Prevalence of Intestinal Protozoa Among Patients Living with HIV in the Peruvian Amazon
Abstract
1. Introduction
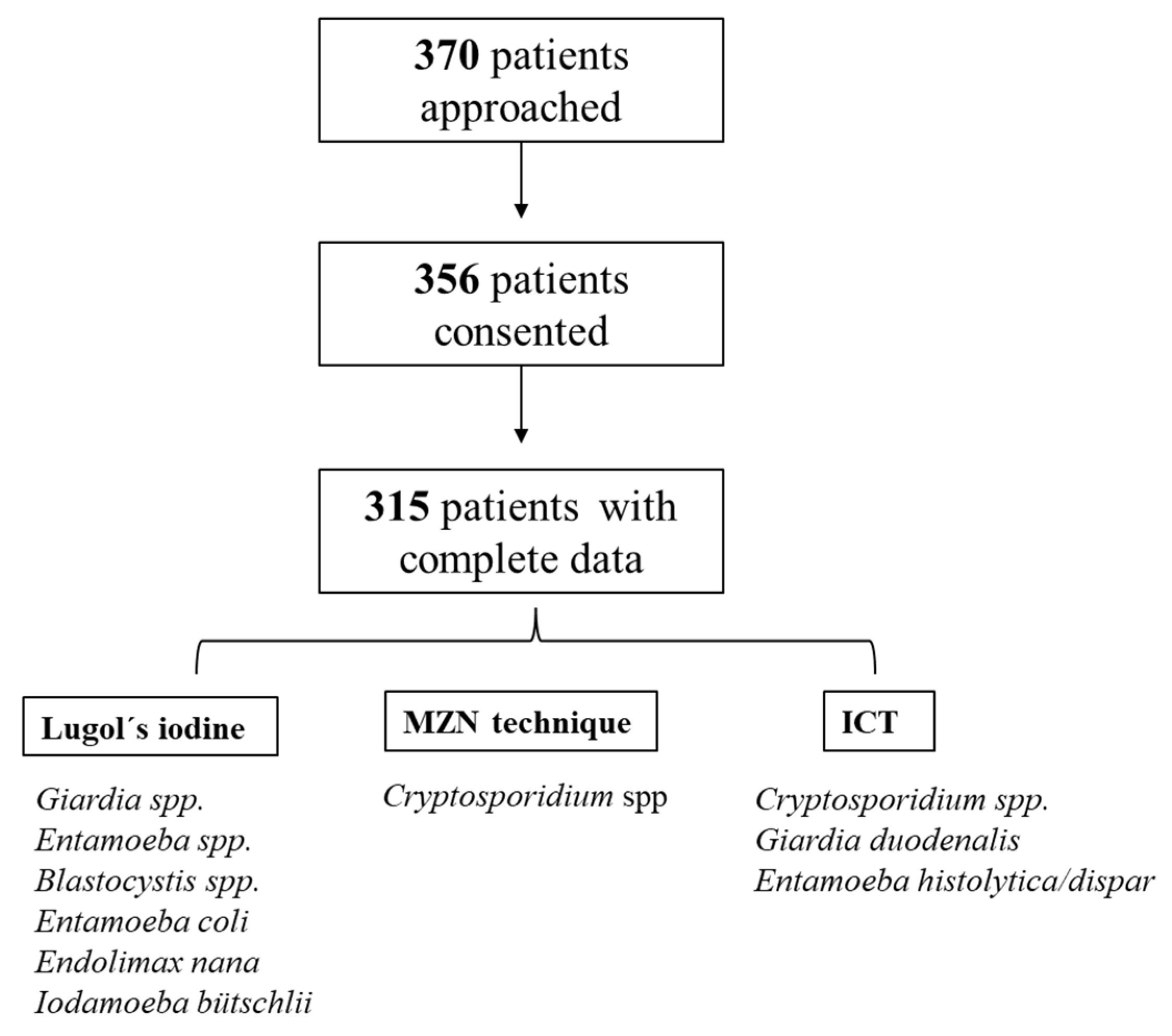
2. Materials and Methods
2.1. Study Population and Inclusion/Exclusion Criteria
2.2. Enrollment Procedures
2.3. Stool Specimen Processing, Staining, and Microscopy
- -
- Lugol’s iodine solution: Each fecal specimen was analyzed using Lugol’s iodine solution to enhance the diagnostic accuracy of direct microscopy of wet mounts, looking for Giardia spp., Entamoeba spp., Blastocystis spp., Entamoeba coli, Endolimax nana, and Iodamoeba bütschlii. Due to the expected high volume of samples and the labor-intensive nature of some techniques, a concentration method was not performed. Moreover, given the anticipated high prevalence of intestinal protozoa in this population and the use of additional diagnostic methods (ICT and MZN), the benefit of performing a concentration technique was considered limited [20]. Lugol’s iodine stains glycogen and other cytoplasmic structures, enhancing the visualization of protozoan cysts and trophozoites. Giardia cysts typically appear oval with internal nuclei and axonemes [21], while Entamoeba cysts show characteristic nuclear structures and chromatoid bodies, and the trophozoite could appear with red blood cells in the cytoplasm, which allows it to be distinguished from the commensal E. dispar, even if it is not a pathognomonic sign [22]. Commensal protozoa, including Blastocystis, display variable shapes and internal granularity, whereas E. coli, E. nana, and I. bütschlii cysts can be distinguished by their size, number of nuclei, and cytoplasmic inclusions [23]. This technique is simple, fast, and useful, and provides a cost-effective approach for preliminary identification of intestinal protozoa in laboratory settings.
