User Experience in Immersive Virtual Reality-Induced Hypoalgesia in Adults and Children Suffering from Pain Conditions
Abstract
1. Introduction
Immersive Virtual Reality in the Approach to Pain
2. Materials and Methods
3. Results
3.1. Distraction
3.2. Presence
3.3. Interactivity
3.4. Gamification
3.5. Virtual Embodiment
- (i)
- Co-localization: being co-located in the same place, time, and space of the real body.
- (ii)
- Agency: having perceived control of the intentions, movements, and actions of the virtual body.
- (ii)
- Ownership: having the feeling or perception of owning a certain part of the virtual body.
- (iv)
- Perspective: observing the virtual body from an egocentric or allocentric point of view.
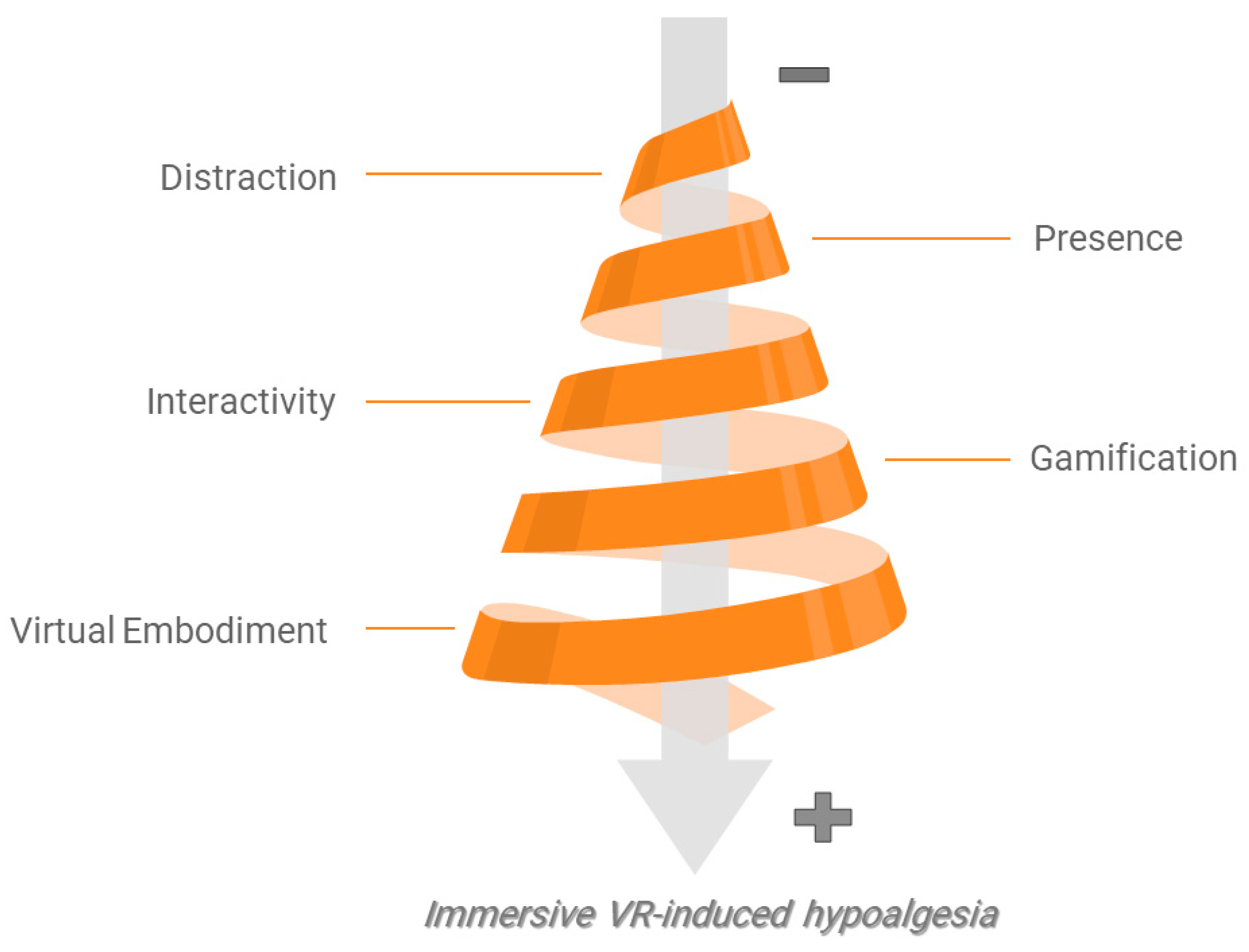
3.6. Hierarchical Relationship of Hypoalgesic Effects and Factors Related to User Experience in Immersive Virtual Reality
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Raja, S.N.; Carr, D.B.; Cohen, M.; Finnerup, N.B.; Flor, H.; Gibson, S.; Keefe, F.J.; Mogil, J.S.; Ringkamp, M.; Sluka, K.A.; et al. The revised International Association for the Study of Pain definition of pain: Concepts, challenges, and compromises. Pain 2020, 161, 1976–1982. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.C.d.C.; Craig, K.D. Updating the definition of pain. Pain 2016, 157, 2420–2423. [Google Scholar] [CrossRef] [PubMed]
- Chapman, C.R.; Tuckett, R.P.; Song, C.W. Pain and stress in a systems perspective: Reciprocal neural, endocrine, and immune interactions. J. Pain 2008, 9, 122–145. [Google Scholar] [CrossRef] [PubMed]
- Foley, H.E.; Knight, J.C.; Ploughman, M.; Asghari, S.; Audas, R. Association of chronic pain with comorbidities and health care utilization: A retrospective cohort study using health administrative data. Pain 2021, 162, 2737–2749. [Google Scholar] [CrossRef] [PubMed]
- Blyth, F.M.; Briggs, A.M.; Schneider, C.H.; Hoy, D.G.; March, L.M. The global burden of musculoskeletal pain—Where to from here? Am. J. Public Health 2019, 109, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.P.; Vase, L.; Hooten, W.M. Chronic pain: An update on burden, best practices, and new advances. Lancet 2021, 397, 2082–2097. [Google Scholar] [CrossRef] [PubMed]
- Gustavsson, A.; Bjorkman, J.; Ljungcrantz, C.; Rhodin, A.; Rivano-Fischer, M.; Sjolund, K.F.; Mannheimer, C. Socio-economic burden of patients with a diagnosis related to chronic pain–Register data of 840,000 S wedish patients. Eur. J. Pain 2012, 16, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Gaskin, D.J.; Richard, P. The economic costs of pain in the United States. J. Pain 2012, 13, 715–724. [Google Scholar] [CrossRef] [PubMed]
- Harvie, D.S.; Smith, R.T.; Martin, D.; Hirsh, A.T.; Trost, Z. Novel applications of virtual and mixed reality in pain research and treatment. Front. Virtual Real. 2022, 3, 1018804. [Google Scholar] [CrossRef]
- Volkow, N.D.; Blanco, C. The changing opioid crisis: Development, challenges and opportunities. Mol. Psychiatry 2021, 26, 218–233. [Google Scholar] [CrossRef]
- Trost, Z.; France, C.; Anam, M.; Shum, C. Virtual reality approaches to pain: Toward a state of the science. Pain 2021, 162, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Skarbez, R.; Smith, M.; Whitton, M.C. Revisiting Milgram and Kishino’s reality-virtuality continuum. Front. Virtual Real. 2021, 2, 647997. [Google Scholar] [CrossRef]
- Zhao, J.; Riecke, B.E.; Kelly, J.W.; Stefanucci, J.; Klippel, A. Human spatial perception, cognition, and behaviour in extended reality. Front. Virtual Real. 2023, 4, 1257230. [Google Scholar] [CrossRef]
- Kardong-Edgren, S.S.; Farra, S.L.; Alinier, G.; Young, H.M. A call to unify definitions of virtual reality. Clin. Simul. Nurs. 2019, 31, 28–34. [Google Scholar] [CrossRef]
- Nilsson, N.C.; Nordahl, R.; Serafin, S. Immersion revisited: A review of existing definitions of immersion and their relation to different theories of presence. Hum. Technol. 2016, 12, 108–134. [Google Scholar] [CrossRef]
- Brady, N.; McVeigh, J.G.; McCreesh, K.; Rio, E.; Dekkers, T.; Lewis, J.S. Exploring the effectiveness of immersive Virtual Reality interventions in the management of musculoskeletal pain: A state-of-the-art review. Phys. Ther. Rev. 2021, 26, 262–275. [Google Scholar] [CrossRef]
- Mallari, B.; Spaeth, E.K.; Goh, H.; Boyd, B.S. Virtual reality as an analgesic for acute and chronic pain in adults: A systematic review and meta-analysis. J. Pain Res. 2019, 12, 2053–2085. [Google Scholar] [CrossRef] [PubMed]
- Tas, F.Q.; van Eijk, C.A.M.; Staals, L.M.; Legerstee, J.S.; Dierckx, B. Virtual reality in pediatrics, effects on pain and anxiety: A systematic review and meta-analysis update. Pediatric Anesthesia 2022, 32, 1292–1304. [Google Scholar] [CrossRef] [PubMed]
- Eijlers, R.; Utens, E.M.W.J.; Staals, L.M.; de Nijs, P.F.A.; Berghmans, J.M.; Wijnen, R.M.H.; Hillegers, M.H.J.; Dierckx, B.; Legerstee, J.S. Systematic review and meta-analysis of virtual reality in pediatrics: Effects on pain and anxiety. Anesthesia Analg. 2019, 129, 1344–1353. [Google Scholar] [CrossRef]
- Hadjiat, Y.; Marchand, S. Virtual reality and the mediation of acute and chronic pain in adult and pediatric populations: Research developments. Front. Pain Res. 2022, 3, 840921. [Google Scholar] [CrossRef]
- Viderman, D.; Tapinova, K.; Dossov, M.; Seitenov, S.; Abdildin, Y.G. Virtual reality for pain management: An umbrella review. Front. Med. 2023, 10, 1203670. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Li, X.; Zhou, X.; Zhan, L.; Wu, F.; Huang, Z.; Sun, Y.; Feng, Y.; Du, Q. Virtual Reality Therapy for the Management of Chronic Spinal Pain: Systematic Review and Meta-Analysis. JMIR Serious Games 2024, 12, e50089. [Google Scholar] [CrossRef] [PubMed]
- Baker, N.A.; Polhemus, A.H.; Ospina, E.H.; Feller, H.; Zenni, M.; Deacon, M.; DeGrado, G.; Basnet, S.; Driscoll, M. The state of science in the use of virtual reality in the treatment of acute and chronic pain: A systematic scoping review. Clin. J. Pain 2022, 38, 424–441. [Google Scholar] [CrossRef] [PubMed]
- Garrett, B.; Taverner, T.; Gromala, D.; Tao, G.; Cordingley, E.; Sun, C. Virtual reality clinical research: Promises and challenges. JMIR Serious Games 2018, 6, e10839. [Google Scholar] [CrossRef]
- Glegg, S.M.N.; Levac, D.E. Barriers, facilitators and interventions to support virtual reality implementation in rehabilitation: A scoping review. PM&R 2018, 10, 1237–1251. [Google Scholar]
