Factors Associated with Utilization of Teleretinal Imaging in a Hospital-Based Primary Care Setting
Abstract
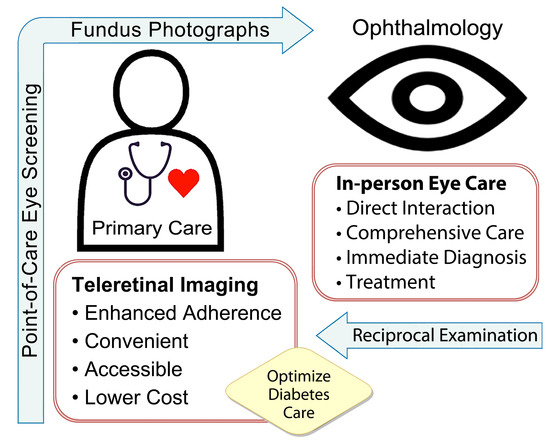
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Time-Driven Activity-Based Costing
2.3. Net-Present Value Analysis
2.4. Statistical Analysis
3. Results
3.1. Demographic, Biometric, and Socioeconomic Factors Predicting Remote Screening
3.2. Multivariate Regression Analysis for Factors Associated with Completing TRI
3.3. Detection of Diabetic Retinopathy
3.4. Cost Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- International Diabetes Foundation. Key Global Findings, 10th ed.; IDF Diabetes Atlas: Brussels, Belgium, 2021; Available online: https://diabetesatlas.org/ (accessed on 12 July 2023).
- Cheung, N.; Mitchell, P.; Wong, T.Y. Diabetic retinopathy. Lancet 2010, 376, 124–136. [Google Scholar] [CrossRef] [PubMed]
- Ramsey, D.J.; Arden, G.B. Hypoxia and dark adaptation in diabetic retinopathy: Interactions, consequences, and therapy. Curr. Diab. Rep. 2015, 15, 118. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Vision Health Initiative (VHI). National Center for Chronic Disease Prevention and Health Promotion, Division of Diabetes Translation. Tips to Prevent Vision Loss. Available online: https://www.cdc.gov/visionhealth/risk/tips.htm (accessed on 28 January 2021).
- Solomon, S.D.; Chew, E.; Duh, E.J.; Sobrin, L.; Sun, J.K.; VanderBeek, B.L.; Wykoff, C.C.; Gardner, T.W. Diabetic retinopathy: A position statement by the American Diabetes Association. Diabetes Care 2017, 40, 412–418. [Google Scholar] [CrossRef]
- Flaxel, C.J.; Adelman, R.A.; Bailey, S.T.; Fawzi, A.; Lim, J.I.; Vemulakonda, G.A.; Ying, G.S. Diabetic Retinopathy Preferred Practice Pattern®. Ophthalmology 2020, 127, P66–P145. [Google Scholar] [CrossRef] [PubMed]
- Keenum, Z.; McGwin, G.; Witherspoon, C.D.; Haller, J.A.; Clark, M.E.; Owsley, C. Patients’ adherence to recommended follow-up eye care after diabetic retinopathy screening in a publicly funded county clinic and factors associated with follow-up eye care use. JAMA Ophthalmol. 2016, 134, 1221–1228. [Google Scholar] [CrossRef]
- Gibson, A.A.; Humphries, J.; Gillies, M.; Nassar, N.; Colagiuri, S. Adherence to eye examination guidelines among individuals with diabetes: An analysis of linked health data. Clin. Exp. Ophthalmol. 2020, 48, 1229–1238. [Google Scholar] [CrossRef] [PubMed]
- Gange, W.S.; Xu, B.Y.; Lung, K.; Toy, B.C.; Seabury, S.A. Rates of eye care and diabetic eye disease among insured patients with newly diagnosed type 2 diabetes. Ophthalmol. Retin. 2021, 5, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Klein, R.; Klein, B.E. Screening for diabetic retinopathy, revisited. Am. J. Ophthalmol. 2002, 134, 261–263. [Google Scholar] [CrossRef]
- Lundeen, E.A.; Wittenborn, J.; Benoit, S.R.; Saaddine, J. Disparities in receipt of eye exams among Medicare Part B fee-for-service beneficiaries with diabetes—United States, 2017. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 1020–1023. [Google Scholar] [CrossRef]
- Daskivich, L.P.; Vasquez, C.; Martinez, C., Jr.; Tseng, C.H.; Mangione, C.M. Implementation and evaluation of a large-scale teleretinal diabetic retinopathy screening program in the Los Angeles County Department of Health Services. JAMA Intern. Med. 2017, 177, 642–649. [Google Scholar] [CrossRef]