- -
- Modified Ziehl–Neelsen stain (MZN): Briefly, each stool sample was homogenized, and a thin smear was prepared on a slide. After heat-fixing, slides were stained with phenolated fuchsin, decolorized with 3% acid alcohol, counterstained with methylene blue, air-dried, and observed under immersion oil at 100× magnification [24]. To assure high-quality microscopy results, the two study staff microscopists were trained by the Cayetano Heredia University’s Microbiology Service and Selva Amazonica Civil Association before study initiation.
- -
- Crypto + Giardia + Entamoeba ICT (CerTest®®, Certest Biotec, Zaragoza, Spain) [25]: This one-step combo card test is a colored chromatographic immunoassay for the simultaneous qualitative detection of Cryptosporidium spp. (via Anti-Crypto MAb (clone CR23) and inactivated Cryptosporidium parvum antigen (native extract)), Giardia duodenalis (via α1-giardin protein and/or the cyst wall protein CWP1, detecting both trophozoites and cysts) and Entamoeba histolytica/dispar (via antigens from both species) in stool samples [26]. It is used by mixing a small amount of stool sample with the provided buffer, applying the mixture to the test cassette, and waiting the specified time (usually 10–15 min). The appearance of lines in the result window indicates the presence of antigens from Cryptosporidium spp. and/or Giardia duodenalis and/or Entamoeba histolytica/dispar.
2.4. Data Analysis
- Overall Giardia spp. prevalence: combined positivity in Lugol’s microscopy and ICT;
- Overall Entamoeba histolytica/dispar prevalence: combined positivity in Lugol’s microscopy and ICT;
- Overall Cryptosporidium spp. prevalence: combined positivity in MZN staining and ICT.