- Brepohl, P.C.A.; Leite, H. Virtual reality applied to physiotherapy: A review of current knowledge. Virtual Real. 2023, 27, 71–95. [Google Scholar] [CrossRef]
- Donegan, T.; Ryan, B.E.; Swidrak, J.; Sanchez-Vives, M.V. Immersive virtual reality for clinical pain: Considerations for effective therapy. Front. Virtual Real. 2020, 1, 9. [Google Scholar] [CrossRef]
- Lier, E.J.; De Vries, M.; Steggink, E.M.; Broek, R.P.G.T.; Van Goor, H. Effect modifiers of virtual reality in pain management: A systematic review and meta-regression analysis. Pain 2023, 164, 1658–1665. [Google Scholar] [CrossRef] [PubMed]
- Mahrer, N.E.; Gold, J.I. The use of virtual reality for pain control: A review. Curr. Pain Headache Rep. 2009, 13, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Gold, J.I.; Belmont, K.A.; Thomas, D.A. The neurobiology of virtual reality pain attenuation. CyberPsychology Behav. 2007, 10, 536–544. [Google Scholar] [CrossRef]
- Guerra-Armas, J.; Flores-Cortes, M.; Pineda-Galan, C.; Luque-Suarez, A.; La Touche, R. Role of Immersive Virtual Reality in Motor Behaviour Decision-Making in Chronic Pain Patients. Brain Sci. 2023, 13, 617. [Google Scholar] [CrossRef]
- Lindsay, N.M.; Chen, C.; Gilam, G.; Mackey, S.; Scherrer, G. Brain circuits for pain and its treatment. Sci. Transl. Med. 2021, 13, eabj7360. [Google Scholar] [CrossRef] [PubMed]
- De Ridder, D.; Adhia, D.; Vanneste, S. The anatomy of pain and suffering in the brain and its clinical implications. Neurosci. Biobehav. Rev. 2021, 130, 125–146. [Google Scholar] [CrossRef] [PubMed]
- Moreau, S.; Thérond, A.; Cerda, I.H.; Studer, K.; Pan, A.; Tharpe, J.; Crowther, J.E.; Abd-Elsayed, A.; Gilligan, C.; Tolba, R.; et al. Virtual reality in acute and chronic pain medicine: An updated review. Curr. Pain Headache Rep. 2024, 1–36. [Google Scholar] [CrossRef] [PubMed]
- Stamm, O.; Dahms, R.; Müller-Werdan, U. Virtual reality in pain therapy: A requirements analysis for older adults with chronic back pain. J. Neuroeng. Rehabil. 2020, 17, 129. [Google Scholar] [CrossRef] [PubMed]
- Matamala-Gomez, M.; Donegan, T.; Bottiroli, S.; Sandrini, G.; Sanchez-Vives, M.V.; Tassorelli, C. Immersive virtual reality and virtual embodiment for pain relief. Front. Hum. Neurosci. 2019, 13, 279. [Google Scholar] [CrossRef] [PubMed]
- Indovina, P.; Barone, D.; Gallo, L.; Chirico, A.; De Pietro, G.; Giordano, A. Virtual reality as a distraction intervention to relieve pain and distress during medical procedures: A comprehensive literature review. Clin. J. Pain 2018, 34, 858–877. [Google Scholar] [CrossRef] [PubMed]
- Slater, M.; Lotto, B.; Arnold, M.M.; Sanchez-Vives, M.V. How we experience immersive virtual environments: The concept of presence and its measurement. Anu. Psicol. 2009, 40, 193–210. [Google Scholar]
- Burdea, G.C.; Coiffet, P. Virtual Reality Technology; John Wiley & Sons: Hoboken, NJ, USA, 2003. [Google Scholar]
- King, D.; Greaves, F.; Exeter, C.; Darzi, A. ‘Gamification’: Influencing health behaviours with games. J. R. Soc. Med. 2013, 106, 76–78. [Google Scholar] [CrossRef] [PubMed]
- Dreesmann, N.J.; Su, H.; Thompson, H.J. A systematic review of virtual reality therapeutics for acute pain management. Pain Manag. Nurs. 2022, 23, 672–681. [Google Scholar] [CrossRef] [PubMed]
- Goudman, L.; Jansen, J.; Billot, M.; Vets, N.; De Smedt, A.; Roulaud, M.; Rigoard, P.; Moens, M. Virtual reality applications in chronic pain management: Systematic review and meta-analysis. JMIR Serious Games 2022, 10, e34402. [Google Scholar] [CrossRef]
- Hoffman, H.G. Interacting with virtual objects via embodied avatar hands reduces pain intensity and diverts attention. Sci. Rep. 2021, 11, 10672. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez-Maldonado, J.; Gutierrez-Martinez, O.; Cabas-Hoyos, K. Interactive and passive virtual reality distraction: Effects on presence and pain intensity. Annu. Rev. Cybertherapy Telemed. 2011, 2011, 69–73. [Google Scholar]
- Tesarz, J.; Herpel, C.; Meischner, M.; Drusko, A.; Friederich, H.-C.; Flor, H.; Reichert, J. Effects of virtual reality on psychophysical measures of pain: Superiority to imagination and nonimmersive conditions. Pain 2024, 165, 796–810. [Google Scholar] [CrossRef] [PubMed]
- Colloca, L.; Raghuraman, N.; Wang, Y.; Akintola, T.; Brawn-Cinani, B.; Colloca, G.; Kier, C.; Varshney, A.; Murthi, S. Virtual reality: Physiological and behavioral mechanisms to increase individual pain tolerance limits. Pain 2020, 161, 2010–2021. [Google Scholar] [CrossRef] [PubMed]
- Won, A.S.; Bailey, J.; Bailenson, J.; Tataru, C.; Yoon, I.A.; Golianu, B. Immersive virtual reality for pediatric pain. Children 2017, 4, 52. [Google Scholar] [CrossRef] [PubMed]
- Araujo-Duran, J.; Kopac, O.; Campana, M.M.; Bakal, O.; Sessler, D.I.; Hofstra, R.L.; Shah, K.; Turan, A.; Ayad, S. Virtual Reality Distraction for Reducing Acute Postoperative Pain After Hip Arthroplasty: A Randomized Trial. Anesth. Analg. 2024, 138, 751–759. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, E.B.; Ahmad, M. Virtual reality as a distraction technique for pain and anxiety among patients with breast cancer: A randomized control trial. Palliat. Support. Care 2019, 17, 29–34. [Google Scholar] [CrossRef] [PubMed]
- McSherry, T.; Atterbury, M.; Gartner, S.; Helmold, E.; Searles, D.M.; Schulman, C. Randomized, crossover study of immersive virtual reality to decrease opioid use during painful wound care procedures in adults. J. Burn. Care Res. 2018, 39, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Patterson, D.R.; Drever, S.; Soltani, M.; Sharar, S.R.; Wiechman, S.; Meyer, W.J.; Hoffman, H.G. A comparison of interactive immersive virtual reality and still nature pictures as distraction-based analgesia in burn wound care. Burns 2023, 49, 182–192. [Google Scholar] [CrossRef]
- Wender, R.; Hoffman, H.G.; Hunner, H.H.; Seibel, E.J.; Patterson, D.R.; Sharar, S.R. Interactivity influences the magnitude of virtual reality analgesia. J. Cyber Ther. Rehabil. 2009, 2, 27. [Google Scholar]
- Lier, E.J.; Oosterman, J.M.; Assmann, R.; de Vries, M.; Van Goor, H. The effect of Virtual Reality on evoked potentials following painful electrical stimuli and subjective pain. Sci. Rep. 2020, 10, 9067. [Google Scholar] [CrossRef] [PubMed]
