Connections and Divergence between Public Health and Built Environment—A Scoping Review
Abstract
1. Introduction
2. Methodology
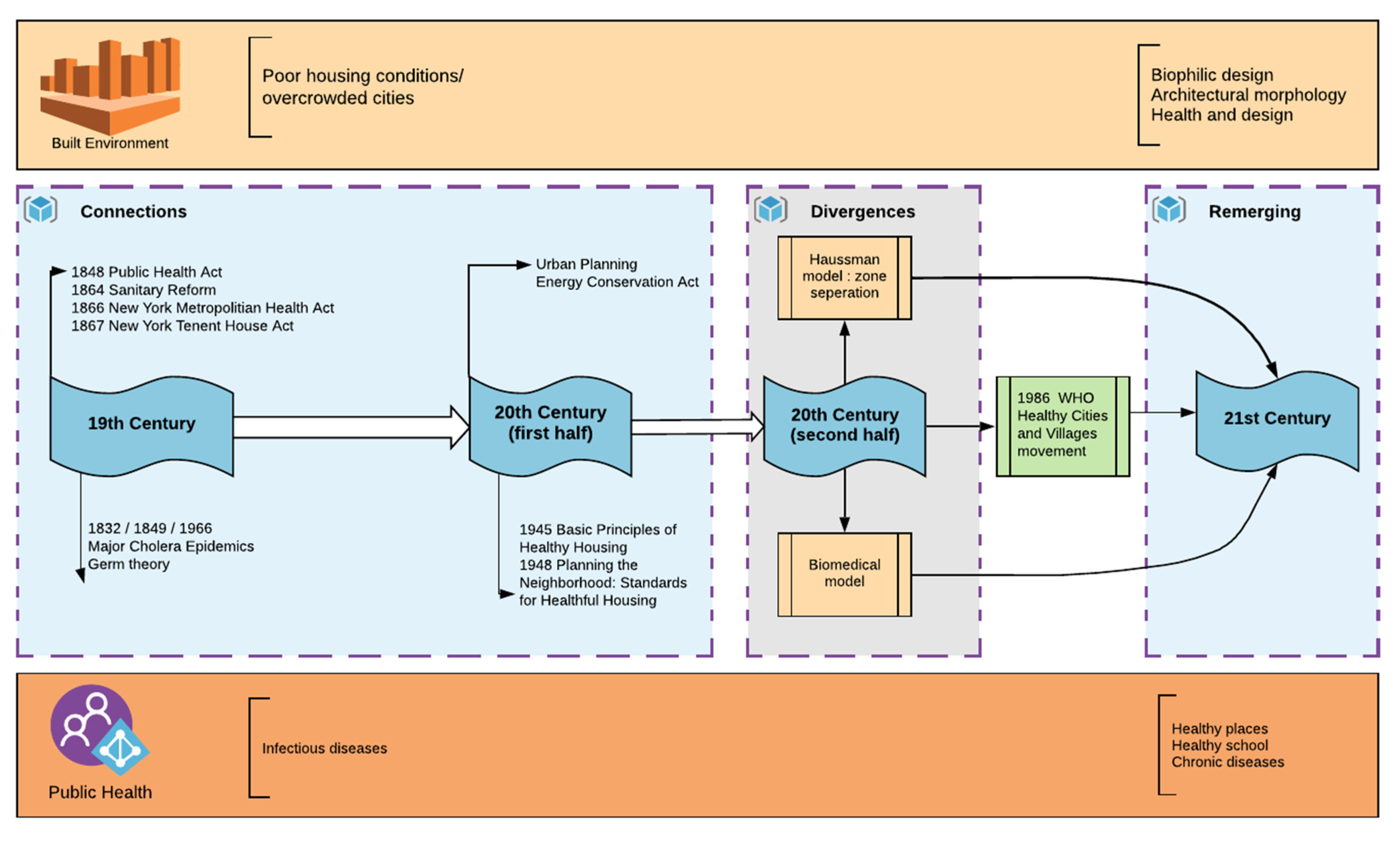
3. Findings
3.1. Connections
3.2. Divergence
3.3. Remerging
3.4. Existing Factors of Health Issues in the Build Environment
3.4.1. Physical Factors
3.4.2. Physiological Factors
3.4.3. Biological Factors
3.4.4. Psychological Factors
4. Future Trends: Reconnecting Public Health and Built Environment Planning and Design
4.1. Multidisciplinary: Human Ecology, Biology, Psychology, and Neurology
4.2. Multilevel: Urban and Building Integration
4.3. Multifactor Assessment
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Frumkin, H. Healthy places: Exploring the evidence. Am. J. Public Health 2003, 93, 1451–1456. [Google Scholar] [CrossRef] [PubMed]
- Pappas, G.; Kiriaze, I.J.; Falagas, M.E. Insights into infectious disease in the era of Hippocrates. Int. J. Infect. Dis. 2008, 12, 347–350. [Google Scholar] [CrossRef] [PubMed]
- Krieger, J.; Higgins, D.L. Housing and health: Time again for public health action. Am. J. Public Health 2002, 92, 758–768. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Elo, S.; Kääriäinen, M.; Kanste, O.; Pölkki, T.; Utriainen, K.; Kyngäs, H. Qualitative content analysis: A focus on trustworthiness. SAGE Open 2014, 4, 2158244014522633. [Google Scholar] [CrossRef]
