Latin American Prevalence of Glaucoma: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Elibility Criteria
2.2. Information Source
2.3. Search Strategy
2.4. Study Selection
2.5. Data Extraction
2.6. Endpoints and Subgroup Analysis
2.7. Statistical Analysis and Risk of Bias Assessment
3. Results
3.1. Study Selection and Baseline Characteristics
3.2. Pooled Analysis
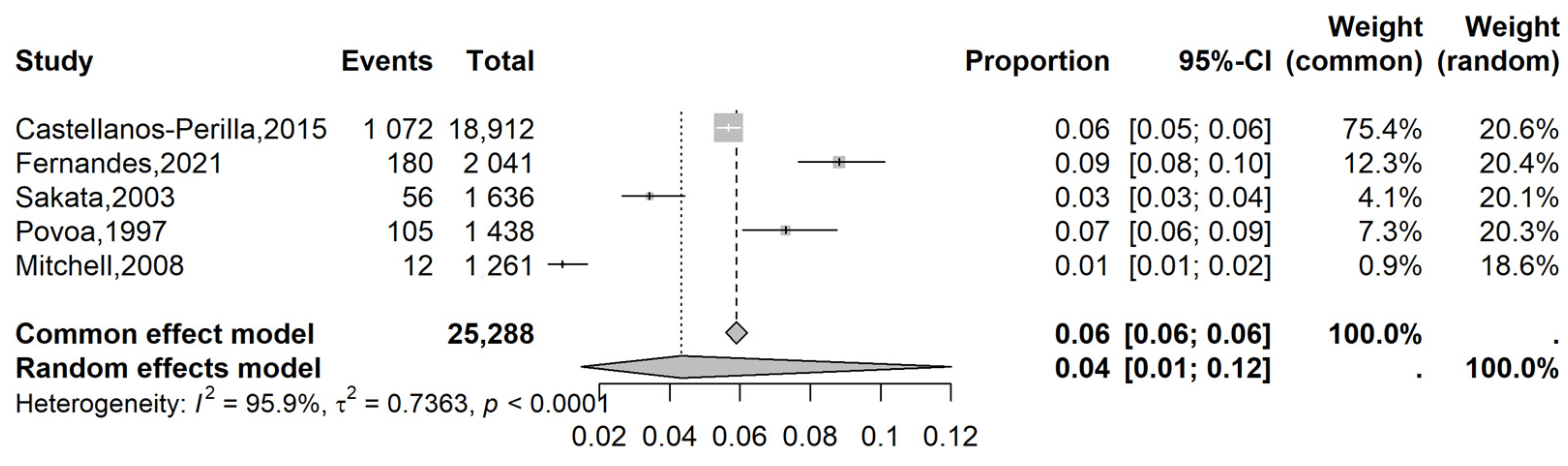
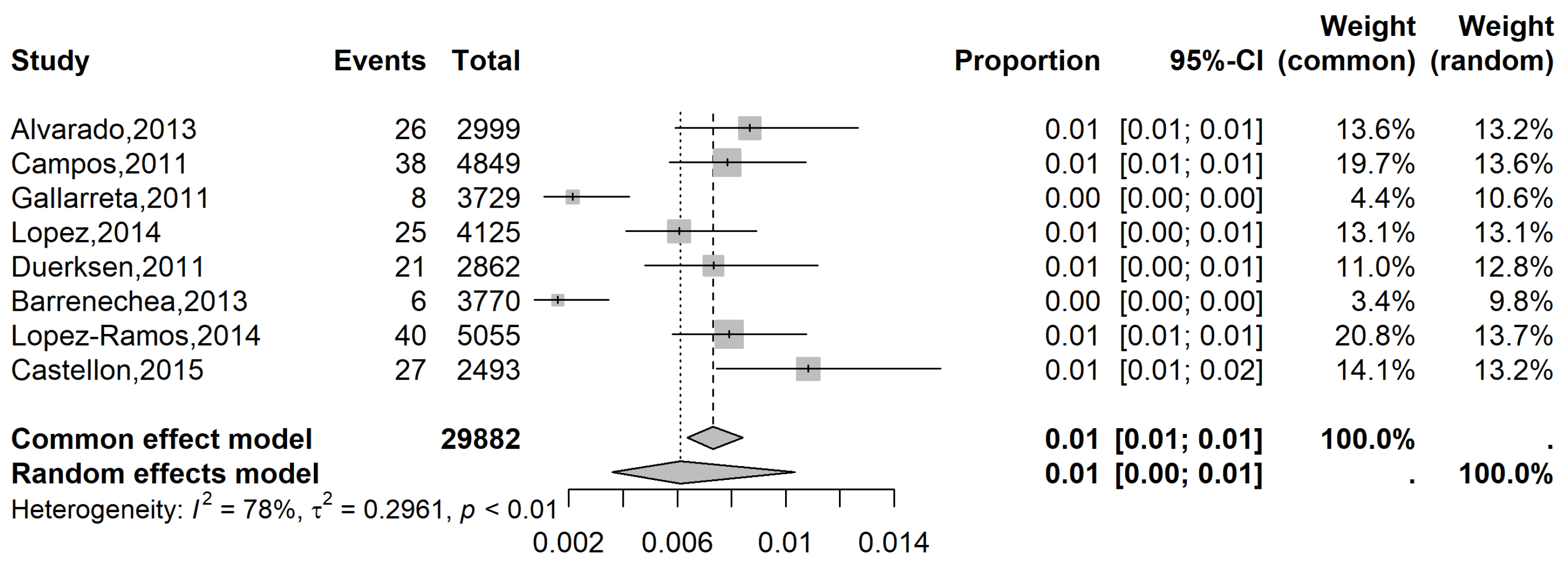
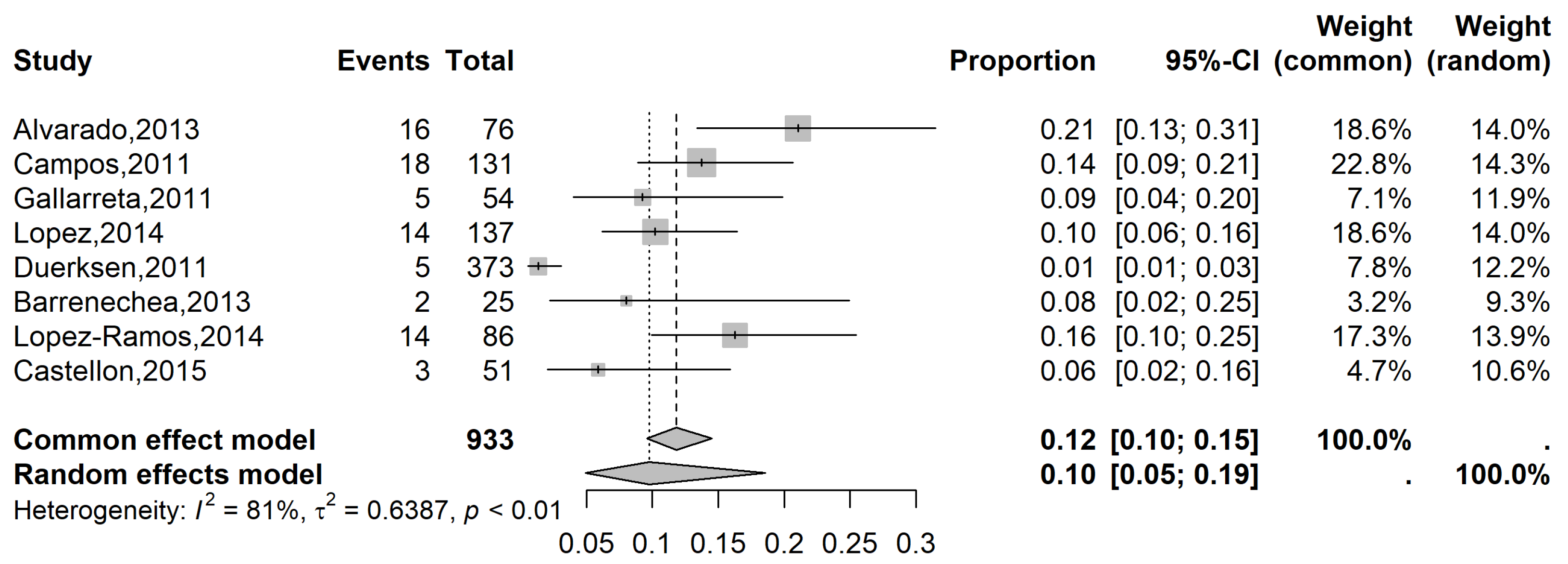
3.2.1. Prevalence of Glaucoma in the LATAM Population
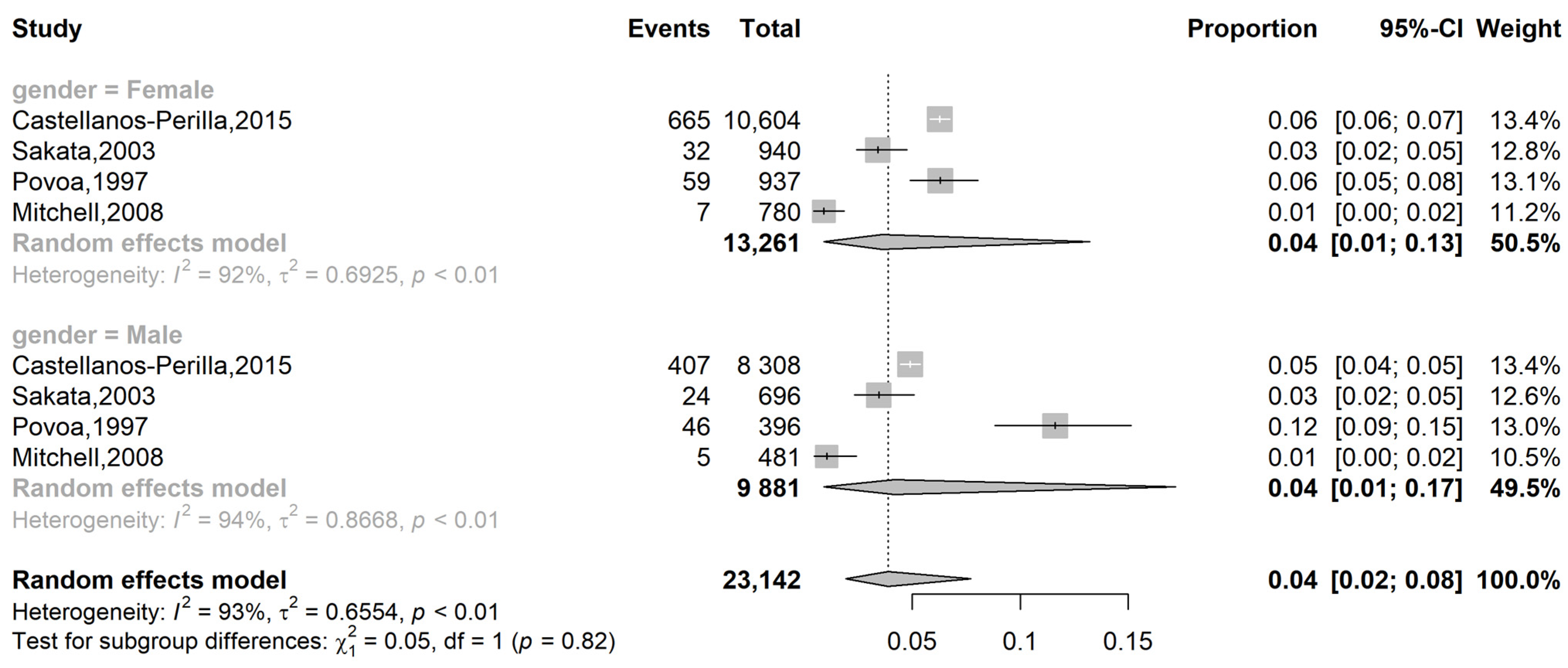
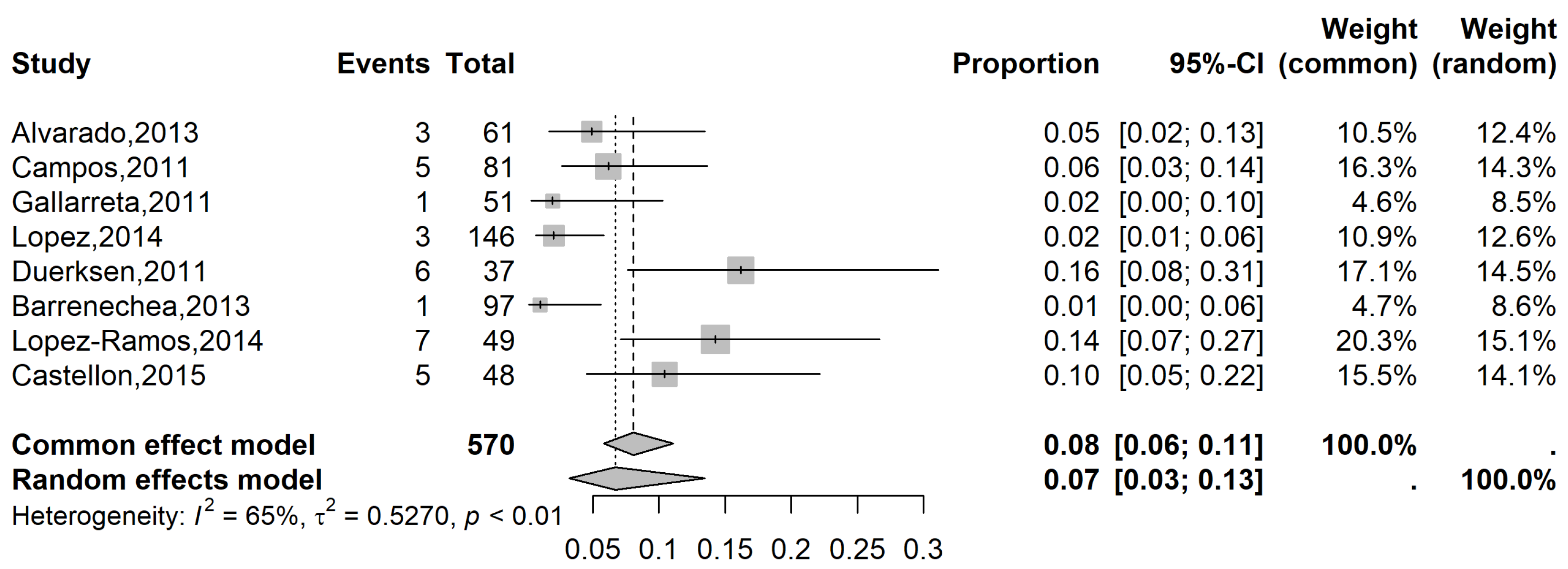
3.2.2. Subgroup Analysis
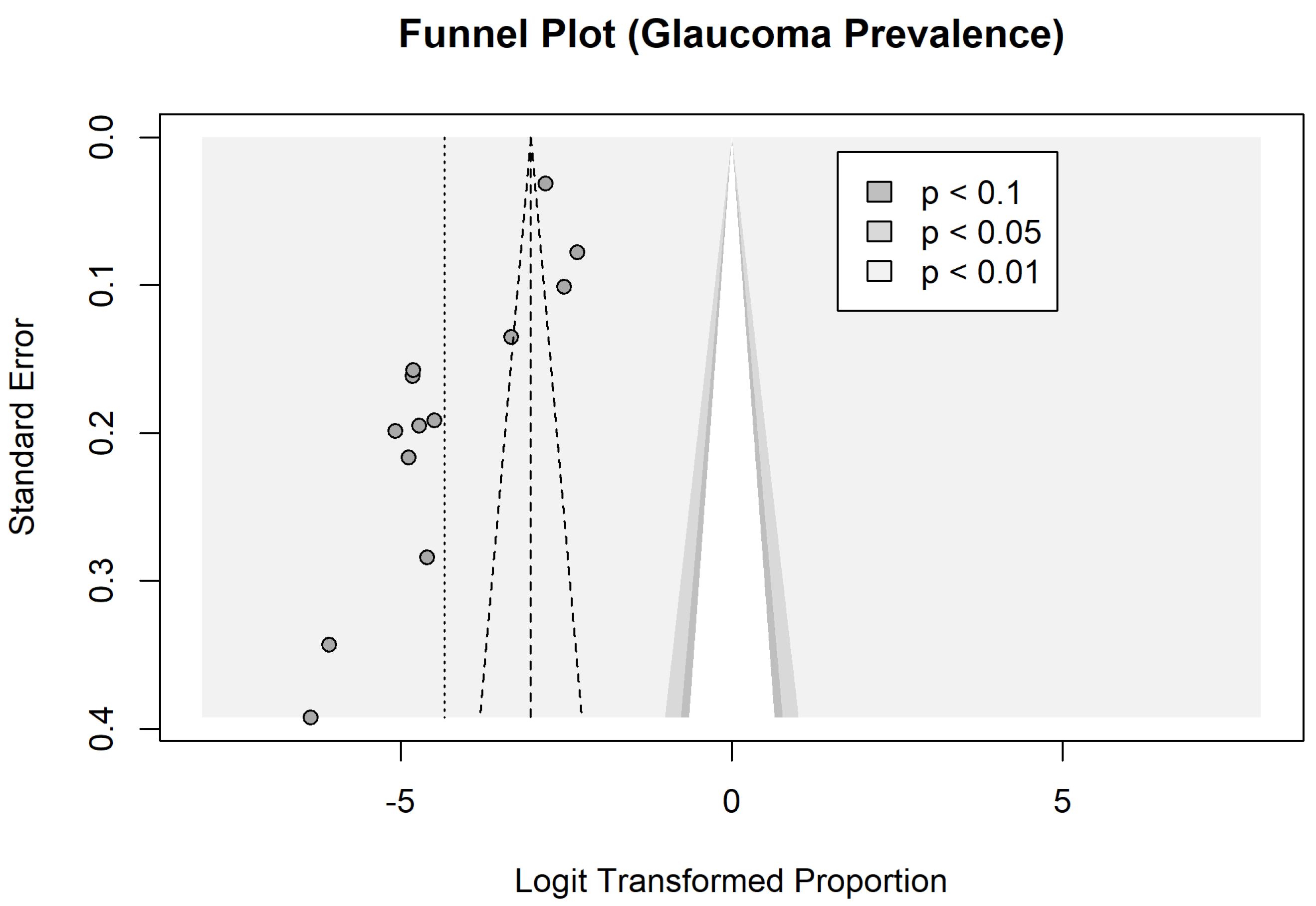
3.3. Quality and Evidence Assessment and Risk of Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| OAG | Open Angle Glaucoma |
| LATAM | Latin America |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analysis |
| CI | Confidence Intervals |
References
- GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: The Right to Sight: An analysis for the Global Burden of Disease Study. Lancet Glob. Health 2021, 9, e144–e160. [Google Scholar] [CrossRef]
- Flaxman, S.R.; Bourne, R.R.A.; Resnikoff, S.; Ackland, P.; Braithwaite, T.; Cicinelli, M.V.; Das, A.; Jonas, J.B.; Keeffe, J.; Kempen, J.H.; et al. Global causes of blindness and distance vision impairment 1990–2020: A systematic review and meta-analysis. Lancet Glob. Health 2017, 5, e1221–e1234. [Google Scholar] [CrossRef] [PubMed]
- Quigley, H.A. Glaucoma. Lancet 2011, 377, 1367–1377. [Google Scholar] [CrossRef]
- Jonas, J.B.; Aung, T.; Bourne, R.R.; Bron, A.M.; Ritch, R.; Panda-Jonas, S. Glaucoma. Lancet 2017, 390, 2183–2193. [Google Scholar] [CrossRef]
- Weinreb, R.N.; Khaw, P.T. Primary open-angle glaucoma. Lancet 2004, 363, 1711–1720. [Google Scholar] [CrossRef]
- Tham, Y.-C.; Li, X.; Wong, T.Y.; Quigley, H.A.; Aung, T.; Cheng, C.-Y. Global prevalence of glaucoma and projections of glaucoma burden through 2040: A systematic review and meta-analysis. Ophthalmology 2014, 121, 2081–2090. [Google Scholar] [CrossRef]