- MacIntyre, E.; Sigerseth, M.; Larsen, T.F.; Fersum, K.V.; Meulders, M.; Meulders, A.; Michiels, B.; Braithwaite, F.A.; Stanton, T.R. Get your head in the game: A replicated single-case experimental design evaluating the effect of a novel virtual reality intervention in people with chronic low back pain. J. Pain 2023, 24, 1449–1464. [Google Scholar] [CrossRef] [PubMed]
- Özlü, A.; Ünver, G.; Tuna, H.İ.; Menekşeoğlu, A.K. The effect of a virtual reality-mediated gamified rehabilitation program on pain, disability, function, and balance in knee osteoarthritis: A prospective randomized controlled study. Games Health J. 2023, 12, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, H.G.; Fontenot, M.R.; Garcia-Palacios, A.; Greenleaf, W.J.; Alhalabi, W.; Curatolo, M.; Flor, H. Adding tactile feedback increases avatar ownership and makes virtual reality more effective at reducing pain in a randomized crossover study. Sci. Rep. 2023, 13, 7915. [Google Scholar] [CrossRef] [PubMed]
- Eccleston, C.; Fisher, E.; Liikkanen, S.; Sarapohja, T.; Stenfors, C.; Jääskeläinen, S.K.; Rice, A.S.; Mattila, L.; Blom, T.; Bratty, J.R. A prospective, double-blind, pilot, randomized, controlled trial of an ‘embodied’ virtual reality intervention for adults with low back pain. Pain 2022, 163, 1700–1715. [Google Scholar] [CrossRef] [PubMed]
- Matamala-Gomez, M.; Nierula, B.; Donegan, T.; Slater, M.; Sanchez-Vives, M.V. Manipulating the perceived shape and color of a virtual limb can modulate pain responses. J. Clin. Med. 2020, 9, 291. [Google Scholar] [CrossRef] [PubMed]
- Matamala-Gomez, M.; Gonzalez, A.M.D.; Slater, M.; Sanchez-Vives, M.V. Decreasing pain ratings in chronic arm pain through changing a virtual body: Different strategies for different pain types. J. Pain 2019, 20, 685–697. [Google Scholar] [CrossRef] [PubMed]
- Harvie, D.S.; Kelly, J.; Kluver, J.; Deen, M.; Spitzer, E.; Coppieters, M.W. A randomized controlled pilot study examining immediate effects of embodying a virtual reality superhero in people with chronic low back pain. Disabil. Rehabil. Assist. Technol. 2024, 19, 851–858. [Google Scholar] [CrossRef] [PubMed]
- de la Campa Crespo, M.Á.; Donegan, T.; Amestoy-Alonso, B.; Just, A.; Combalía, A.; Sanchez-Vives, M.V. Virtual embodiment for improving range of motion in patients with movement-related shoulder pain: An experimental study. J. Orthop. Surg. Res. 2023, 18, 729. [Google Scholar] [CrossRef]
- Hua, Y.; Qiu, R.; Yao, W.; Zhang, Q.; Chen, X. The effect of virtual reality distraction on pain relief during dressing changes in children with chronic wounds on lower limbs. Pain Manag. Nurs. 2015, 16, 685–691. [Google Scholar] [CrossRef]
- Ryu, J.H.; Park, J.W.; Nahm, F.S.; Jeon, Y.T.; Oh, A.Y.; Lee, H.J.; Kim, J.H.; Han, S.H. The effect of gamification through a virtual reality on preoperative anxiety in pediatric pa-tients undergoing general anesthesia: A prospective, randomized, and controlled trial. J. Clin. Med. 2018, 7, 284. [Google Scholar] [CrossRef]
- Dumoulin, S.; Bouchard, S.; Ellis, J.; Lavoie, K.L.; Vézina, M.-P.; Charbonneau, P.; Tardif, J.; Hajjar, A. A randomized controlled trial on the use of virtual reality for needle-related procedures in children and adolescents in the emergency department. Games Health J. 2019, 8, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Griffin, A.; Wilson, L.; Feinstein, A.B.; Bortz, A.; Heirich, M.S.; Gilkerson, R.; Wagner, J.F.; Menendez, M.; Caruso, T.J.; Rodriguez, S.; et al. Virtual reality in pain rehabilitation for youth with chronic pain: Pilot feasibility study. JMIR Rehabil. Assist. Technol. 2020, 7, e22620. [Google Scholar] [CrossRef]
- Bascour-Sandoval, C.; Salgado-Salgado, S.; Gómez-Milán, E.; Fernández-Gómez, J.; Michael, G.A.; Gálvez-García, G. Pain and distraction according to sensory modalities: Current findings and future directions. Pain Pract. 2019, 19, 686–702. [Google Scholar] [CrossRef]
- Johnson, M.H. How does distraction work in the management of pain? Curr. Pain Headache Rep. 2005, 9, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Xu, Y.; Liu, N.; Fan, L. Effectiveness of virtual reality intervention on reducing the pain, anxiety and fear of needle-related procedures in paediatric patients: A systematic review and meta-analysis. J. Adv. Nurs. 2023, 79, 15–30. [Google Scholar] [CrossRef]
- Simonetti, V.; Tomietto, M.; Comparcini, D.; Vankova, N.; Marcelli, S.; Cicolini, G. Effectiveness of virtual reality in the management of paediatric anxiety during the peri-operative period: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2022, 125, 104115. [Google Scholar] [CrossRef] [PubMed]
- Lluesma-Vidal, M.; González, R.C.; García-Garcés, L.; Sánchez-López, M.I.; Peyro, L.; Ruiz-Zaldibar, C. Effect of virtual reality on pediatric pain and fear during procedures involving needles: Systematic review and meta-analysis. JMIR Serious Games 2022, 10, e35008. [Google Scholar] [CrossRef]
- Addab, S.; Hamdy, R.; Thorstad, K.; Le May, S.; Tsimicalis, A. Use of virtual reality in managing paediatric procedural pain and anxiety: An integrative literature review. J. Clin. Nurs. 2022, 31, 3032–3059. [Google Scholar] [CrossRef]
- Do, A.L.; Enax-Krumova, E.K.; Özgül, Ö.; Eitner, L.B.; Heba, S.; Tegenthoff, M.; Maier, C.; Höffken, O. Distraction by a cognitive task has a higher impact on electrophysiological measures compared with conditioned pain modulation. BMC Neurosci. 2020, 21, 53. [Google Scholar] [CrossRef]
- Smith, K.L.; Wang, Y.; Colloca, L. Impact of virtual reality technology on pain and anxiety in pediatric burn patients: A systematic review and meta-analysis. Front. Virtual Real. 2022, 2, 751735. [Google Scholar] [CrossRef] [PubMed]
- López-Valverde, N.; Muriel Fernandez, J.; López-Valverde, A.; Valero Juan, L.F.; Ramírez, J.M.; Flores Fraile, J.; Herrero Payo, J.; Blanco Antona, L.A.; Macedo de Sousa, B.; Bravo, M. Use of virtual reality for the management of anxiety and pain in dental treatments: Systematic review and meta-analysis. J. Clin. Med. 2020, 9, 1025. [Google Scholar] [CrossRef]
- Slater, M.; Wilbur, S. A framework for immersive virtual environments (FIVE): Speculations on the role of presence in virtual environments. Presence Teleoperators Virtual Environ. 1997, 6, 603–616. [Google Scholar] [CrossRef]
- Tseng, P.; Juan, C.-H. Virtual reality in the neuroscience of multisensory integration and consciousness of bodily self. J. Neurosci. Neuroeng. 2013, 2, 387–392. [Google Scholar] [CrossRef]