2.5. Ethical Considerations
3. Results
3.1. Description of the Cohort
3.2. Stool Diagnosis
3.2.1. Prevalence of Giardia spp., Entamoeba spp., Blastocystis spp., and Commensal Pathogens
3.2.2. Prevalence of Cryptosporidium spp.
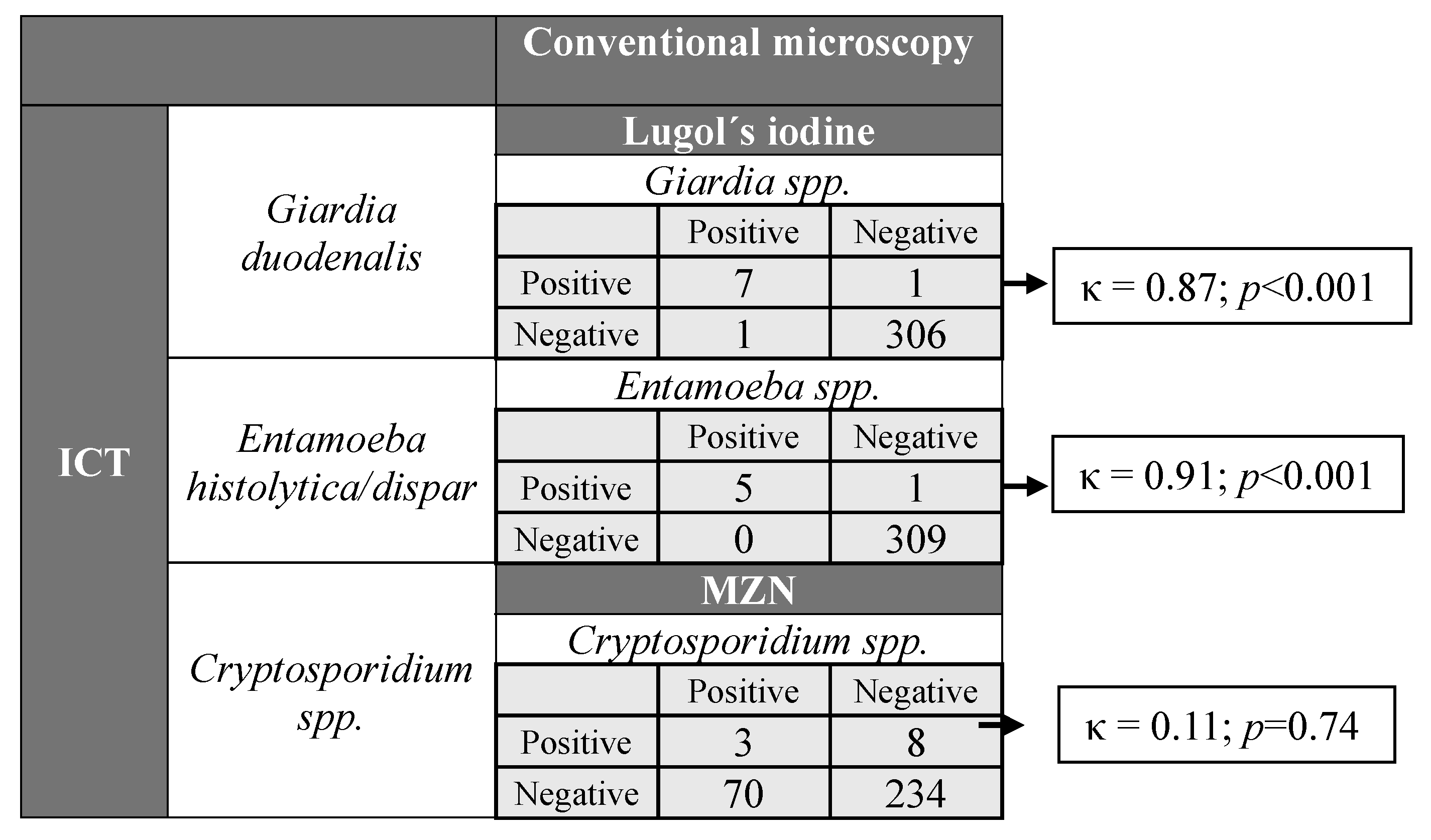
3.2.3. Evaluation of Diagnostic Test Agreement
3.2.4. Prevalence of Co-Infection with Giardia spp., Entamoeba spp., Cryptosporidium spp., and Blastocystis spp.
3.2.5. Epidemiological Risk Factors Associated with Pathogenic Intestinal Protozoa Positivity
3.2.6. Prevalence Pattern of Protozoa in People Referring Diarrhea
4. Discussion
4.1. Cryptosporidium spp. Prevalence in Stool
4.2. Giardia and Entamoeba spp. Prevalence in Stool
4.3. Prevalence of Blastocystis and Commensal Pathogens in Stool
4.4. Risk Factors for Pathogenic Intestinal Protozoa Acquisition
4.5. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HIV | Human immunodeficiency virus |
| PWH | People with HIV |
| MZN | Modified Ziehl–Neelsen staining |
| ICT | Immunochromatography |
| CI | Confidence interval |
| AOR | Adjusted odds ratio |
| ELISA | Enzyme-linked immunosorbent assay |
| IQRs | Interquartile ranges |
| N/A | Not applicable |
| ART | Anti-retroviral therapy |
References
- Zorbozan, O.; Quliyeva, G.; Tunali, V.; Ozbilgin, A.; Turgay, N.; Gokengin, A.D. Intestinal Protozoa in Hiv-Infected Patients: A Retrospective Analysis. Turk. J. Parasitol. 2018, 42, 187–190. [Google Scholar] [CrossRef]
- Bednarska, M.; Jankowska, I.; Pawelas, A.; Piwczyńska, K.; Bajer, A.; Wolska-Kuśnierz, B.; Wielopolska, M.; Welc-Falęciak, R. Prevalence of Cryptosporidium, Blastocystis, and Other Opportunistic Infections in Patients with Primary and Acquired Immunodeficiency. Parasitol. Res. 2018, 117, 2869–2879. [Google Scholar] [CrossRef]
- Bahmani, P.; Maleki, A.; Sadeghi, S.; Shahmoradi, B.; Ghahremani, E. Prevalence of Intestinal Protozoa Infections and Associated Risk Factors among Schoolchildren in Sanandaj City, Iran. Iran. J. Parasitol. 2017, 12, 108–116. [Google Scholar]
- Darlan, D.M.; Rozi, M.F.; Nurangga, M.A.; Amsari, L.C. Cryptosporidium sp. and Blastocystishominis Findings: A Cross-Sectional Study among Healthy Versus Immunocompromised Individuals. Int. J. Psychosoc. Rehabil. 2020, 24, 2346–2351. [Google Scholar] [CrossRef]
- Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV; National Institutes of Health: Bethesda, MD, USA; HIV Medicine Association: Arlington, VA, USA; Infectious Diseases Society of America: Arlington, VA, USA. Available online: https://clinicalinfo.hiv.gov/sites/default/files/guidelines/archive/adult-adolescent-oi-2025-07-14.pdf (accessed on 20 May 2025).
- Gerace, E.; Lo Presti, V.D.M.; Biondo, C. Cryptosporidium Infection: Epidemiology, Pathogenesis, and Differential Diagnosis. Eur. J. Microbiol. Immunol. 2019, 9, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Shirley, D.-A.T.; Moonah, S.N.; Kotloff, K.L. Burden of Disease from Cryptosporidiosis. Curr. Opin. Infect. Dis. 2012, 25, 555–563. [Google Scholar] [CrossRef]
- Aghamolaie, S.; Rostami, A.; Fallahi, S.; Biderouni, F.T.; Haghighi, A.; Salehi, N. Evaluation of Modified Ziehl-Neelsen, Direct Fluorescent-Antibody and PCR Assay for Detection of Cryptosporidium spp. in Children Faecal Specimens. J. Parasit. Dis. Off. Organ. Indian Soc. Parasitol. 2016, 40, 958–963. [Google Scholar] [CrossRef]
- Nash, T.E.; Ohl, C.A.; Thomas, E.; Subramanian, G.; Keiser, P.; Moore, T.A. Treatment of Patients with Refractory Giardiasis. Clin. Infect. Dis. 2001, 33, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Chakrabarti, S. Multiple Amoebic Liver Abscess As Initial Manifestation in Hiv Sero-Positive Male. J. Clin. Diagn. Res. JCDR 2015, 9, OD04–OD05. [Google Scholar] [CrossRef]