- Kuo, J.; Liu, J.C.; Gibson, E.; Rao, P.K.; Margolis, T.P.; Wilson, B.; Gordon, M.O.; Fondahn, E.; Rajagopal, R. Factors associated with adherence to screening guidelines for diabetic retinopathy among low-income metropolitan patients. Mo. Med. 2020, 117, 258–264. [Google Scholar] [PubMed]
- Nguyen, H.V.; Tan, G.S.; Tapp, R.J.; Mital, S.; Ting, D.S.; Wong, H.T.; Tan, C.S.; Laude, A.; Tai, E.S.; Tan, N.C.; et al. Cost-effectiveness of a national telemedicine diabetic reitinopathy screening program in Singapore. Ophthalmology 2018, 123, 2571–2580. [Google Scholar] [CrossRef] [PubMed]
- Pearce, E.; Sivaprasad, S. A review of advancements and evidence gaps in diabetic retinopathy screening models. Clin. Ophthalmol. 2020, 14, 3285–3296. [Google Scholar] [CrossRef] [PubMed]
- Silva, P.S.; Cavallerano, J.D.; Sun, J.K.; Noble, J.; Aiello, L.M.; Aiello, L.P. Nonmydriatic ultrawide field retinal imaging compared with dilated standard 7-field 35-mm photography and retinal specialist examination for evaluation of diabetic retinopathy. Am. J. Ophthalmol. 2012, 154, 549–559.e2. [Google Scholar] [CrossRef]
- Piyasena, M.M.P.N.; Yip, J.L.Y.; MacLeod, D.; Kim, M.; Gudlavalleti, V.S.M. Diagnostic test accuracy of diabetic retinopathy screening by physician graders using a hand-held non-mydriatic retinal camera at a tertiary level medical clinic. BMC Ophthalmol. 2019, 19, 89. [Google Scholar] [CrossRef]
- Ullah, W.; Pathan, S.K.; Panchal, A.; Anandan, S.; Saleem, K.; Sattar, Y.; Ahmad, E.; Mukhtar, M.; Nawaz, H. Cost-effectiveness and diagnostic accuracy of telemedicine in macular disease and diabetic retinopathy: A systematic review and meta-analysis. Medicine 2020, 99, e20306. [Google Scholar] [CrossRef]
- Fuller, S.D.; Hu, J.; Liu, J.C.; Gibson, E.; Gregory, M.; Kuo, J.; Rajagopal, R. Five-year cost-effectiveness modeling of primary care-based, nonmydriatic automated retinal image analysis screening among low-income patients with diabetes. J. Diabetes Sci. Technol. 2022, 16, 415–427. [Google Scholar] [CrossRef]
- Aleo, C.L.; Murchison, A.P.; Dai, Y.; Hark, L.A.; Mayro, E.L.; Collymore, B.; Haller, J.A. Improving eye care follow-up adherence in diabetic patients with ocular abnormalities: The effectiveness of patient contracts in a free, pharmacy-based eye screening. Public Health 2015, 129, 996–999. [Google Scholar] [CrossRef]
- Gu, D.; Agron, S.; May, L.N.; Mirza, R.G.; Bryar, P.J. Nonmydriatic retinal diabetic screening in the primary care setting: Assessing degree of retinopathy and incidence of nondiabetic ocular diagnoses. Telemed. J. E Health 2020, 26, 1252–1256. [Google Scholar] [CrossRef]
- Owsley, C.; McGwin, G.; Lee, D.J.; Lam, B.L.; Friedman, D.S.; Gower, E.W.; Haller, J.A.; Hark, L.A.; Saaddine, J.; Innovative Network for Sight (INSIGHT) Research Group. Diabetes eye screening in urban settings serving minority populations: Detection of diabetic retinopathy and other ocular findings using telemedicine. JAMA Ophthalmol. 2015, 133, 174–181. [Google Scholar] [CrossRef]
- Jani, P.D.; Forbes, L.; Choudhury, A.; Preisser, J.S.; Viera, A.J.; Garg, S. Evaluation of diabetic retinal screening and factors for ophthalmology referral in a telemedicine network. JAMA Ophthalmol. 2017, 135, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Martinez, J.A.; Parikh, P.D.; Wong, R.W.; Harper, C.A.; Dooner, J.W.; Levitan, M.; Nixon, P.A.; Young, R.C.; Ghafoori, S.D. Telemedicine for diabetic retinopathy screening in an urban, insured population using fundus cameras in a primary care office setting. Ophthalmic Surg. Lasers Imaging Retin. 2019, 50, e274–e277. [Google Scholar] [CrossRef] [PubMed]