- Bohil, C.J.; Alicea, B.; Biocca, F.A. Virtual reality in neuroscience research and therapy. Nat. Rev. Neurosci. 2011, 12, 752–762. [Google Scholar] [CrossRef]
- Brown, P.; Powell, W.; Dansey, N.; Al-Abbadey, M.; Stevens, B.; Powell, V. Virtual reality as a pain distraction modality for experimentally induced pain in a chronic pain population: An exploratory study. Cyberpsychol. Behav. Soc. Netw. 2022, 25, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, H.G.; Sharar, S.R.; Coda, B.; Everett, J.J.; Ciol, M.; Richards, T.; Patterson, D.R. Manipulating presence influences the magnitude of virtual reality analgesia. Pain 2004, 111, 162–168. [Google Scholar] [CrossRef]
- Flores-Cortes, M.; Guerra-Armas, J.; Pineda-Galan, C.; La Touche, R.; Luque-Suarez, A. Sensorimotor Uncertainty of Immersive Virtual Reality Environments for People in Pain: Scoping Review. Brain Sci. 2023, 13, 1461. [Google Scholar] [CrossRef]
- McAnally, K.; Wallis, G. Visual–haptic integration, action and embodiment in virtual reality. Psychol. Res. 2022, 86, 1847–1857. [Google Scholar] [CrossRef]
- Choudhury, S.; Charman, T.; Bird, V.; Blakemore, S.-J. Adolescent development of motor imagery in a visually guided pointing task. Conscious. Cogn. 2007, 16, 886–896. [Google Scholar] [CrossRef]
- Gupta, A.; Scott, K.; Dukewich, M. Innovative technology using virtual reality in the treatment of pain: Does it reduce pain via distraction, or is there more to it? Pain Med. 2018, 19, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Wittkopf, P.G.; Lloyd, D.M.; Coe, O.; Yacoobali, S.; Billington, J. The effect of interactive virtual reality on pain perception: A systematic review of clinical studies. Disabil. Rehabil. 2020, 42, 3722–3733. [Google Scholar] [CrossRef] [PubMed]
- Czub, M.; Piskorz, J. Body movement reduces pain intensity in virtual reality-based analgesia. Int. J. Hum. Comput. Interact. 2018, 34, 1045–1051. [Google Scholar] [CrossRef]
- Wiederhold, M.D.; Wiederhold, B.K. Virtual reality and interactive simulation for pain distraction. Pain Med. 2007, 8 (Suppl. S3), S182–S188. [Google Scholar] [CrossRef]
- Lier, E.J.; Harder, J.; Oosterman, J.M.; de Vries, M.; van Goor, H. Modulation of tactile perception by Virtual Reality distraction: The role of individual and VR-related factors. PLoS ONE 2018, 13, e0208405. [Google Scholar] [CrossRef] [PubMed]
- Deng, X.; Jian, C.; Yang, Q.; Jiang, N.; Huang, Z.; Zhao, S. The analgesic effect of different interactive modes of virtual reality: A prospective functional near-infrared spectroscopy (fNIRS) study. Front. Neurosci. 2022, 16, 1033155. [Google Scholar] [CrossRef] [PubMed]
- Juan, M.-C.; Elexpuru, J.; Dias, P.; Santos, B.S.; Amorim, P. Immersive virtual reality for upper limb rehabilitation: Comparing hand and controller interaction. Virtual Real. 2023, 27, 1157–1171. [Google Scholar] [CrossRef] [PubMed]
- Fandim, J.V.; Saragiotto, B.T.; Porfírio, G.J.M.; Santana, R.F. Effectiveness of virtual reality in children and young adults with cerebral palsy: A systematic review of randomized controlled trial. Braz. J. Phys. Ther. 2021, 25, 369–386. [Google Scholar] [CrossRef]
- Evans, C.; Moonesinghe, R. Virtual reality in pediatric anesthesia: A toy or a tool. Pediatr. Anesthesia 2020, 30, 386–387. [Google Scholar] [CrossRef]
- Alfieri, F.M.; da Silva Dias, C.; de Oliveira, N.C.; Battistella, L.R. Gamification in musculoskeletal rehabilitation. Curr. Rev. Musculoskelet. Med. 2022, 15, 629–636. [Google Scholar] [CrossRef]
- Primack, B.A.; Carroll, M.V.; McNamara, M.; Klem, M.L.; King, B.; Rich, M.; Chan, C.W.; Nayak, S. Role of video games in improving health-related outcomes: A systematic review. Am. J. Prev. Med. 2012, 42, 630–638. [Google Scholar] [CrossRef] [PubMed]
- Mouatt, B.; Smith, A.E.; Mellow, M.L.; Parfitt, G.; Smith, R.T.; Stanton, T.R. The use of virtual reality to influence motivation, affect, enjoyment, and engagement during exercise: A scoping review. Front. Virtual Real. 2020, 1, 564664. [Google Scholar] [CrossRef]
- Tao, G.; Garrett, B.; Taverner, T.; Cordingley, E.; Sun, C. Immersive virtual reality health games: A narrative review of game design. J. Neuroeng. Rehabil. 2021, 18, 31. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.S.; Cafazzo, J.A.; Seto, E. A game plan: Gamification design principles in mHealth applications for chronic disease management. Health Inform. J. 2016, 22, 184–193. [Google Scholar] [CrossRef]
- Janssen, J.; Verschuren, O.; Renger, W.J.; Ermers, J.; Ketelaar, M.; Van Ee, R. Gamification in physical therapy: More than using games. Pediatr. Phys. Ther. 2017, 29, 95–99. [Google Scholar] [CrossRef] [PubMed]
- Suleiman-Martos, N.; García-Lara, R.A.; Membrive-Jiménez, M.J.; Pradas-Hernández, L.; Romero-Béjar, J.L.; Dominguez-Vías, G.; Gómez-Urquiza, J.L. Effect of a game-based intervention on preoperative pain and anxiety in children: A systematic review and meta-analysis. J. Clin. Nurs. 2022, 31, 3350–3367. [Google Scholar] [CrossRef] [PubMed]
- Naqvi, W.; Quershi, M.I. Impact of Gamification on Pain, Range of Motion, Muscle Strength, and Functional Independence Post Distal Radius Fracture. Arch. Phys. Med. Rehabil. 2024, 105, e163. [Google Scholar] [CrossRef]
- Gava, V.; Fialho, H.R.F.; Calixtre, L.B.; Barbosa, G.M.; Kamonseki, D.H. Effects of gaming on pain-related fear, pain catastrophizing, anxiety, and depression in patients with chronic musculoskeletal pain: A systematic review and meta-analysis. Games Health J. 2022, 11, 369–384. [Google Scholar] [CrossRef] [PubMed]
- Meulders, A. From fear of movement-related pain and avoidance to chronic pain disability: A state-of-the-art review. Curr. Opin. Behav. Sci. 2019, 26, 130–136. [Google Scholar] [CrossRef]
- Vittersø, A.D.; Halicka, M.; Buckingham, G.; Proulx, M.J.; Bultitude, J.H. The sensorimotor theory of pathological pain revisited. Neurosci. Biobehav. Rev. 2022, 139, 104735. [Google Scholar] [CrossRef]
- Kantak, S.S.; Johnson, T.; Zarzycki, R. Linking pain and motor control: Conceptualization of movement deficits in patients with painful conditions. Phys. Ther. 2022, 102, pzab289. [Google Scholar] [CrossRef] [PubMed]
- Senkowski, D.; Heinz, A. Chronic pain and distorted body image: Implications for multisensory feedback interventions. Neurosci. Biobehav. Rev. 2016, 69, 252–259. [Google Scholar] [CrossRef]
- Lotze, M.; Moseley, G.L. Role of distorted body image in pain. Curr. Rheumatol. Rep. 2007, 9, 488–496. [Google Scholar] [CrossRef]