- Ocaña-Losada, C.; Cuenca-Gómez, J.; Cabezas-Fernández, M.; Vázquez-Villegas, J.; Soriano-Pérez, M.; Cabeza-Barrera, I.; Salas-Coronas, J. Características Clínicas y Epidemiológicas de La Parasitación Intestinal Por Blastocystis Hominis. Rev. Clin. Esp. 2018, 218, 115–120. [Google Scholar] [CrossRef]
- Khorshidvand, Z.; Khazaei, S.; Amiri, M.; Taherkhani, H.; Mirzaei, A. Worldwide Prevalence of Emerging Parasite Blastocystis in Immunocompromised Patients: A Systematic Review and Meta-Analysis. Microb. Pathog. 2021, 152, 104615. [Google Scholar] [CrossRef]
- Wawrzyniak, I.; Poirier, P.; Viscogliosi, E.; Dionigia, M.; Texier, C.; Delbac, F.; Alaoui, H.E. Blastocystis, an Unrecognized Parasite: An Overview of Pathogenesis and Diagnosis. Ther. Adv. Infect. Dis. 2013, 1, 167–178. [Google Scholar] [CrossRef]
- Espinosa Aranzales, A.F.; Radon, K.; Froeschl, G.; Rondón, Á.M.P.; Delius, M. Prevalence and Risk Factors for Intestinal Parasitic Infections in Pregnant Women Residing in Three Districts of Bogotá, Colombia. BMC Public Health 2018, 18, 1071. [Google Scholar] [CrossRef] [PubMed]
- Marcos, L.A.; Gotuzzo, E. Intestinal Protozoan Infections in the Immunocompromised Host. Curr. Opin. Infect. Dis. 2013, 26, 295. [Google Scholar] [CrossRef] [PubMed]
- Cárcamo, C.; Hooton, T.; Wener, M.H.; Weiss, N.S.; Gilman, R.; Arevalo, J.; Carrasco, J.; Seas, C.; Caballero, M.; Holmes, K.K. Etiologies and Manifestations of Persistent Diarrhea in Adults with HIV-1 Infection: A Case-Control Study in Lima, Peru. J. Infect. Dis. 2005, 191, 11–19. [Google Scholar] [CrossRef]
- García, C.; Rodríguez, E.; Do, N.; López de Castilla, D.; Terashima, A.; Gotuzzo, E. Parasitosis Intestinal En El Paciente Con Infección VIH-SIDA [Intestinal Parasitosis in Patients with HIV-AIDS]. Rev. Gastroenterol. Peru. 2006, 26, 21–24. [Google Scholar] [PubMed]
- Vergaray, S.; Paima-Olivari, R.; Runzer-Colmenares, F.M. Parasitosis intestinal y estado inmunológico en pacientes adultos con infección por VIH del Centro Médico Naval “Cirujano Mayor Santiago Távara”. Horiz. Méd. Lima 2019, 19, 32–36. [Google Scholar] [CrossRef]
- Centro Nacional de Epidemiología; Prevención y Control de Enfermedades. Situación Epidemiológica Del VIH-Sida En El Perú. Boletín VIH, II Trimestre-2024. Available online: https://www.Dge.Gob.Pe/Epipublic/Uploads/Vih-Sida/Vih-sida_20246_16_153419.pdf (accessed on 20 February 2025).
- Wahdini, S.; Putra, V.P.; Sungkar, S. The Prevalence of Intestinal Protozoan Infections among Children in Southwest Sumba Based on the Type of Water Sources. Infect. Chemother. 2021, 53, 519. [Google Scholar] [CrossRef]
- Calchi, M.; Acurero, E.; Villalobos, R.; Colina, M.; Di Toro, L.; Villalobos, C. Comparación de Técnicas de Laboratorio Para El Diagnóstico de Giardia Intestinalis. Kasmera 2014, 42, 32–40. [Google Scholar]
- Botero, D.; Restrepo, M. Parasitosis Humanas, 5th ed.; Medellín, Corporación Para Investigaciones Biológicas: Medellín, Colombia, 2012; pp. 38–56. [Google Scholar]
- Flórez, A.C.; García, D.A.; Moncada, L.; Beltrán, M. Prevalencia de microsporidios y otros parásitos intestinales en pacientes con infección por VIH, Bogotá, 2001. Biomédica 2003, 23, 274. [Google Scholar] [CrossRef][Green Version]
- Henriksen, S.A.; Pohlenz, J.F. Staining of Cryptosporidia by a Modified Ziehl-Neelsen Technique. Acta Vet. Scand. 1981, 22, 594–596. [Google Scholar] [CrossRef]
- CerTest Biotec, S.L. Crypto + Giardia + Entamoeba Rapid Test: One-Step Combo Card Test–Specifications; CerTest Biotec: San Mateo de Gállego, Spain. Available online: https://www.certest.es/products/crypto-giardia-entamoeba-3/ (accessed on 6 November 2025).
- Tokyo Future Style Co., Ltd. IVD Raw Material—Infectious Disease; Tokyo Future Style: Tokyo, Japan, 2025; Available online: https://En.Tokyofuturestyle.Com/Ivd-Raw-Material-Infectious-Disease (accessed on 6 November 2025).