- Khachatryan, N.; Pistilli, M.; Maguire, M.G.; Salowe, R.J.; Fertig, R.M.; Moore, T.; Gudiseva, H.V.; Chavali, V.R.M.; Collins, D.W.; Daniel, E.; et al. Primary Open-Angle African American Glaucoma Genetics (POAAGG) Study: Gender and risk of POAG in African Americans. PLoS ONE 2019, 14, e0218804. [Google Scholar] [CrossRef]
- Vajaranant, T.S.; Wu, S.; Torres, M.; Varma, R. The changing face of primary open-angle glaucoma in the united states: Demographic and geographic changes from 2011 to 2050. Arch. Ophthalmol. 2012, 154, 303–314.e3. [Google Scholar] [CrossRef] [PubMed]
- Friedman, D.S.; Foster, P.J.; Aung, T.; He, M. Angle closure and angle-closure glaucoma: What we are doing now and what we will be doing in the future. Clin. Exp. Ophthalmol. 2012, 40, 381–387. [Google Scholar] [CrossRef]
- Chan, E.W.; Li, X.; Tham, Y.-C.; Liao, J.; Wong, T.Y.; Aung, T.; Cheng, C.-Y. Glaucoma in Asia: Regional prevalence variations and future projections. Br. J. Ophthalmol. 2016, 100, 78–85. [Google Scholar] [CrossRef]