- Martini, M. Real, rubber or virtual: The vision of ‘one’s own’ body as a means for pain modulation. A narrative review. Conscious. Cogn. 2016, 43, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Boesch, E.; Bellan, V.; Moseley, G.L.; Stanton, T.R. The effect of bodily illusions on clinical pain: A systematic review and meta-analysis. Pain 2016, 157. [Google Scholar] [CrossRef]
- Kokkinara, E.; Slater, M. Measuring the effects through time of the influence of visuomotor and visuotactile synchronous stimulation on a virtual body ownership illusion. Perception 2014, 43, 43–58. [Google Scholar] [CrossRef] [PubMed]
- Buetler, K.A.; Penalver-Andres, J.; Özen, Ö.; Ferriroli, L.; Müri, R.M.; Cazzoli, D.; Marchal-Crespo, L. ‘Tricking the Brain’ Using Immersive Virtual Reality: Modifying the Self-Perception Over Embodied Avatar Influences Motor Cortical Excitability and Action Initiation. Front. Hum. Neurosci. 2022, 15, 787487. [Google Scholar] [CrossRef] [PubMed]
- Hechler, T. Altered interoception and its role for the co-occurrence of chronic primary pain and mental health problems in children. Pain 2021, 162, 665–671. [Google Scholar] [CrossRef]
- Arzy, S.; Thut, G.; Mohr, C.; Michel, C.M.; Blanke, O. Neural Basis of Embodiment: Distinct Contributions of Temporoparietal Junction and Extrastriate Body Area. J. Neurosci. 2006, 26, 8074. [Google Scholar] [CrossRef]
- Matamala-Gomez, M.; Maselli, A.; Malighetti, C.; Realdon, O.; Mantovani, F.; Riva, G. Virtual Body Ownership Illusions for Mental Health: A Narrative Review. J. Clin. Med. 2021, 10, 139. [Google Scholar] [CrossRef]
- Joy, T.; Ugur, E.; Ayhan, I. Trick the body trick the mind: Avatar representation affects the perception of available action possibilities in virtual reality. Virtual Real. 2022, 26, 615–629. [Google Scholar] [CrossRef]
- Tsakiris, M.; Prabhu, G.; Haggard, P. Having a body versus moving your body: How agency structures body-ownership. Conscious. Cogn. 2006, 15, 423–432. [Google Scholar] [CrossRef]
- Gonçalves, G.; Melo, M.; Barbosa, L.; Vasconcelos-Raposo, J.; Bessa, M. Evaluation of the impact of different levels of self-representation and body tracking on the sense of presence and embodiment in immersive VR. Virtual Real. 2022, 26, 1–14. [Google Scholar] [CrossRef]
- Kelly, J.M.; Coppieters, M.W.; Kluver, J.; Deen, M.; Rio, E.; Harvie, D.S. ‘It made you feel like you’ve still got it’: Experiences of people with chronic low back pain undertaking a single session of body image training in virtual reality. Physiother. Theory Pract. 2023, 39, 2651–2661. [Google Scholar] [CrossRef]
- Austin, P.D. The Analgesic Effects of Virtual Reality for People with Chronic Pain: A Scoping Review. Pain Med. 2022, 23, 105–121. [Google Scholar] [CrossRef] [PubMed]
- Moont, R.; Pud, D.; Sprecher, E.; Sharvit, G.; Yarnitsky, D. ‘Pain inhibits pain’ mechanisms: Is pain modulation simply due to distraction? Pain 2010, 150, 113–120. [Google Scholar] [CrossRef]
- Parker, M.; Delahunty, B.; Heberlein, N.; Devenish, N.; Wood, F.M.; Jackson, T.; Carter, T.; Edgar, D.W. Interactive gaming consoles reduced pain during acute minor burn rehabilitation: A randomized, pilot trial. Burns 2016, 42, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Ho, J.T.; Krummenacher, P.; Lesur, M.R.; Saetta, G.; Lenggenhager, B. Real Bodies Not Required? Placebo Analgesia and Pain Perception in Immersive Virtual and Augmented Reality. J. Pain 2022, 23, 625–640. [Google Scholar] [CrossRef] [PubMed]
- McNaughton, D.; Beath, A.; Hush, J.; Jones, M. Perceptual sensory attenuation in chronic pain subjects and healthy controls. Sci. Rep. 2022, 12, 8958. [Google Scholar] [CrossRef]
- Flor, H.; Noguchi, K.; Treede, R.-D.; Turk, D.C. The role of evolving concepts and new technologies and approaches in advancing pain research, management, and education since the establishment of the International Association for the Study of Pain. Pain 2023, 164, S16–S21. [Google Scholar] [CrossRef]
- Simón-Vicente, L.; Rodríguez-Cano, S.; Delgado-Benito, V.; Ausín-Villaverde, V.; Delgado, E.C. Cybersickness. A systematic literature review of adverse effects related to virtual reality. Neurología 2022. [Google Scholar] [CrossRef]
- Caserman, P.; Garcia-Agundez, A.; Zerban, A.G.; Göbel, S. Cybersickness in current-generation virtual reality head-mounted displays: Systematic review and outlook. Virtual Real. 2021, 25, 1153–1170. [Google Scholar] [CrossRef]
- Weech, S.; Kenny, S.; Barnett-Cowan, M. Presence and cybersickness in virtual reality are negatively related: A review. Front. Psychol. 2019, 10, 158. [Google Scholar] [CrossRef] [PubMed]
- Saredakis, D.; Szpak, A.; Birckhead, B.; Keage, H.A.D.; Rizzo, A.; Loetscher, T. Factors associated with virtual reality sickness in head-mounted displays: A systematic review and meta-analysis. Front. Hum. Neurosci. 2020, 14, 96. [Google Scholar] [CrossRef] [PubMed]
- Fan, T.; Wang, X.; Song, X.; Zhao, G.; Zhang, Z. Research status and emerging trends in virtual reality rehabilitation: Bibliometric and knowledge graph study. JMIR Serious Games 2023, 11, e41091. [Google Scholar] [CrossRef]
- Birckhead, B.; Khalil, C.; Liu, X.; Conovitz, S.; Rizzo, A.; Danovitch, I.; Bullock, K.; Spiegel, B. Recommendations for Methodology of Virtual Reality Clinical Trials in Health Care by an International Working Group: Iterative Study. JMIR Ment. Health 2019, 6, e11973. [Google Scholar] [CrossRef] [PubMed]
- Brassel, S.; Power, E.; Campbell, A.; Brunner, M.; Togher, L. Recommendations for the Design and Implementation of Virtual Reality for Acquired Brain Injury Rehabilitation: Systematic Review. J. Med. Internet Res. 2021, 23, e26344. [Google Scholar] [CrossRef] [PubMed]
- Badia, S.B.I.; Fluet, G.G.; Llorens, R.; Deutsch, J.E. Virtual Reality for Sensorimotor Rehabilitation Post Stroke: Design Principles and Evidence. In Neurorehabilitation Technology; Springer International Publishing: New York, NY, USA, 2016; pp. 573–603. [Google Scholar]
- Slatman, S.; Groenveld, T.; Ostelo, R.; van Goor, H.; Staal, J.B.; Knoop, J. Development of a Multimodal, Personalized Intervention of Virtual Reality Integrated within Physiotherapy for Patients with Complex Chronic Low-Back Pain. J. Med. Ext. Real. 2024, 1, 30–43. [Google Scholar] [CrossRef] [PubMed]