- United Kingdom Parliament. Sunderland the Public Health Act. Available online: https://www.parliament.uk/about/living-heritage/transformingsociety/towncountry/towns/tyne-and-wear-case-study/about-the-group/public-administration/sunderland-and-the-public-health-act/ (accessed on 17 November 2019).
- Neuendorf, K.A. The Content Analysis Guidebook; Sage: Thousand Oaks, CA, USA, 2016. [Google Scholar]
- Rosenberg, C.E. The Cholera Years: The United States in 1832, 1849, and 1866; University of Chicago Press: Chicago, IL, USA, 2009. [Google Scholar]
- People, H. Healthy People in Healthy Communities: A Systematic Approach to Health Improvement; Report; US Department of Health and Human Services: Washington, DC, USA, 2000.
- Corburn, J. Confronting the challenges in reconnecting urban planning and public health. Am. J. Public Health 2004, 94, 541–546. [Google Scholar] [CrossRef]
- Vandenbroucke, J. Is ‘the causes of cancer’a miasma theory for the end of the twentieth century? Int. J. Epidemiol. 1998, 17, 708–709. [Google Scholar] [CrossRef]
- Li, Y.; Boufford, J.I.; Pagán, J.A. Systems Science Simulation Modeling to Inform Urban Health Policy and Planning. In Smart City Networks; Springer: Berlin/Heidelberg, Germany, 2017; pp. 151–166. [Google Scholar]
- National Healthy Housing Standard. Available online: https://nchh.org/tools-and-data/housing-code-tools/national-healthy-housing-standard/ (accessed on 20 July 2018).
- Standards for Healthful Housing: Planning for the Neighborhood. Available online: https://babel.hathitrust.org/cgi/pt?id=mdp.39015007191813;view=1up;seq=5 (accessed on 20 July 2018).