- Kapetanakis, V.V.; Chan, M.P.Y.; Foster, P.J.; Cook, D.G.; Owen, C.G.; Rudnicka, A.R. Global variations and time trends in the prevalence of primary open angle glaucoma (POAG): A systematic review and meta-analysis. Br. J. Ophthalmol. 2016, 100, 86–93. [Google Scholar] [CrossRef]
- United Nations Web Site. Available online: http://esa.un.org (accessed on 15 February 2024).
- Varma, R.; Ying-Lai, M.; A Francis, B.; Nguyen, B.B.-T.; Deneen, J.; Wilson, M.; Azen, S.P.; Los Angeles Latino Eye Study Group. Prevalence of open-angle glaucoma and ocular hypertension in Latinos: The Los Angeles Latino Eye Study. Ophthalmology 2004, 111, 1439–1448. [Google Scholar] [CrossRef] [PubMed]
- Quigley, H.A.; West, S.K.; Rodriguez, J.; Munoz, B.; Klein, R.; Snyder, R. The prevalence of glaucoma in a population-based study of hispanic subjects: Proyecto VER. Arch. Ophthalmol. 2001, 119, 1819–1826. [Google Scholar] [CrossRef] [PubMed]
- Sakata, K.; Sakata, L.M.; Sakata, V.M.; Santini, C.; Hopker, L.M.; Bernardes, R.; Yabumoto, C.; Moreira, A.T.R. Prevalence of glaucoma in a south brazilian population: Projeto Glaucoma. Investig. Opthalmol. Vis. Sci. 2007, 48, 4974–4979. [Google Scholar] [CrossRef] [PubMed]
- Castellanos-Perilla, N.; Garcia-Cifuentes, E.; Pineda-Ortega, J.; Lema, S.; Gelvis, G.; Cano-Gutierrez, C.A.; Mejia-Vergara, A.J. Self-reported glaucoma prevalence and related factors, contribution to reported visual impairment, and functional burden in a cross-sectional study in Colombia. Int. Ophthalmol. 2023, 43, 2447–2455. [Google Scholar] [CrossRef]
- Fernandes, A.G.; Berezovsky, A.; Watanabe, S.E.S.; Mitsuhiro, M.R.K.H.; Cypel, M.C.; Ferraz, N.N.; Furtado, J.M.; Sacai, P.Y.; Muñoz, S.; Cunha, C.C.; et al. Prevalence of ocular findings regardless of visual acuity status in older adults from the Brazilian Amazon Region. Sci. Rep. 2021, 11, 23710. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, Version 6.4 (Updated August 2023); Cochrane: London, UK, 2023; Available online: www.training.cochrane.org/handbook (accessed on 15 February 2024).