- Braithwaite, F.; Arnold, J.; Davis, A.; Gwilt, I.; MacIntyre, E.; Morris, S.; James, K.; Lee, K.; Marshall, H.; Ninnes, P.; et al. Osteoarthritis consumers as co-researchers: Identifying consumer insights to improve osteoarthritis management by co-designing translational research solutions. Osteoarthr. Cartil. 2023, 31, 944–953. [Google Scholar] [CrossRef]
- Maddox, T.; Garcia, H.; Ffrench, K.; Maddox, R.; Garcia, L.; Krishnamurthy, P.; Okhotin, D.; Sparks, C.; Oldstone, L.; Birckhead, B.; et al. In-home virtual reality program for chronic low back pain: Durability of a randomized, placebo-controlled clinical trial to 18 months post-treatment. Reg. Anesthesia Pain Med. 2024, 49, 373–375. [Google Scholar] [CrossRef]
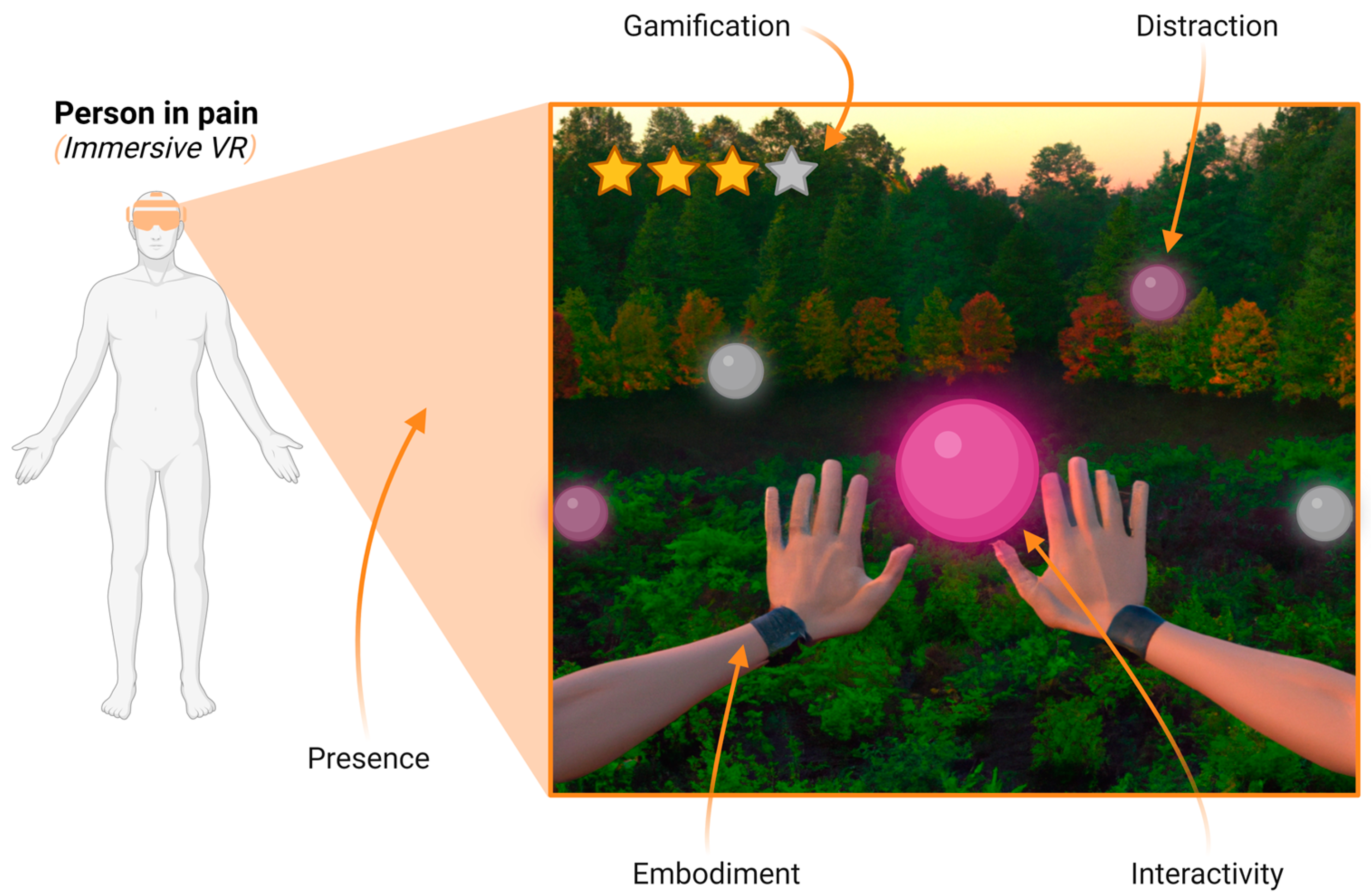
| Feature | Definition |
|---|---|
| Distraction | It refers to the redirection of an individual’s attentional resources away from pain, towards other stimuli (visual, auditory, tactile, and cognitive), resulting from a competition for the limited attentional resources shared between the sensory inputs proposed by VR and the incoming nociceptive signals [37]. |
| Presence | It defines the subjective experience of being in one place or environment, even when physically in another place, allowing the user to easily “forget” that it is a computer-generated simulation [38]. |
| Interactivity | It refers to the level of participation allowed by the user in the virtual reality environment [39]. |
| Gamification | It refers to the application of game elements in non-game contexts [40]. |
| Virtual Embodiment | It refers to the replacement of a person’s real body with a virtual body representation, allowing the subject to feel embodied in a virtual body [36]. |
| Author and Year | Country | Study Details Design Number (n) Target Population | Type of VR User-Related Factor | Main Objective | Main Results |
|---|---|---|---|---|---|
| Araujo-Duran et al. (2024) [48] | United States | Randomized control trial design 106 adults with acute postoperative pain after hip arthroplasty | Immersive VR passive distraction | Examine if virtual reality program decreases acute postoperative pain and opioid requirements in patients recovering from hip arthroplasty | A virtual reality program did not provide significant reductions in average pain (NRS virtual reality group mean = 3.4; NRS reference group mean = 3.5; p = 0.391) scores or opioid consumption compared with 2-dimensional sham video presentations. |
| Mohammad et al. (2019) [49] | Jordan | Randomized control trial design 80 female patients with chronic pain related to breast cancer | Immersive VR passive distraction | Assess the effectiveness of immersive VR distraction in reducing pain and anxiety among female patients with breast cancer | Findings showed that one session of the immersive VR plus morphine made a significant reduction in pain (pre–post intervention means = 7.32–0.33 and p < 0.001, pre–post comparation means = 7.33–4.84 and p < 0.001) and anxiety (pre–post intervention means = 64.98–37.68 and p < 0.001, pre–post comparation means = 63.30–50.13 and p < 0.001) self-reported scores, compared with morphine alone, in breast cancer patients. |
| Tesarz et al. (2023) [45] | Germany | A within-subject randomized control trial design 28 individuals with chronic pain and 31 pain-free controls received painful stimuli | Immersive VR distraction and presence | Investigate the direct effects of an immersive VR environment on the perception of experimental pain in individuals with chronic pain and pain-free controls | VR effectively modulates pain perception in both patients and controls; specifically, the presence in a VR has an increasing effect on pain thresholds (F = 22.946, p < 0.001) and reduces pain inhibition (t = 2.777, p = 0.018) in a conditioned pain modulation paradigm. |
| McSherry et al. (2017) [50] | United States | A within-subject randomized control trial design 18 adults during painful wound care procedures | Immersive VR distraction and interactivity | Evaluate the effect of immersive VR distraction therapy during painful wound care procedures in adults on the amount of opioid medications required to manage pain | Pain and anxiety scores were similar for the wound procedures with and without immersive VR (p > 0.05). Immersive VR significantly reduced the amount of opioid medication administered during painful wound care procedures when IVR was used compared with no IVR (t = −2.7; df = 14; p = 0.02). |
| Patterson et al. (2023) [51] | United States | A within-subject non-randomized trial design 44 adults during painful wound care procedures | Immersive VR distraction, presence, and interactivity | Explore the feasibility of immersive VR during burn debridement, and whether interactive VR would reduce pain more effectively than nature stimuli viewed in the same VR goggles | No significant differences in pain unpleasantness or “presence in VR” between the two conditions were found (p > 0.05). Participants reported significantly less worst pain when distracted with adjunctive computer-generated VR than during standard wound care without distraction (p < 0.05, SD = 17.38). |
| Colloca et al. (2020) [46] | United States | Within-subject non-randomized trial design 59 healthy adults received heat thermal painful stimuli | Immersive VR passive distraction, presence, and interactivity | Explore how immersive VR can increase individual heat-pain tolerance limits | It found a significant main effect of the five conditions (1. immersive VR Ocean, 2. immersive VR Opera, 3. control (non-immersive) Ocean, 4. control (non-immersive) Opera, 5. 2-Back Memory Task) on heat-pain tolerance limit increases (F4,176 = 7.47, Greenhouse–Geisser-corrected p < 0.001). Bonferroni-corrected post hoc comparisons indicated that immersion in the VR Ocean condition led to significantly greater increase in heat-pain tolerance limits (mean increase: 1.025 ± 0.517 °C, baseline temperature: 46.19 ± 2.93 °C; during VR Ocean: 47.09 ± 2.05 °C; scale from 32 to 52 °C) than the VR Opera condition (p = 0.001), control Ocean (p = 0.001), and control Opera (p < 0.001). The VR Ocean condition led to significantly greater increase in the duration (10.04 ± 3.27%) of heat-pain tolerance limits than the VR Opera condition (4.47 ± 2.67%; p = 0.001), control Ocean (3 ± 2.56%; p = 0.001), and control Opera (1.53 ± 1.95%; p < 0.001). The results provided evidence that the immersive VR Ocean intervention induced a larger activation of the parasympathetic nervous system compared to the other four conditions. Immersive VR Ocean condition yielded significantly higher SDNN compared to immersive VR Opera (p = 0.017), non-immersive control Ocean (p = 0.022), non-immersive control Opera (p = 0.023), and 2-Back Memory Task (p = 0.013). The immersive VR Ocean condition was characterized by a higher level of SDNN, which was associated with greater gain in the painful intensities that were tolerated (r = 0.529, p < 0.001). |