- Ewing, R.; Clemente, O. Measuring Urban Design: Metrics for Livable Places; Island Press: Washington, DC, USA, 2013. [Google Scholar]
- Duhl, L.J.; Hancock, T. Promoting Health in the Urban Context; WHO Healthy Cities Project Office: Geneva, Switzerland, 1988. [Google Scholar]
- Abrams, R.F.; Malizia, E.; Wendel, A.; Sallis, J.; Millstein, R.A.; Carlson, J.A.; Cannuscio, C.; Glanz, K.; Samet, J.; Sleet, D.A.; et al. Making Healthy Places: Designing and Building for Health, Well-Being, and Sustainability; Island Press: Washington, DC, USA, 2012. [Google Scholar]
- Hamlin, C.; Sidley, P. Revolutions in public health: 1848, and 1998? BMJ 1998, 317, 587–591. [Google Scholar] [CrossRef]
- Hamlin, C. Edwin Chadwick and the engineers, 1842-1854: Systems and antisystems in the pipe-and-brick sewers war. Technol. Cult. 1992, 33, 680–709. [Google Scholar] [CrossRef]
- Finer, S.E. The Life and Times of Sir Edwin Chadwick; Routledge: London, UK, 2016. [Google Scholar]
- Brieger, G.H. Sanitary Reform in New York City: Stephen Smith and the Passage of the Metropolitan Health Bill. Bull. Hist. Med. 1966, 40, 407–429. [Google Scholar]
- Kramer, H.D. The beginnings of the public health movement in the United States. Bull. Hist. Med. 1947, 21, 352–376. [Google Scholar] [PubMed]
- Krueckeberg, D.A. Introduction to Planning History in the United States; Routledge: London, UK, 2018. [Google Scholar]
- Brucemann, R.; Prowler, D. 19th century mechanical system designs. J. Archit. Educ. 1977, 30, 11–15. [Google Scholar] [CrossRef]
- Rosen, G. A History of Public Health; JHU Press: Baltimore, MD, USA, 2015. [Google Scholar]
- Cretti, D.J. Permanently Installed Pest Extermination System; United States Patent and Tradeark Office: Washington, DC, USA, 1988.
- Krieger, N. Theories for social epidemiology in the 21st century: An ecosocial perspective. Int. J. Epidemiol. 2001, 30, 668–677. [Google Scholar] [CrossRef] [PubMed]
- Porter, D. Health, Civilization and the State: A History of Public Health from Ancient to Modern Times; Routledge: London, UK, 2005. [Google Scholar]
- Planning & Zoning for Health in the Built Environment. Available online: https://www.planning.org/pas/infopackets/eip38/ (accessed on 20 July 2018).
- Liebmann, G. It’s Time to Reconsider Oppressive Zoning. USA TODAY N. Y. 1996, 125, 62–64. [Google Scholar]
- Platt, R.H. Land Use and Society, Revised Edition: Geography, law, and Public Policy; Island Press: Washington, DC, USA, 2004. [Google Scholar]
- Hirt, S. The devil is in the definitions: Contrasting American and German approaches to zoning. J. Am. Plan. Assoc. 2007, 73, 436–450. [Google Scholar] [CrossRef]
- Susser, M.; Susser, E. Choosing a future for epidemiology: I. Eras and paradigms. Am. J. Public Health 1996, 86, 668–673. [Google Scholar] [CrossRef]
- Baum, F. Researching public health: Behind the qualitative-quantitative methodological debate. Soc. Sci. Med. 1995, 40, 459–468. [Google Scholar] [CrossRef]
- Thomson, H.; Petticrew, M.; Morrison, D. Health effects of housing improvement: Systematic review of intervention studies. BMJ 2001, 323, 187–190. [Google Scholar] [CrossRef]
- Fishman, R. The American Planning Tradition: Culture and Policy; Woodrow Wilson Center Press: Washington, DC, USA, 2000. [Google Scholar]
- Duhl, L.J.; Sanchez, A.K.; World Health Organization. Healthy Cities and the City Planning Process: A Background Document on Links between Health and Urban Planning; WHO Regional Office for Europe: Copenhagen, Denmark, 1999. [Google Scholar]
- Li, W.; Keegan, T.H.; Sternfeld, B.; Sidney, S.; Quesenberry, C.P., Jr.; Kelsey, J.L. Outdoor falls among middle-aged and older adults: A neglected public health problem. Am. J. Public Health 2006, 96, 1192–1200. [Google Scholar] [CrossRef]
- Oakley, A.; Dawson, M.F.; Holland, J.; Arnold, S.; Cryer, C.; Doyle, Y.; Rice, J.; Hodgson, C.R.; Sowden, A.; Sheldon, T.; et al. Preventing falls and subsequent injury in older people. Qual. Health Care 1996, 5, 243. [Google Scholar] [CrossRef]
- American Academy of Pediatrics. Falls from heights: Windows, roofs, and balconies. Pediatrics 2001, 107, 1188–1191. [Google Scholar] [CrossRef] [PubMed]
- Falls. Available online: https://www.who.int/news-room/fact-sheets/detail/falls (accessed on 20 July 2018).