- Chin, E.; Ventura, B.V.; See, K.Y.; Seibles, J.; Park, S.S. Nonmydriatic fundus photography for teleophthalmology diabetic retinopathy screening in rural and urban clinics. Telemed. J. E Health 2014, 20, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Toy, B.C.; Aguinaldo, T.; Eliason, J.; Egbert, J. Non-mydriatic fundus camera screening for referral-warranted diabetic retinopathy in a northern California safety-net setting. Ophthalmic Surg. Lasers Imaging Retin. 2016, 47, 636–642. [Google Scholar] [CrossRef]
- Tsui, I.; Havunjian, M.A.; Davis, J.A.; Giaconi, J.A. Snapshot of teleretinal screening for diabetic retinopathy at the West Los Angeles Medical Center. Telemed. J. E Health 2016, 22, 843–846. [Google Scholar] [CrossRef]
- Dorali, P.; Shahmoradi, Z.; Weng, C.Y.; Lee, T. Cost-effectiveness analysis of a personalized, teleretinal-inclusive screening policy for diabetic retinopathy via Markov modeling. Ophthalmol. Retina 2023, 7, 532–542. [Google Scholar] [CrossRef]
- Kuo, K.H.; Anjum, S.; Nguyen, B.; Marx, J.L.; Roh, S.; Ramsey, D.J. Utilization of remote diabetic retinal screening in a suburban healthcare system. Clin. Ophthalmol. 2021, 15, 3865–3875. [Google Scholar] [CrossRef]
- Garoon, R.B.; Lin, W.V.; Young, A.K.; Yeh, A.G.; Chu, Y.I.; Weng, C.Y. Cost savings analysis for a diabetic retinopathy teleretinal screening program using an activity-based costing approach. Ophthalmol. Retina 2018, 2, 906–913. [Google Scholar] [CrossRef]
- Centers for Medicare and Medicaid Services. Current Medicare Coverage of Diabetes Supplies. 2021. Available online: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/Downloads/SE18011.pdf#:~:text=Medicare%20covers%20certain%20supplies%20if%20a%20beneficiary%20has,pumps%20and%20the%20insulin%20used%20in%20the%20pumps (accessed on 19 July 2021).
- Calman, N.S.; Hauser, D.; Chokshi, D.A. “Lost to follow-up”: The public health goals of accountable care. Arch. Intern. Med. 2012, 172, 584–586. [Google Scholar] [CrossRef]
- Sabharwal, S.; Kuo, K.H.; Roh, S.; Ramsey, D.J. An initiative to improve follow-up of patients with diabetic retinopathy. Ophthalmic. Physiol. Opt. 2022, 42, 965–972. [Google Scholar] [CrossRef]
- National Committee for Quality Assurance. Comprehensive Diabetes Care (CDC). Available online: https://www.ncqa.org/hedis/measures/comprehensive-diabetes-care/ (accessed on 3 June 2022).
- Internal Revenue Service. SOI Tax Stats—Individual Income Tax Statistics—ZIP Code Data (SOI). 2021. Available online: https://www.irs.gov/statistics/soi-tax-stats-individual-income-tax-statistics-zip-code-data-soi (accessed on 6 April 2021).
- Salary.com. Physician-Ophthalmology Salary in the United States. Available online: https://www.salary.com/research/salary/benchmark/opthalmologist-salary (accessed on 28 January 2021).
- Salary.com. Optometrist Salary in the United States. Available online: https://www.salary.com/research/salary/benchmark/optometrist-salary (accessed on 28 January 2021).
- Salary.com. Hourly Wage for Medical Assistant Salary in the United States. Available online: https://www.salary.com/research/salary/benchmark/medical-assistant-hourly-wages (accessed on 28 January 2021).