| Guiterrez-Maldonado et al. (2011) [44] | Spain | Randomized control trial design 68 healthy adults received cold thermal painful stimuli | Immersive VR passive distraction, presence, and interactivity | Evaluate effects of interactive versus passive VR distraction on the sense of presence and pain intensity | Most of the participants (73.5%) who experienced the interactive VR distraction reported less pain intensity relative to the no-VR trial (χ2 = 7.5, p < 0.01). In the passive VR condition, only 5.9% of participants showed a decreased level of pain intensity and the change did not reach statistical significance (χ2 = 0.47, p = 0.49). Participants reported a greater sense of presence during interactive VR distraction (M = 3.5, SD = 1.0), compared with the passive VR condition (M = 2.7, SD = 1.2, t (66) = 3.0, p < 0.005). The relationship between presence and pain intensity in VR conditions was assessed using Pearson product–moment correlation coefficients. The amount of VR presence reported correlated significantly and negatively with pain intensity (r (68) = −0.29, p < 0.05). |
| Wender et al. (2009) [52] | United States | Randomized control trial design 21 healthy adults received heat thermal painful stimuli | Immersive VR passive distraction, presence, and interactivity | Explores the effect of interactivity on the hypoalgesic effectiveness of virtual reality | Compared to the non-interactive VR group, participants in the interactive VR group showed 75% more reduction in pain unpleasantness (p < 0.005) and 74% more reduction in worst pain (p < 0.005) and in fun (p = 0.10), but not in time spent thinking about pain (p = 0.10). |
| Hoffman (2021) [43] | United States | A within-subject randomized crossover design study 24 adults received heat thermal painful stimuli | Immersive VR passive distraction, presence, interactivity, and virtual embodiment | Evaluate if presence, interactivity, and virtual embodiment would increase VR hypoalgesia | Compared to the passive VR condition, during the interactive avatar VR, participants reported statistically significant reductions in worst pain (χ2 = 31.74, p = 0.000), pain unpleasantness (χ2 = 34.87, p = 0.000), and time thinking about pain (χ2 = 31.17, p = 0.000) and increased fun (χ2 = 30.61, p = 0.000) during the pain stimulus. |
| Lier et al. (2020) [53] | United States | Within-subject randomized crossover design study 30 adults received painful electrical stimuli | Immersive VR passive distraction, presence, and interactivity | Investigated the effect of two VR conditions on reported pain | Active VR significantly decreased pain scores (p = 0.005) (NRS = 3.17 ± 1.54) but passive VR (NRS = 4.93 ± 1.53) and no VR had no analgesic effect (NRS = 5.59 ± 1.35). |
| MacIntyre et al. (2023) [54] | Norway | Multiple-baseline single-case experimental design (SCED) 10 adults with chronic low back pain (CLBP) | Immersive VR presence, gamification, and interactivity | Evaluate the effects of a gamified VR graded activity intervention in people with CLBP | The VR graded activity intervention resulted in a significant reduction in pain intensity (p = 0.016) Average pain (NRS) decreases (1.0 ± 0.27). |
| Ozlu et al. (2024) [55] | Turkey | Randomized crossover design study 73 patients with knee osteoarthritis (OA) | Immersive VR presence, gamification, and interactivity | Assess the disease-specific gamification through immersive VR on pain, disability, functionality, and balance in knee osteoarthritis (OA) | Gamification through immersive VR added to the conservative treatment has a positive effect on pain (p = 0.000), functionality pain (p = 0.000), and balance pain (p = 0.013) Pain (VAS) from 5.57–0.88 to 4.05–0.72. |
| Hofman et al. (2023) [56] | United States | Randomized crossover design study 48 healthy adults received heat thermal painful stimuli | Immersive VR passive distraction, presence, interactivity, and virtual embodiment | Evaluate if adding tactile feedback increases virtual embodiment and hypoalgesic effects | Tactile feedback significantly decreased pain intensity (VR analgesia, p < 0.01), compared to VR with no tactile feedback, and compared to no VR (baseline); r = 0.4, medium effect size. Tactile feedback also significantly increased avatar embodiment. Worst pain (NRS) from 4.71 ± 1.25 to 3.08 ± 1.65. |
| Eccleston et al. (2022) [57] | Finland | Three-arm, prospective, double-blind, pilot, randomized, controlled trial 42 adults with chronic low back pain | Immersive VR passive distraction, presence, interactivity, and virtual embodiment | Compare active VR intervention (Digital Therapeutics for Pain, DTxP) with a sham placebo comparator and a standard care group | Immersive VR was superior to both a sham placebo comparator and standard care control in reducing fear of movement and reinjury (p < 0.04 and p < 0.01) but no differences between groups at any time point for average pain intensity (p > 0.05). Average pain (NRS) from 6.0 (1.4) to 4.1 (1.7) in DTxP intervention group. |
| Matamala-Gomez et al. (2020) [58] | Spain | Within-subject non-randomized trial design 27 healthy adults received painful stimuli | Immersive VR presence and virtual embodiment | Investigate whether distorting an embodied virtual arm in virtual reality modulated pain perception | In the distorted virtual arm conditions, the higher the level of ownership of the distorted (rs = 0.226, p < 0.01) and reddened–distorted (rs = 0.225, p < 0.01) virtual arm, the higher the pain/discomfort perception (VAS). |
| Matamala-Gomez et al. (2019) [59] | Spain | Within-subject non-randomized trial design 19 adults with chronic neuropathic pain | Immersive VR presence and virtual embodiment | Explore whether varying properties of an embodied virtual arm modulated pain ratings in patients with chronic pain due to complex regional pain syndrome (CRPS) type I or peripheral nerve injury (PNI) | Increasing transparency decreased pain in CRPS but did the opposite in PNI, whereas increasing size slightly increased pain ratings only in CRPS. No correlation was statistically significant (p > 0.05). |