- Póvoa, C.A.; Nicolela, M.T.; Valle, A.L.S.L.; Gomes, L.E.d.S.; Neustein, I. Prevalência de glaucoma identificada em campanha de detecção em São Paulo. Arq. Bras. Oftalmol. 2001, 64, 303–307. [Google Scholar] [CrossRef]
- Mitchell, J.P.; Williams, N.; Martin, R.; Keshava, P.; Bynum, M.M.; Figueroa, M.; Yancy, A.; DellaRocca, R. The Venezuela eye evaluation study. J. Natl. Med. Assoc. 2008, 100, 435–438. [Google Scholar] [CrossRef]
- Alvarado, D.; Rivera, B.; Lagos, L.; Ochoa, M.; Starkman, I.; Castillo, M.; Flores, E.; Lansingh, V.C.; Limburg, H.; Silva, J.C. Encuesta nacional de ceguera y deficiencia visual evitables en Honduras. Rev. Panam. Salud Pública 2014, 36, 300–305. [Google Scholar]
- Campos, B.; Cerrate, A.; Montjoy, E.; Dulanto Gomero, V.; Gonzales, C.; Tecse, A.; Pariamachi, A.; Lansingh, V.C.; Dulanto Reinoso, V.; Minaya Barba, J.; et al. Prevalencia y causas de ceguera en Perú: Encuesta nacional. Rev. Panam. Salud Publica-Pan Am. J. Public Health 2014, 36, 283–289. [Google Scholar]
- Gallarreta, M.; Furtado, J.M.; Lansingh, V.C.; Silva, J.C.; Limburg, H. Rapid assessment of avoidable blindness in Uruguay: Results of a nationwide survey. Rev. Panam Salud Publica 2014, 36, 219–224. [Google Scholar]
- Lopez-Ramos, A.; Gomez-Bastar, P.A.; Lansingh, V.C.; Rodriguez-Gomez, J.A.; Vargas-Fragoso, V.; Soria-Arellano, F.A.; Silva-Camacho, S.H.; Castillo-Velazquez, J.; Zepeda-Romero, L.C.; Limburg, H. Rapid assessment of avoidable blindness: Prevalence of blindness, visual impairment and diabetes in nuevo leon, Mexico 2014. Ophthalmic Epidemiol. 2018, 25, 412–418. [Google Scholar] [CrossRef]
- Duerksen, R.; Limburg, H.; Lansingh, V.C.; Silva, J.C. Review of blindness and visual impairment in paraguay: Changes between 1999 and 2011. Ophthalmic Epidemiol. 2013, 20, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Barrenechea, R.; la Fuente, I.D.; Plaza, R.G.; Flores, N.; Segovia, L.; Villagómez, Z.; Camarero, E.E.; Zepeda-Romero, L.C.; Lansingh, V.C.; Limburg, H.; et al. Encuesta nacional de ceguera y deficiencia visual evitable en Argentina, 2013. Rev. Panam. Salud Pública 2015, 37, 7–12. [Google Scholar]
- Castellón, R.I.A.; Vargas, E.C.; Chavarría, R.E.C.; Vargas, G.A.R. Rapid assessment of avoidable blindness and diabetic retinopathy in individuals aged 50 years or older in Costa Rica. PLoS ONE 2019, 14, e0212660. [Google Scholar] [CrossRef]
- Harrer, M.; Cuijpers, P.; Furukawa, T.; Ebert, D. Doing Meta-Analysis with R: A Hands-On Guide; Chapman and Hall/CRC: Boca Raton, FL, USA, 2021. [Google Scholar]
- Takkouche, B.; Cadarso-Suárez, C.; Spiegelman, D. Evaluation of old and new tests of heterogeneity in epidemiologic meta-analysis. Am. J. Epidemiol. 1999, 150, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef]
- Viechtbauer, W. Conducting Meta-Analyses in R with The meta for Package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Reis, T.F.; Paula, J.S.; Furtado, J.M. Primary glaucomas in adults: Epidemiology and public health-A review. Clin. Exp. Ophthalmol. 2022, 50, 128–142. [Google Scholar] [CrossRef]
- Rudnicka, A.R.; Mt-Isa, S.; Owen, C.G.; Cook, D.G.; Ashby, D. Variations in primary open-angle glaucoma prevalence by age, gender, and race: A bayesian meta-analysis. Investig. Opthalmology Vis. Sci. 2006, 47, 4254–4261. [Google Scholar] [CrossRef]
- Vajaranant, T.S.; Nayak, S.; Wilensky, J.T.; E Joslin, C. Gender and glaucoma: What we know and what we need to know. Curr. Opin. Ophthalmol. 2010, 21, 91–99. [Google Scholar] [CrossRef]
- Higginbotham, E.J. Does sex matter in glaucoma? Arch. Ophthalmol. 2004, 122, 374–375. [Google Scholar] [CrossRef]
- Hulsman, C.A.A.; Westendorp, I.C.D.; Ramrattan, R.S.; Wolfs, R.C.W.; Witteman, J.C.M.; Vingerling, J.R.; Hofman, A.; de Jong, P.T.V.M. Is open-angle glaucoma associated with early menopause?: The Rotterdam Study. Am. J. Epidemiol. 2001, 154, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Mark, H.H. Gender differences in glaucoma and ocular hypertension. Arch. Ophthalmol. 2005, 123, 284. [Google Scholar] [CrossRef]