- Mead, M.; Atkinson, T.; Srivastava, A.; Walter, N. The return on investment of orthopaedic fellowship training: A ten-year update. J. Am. Acad. Orthop. Surg. 2020, 28, e524–e531. [Google Scholar] [CrossRef]
- Eppley, S.E.; Mansberger, S.L.; Ramanathan, S.; Lowry, E.A. Characteristics associated with adherence to annual dilated eye examinations among US patients with diagnosed diabetes. Ophthalmology 2019, 126, 492–1499. [Google Scholar] [CrossRef]
- Klein, R.; Klein, B.E. The prevalence of age-related eye diseases and visual impairment in aging: Current estimates. Invest. Ophthalmol. Vis. Sci. 2013, 54, ORSF5–ORSF13. [Google Scholar] [CrossRef] [PubMed]
- Munzar, R.; Anaya, J.A.; Lasalle, C.; Roh, S.; Ramsey, D.J. Effectiveness and financial viability of telehealth physician extenders for re-engagement of patients with diabetic retinopathy. Telemed. J. e-Health 2023. published online ahead of print. [Google Scholar] [CrossRef]
- Bryl, A.; Mrugacz, M.; Falkowski, M.; Zorena, K. The effect of hyperlipidemia on the course of diabetic retinopathy-literature review. J. Clin. Med. 2022, 11, 2761. [Google Scholar] [CrossRef] [PubMed]
- Tapp, R.J.; Shaw, J.E.; Harper, C.A.; de Courten, M.P.; Balkau, B.; McCarty, D.J.; Taylor, H.R.; Welborn, T.A.; Zimmet, P.Z.; AusDiab Study Group. The prevalence of and factors associated with diabetic retinopathy in the Australian population. Diabetes Care 2003, 26, 1731–1737. [Google Scholar] [CrossRef] [PubMed]
- Pearce, I.; Simó, R.; Lövestam-Adrian, M.; Wong, D.T.; Evans, M. Association between diabetic eye disease and other complications of diabetes: Implications for care. A systematic review. Diabetes Obes. Metab. 2019, 21, 467–478. [Google Scholar] [CrossRef]
- Ramsey, D.J.; Lasalle, C.C.; Anjum, S.; Marx, J.L.; Roh, S. Telehealth encourages patients with diabetes in racial and ethnic minority groups to return for in-person ophthalmic care during the COVID-19 pandemic. Clin. Ophthalmol. 2022, 16, 2157–2166. [Google Scholar] [CrossRef]
- Shan, R.; Ding, J.; Plante, T.B.; Martin, S.S. Mobile health access and use among individuals with or at risk for cardiovascular disease: 2018 Health Information National Trends Survey (HINTS). J. Am. Heart Assoc. 2019, 8, e014390. [Google Scholar] [CrossRef]
- Shi, L.; Wu, H.; Dong, J.; Jiang, K.; Lu, X.; Shi, J. Telemedicine for detecting diabetic retinopathy: A systematic review and meta-analysis. Br. J. Ophthalmol. 2015, 99, 823–831. [Google Scholar] [CrossRef]
- Borrelli, E.; Querques, L.; Lattanzio, R.; Cavalleri, N.; Moretti, A.G.; Di Biase, C.; Signorino, A.; Gelormini, F.; Sacconi, R.; Bandello, F.; et al. Nonmydriatic widefield retinal imaging with an automatic white LED confocal imaging system compared with dilated ophthalmoscopy in screening for diabetic retinopathy. Acta Diabetol. 2020, 57, 1043–1047. [Google Scholar] [CrossRef]
- World Health Organization Regional Office for Europe. Diabetic Retinopathy Screening: A Short Guide. 2020. Available online: https://www.euro.who.int/en/publications/abstracts/diabetic-retinopathy-screening-a-short-guide-2020 (accessed on 17 August 2021).