- Persily, A. Challenges in developing ventilation and indoor air quality standards: The story of ASHRAE Standard 62. Build. Environ. 2015, 91, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Stollard, P.; Stollard, P. Crime Prevention through Housing Design; Taylor & Francis: London, UK, 2003. [Google Scholar]
- Day, C. Places of the Soul: Architecture and Environmental Design as a Healing Art; Routledge: London, UK, 2017. [Google Scholar]
- Collins, K. Low indoor temperatures and morbidity in the elderly. Age Ageing 1986, 15, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Burge, S.; Hedge, A.; Wilson, S.; Bass, J.H.; Robertson, A. Sick building syndrome: A study of 4373 office workers. Ann. Occup. Hyg. 1987, 31, 493–504. [Google Scholar]
- Holmes, S.H.; Phillips, T.; Wilson, A. Overheating and passive habitability: Indoor health and heat indices. Build. Res. Inf. 2016, 44, 1–19. [Google Scholar] [CrossRef]
- Pitarma, R.; Marques, G.; Ferreira, B.R. Monitoring indoor air quality for enhanced occupational health. J. Med. Syst. 2017, 41, 23. [Google Scholar] [CrossRef]
- Figueiro, M.G.; Steverson, B.; Heerwagen, J.H.; Rea, M.S. Daylight in office buildings: Impact of building design on personal light exposures, sleep and mood. In Proceedings of the 28th Session of the CIE, Manchester, UK, 28 June–4 July 2015. [Google Scholar]
- Freihoefer, K.; Guerin, D.; Martin, C.; Kim, H.Y.; Brigham, J.K. Occupants’ satisfaction with, and physical readings of, thermal, acoustic, and lighting conditions of sustainable office workspaces. Indoor Built Environ. 2015, 24, 457–472. [Google Scholar] [CrossRef]
- Boechat, J.; Rios, J.; Ramos, M.; Luiz, R.; Neto, F.A.; Lapa e Silva, J.R. Sick Building Syndrome (SBS) Among Office Workers and Exposure to Indoor Fungal Allergens in Rio de Janeiro, Brazil. J. Allergy Clin. Immunol. 2011, 127, AB178. [Google Scholar] [CrossRef]
- Shaw, M. Housing and public health. Annu. Rev. Public Health 2004, 25, 397–418. [Google Scholar] [CrossRef]
- Bambra, C. Health Divides: Where You Live Can Kill You; Policy Press: Bristol, UK, 2016. [Google Scholar]
- Benveniste, G. Mastering the Politics of Planning: Crafting Credible Plans and Policies that Make a Difference; Jossey-Bass Inc Publiser: San Francisco, CA, USA, 1989. [Google Scholar]
- Jargowsky, P.A. Poverty and Place: Ghettos, Barrios, and the American City; Russell Sage Foundation: New York, NY, USA, 1997. [Google Scholar]
- Tesh, S.N. Uncertain Hazards: Environmental Activists and Scientific Proof; Cornell University Press: Ithaca, NY, USA, 2018. [Google Scholar]
- Heiman, M.K. Science by the people: Grassroots environmental monitoring and the debate over scientific expertise. J. Plan. Educ. Res. 1997, 16, 291–299. [Google Scholar] [CrossRef]
- Krieger, N. Questioning epidemiology: Objectivity, advocacy, and socially responsible science. Am. J. Public Health 1999, 89, 1151–1153. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Brawley, E.C. Enriching lighting design. NeuroRehabilitation 2009, 25, 189–199. [Google Scholar] [CrossRef] [PubMed]