- Newcombe, R.G. Two-Sided Confidence Intervals for the Single Proportion: Comparison of Seven Methods. Stat. Med. 1998, 17, 857–872. [Google Scholar] [CrossRef]
- Benson, C.A.; Kaplan, J.E.; Masur, H.; Pau, A.; Holmes, K.K.; CDC.; National Institutes of Health; Infectious Diseases Society of America. Treating Opportunistic Infections Among HIV-Infected Adults and Adolescents: Recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association/Infectious Diseases Society of America. MMWR Recomm. Rep. Morb. Mortal. Wkly. Rep. Recomm. Rep. 2004, 53, 1–112. [Google Scholar] [CrossRef]
- Cama, V.A.; Bern, C.; Sulaiman, I.M.; Gilman, R.H.; Ticona, E.; Vivar, A.; Kawai, V.; Vargas, D.; Zhou, L.; Xiao, L. Cryptosporidium Species and Genotypes in HIV-Positive Patients in Lima, Peru. J. Eukaryot. Microbiol. 2003, 50, 531–533. [Google Scholar] [CrossRef] [PubMed]
- Dankwa, K.; Nuvor, S.V.; Obiri-Yeboah, D.; Feglo, P.K.; Mutocheluh, M. Occurrence of Cryptosporidium Infection and Associated Risk Factors among HIV-Infected Patients Attending ART Clinics in the Central Region of Ghana. Trop. Med. Infect. Dis. 2021, 6, 210. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, A.; Munoz, M.; Gómez, N.; Tabares, J.; Segura, L.; Salazar, Á.; Restrepo, C.; Ruíz, M.; Reyes, P.; Qian, Y.; et al. Molecular Epidemiology of Giardia, Blastocystis and Cryptosporidium among Indigenous Children from the Colombian Amazon Basin. Front. Microbiol. 2017, 8, 248. [Google Scholar] [CrossRef]
- Ahmed, S.A.A.; Quattrocchi, A.; Elzagawy, S.M.; Karanis, P.; Gad, S.E.M. Diagnostic Performance of Toluidine Blue Stain for Direct Wet Mount Detection of Cryptosporidium Oocysts: Qualitative and Quantitative Comparison to the Modified Ziehl-Neelsen Stain. Diagn. Basel Switz. 2023, 13, 2557. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Stool Specimens–Staining Procedures; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2023. Available online: https://www.cdc.gov/dpdx/diagnosticprocedures/stool/staining.html (accessed on 30 September 2025).
- Omoruyi, B.E.; Nwodo, U.U.; Udem, C.S.; Okonkwo, F.O. Comparative Diagnostic Techniques for Cryptosporidium Infection. Molecules 2014, 19, 2674–2683. [Google Scholar] [CrossRef] [PubMed]
- CerTest Biotec, S.L. Cryptosporidium Parvum (Crypto-2) Rapid Test; CerTest Biotec: San Mateo de Gállego, Spain. Available online: https://www.certest.es/products/cryptosporidium-parvum-crypto/ (accessed on 6 November 2025).
- Manouana, G.P.; Lorenz, E.; Mbong Ngwese, M.; Nguema Moure, P.A.; Maiga Ascofaré, O.; Akenten, C.W.; Amuasi, J.; Rakotozandrindrainy, N.; Rakotozandrindrainy, R.; Mbwana, J.; et al. Performance of a Rapid Diagnostic Test for the Detection of Cryptosporidium spp. in African Children Admitted to Hospital with Diarrhea. PLoS Negl. Trop. Dis. 2020, 14, e0008448. [Google Scholar] [CrossRef]
- Ghafari, R.; Rafiei, A.; Tavalla, M.; Moradi Choghakabodi, P.; Nashibi, R.; Rafiei, R. Prevalence of Cryptosporidium Species Isolated from HIV/AIDS Patients in Southwest of Iran. Comp. Immunol. Microbiol. Infect. Dis. 2018, 56, 39–44. [Google Scholar] [CrossRef]
- Cama, V.A.; Bern, C.; Roberts, J.; Cabrera, L.; Sterling, C.R.; Ortega, Y.; Gilman, R.H.; Xiao, L. Cryptosporidium Species and Subtypes and Clinical Manifestations in Children, Peru. Emerg. Infect. Dis. 2008, 14, 1567–1574. [Google Scholar] [CrossRef] [PubMed]
- Mahdavi, F.; Shams, M.; Sadrebazzaz, A.; Shamsi, L.; Omidian, M.; Asghari, A.; Hassanipour, S.; Salemi, A.M. Global Prevalence and Associated Risk Factors of Diarrheagenic Giardia duodenalis in HIV/AIDS Patients: A Systematic Review and Meta-Analysis. Microb. Pathog. 2021, 160, 105202. [Google Scholar] [CrossRef]
- Peréz Cordón, G.; Cordova Paz Soldan, O.; Vargas Vásquez, F.; Velasco Soto, J.R.; Sempere Bordes, L.; Sánchez Moreno, M.; Rosales, M.J. Prevalence of Enteroparasites and Genotyping of Giardia lamblia in Peruvian Children. Parasitol. Res. 2008, 103, 459–465. [Google Scholar] [CrossRef]
- Chincha, L.O.; Bernabé-Ortiz, A.; Samalvides, C.F.; Soto, A.L.; Gotuzzo, H.E.; Terashima, I.A. Parasite Intestinal Infection and Factors Associated with Coccidian Infection in Adults at Public Hospital in Lima, Peru. Rev. Chil. Infectol. 2009, 26, 440–444. [Google Scholar] [CrossRef]
- Marcos, L.; Maco, V.; Machicado, A.; Samalvides, F.; Terashima, A.; Quijano, C.; Gotuzzo, E. Diferencias de Prevalencia de Parasitosis Intestinal Entre Los Hospitales Militar y Regional de Iquitos, Loreto-Perú. Rev. Médica Hered. 2002, 41, 4. Available online: https://www.fihu.org.pe/revista/numeros/2002/julago02/185-187.html (accessed on 6 November 2025).
