2017, 19, 155–168. [Google Scholar]
- Toth, M.; Messer, L.C.; Quinlivan, E.B. Barriers to HIV care for women of color living in the Southeastern US are associated with physical symptoms, social environment, and self-determination. AIDS Patient Care STDS 2013, 27, 613–620. [Google Scholar] [CrossRef]
- Park, E.; Stockman, J.K.; Thrift, B.; Nicole, A.; Smith, L.R. Structural Barriers to Women’s Sustained Engagement in HIV Care in Southern California. AIDS Behav. 2020, 24, 2966–2974. [Google Scholar] [CrossRef]
- Liu, Y.; Osborn, C.Y.; Qian, H.Z.; Yin, L.; Xiao, D.; Ruan, Y.; Simoni, J.M.; Zhang, X.; Shao, Y.; Vermund, S.H.; et al. Barriers and Facilitators of Linkage to and Engagement in HIV Care Among HIV-Positive Men Who Have Sex with Men in China: A Qualitative Study. AIDS Patient Care STDS 2016, 30, 70–77. [Google Scholar] [CrossRef] [PubMed]

| Gender | Year | Cause | Total | Crude Rate & | ASR @ | WHO $ |
|---|---|---|---|---|---|---|
| Men | 2005–2018 | B20-B24 | 594 | 13.2 | 10.8 | 12.3 |
| Women | 2005–2018 | B20-B24 | 113 | 2.5 | 2.2 | 2.4 |
| Both genders | 2005–2018 | B20-B24 | 707 | 7.8 | 6.6 | 7.4 |
| Year | Case | Crude Rate & | WHO $ | MRR (95%CI) $$ | p |
|---|---|---|---|---|---|
| Both genders | |||||
| 2005 | 170 | 23.6 | 22.3 | 1 (reference) | |
| 2006 | 153 | 20.9 | 19.6 | 0.885 (0.711, 1.101) | 0.27 |
| 2007 | 117 | 15.9 | 15.2 | 0.673 (0.532, 0.852) | 0.001 |
| 2008 | 98 | 13.1 | 12.6 | 0.556 (0.434, 0.713) | <0.001 |
| 2011 | 38 | 5.2 | 5.1 | 0.219 (0.154, 0.312) | <0.001 |
| 2012 | 27 | 3.6 | 3.4 | 0.153 (0.102, 0.230) | <0.001 |
| 2013 | 22 | 3.0 | 2.9 | 0.126 (0.081, 0.197) | <0.001 |
| 2014 | 27 | 3.5 | 3.3 | 0.146 (0.097, 0.220) | <0.001 |
| 2015 | 16 | 2.0 | 1.9 | 0.086 (0.052, 0.144) | <0.001 |
| 2016 | 13 | 1.7 | 1.5 | 0.070 (0.040, 0.123) | <0.001 |
| 2017 | 15 | 1.9 | 1.8 | 0.080 (0.047, 0.135) | <0.001 |
| 2018 | 11 | 1.4 | 1.3 | 0.059 (0.032, 0.109) | <0.001 |
| Men | |||||
| 2005 | 147 | 41.1 | 38.0 | 1 (reference) | |
| 2006 | 130 | 35.7 | 32.9 | 0.869 (0.687, 1.100) | 0.24 |
| 2007 | 103 | 28.2 | 26.0 | 0.685 (0.533, 0.882) | 0.003 |
| 2008 | 80 | 21.9 | 20.4 | 0.525 (0.400, 0.689) | <0.001 |
| 2011 | 27 | 7.4 | 7.1 | 0.180 (0.120, 0.272) | <0.001 |
| 2012 | 21 | 5.7 | 5.3 | 0.138 (0.087, 0.217) | <0.001 |
| 2013 | 17 | 4.6 | 4.5 | 0.113 (0.068, 0.186) | <0.001 |
| 2014 | 25 | 6.4 | 6.1 | 0.157 (0.102, 0.239) | <0.001 |
| 2015 | 15 | 3.8 | 3.7 | 0.093 (0.055, 0.159) | <0.001 |
| 2016 | 9 | 2.3 | 2.1 | 0.056 (0.029, 0.110) | <0.001 |
| 2017 | 11 | 2.8 | 2.6 | 0.068 (0.037, 0.125) | <0.001 |
| 2018 | 9 | 2.3 | 2.2 | 0.056 (0.029, 0.110) | <0.001 |
| Women | |||||
| 2005 | 23 | 6.4 | 6.3 | 1 (reference) | |
| 2006 | 23 | 6.3 | 5.9 | 0.983 (0.552, 1.753) | 0.95 |
| 2007 | 14 | 3.8 | 3.9 | 0.596 (0.306, 1.157) | 0.13 |
| 2008 | 18 | 4.8 | 4.7 | 0.755 (0.407, 1.399) | 0.37 |
| 2011 | 11 | 3.0 | 3.0 | 0.469 (0.229, 0.963) | 0.039 |
| 2012 | 6 | 1.6 | 1.5 | 0.251 (0.102, 0.617) | 0.003 |
| 2013 | 5 | 1.3 | 1.3 | 0.212 (0.081, 0.558) | 0.002 |
| 2014 | 2 | 0.5 | 0.5 | 0.080 (0.019, 0.340) | 0.001 |
| 2015 | 1 | 0.3 | 0.2 | 0.040 (0.005, 0.294) | 0.002 |
| 2016 | 4 | 1.0 | 1.0 | 0.159 (0.055, 0.461) | 0.001 |
| 2017 | 4 | 1.0 | 1.1 | 0.157 (0.054, 0.455) | 0.001 |
| 2018 | 2 | 0.5 | 0.5 | 0.080 (0.019, 0.338) | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Le, N.T.; Le, L.T.; Ta, N.D.T.; Nguyen, H.M.; Ha, T. HIV/AIDS Mortality Trends in Lang Son, Vietnam: Insights from a Population-Based Mortality Registration from 2005 to 2018. Trop. Med. Infect. Dis. 2025, 10, 52. https://doi.org/10.3390/tropicalmed10020052
Le NT, Le LT, Ta NDT, Nguyen HM, Ha T. HIV/AIDS Mortality Trends in Lang Son, Vietnam: Insights from a Population-Based Mortality Registration from 2005 to 2018. Tropical Medicine and Infectious Disease. 2025; 10(2):52. https://doi.org/10.3390/tropicalmed10020052
Chicago/Turabian StyleLe, Ngoan Tran, Linh Thuy Le, Ngan Dieu Thi Ta, Hung Manh Nguyen, and Toan Ha. 2025. "HIV/AIDS Mortality Trends in Lang Son, Vietnam: Insights from a Population-Based Mortality Registration from 2005 to 2018" Tropical Medicine and Infectious Disease 10, no. 2: 52. https://doi.org/10.3390/tropicalmed10020052
APA StyleLe, N. T., Le, L. T., Ta, N. D. T., Nguyen, H. M., & Ha, T. (2025). HIV/AIDS Mortality Trends in Lang Son, Vietnam: Insights from a Population-Based Mortality Registration from 2005 to 2018. Tropical Medicine and Infectious Disease, 10(2), 52. https://doi.org/10.3390/tropicalmed10020052