- Foraster, M.; Künzli, N.; Aguilera, I.; Rivera, M.; Agis, D.; Vila, J.; Bouso, L.; Deltell, A.; Marrugat, J.; Ramos, R.; et al. High blood pressure and long-term exposure to indoor noise and air pollution from road traffic. Environ. Health Perspect. 2014, 122, 1193–1200. [Google Scholar] [CrossRef] [PubMed]
- Seabi, J. An epidemiological prospective study of children’s health and annoyance reactions to aircraft noise exposure in South Africa. Int. J. Environ. Res. Public Health 2013, 10, 2760–2777. [Google Scholar] [CrossRef] [PubMed]
- Gou, Z.; Lau, S.S.-Y.; Shen, J. Indoor environmental satisfaction in two LEED offices and its implications in green interior design. Indoor Built Environ. 2012, 21, 503–514. [Google Scholar] [CrossRef]
- Lee, Y.S.; Kim, S.-K. Indoor environmental quality in LEED-certified buildings in the US. J. Asian Archit. Build. Eng. 2008, 7, 293–300. [Google Scholar] [CrossRef]
- Johansson, P.; Svensson, T.; Ekstrand-Tobin, A. Validation of critical moisture conditions for mould growth on building materials. Build. Environ. 2013, 62, 201–209. [Google Scholar] [CrossRef]
- Pietrzyk, K. A systemic approach to moisture problems in buildings for mould safety modelling. Build. Environ. 2015, 86, 50–60. [Google Scholar] [CrossRef]
- Norbäck, D.; Zock, J.; Plana, E.; Heinrich, J.; Tischer, C.; Jacobsen Bertelsen, R.; Olivieri, M. Building dampness and mold in European homes in relation to climate, building characteristics and socio-economic status: The European Community Respiratory Health Survey ECRHS II. Indoor Air 2017, 27, 921–932. [Google Scholar] [CrossRef]
- Kielb, C.; Lin, S.; Muscatiello, N.; Hord, W.; Rogers-Harrington, J.; Healy, J. Building-related health symptoms and classroom indoor air quality: A survey of school teachers in New York State. Indoor Air 2015, 25, 371–380. [Google Scholar] [CrossRef]
- Hwang, T.; Kim, J.T. Effects of indoor lighting on occupants’ visual comfort and eye health in a green building. Indoor Built Environ. 2011, 20, 75–90. [Google Scholar] [CrossRef]
- Ghaffarianhoseini, A.; AlWaer, H.; Omrany, H.; Ghaffarianhoseini, A.; Alalouch, C.; Clements-Croome, D.; Tookey, J. Sick building syndrome: Are we doing enough? Archit. Sci. Rev. 2018, 61, 99–121. [Google Scholar] [CrossRef]
- Dunn, J.R.; Hayes, M.V. Social inequality, population health, and housing: A study of two Vancouver neighborhoods. Soc. Sci. Med. 2000, 51, 563–587. [Google Scholar] [CrossRef]
- MacNaughton, P.; Satish, U.; Laurent, J.G.C.; Flanigan, S.; Vallarino, J.; Coull, B.; Spengler, J.D.; Allen, J.G. The impact of working in a green certified building on cognitive function and health. Build. Environ. 2017, 114, 178–186. [Google Scholar] [CrossRef]
- Richards, E.H. Sanitation in Daily Life; Whitcomb & Barrows: Boston, MA, USA, 1910. [Google Scholar]
- Vaillancourt, J.G. Sociology of the environment: From human ecology to ecosociology. In Environmental Sociology: Theory and Practice; Captus Press: Concord, ON, Canada, 1995; pp. 3–32. [Google Scholar]