| Harvie et al. (2024) [60] | Australia | Non-blinded pilot randomized controlled trial 30 adults with chronic low back pain | Immersive VR presence, interactivity, and virtual embodiment | Evaluate whether embodying superhero-like avatars can change self-perceptions in people with chronic low back pain | In the VR-Play condition, body image scores were improved during (F (3, 83) = 18.83, p < 0.001) but not immediately after or at one-week follow-up. No differences in pain intensity, force production, and fear of movement. |
| Álvarez de la Campa Crespo et al. (2023) [61] | Spain | A single-arm pre–post non-randomized trial design 21 adults with acute and chronic shoulder pain | Immersive VR presence and virtual embodiment | Ascertain whether the experience of movement of an embodied virtual arm, in the absence of actual physical movement, could enhance the range of pain-free motion for patients suffering from shoulder pain related to movement | After completing 15 min VR embodiment intervention, a significant difference in active abduction range of the affected shoulder was found. The mean improvement was 12.3° (95%CI 4.94–19.57; Student’s t-test, p = 0.002, Cohen’s d = 0.76). Also, there was a significant difference in active hand behind-the-back range of motion (95%CI 0.473–0.916; Wilcoxon signed-rank test, p = 0.004; rank biserial correlation, 0.778). Positive correlations between virtual body ownership and levels of improvement in both hand-behind-back movements (Spearman’s ρ = 0.635, p = 0.004) and flexion movements (Spearman’s ρ = 0.646, p = 0.003) were found. |
| Hua et al. (2015) [62] | China | A prospective randomized study. Sixty-five children (4 to 16 years) with chronic pain in lower limbs | Immersive VR distraction, interactivity, and virtual embodiment | To investigate the effect of virtual reality distraction on alleviating pain during dressing changes in children with chronic pain | Virtual reality distraction significantly relieved pain before (p = 0.016), during (p = 0.001), and after (p = 0.034) the dressing change. Anxiety scores during dressing were reduced by 43% as compared to the control group (p < 0.001). VR distraction group had lower pulse rates during dressing change as compared to the control group (106.2 ± 11.45 vs. 98.88 ± 11.57, p < 0.05). Time length of dressing change was significantly reduced in the VR distraction groups as compared to the control group (27.9 ± 6.83 vs. 22.3 ± 7.85 min, p < 0.01). |
| Ryu et al. (2018) [63] | Korea | Prospective randomized control trial. Seventy children scheduled for elective surgery under general anesthesia were randomly divided into either the control or gamification group | Immersive VR presence, gamification, and virtual embodiment | To evaluate whether gamification of the preoperative process—via VR gaming that provides a vivid, immersive, and realistic experience—could reduce preoperative anxiety in children | Preoperative anxiety (mean = 28.3 [23.3–36.7] vs. mean = 46.7 [31.7–51.7]; p < 0.001) and intraoperative compliance (p = 0.038) were lower in the gamification group than in the control group. |
| Dumoulin, et al. (2019) [64] | Canada | Three-arm randomized controlled trial. Fifty-nine children (8–17 years old) from an emergency department were randomized to the three groups | Immersive VR distraction, interactivity, gamification | To document the efficacy of VR as a mode of distraction during a medical procedure (needle-related procedures) compared with two comparison conditions: watching television (TV, minimal control condition) and distraction provided by the Child Life (gold standard control condition) program | A significant reduction in fear of pain and pain intensity was reported in all three conditions (p < 0.05). A larger and statistically significant reduction in fear of pain was observed among children who used VR (p < 0.0001) distraction compared with the CL and TV conditions (p = 0.002). The children’s satisfaction with the VR procedure was significantly higher than for TV and comparable to CL (p < 0.05). |
| Griffin, et al. (2020) [65] | United States | Clinical trial Seventeen children with chronic pain enrolled from a pediatric pain rehabilitation program | Immersive VR interactivity, gamification, presence, body embodiment | Initial implementation of a VR program in pain rehabilitation intervention to enhance function in youth with chronic pain | Overall reports of presence were high (mean of 28.98; max of 40; SD of 4.02), suggestive of a high level of immersion. Among those with multisession data (n = 8), reports of pain (p < 0.001), fear (p = 0.003), avoidance (p = 0.004), and functional limitations (p = 0.01) significantly decreased. Qualitative analysis revealed (1) a positive experience with VR (e.g., enjoyed VR, would like to utilize the VR program again, felt VR was a helpful tool); (2) feeling distracted from pain while engaged in VR; (3) greater perceived mobility; and (4) fewer clinician-observed pain behaviors during VR. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guerra-Armas, J.; Flores-Cortes, M.; Ceniza-Bordallo, G.; Matamala-Gomez, M. User Experience in Immersive Virtual Reality-Induced Hypoalgesia in Adults and Children Suffering from Pain Conditions. Multimodal Technol. Interact. 2024, 8, 66. https://doi.org/10.3390/mti8080066
Guerra-Armas J, Flores-Cortes M, Ceniza-Bordallo G, Matamala-Gomez M. User Experience in Immersive Virtual Reality-Induced Hypoalgesia in Adults and Children Suffering from Pain Conditions. Multimodal Technologies and Interaction. 2024; 8(8):66. https://doi.org/10.3390/mti8080066
Chicago/Turabian StyleGuerra-Armas, Javier, Mar Flores-Cortes, Guillermo Ceniza-Bordallo, and Marta Matamala-Gomez. 2024. "User Experience in Immersive Virtual Reality-Induced Hypoalgesia in Adults and Children Suffering from Pain Conditions" Multimodal Technologies and Interaction 8, no. 8: 66. https://doi.org/10.3390/mti8080066
APA StyleGuerra-Armas, J., Flores-Cortes, M., Ceniza-Bordallo, G., & Matamala-Gomez, M. (2024). User Experience in Immersive Virtual Reality-Induced Hypoalgesia in Adults and Children Suffering from Pain Conditions. Multimodal Technologies and Interaction, 8(8), 66. https://doi.org/10.3390/mti8080066