- Amerasinghe, N.; Aung, T. Angle-closure: Risk factors, diagnosis and treatment. Prog. Brain Res. 2008, 173, 31–45. [Google Scholar] [CrossRef] [PubMed]
- Drance, S.; Anderson, D.R.; Schulzer, M.; Group CN-TGS. Risk factors for progression of visual field abnormalities in normal-tension glaucoma. Am. J. Ophthalmol. 2001, 131, 699–708. [Google Scholar] [CrossRef]
- Quigley, H.A.; Broman, A.T. The number of people with glaucoma worldwide in 2010 and 2020. Br. J. Ophthalmol. 2006, 90, 262–267. [Google Scholar] [CrossRef]
- Foster, P.J.; Broadway, D.C.; Hayat, S.; Luben, R.; Dalzell, N.; Bingham, S.; Wareham, N.J.; Khaw, K.-T. Refractive error, axial length and anterior chamber depth of the eye in British adults: The EPIC-Norfolk Eye Study. Br. J. Ophthalmol. 2010, 94, 827–830. [Google Scholar] [CrossRef]
- Hashemi, H.; Khabazkhoob, M.; Miraftab, M.; Emamian, M.H.; Shariati, M.; Abdolahinia, T.; Fotouhi, A. The distribution of axial length, anterior chamber depth, lens thickness, and vitreous chamber depth in an adult population of Shahroud, Iran. BMC Ophthalmol. 2012, 12, 50. [Google Scholar] [CrossRef]
- Chen, H.; Lin, H.; Lin, Z.; Chen, J.; Chen, W. Distribution of axial length, anterior chamber depth, and corneal curvature in an aged population in South China. BMC Ophthalmol. 2016, 16, 47. [Google Scholar] [CrossRef] [PubMed]
- Cedrone, C.; Mancino, R.; Cerulli, A.; Cesareo, M.; Nucci, C. Epidemiology of primary glaucoma: Prevalence, incidence, and blinding effects. Prog. Brain Res. 2008, 173, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Chen, A.; Zou, M.; Zhang, Y.; Jin, L.; Li, Y.; Zheng, D.; Jin, G.; Congdon, N. Time trends, associations and prevalence of blindness and vision loss due to glaucoma: An analysis of observational data from the Global Burden of Disease Study 2017. BMJ Open 2022, 12, e053805. [Google Scholar] [CrossRef] [PubMed]
- Davuluru, S.S.; Jess, A.T.; Bin Kim, J.S.; Yoo, K.; Nguyen, V.; Xu, B.Y. Identifying, Understanding, and Addressing Disparities in Glaucoma Care in the United States. Transl. Vis. Sci. Technol. 2023, 12, 18. [Google Scholar] [CrossRef]
- Garg, H.; Singh, L.K.; Khanna, M.; Pooja, N. Performance analysis of machine learning techniques for glaucoma detection based on textural and intensity features. Int. J. Innov. Comput. Appl. 2020, 11, 216. [Google Scholar] [CrossRef]
- Singh, L.K.; Pooja; Garg, H.; Khanna, M. Histogram of Oriented Gradients (HOG)-Based Artificial Neural Network (ANN) Classifier for Glaucoma Detection. Int. J. Swarm Intell. Res. 2022, 13, 1–32. [Google Scholar] [CrossRef]
- Singh, L.K.; Khanna, M.; Thawkar, S.; Singh, R. A novel hybridized feature selection strategy for the effective prediction of glaucoma in retinal fundus images. Multimed. Tools Appl. 2023, 83, 46087–46159. [Google Scholar] [CrossRef]
- Assefa, A.; Bihon, A. A systematic review and meta-analysis of prevalence of Escherichia coli in foods of animal origin in Ethiopia. Heliyon 2018, 4, e00716. [Google Scholar] [CrossRef]
- Guedes, J.; Neto, A.B.d.C.; Fernandes, B.F.; Faneli, A.C.; Ferreira, M.A.; Amaral, D.C.; Mora-Paez, D.J.; Ambrósio, R. Myopia Prevalence in Latin American Children and Adolescents: A Systematic Review and Meta-Analysis. Cureus 2024, 16, e63482. [Google Scholar] [CrossRef] [PubMed]
- Costa Neto, A.; Guedes, J.; Mora-Paez, D.J.; Ferreira, M.A.; Faneli, A.C.; Amaral, D.C.; Pereira, S.; Almeida, G.; Manteufel, V.; Haddad Neto, J.S.; et al. Systematic review and meta-analysis of myopia prevalence in Brazilian school children. Rev. Bras. Oftalmol. 2024, 83, e0056. [Google Scholar] [CrossRef]
- Nikolakopoulou, A.; Mavridis, D.; Salanti, G. Demystifying fixed and random effects meta-analysis. Evid. Based Ment. Health 2014, 17, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Ades, A.E.; Lu, G.; Higgins, J.P.T. The interpretation of random-effects meta-analysis in decision models. Med. Decis. Mak. 2005, 25, 646–654. [Google Scholar] [CrossRef]