- Sharif, A.; Jendle, J.; Hellgren, K.J. Screening for diabetic retinopathy with extended intervals, safe and without compromising adherence: A retrospective cohort study. Diabetes Ther. 2021, 12, 223–234. [Google Scholar] [CrossRef]
- Conlin, P.R.; Fisch, B.M.; Cavallerano, A.A.; Cavallerano, J.D.; Bursell, S.E.; Aiello, L.M. Nonmydriatic teleretinal imaging improves adherence to annual eye examinations in patients with diabetes. J. Rehabil. Res. Dev. 2006, 43, 733–740. [Google Scholar] [CrossRef] [PubMed]
- Fonda, S.J.; Bursell, S.E.; Lewis, D.G.; Garren, J.; Hock, K.; Cavallerano, J. The relationship of a diabetes telehealth eye care program to standard eye care and change in diabetes health outcomes. Telemed. J. E Health 2007, 13, 635–644. [Google Scholar] [CrossRef]
- Sabanayagam, C.; Banu, R.; Chee, M.L.; Lee, R.; Wang, Y.X.; Tan, G.; Jonas, J.B.; Lamoureux, E.L.; Cheng, C.Y.; Klein, B.E.K.; et al. Incidence and progression of diabetic retinopathy: A systematic review. Lancet Diabetes Endocrinol. 2019, 7, 140–149. [Google Scholar] [CrossRef] [PubMed]
- Fatehi, F.; Jahedi, F.; Tay-Kearney, M.L.; Kanagasingam, Y. Teleophthalmology for the elderly population: A review of the literature. Int. J. Med. Inform. 2020, 136, 104089. [Google Scholar] [CrossRef] [PubMed]
- Patzer, K.H.; Ardjomand, P.; Göhring, K.; Klempt, G.; Patzelt, A.; Redzich, M.; Zebrowski, M.; Emmerich, S.; Schnell, O. Implementation of HbA1c point of care testing in 3 German medical practices: Impact on workflow and physician, staff, and patient satisfaction. J. Diabetes Sci. Technol. 2018, 12, 687–694. [Google Scholar] [CrossRef]

| Parameter | All Patients | Teleretinal Imaging | p-Value | |
|---|---|---|---|---|
| Completed | Not Imaged | |||
| n | 4743 | 275 | 4468 | |
| Age (years) | ||||
| Mean (SD) | 66.8 (13.8) | 65.7 (13.0) | 66.9 (13.8) | 0.158 |
| Median | 68 | 66 | 68 | |
| Range | 18–100 | 22–97 | 18–100 | |
| Male, n (%) | 2756 (58.1) | 196 (71.3) | 2560 (57.3) | <0.001 |
| Race, n (%) | ||||
| White, Non-Hispanic | 3911 (82.5) | 211 (76.7) | 3700 (82.8) | 0.010 |
| Asian or Asian American | 441 (9.3) | 32 (11.6) | 409 (9.2) | 0.168 |
| Black or African American | 161 (3.4) | 15 (5.5) | 146 (3.3) | 0.053 |
| Hispanic or Latin American | 43 (0.9) | 2 (0.7) | 41 (0.9) | 0.747 |
| More than One Race | 26 (0.6) | 1 (0.4) | 25 (0.6) | 0.663 |
| Other Races or Ethnicities | 125 (2.6) | 12 (4.4) | 113 (2.5) | 0.066 |
| Missing | 36 (0.8) | 2 (0.7) | 34 (0.8) | 0.956 |
| Insurance Type, n (%) | ||||
| Commercial | 1767 (37.3) | 108 (39.3) | 1659 (37.1) | 0.476 |
| Medicare | 2511 (59.9) | 134 (48.7) | 2377 (53.2) | 0.150 |
| Medicaid | 437 (9.2) | 30 (10.9) | 407 (9.1) | 0.317 |
| Other † | 28 (0.6) | 3 (1.1) | 25 (0.6) | 0.266 |
| Distance to Clinic (mi) | ||||
| Mean (SD) | 18.71 (25.85) | 20.48 (28.02) | 18.60 (25.71) | 0.651 |
| Income by Zip Code ($K) | ||||
| Mean (SD) | 105.7 (61.2) | 104.3 (53.5) | 105.8 (61.6) | 0.851 |
| Smoking Status, n (%) | ||||
| Never | 2299 (48.5) | 140 (50.9) | 2159 (48.3) | 0.404 |
| Former | 1908 (40.2) | 105 (38.2) | 1803 (40.4) | 0.476 |
| Passive | 16 (0.3) | 0 (0) | 16 (0.4) | 0.319 |