- Douglas, I.; James, P. Urban Ecology: An Introduction; Routledge: London, UK, 2014. [Google Scholar]
- Evans, G.W.; McCoy, J.M. When buildings don’t work: The role of architecture in human health. J. Environ. Psychol. 1998, 18, 85–94. [Google Scholar] [CrossRef]
- Wohlwill, J.F. Human adaptation to levels of environmental stimulation. Hum. Ecol. 1974, 2, 127–147. [Google Scholar] [CrossRef]
- Kembel, S.W.; Jones, E.; Kline, J.; Northcutt, D.; Stenson, J.; Womack, A.M.; Bohannan, B.J.; Brown, G.Z.; Green, J.L. Architectural design influences the diversity and structure of the built environment microbiome. ISME J. 2012, 6, 1469. [Google Scholar] [CrossRef]
- Stephens, B. What have we learned about the microbiomes of indoor environments? MSystems 2016, 1, e00083-16. [Google Scholar] [CrossRef]
- Rintala, H.; Pitkäranta, M.; Toivola, M.; Paulin, L.; Nevalainen, A. Diversity and seasonal dynamics of bacterial community in indoor environment. BMC Microbiol. 2008, 8, 56. [Google Scholar] [CrossRef]
- Lax, S.; Smith, D.P.; Hampton-Marcell, J.; Owens, S.M.; Handley, K.M.; Scott, N.M.; Gibbons, S.M.; Larsen, P.; Shogan, B.D.; Weiss, S.; et al. Longitudinal analysis of microbial interaction between humans and the indoor environment. Science 2014, 345, 1048–1052. [Google Scholar] [CrossRef]
- Dunn, R.R.; Fierer, N.; Henley, J.B.; Leff, J.W.; Menninger, H.L. Home life: Factors structuring the bacterial diversity found within and between homes. PLoS ONE 2013, 8, e64133. [Google Scholar] [CrossRef] [PubMed]
- Hospodsky, D.; Qian, J.; Nazaroff, W.W.; Yamamoto, N.; Bibby, K.; Rismani-Yazdi, H.; Peccia, J. Human occupancy as a source of indoor airborne bacteria. PLoS ONE 2012, 7, e34867. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, J.A.; Stephens, B. Microbiology of the built environment. Nat. Rev. Microbiol. 2018, 16, 661–670. [Google Scholar] [CrossRef] [PubMed]
- Jeon, Y.-S.; Chun, J.; Kim, B.-S. Identification of household bacterial community and analysis of species shared with human microbiome. Curr. Microbiol. 2013, 67, 557–563. [Google Scholar] [CrossRef]
- Brown, G.; Kline, J.; Mhuireach, G.; Northcutt, D.; Stenson, J. Making microbiology of the built environment relevant to design. Microbiome 2016, 4, 6. [Google Scholar] [CrossRef]
- Hoisington, A.J.; Brenner, L.A.; Kinney, K.A.; Postolache, T.T.; Lowry, C.A. The microbiome of the built environment and mental health. Microbiome 2015, 3, 60. [Google Scholar] [CrossRef]
- Canter, D.V.; Craik, K.H. Environmental psychology. J. Environ. Psychol. 1981, 1, 1–11. [Google Scholar] [CrossRef]
- Oseland, N. The impact of psychological needs on office design. J. Corp. Real Estate 2009, 11, 244–254. [Google Scholar] [CrossRef]
- Cohen, R.A. Yerkes–Dodson Law. Encycl. Clin. Neuropsychol. 2011, 2737–2738. Available online: https://link.springer.com/referenceworkentry/10.1007%2F978-0-387-79948-3_1340 (accessed on 3 March 2020).