- Cheng, J.-W.; Zong, Y.; Zeng, Y.-Y.; Wei, R.-L. The prevalence of primary angle closure glaucoma in adult asians: A systematic review and meta-analysis. PLoS ONE 2014, 9, e103222. [Google Scholar] [CrossRef]


| Author | Year | Location | Age Inclusion | Mean Age | N Total | N Total (M/F) | N Glaucoma | N Glaucoma (M/F) | Quality Score |
|---|---|---|---|---|---|---|---|---|---|
| Group 1 | |||||||||
| Sakata | 2003 | Brazil | 40 at least | 53.7 | 1636 | 696/940 | 56 | 24/32 | 10 |
| Povoa | 1997 | Brazil | 40 at least | 58.2 | 1438 | 396/937 | 105 | 46/59 | 10 |
| Mitchell | 2008 | Venezuela | NA | NA | 1261 | 481/780 | 12 | 5/7 | 8 |
| Castellanos-Perilla | 2015 | Colombia | 60 at least | 69.11 | 18,912 | 8308/10,604 | 1072 | 407/665 | 10 |
| Fernandes | 2021 | Brazil | 45 at least | 60.33 | 2041 | NA | 180 | NA | 8 |
| Group 2 | |||||||||
| Gallarreta | 2011 | Uruguay | 50 at least | NA | 3729 | 1571/2158 | 8 | NA | 9 |
| Lopez | 2014 | Panamá | 50 at least | NA | 4125 | NA | 25 | NA | 8 |
| Alvarado | 2013 | Honduras | 50 at least | NA | 2999 | NA | 26 | NA | 8 |
| Campos | 2011 | Peru | 50 at least | 65.07 | 4849 | 2014/2835 | 38 | NA | 9 |
| Duerksen | 2011 | Paraguay | 50 at least | NA | 2862 | NA | 21 | NA | 8 |
| Barrenechea | 2013 | Argentina | 50 at least | NA | 3770 | 1691/2079 | 6 | NA | 9 |
| Lopez-Ramos | 2014 | Mexico | 50 at least | NA | 5055 | NA | 40 | NA | 8 |
| Castellon | 2015 | Costa Rica | 50 at least | 64.64 | 2493 | 923/1570 | 27 | NA | 9 |
| Author | Year | Definition of Glaucoma |
|---|---|---|
| Group 1 | ||
| Sakata | 2003 | Diagnosis required either: (1) optic disc abnormalities (VCDR ≥ 97.5th percentile in a hypernormal population) plus compatible VF defect; or (2) if VF could not be performed, a severely damaged optic disc (VCDR ≥ 99.5th percentile) alone was sufficient. |
| Povoa | 1997 | Referred to second phase if IOP ≥ 21 mmHg and/or at least one of the following: C/D ratio ≥ 0.5, disc asymmetry ≥ 0.2, localized rim thinning, papillary hemorrhage, or pallor. Diagnosis based on comprehensive ophthalmic assessment. |
| Mitchell | 2008 | Presumed glaucoma was diagnosed with IOP > 25 mmHg, disc abnormalities (as defined), and nerve fiber bundle loss. |
| Castellanos-Perilla | 2015 | Glaucoma status based on self-reported history of diagnosis. |
| Fernandes | 2021 | Diagnosis based on anterior segment biomicroscopy, lens status, IOP measurement, and dilated fundus examination. |
| Group 2 | ||
| Gallarreta | 2011 | NA |
| Lopez | 2014 | NA |
| Alvarado | 2013 | NA |
| Campos | 2011 | NA |
| Duerksen | 2011 | Based on afferent pupil defect and corneal edema, VCDR > 0.8, or stone-hard eye on palpation. |
| Barrenechea | 2013 | NA |
| Lopez-Ramos | 2014 | NA |
| Castellon | 2015 | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mora-Paez, D.J.; Guedes, J.; Amaral, D.C.; Ferreira, M.A.; Fernandes, B.F.; Pereira, S.F.; Botton, B.; Desai, A.; Pakter, H.M.; Lavinsky, F.; et al. Latin American Prevalence of Glaucoma: A Systematic Review and Meta-Analysis. Vision 2025, 9, 42. https://doi.org/10.3390/vision9020042
Mora-Paez DJ, Guedes J, Amaral DC, Ferreira MA, Fernandes BF, Pereira SF, Botton B, Desai A, Pakter HM, Lavinsky F, et al. Latin American Prevalence of Glaucoma: A Systematic Review and Meta-Analysis. Vision. 2025; 9(2):42. https://doi.org/10.3390/vision9020042
Chicago/Turabian StyleMora-Paez, Denisse J., Jaime Guedes, Dillan Cunha Amaral, Marcelo Alves Ferreira, Bruno F. Fernandes, Sacha F. Pereira, Bruno Botton, Alisha Desai, Helena Messinger Pakter, Fabio Lavinsky, and et al. 2025. "Latin American Prevalence of Glaucoma: A Systematic Review and Meta-Analysis" Vision 9, no. 2: 42. https://doi.org/10.3390/vision9020042
APA StyleMora-Paez, D. J., Guedes, J., Amaral, D. C., Ferreira, M. A., Fernandes, B. F., Pereira, S. F., Botton, B., Desai, A., Pakter, H. M., Lavinsky, F., & Filho, A. A. C. (2025). Latin American Prevalence of Glaucoma: A Systematic Review and Meta-Analysis. Vision, 9(2), 42. https://doi.org/10.3390/vision9020042