| Current | 456 (9.6) | 27 (9.8) | 429 (9.6) | 0.904 |
| Missing | 64 (1.4) | 3 (1.1) | 61 (1.4) | 0.700 |
| Type 1 Diabetes, n (%) | 166 (3.5) | 5 (1.8) | 161 (3.6) | 0.118 |
| Biometric Factors, n (%) | ||||
| HbA1c Testing | 4380 (92.4) | 269 (97.8) | 4111 (92.0) | <0.001 |
| HbA1c < 8% | 3835 (82.4) | 210 (76.6) | 3625 (82.7) | 0.010 |
| HbA1c > 9% | 443 (9.3) | 29 (10.5) | 414 (9.3) | 0.479 |
| BP < 140/90 mmHg | 3373 (71.3) | 203 (73.8) | 3170 (71.2) | 0.349 |
| Microalbumin Testing | 3123 (65.8) | 238 (86.6) | 2885 (64.6) | <0.001 |
| LDL Testing | 3307 (69.7) | 218 (79.3) | 3089 (69.1) | <0.001 |
| LDL < 100 mg/dL | 2994 (71.0) | 176 (70.1) | 2818 (71.0) | 0.750 |
| BMI < 30 kg/m2 | 2185 (46.3) | 129 (47.3) | 2056 (46.3) | 0.754 |
| Diabetic Complications, n (%) | ||||
| Nephropathy | 569 (12.6) | 38 (13.8) | 558 (12.5) | 0.518 |
| Peripheral Neuropathy | 1811 (38.2) | 99 (36.0) | 1712 (38.3) | 0.444 |
| Parameter | β | Standard Error | Wald χ2 | OR | 95% CI | p-Value |
|---|---|---|---|---|---|---|
| Male Sex (relative to female) | 0.572 | 0.138 | 17.265 | 1.772 | 1.353–2.322 | <0.001 |
| Other Race/Ethnicity (relative to White) † | 0.351 | 0.150 | 5.474 | 1.420 | 1.059–1.905 | 0.019 |
| HbA1c < 8% | −0.346 | 0.150 | 5.301 | 0.708 | 0.527–0.950 | 0.021 |
| Completion of Biometric Testing | ||||||
| HbA1c | 0.577 | 0.441 | 1.711 | 1.781 | 0.750–4.229 | 0.191 |
| Microalbumin | 1.080 | 0.188 | 33.157 | 2.945 | 2.039–4.253 | <0.001 |
| LDL | 0.259 | 0.161 | 2.594 | 1.295 | 0.945–1.775 | 0.107 |
| Constant | −4.530 | 0.439 | 106.701 | 0.011 | <0.001 |
| Modality | Required Personnel | Annual Salary (USD in Thousands) | Hours Worked | Wage Per Hour (USD) | Time Required (Hours) | TDABC (USD) |
|---|---|---|---|---|---|---|
| In-person Eye Examination | Ophthalmologist | 299 | 1800 | 166 | 0.25 | 41.53 |
| Optometrist | 127 | 1800 | 71 | 0.25 | 17.64 | |
| Remote Screening Examination | Medical Assistant | N/A | 1800 | 17 | 0.20 | 3.40 |
| Image Grading | Ophthalmologist | 299 | 1800 | 166 | 0.03 | 4.98 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szulborski, K.J.; Gumustop, S.; Lasalle, C.C.; Hughes, K.; Roh, S.; Ramsey, D.J. Factors Associated with Utilization of Teleretinal Imaging in a Hospital-Based Primary Care Setting. Vision 2023, 7, 53. https://doi.org/10.3390/vision7030053
Szulborski KJ, Gumustop S, Lasalle CC, Hughes K, Roh S, Ramsey DJ. Factors Associated with Utilization of Teleretinal Imaging in a Hospital-Based Primary Care Setting. Vision. 2023; 7(3):53. https://doi.org/10.3390/vision7030053
Chicago/Turabian StyleSzulborski, Kira J., Selin Gumustop, Claudia C. Lasalle, Kate Hughes, Shiyoung Roh, and David J. Ramsey. 2023. "Factors Associated with Utilization of Teleretinal Imaging in a Hospital-Based Primary Care Setting" Vision 7, no. 3: 53. https://doi.org/10.3390/vision7030053
APA StyleSzulborski, K. J., Gumustop, S., Lasalle, C. C., Hughes, K., Roh, S., & Ramsey, D. J. (2023). Factors Associated with Utilization of Teleretinal Imaging in a Hospital-Based Primary Care Setting. Vision, 7(3), 53. https://doi.org/10.3390/vision7030053