- Pascual, G.; Oliver, J.A.I.; Hernandez, A.; Salazar, N. Parasitos intestinales en pobladores de dos localidades de Yurimaguas, Alto Amazonas, Loreto, Perú. Neotrop. Helminthol. 2010, 4, 127–136. [Google Scholar] [CrossRef]
- Ibáñez, H.N.; Jara, C.C.; Guerra, M.A.; Díaz, L.E. Prevalencia del enteroparasitismo en escolares de comunidades andinas nativas del Alto Marañón, Amazonas, Perú. Rev. Peru. Med. Exp. Salud Pública 2004, 21, 126–133. [Google Scholar]
- Sannella, A.R.; Suputtamongkol, Y.; Wongsawat, E.; Cacciò, S.M. A Retrospective Molecular Study of Cryptosporidium Species and Genotypes in HIV-Infected Patients from Thailand. Parasit. Vectors 2019, 12, 91. [Google Scholar] [CrossRef] [PubMed]
- Adeyemo, F.E.; Singh, G.; Reddy, P.; Bux, F.; Stenström, T.A. Efficiency of Chlorine and UV in the Inactivation of Cryptosporidium and Giardia in Wastewater. PLoS ONE 2019, 14, e0216040. [Google Scholar] [CrossRef]
- Han, M.; Xiao, S.; An, W.; Sang, C.; Li, H.; Ma, J.; Yang, M. Co-Infection Risk Assessment of Giardia and Cryptosporidium with HIV Considering Synergistic Effects and Age Sensitivity Using Disability-Adjusted Life Years. Water Res. 2020, 175, 115698. [Google Scholar] [CrossRef]
- Garcia, C.; Chincha, O.; Leon, M.; Iglesias, D.; Barletta, F.; Mercado, E.; Ochoa, T. High Frequency of Diarrheagenic Escherichia coli in Human Immunodeficiency Virus (HIV) Patients with and without Diarrhea in Lima, Peru. Am. J. Trop. Med. Hyg. 2010, 82, 1118–1120. [Google Scholar] [CrossRef] [PubMed]
- Molina Recio, G.; Moreno Rojas, R.; García Rodríguez, M.; Vaquero Abellán, M. Valoración Nutricional de Los Platos Más Frecuentemente Consumidos En Un Barrio Marginal de Iquitos, Amazonía Peruana. Nutr. Hosp. 2016, 33, 70–79. [Google Scholar] [CrossRef]
- Robles-Cabrera, M.X.; Maguiña, J.L.; Gonzales-Huerta, L.; Panduro-Correa, V.; Dámaso-Mata, B.; Pecho-Silva, S.; Navarro-Solsol, A.C.; Rabaan, A.A.; Rodríguez-Morales, A.J.; Arteaga-Livias, K. Blastocystis species and Gastrointestinal Symptoms in Peruvian Adults Attended in a Public Hospital. Infect. Chemother. 2021, 53, 374–380. [Google Scholar] [CrossRef]
- Fontanelli Sulekova, L.; Gabrielli, S.; Furzi, F.; Milardi, G.L.; Biliotti, E.; De Angelis, M.; Iaiani, G.; Fimiani, C.; Maiorano, M.; Mattiucci, S.; et al. Molecular Characterization of Blastocystis Subtypes in HIV-Positive Patients and Evaluation of Risk Factors for Colonization. BMC Infect. Dis. 2019, 19, 876. [Google Scholar] [CrossRef]
- Salazar-Sánchez, R.S.; Ascuña-Durand, K.; Ballón-Echegaray, J.; Vásquez-Huerta, V.; Martínez-Barrios, E.; Castillo-Neyra, R. Socio-Demographic Determinants Associated with Blastocystis Infection in Arequipa, Peru. Am. J. Trop. Med. Hyg. 2020, 104, 700–707. [Google Scholar] [CrossRef] [PubMed]
- Ntonifor, N.H.; Tamufor, A.S.W.; Abongwa, L.E. Prevalence of Intestinal Parasites and Associated Risk Factors in HIV Positive and Negative Patients in Northwest Region, Cameroon. Sci. Rep. 2022, 12, 16747. [Google Scholar] [CrossRef] [PubMed]
- Feleke, D.G.; Ali, A.; Bisetegn, H.; Andualem, M. Intestinal Parasitic Infections and Associated Factors among People Living with HIV Attending Dessie Referral Hospital, Dessie Town, North-East Ethiopia: A Cross-Sectional Study. AIDS Res. Ther. 2022, 19, 19. [Google Scholar] [CrossRef]
- Nahn Junior, E.P.; de Oliveira, E.C.; Barbosa, M.J.; Mareco, T.C.d.S.; Brígido, H.A. Protocolo Brasileño Para Infecciones de Transmisión Sexual 2020: Infecciones Entéricas de Transmisión Sexual. Epidemiol. E Serviços Saúde 2021, 30, e2020598. [Google Scholar] [CrossRef]
- McNeil, C.J.; Kirkcaldy, R.D.; Workowski, K. Enteric Infections in Men Who Have Sex With Men. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2022, 74, S169–S178. [Google Scholar] [CrossRef]