- Franz, G. Space, color, and perceived qualities of indoor environments. In Proceedings of the 19th International Association for People-Environment Studies Conference (IAPS 2006), Seattle, WA, USA, 11–16 September 2006; Hogrefe & Huber: Seattle, WA, USA, 2006. [Google Scholar]
- Nanda, U.; Pati, D.; Ghamari, H.; Bajema, R. Lessons from neuroscience: Form follows function, emotions follow form. Intell. Build. Int. 2013, 5, 61–78. [Google Scholar] [CrossRef]
- Brownson, R.C.; Fielding, J.E.; Maylahn, C.M. Evidence-based public health: A fundamental concept for public health practice. Annu. Rev. Public Health 2009, 30, 175–201. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, M.; Thompson, J.; de Sá, T.H.; Ewing, R.; Mohan, D.; McClure, R.; Roberts, I.; Tiwari, G.; Giles-Corti, B.; Sun, X.; et al. Land use, transport, and population health: Estimating the health benefits of compact cities. Lancet 2016, 388, 2925–2935. [Google Scholar] [CrossRef]
- Wei, Y.; Xiao, W.; Wen, M.; Wei, R. Walkability, land use and physical activity. Sustainability 2016, 8, 65. [Google Scholar] [CrossRef]
- Knuiman, M.W.; Christian, H.E.; Divitini, M.L.; Foster, S.A.; Bull, F.C.; Badland, H.M.; Giles-Corti, B. A longitudinal analysis of the influence of the neighborhood built environment on walking for transportation: The RESIDE study. Am. J. Epidemiol. 2014, 180, 453–461. [Google Scholar] [CrossRef]
- Larice, M.; Macdonald, E. The Urban Design Reader; Routledge: London, UK, 2013. [Google Scholar]
- Jackson, R.J.; Dannenberg, A.L.; Frumkin, H. Health and the built environment: 10 years after. Am. J. Public Health 2013, 103, 1542–1544. [Google Scholar] [CrossRef]
- Wolch, J.R.; Byrne, J.; Newell, J.P. Urban green space, public health, and environmental justice: The challenge of making cities ‘just green enough’. Landsc. Urban Plan. 2014, 125, 234–244. [Google Scholar] [CrossRef]
- Koohsari, M.J.; Badland, H.; Giles-Corti, B. (Re) Designing the built environment to support physical activity: Bringing public health back into urban design and planning. Cities 2013, 35, 294–298. [Google Scholar] [CrossRef]
- Koohsari, M.J.; Mavoa, S.; Villanueva, K.; Sugiyama, T.; Badland, H.; Kaczynski, A.T.; Owen, N.; Giles-Corti, B. Public open space, physical activity, urban design and public health: Concepts, methods and research agenda. Health Place 2015, 33, 75–82. [Google Scholar] [CrossRef]
- Kaczynski, A.T.; Koohsari, M.J.; Stanis, S.A.W.; Bergstrom, R.; Sugiyama, T. Association of street connectivity and road traffic speed with park usage and park-based physical activity. Am. J. Health Promot. 2014, 28, 197–203. [Google Scholar] [CrossRef]
- Giles-Corti, B.; Bull, F.; Knuiman, M.; McCormack, G.; Van Niel, K.; Timperio, A.; Christian, H.; Foster, S.; Divitini, M.; Middleton, N.; et al. The influence of urban design on neighbourhood walking following residential relocation: Longitudinal results from the RESIDE study. Soc. Sci. Med. 2013, 77, 20–30. [Google Scholar] [CrossRef]
- The Drive towards Healthier Buildings 2016. Available online: https://www.worldgbc.org/sites/default/files/Drive%20Toward%20Healthier%20Buildings%202016_ffff.pdf (accessed on 20 July 2018).
- Nelbach, P. An Appraisal Method for Measuring the Quality of Housing: A Yardstick for Health Officers, Housing Officials and Planners. Part III. Appraisal of Neighborhood Environment; American Public Health Association: Washington, DC, USA, 1950. [Google Scholar]
- American Housing Survey: A Measure of (Poor) Housing Quality. Available online: https://www.census.gov/programs-surveys/ahs/research/publications/PoorHousingQuality.html (accessed on 20 July 2018).
- American Planning Association. Planning for Public Health. Available online: https://www.planning.org/research/publichealth/ (accessed on 1 May 2019).
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hu, M.; Roberts, J.D. Connections and Divergence between Public Health and Built Environment—A Scoping Review. Urban Sci. 2020, 4, 12. https://doi.org/10.3390/urbansci4010012
Hu M, Roberts JD. Connections and Divergence between Public Health and Built Environment—A Scoping Review. Urban Science. 2020; 4(1):12. https://doi.org/10.3390/urbansci4010012
Chicago/Turabian StyleHu, Ming, and Jennifer D. Roberts. 2020. "Connections and Divergence between Public Health and Built Environment—A Scoping Review" Urban Science 4, no. 1: 12. https://doi.org/10.3390/urbansci4010012
APA StyleHu, M., & Roberts, J. D. (2020). Connections and Divergence between Public Health and Built Environment—A Scoping Review. Urban Science, 4(1), 12. https://doi.org/10.3390/urbansci4010012