- Ettinger, S.; Castle, J.C.; Robinson, J.; Pinto-Sander, N.; Richardson, D. The Characteristics of Men Who Have Sex with Men with Blastocystis: A Systematic Review. Int. J. STD AIDS 2025, 36, 841–848. [Google Scholar] [CrossRef]
- Escolà-Vergé, L.; Arando, M.; Vall, M.; Rovira, R.; Espasa, M.; Sulleiro, E.; Armengol, P.; Zarzuela, F.; Barberá, M.-J. Outbreak of Intestinal Amoebiasis among Men Who Have Sex with Men, Barcelona (Spain), October 2016 and January 2017. Eurosurveillance 2017, 22, 30581. [Google Scholar] [CrossRef] [PubMed]
- Di Benedetto, M.A.; Di Piazza, F.; Amodio, E.; Taormina, S.; Romano, N.; Firenze, A. Prevalence of Sexually Transmitted Infections and Enteric Protozoa among Homosexual Men in Western Sicily (South Italy). J. Prev. Med. Hyg. 2012, 53, 181–185. [Google Scholar] [PubMed]
- Chessell, C.; Rabuszko, L.; Richardson, D.; Llewellyn, C. Factors Associated with the Sexual Transmission of Strongyloides stercoralis in Men Who Have Sex with Men: A Systematic Review. J. Eur. Acad. Dermatol. Venereol. JEADV 2024, 38, 673–679. [Google Scholar] [CrossRef] [PubMed]
- To, B.; Chai, N.; Fitzpatrick, C.; Richardson, D. Factors Associated with Cryptosporidium in Men Who Have Sex with Men: A Systematic Review. Int. J. STD AIDS 2024, 35, 668–674. [Google Scholar] [CrossRef]
- Mohebali, M.; Yimam, Y.; Woreta, A. Cryptosporidium Infection among People Living with HIV/AIDS in Ethiopia: A Systematic Review and Meta-Analysis. Pathog. Glob. Health 2020, 114, 183–193. [Google Scholar] [CrossRef]
- Tian, L.-G.; Wang, T.-P.; Lv, S.; Wang, F.-F.; Guo, J.; Yin, X.-M.; Cai, Y.-C.; Dickey, M.K.; Steinmann, P.; Chen, J.-X. HIV and Intestinal Parasite Co-Infections among a Chinese Population: An Immunological Profile. Infect. Dis. Poverty 2013, 2, 18. [Google Scholar] [CrossRef]
| Variables | Pathogenic Protozoa Positive (N = 92) | Pathogenic Protozoa Negative (N = 223) | OR | p |
|---|---|---|---|---|
| Male, % (n/N) | 60.9 (56/92) | 64.6 (144/223) | 0.85 | 0.54 |
| Age, mean ± SD, years | 42 ± 12 | 41 ± 12 | 1.26 | 0.39 |
| Hospital attended, % (n/N) | ||||
| Hospital of Iquitos | 26.1 (24/92) | 10.8 (24/223) | 2.93 | <0.001 |
| Regional Hospital of Loreto | 73.9 (68/92) | 89.2 (199/223) | ||
| Residence, % (n/N) | ||||
| Iquitos district | 33.7 (31/92) | 34.5 (77/223) | N/A | 0.58 |
| Punchana district | 29.3 (27/92) | 25.1 (56/223) | ||
| Belen district | 15.2 (14/92) | 15.7 (35/223) | ||
| San Juan district | 16.3 (15/92) | 22.0 (49/223) | ||
| Outside of Iquitos | 5.4 (5/92) | 2.7 (6/223) | ||
| Occupation, % (n/N) | ||||
| Unemployed or student (yes) | 38.1 (35/92) | 46.2 (103/223) | N/A | 0.19 |
| Cattle, agriculture or construction (yes) | 16.3 (15/92) | 15.2 (34/223) | ||
| Craft work (yes) | 4.3 (4/92) | 4.5 (10/223) | ||
| Intellectual work a (yes) | 15.2 (14/92) | 6.7 (15/223) | ||
| Self-employment (yes) | 26.1 (24/92) | 27.4 (61/223) | ||
| Education, % (n/N) | ||||
| None (yes) | 3.3 (3/92) | 2.7 (6/223) | N/A | 0.31 |
| Attended primary school (yes) | 22.2 (20/92) | 14.3 (32/223) | ||
| Attended secondary school (yes) | 48.9 (45/92) | 59.2 (132/223) | ||
| Attended university (yes) | 26.1 (24/92) | 23.8 (53/223) | ||
| Epidemiological risk factors, % (n/N) | ||||
| Lives with dogs/cats/farm animals (yes) | 69.6 (64/92) | 70.0 (156/223) | 0.98 | 0.94 |
| Walks barefoot (yes) | 33.7 (31/92) | 26.0 (58/223) | 1.45 | 0.17 |
| Resides in a rural location b (yes) | 30.4 (28/92) | 33.6 (75/223) | 0.86 | 0.58 |
| Lives in a house made of wood/leaves (yes) | 44.6 (41/92) | 48.9 (109/223) | 0.84 | 0.49 |
| Alcohol or tobacco consumption (yes) | 55.4 (51/92) | 51.6 (115/223) | 1.17 | 0.53 |
| Comorbidity, % (n/N) | ||||
| Diabetes or high blood pressure (yes) | 6.5 (6/92) | 7.6 (17/223) | 0.85 | 0.73 |
| Other cardiovascular disease (yes) | 1.0 (1/92) | 3.6 (8/223) | 0.30 | 0.23 |
| Digestive disease (yes) | 8.7 (8/92) | 5.4 (12/223) | 1.68 | 0.27 |
| Urinary disease (yes) | 3.3 (3/92) | 0.9 (2/223) | 3.73 | 0.13 |
| Dermatological disease (yes) | 1.0 (1/92) | 0.4 (1/223) | 2.44 | 0.52 |
| Other (yes) | 0.0 (0/92) | 0.9 (2/223) | 1.42 | 0.36 |
| Previous infections, % (n/N) | ||||
| Tuberculosis (yes) | 20.7 (19/92) | 22.0 (49/223) | 0.92 | 0.80 |
| Intestinal parasitosis (yes) | 18.5 (17/92) | 9.0 (20/223) | 2.30 | 0.017 |
| Gonorrhea (yes) | 19.6 (18/92) | 10.3 (23/223) | 2.12 | 0.026 |
| Syphilis (yes) | 18.5 (17/92) | 13.5 (30/223) | 1.46 | 0.26 |
| Chronic hepatitis (yes) | 8.7 (8/92) | 5.8 (13/223) | 1.54 | 0.35 |
| Cerebral toxoplasmosis (yes) | 0.0 (0/92) | 4.9 (11/223) | 1.43 | 0.038 |
| Symptoms, % (n/N) | ||||
| Cough, cold symptoms (yes) | 14.1 (13/92) | 8.1 (18/223) | 1.87 | 0.10 |
| Fever (yes) | 1.1 (1/92) | 2.2 (5/223) | 0.48 | 0.68 |
| Diarrhea (yes) | 26.1 (24/92) | 19.7 (44/223) | 1.44 | 0.21 |
| Frequency of diarrhea, % (n/N) | ||||
| No diarrhea | 73.9 (68/92) | 80.3 (179/223) | N/A | 0.014 |
| Once a month | 16.3 (15/92) | 16.6 (37/223) | ||
| Once a week | 2.2 (2/92) | 2.2 (5/223) | ||
| Once a day | 7.6 (7/92) | 0.9 (2/223) | ||
| Risk group, % (n/N) | ||||
| Heterosexual | 70.9 (61/86) | 79.0 (166/210) | N/A | 0.046 |
| Homosexual | 27.9 (24/86) | 15.7 (33/210) | ||
| Transexual/Bisexual | 1.2 (1/86) | 5.2 (11/210) | ||
| 6.5 (6/92) | 5.8 (13/223) | ||
| HIV acquisition, % (n/N) | ||||
| Sexual | 92.4 (85/92) | 88.8 (198/223) | N/A | 0.64 |
| Vertical | 0.0 (0/92) | 0.9 (2/223) | ||
| Parenteral | 0.0 (0/92) | 0.4 (1/223) | ||
| Unknown | 7.6 (7/92) | 9.9 (22/223) | ||
| CD4+ nadir, median (IQR), /μL | 234 (131, 369) | 261 (117, 378) | N/A | 0.84 |
| 46.7 (43/92) | (92/223) | ||
| Current CD4+, median (IQR), /μL | 427 (265, 574) | 431 (293, 592) | N/A | 0.61 |
| 30.4 (28/92) | 31.4 (70/223) | ||
| Current CD4+ < 200/mL, % (n/N), /mL | 18.8 (12/64) | 9.8 (15/153) | 2.12 | 0.069 |
| 30.4 (28/92) | 31.4 (70/223) | ||
| Uncontrolled HIV viral load, (>20 copies/mL), % (n/N) | 29.4 (25/85) | 18.4 (40/217) | 1.84 | 0.037 |
| 7.6 (7/92) | 2.7 (6/223) | ||
| Poor ART adherence ≤ 95%, % (n/N) | 14.8 (12/81) | 14.2 (26/183) | 1.05 | 0.90 |
| 12.0 (11/92) | 17.9 (40/223) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Otero-Rodriguez, S.; Pinedo-Cancino, V.; Casapia-Morales, M.; Villacorta-Pezo, V.-Y.; Mego-Campos, S.; Parráguez-de-la-Cruz, J.; Merino, E.; Clark, E.H.; Ramos-Rincón, J.-M. Prevalence of Intestinal Protozoa Among Patients Living with HIV in the Peruvian Amazon. Trop. Med. Infect. Dis. 2025, 10, 324. https://doi.org/10.3390/tropicalmed10110324
Otero-Rodriguez S, Pinedo-Cancino V, Casapia-Morales M, Villacorta-Pezo V-Y, Mego-Campos S, Parráguez-de-la-Cruz J, Merino E, Clark EH, Ramos-Rincón J-M. Prevalence of Intestinal Protozoa Among Patients Living with HIV in the Peruvian Amazon. Tropical Medicine and Infectious Disease. 2025; 10(11):324. https://doi.org/10.3390/tropicalmed10110324
Chicago/Turabian StyleOtero-Rodriguez, Silvia, Viviana Pinedo-Cancino, Martin Casapia-Morales, Victoria-Ysabel Villacorta-Pezo, Seyer Mego-Campos, Jorge Parráguez-de-la-Cruz, Esperanza Merino, Eva H. Clark, and José-Manuel Ramos-Rincón. 2025. "Prevalence of Intestinal Protozoa Among Patients Living with HIV in the Peruvian Amazon" Tropical Medicine and Infectious Disease 10, no. 11: 324. https://doi.org/10.3390/tropicalmed10110324
APA StyleOtero-Rodriguez, S., Pinedo-Cancino, V., Casapia-Morales, M., Villacorta-Pezo, V.-Y., Mego-Campos, S., Parráguez-de-la-Cruz, J., Merino, E., Clark, E. H., & Ramos-Rincón, J.-M. (2025). Prevalence of Intestinal Protozoa Among Patients Living with HIV in the Peruvian Amazon. Tropical Medicine and Infectious Disease, 10(11), 324. https://doi.org/10.3390/tropicalmed10110324








