Plasma Levels of Matrix Metalloprotease MMP-9 and Tissue Inhibitor TIMP-1 in Caucasian Patients with Polypoidal Choroidal Vasculopathy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Participant Recruitment and Data Collection
2.4. Quantification of Plasma MMP-9 and TIMP-1
2.5. Data Analysis and Statistics
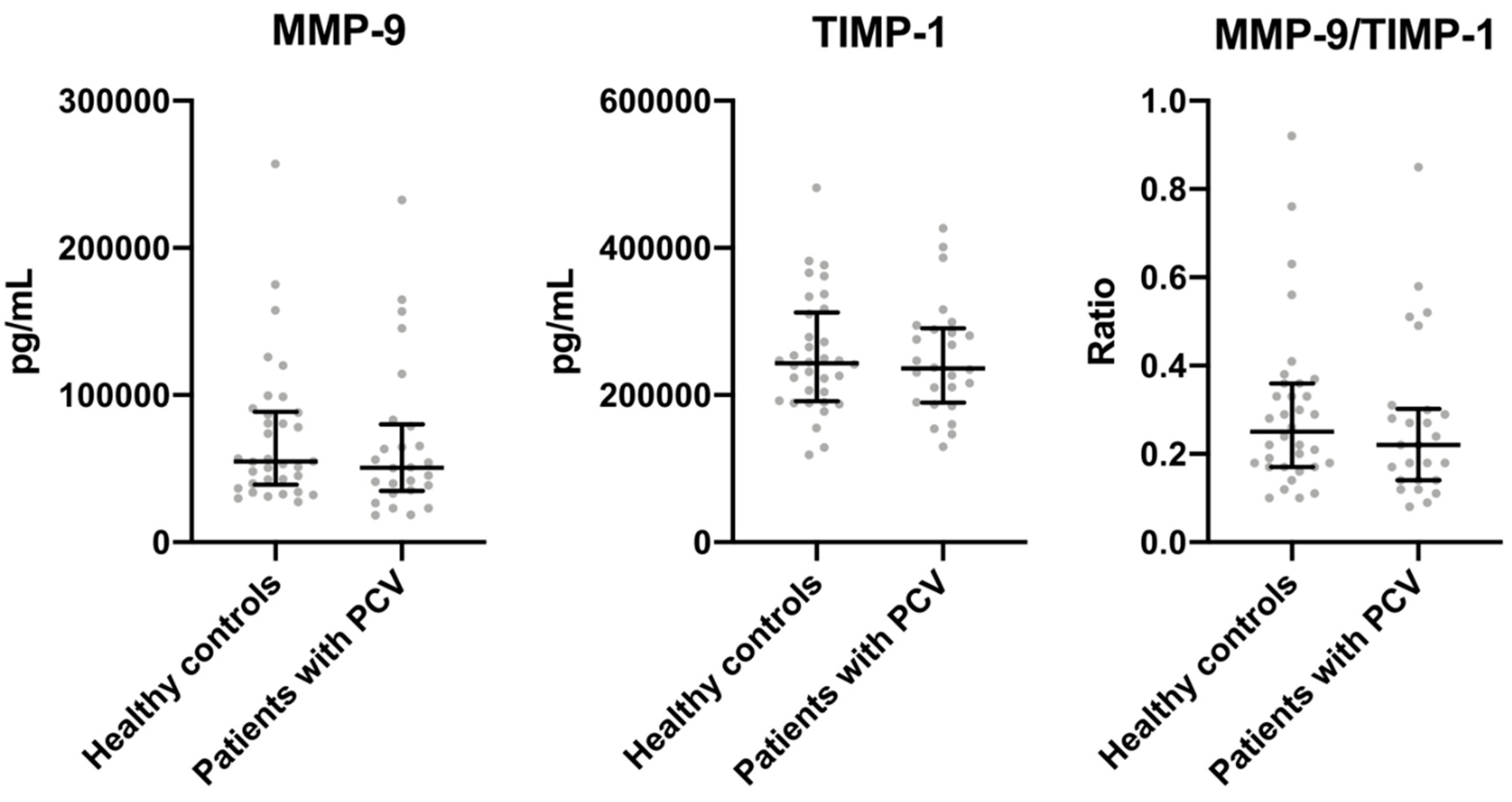
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Laude, A.; Cackett, P.D.; Vithana, E.N.; Yeo, I.Y.; Wong, D.; Koh, A.H.; Wong, T.Y.; Aung, T. Polypoidal choroidal vasculopathy and neovascular age-related macular degeneration: Same or different disease? Prog. Retin. Eye Res. 2010, 29, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Dansingani, K.K.; Gal-Or, O.; Sadda, S.R.; Yannuzzi, L.A.; Freund, K.B. Understanding aneurysmal type 1 neovascularization (polypoidal choroidal vasculopathy): A lesson in the taxonomy of ’expanded spectra’—A review. Clin. Exp. Ophthalmol. 2018, 46, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Kumawat, D.; Sundar, M.D.; Gagrani, M.; Gupta, B.; Roop, P.; Hasan, N.; Sharma, A.; Chawla, R. Polypoidal choroidal vasculopathy: A comprehensive clinical update. Ther. Adv. Ophthalmol. 2019, 11. [Google Scholar] [CrossRef]
- van Dijk, E.H.C.; van Rijssen, T.J.; Subhi, Y.; Boon, C.J.F. Photodynamic Therapy for Chorioretinal Diseases: A Practical Approach. Ophthalmol. Ther. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lorentzen, T.D.; Subhi, Y.; Sørensen, T.L. PREVALENCE OF POLYPOIDAL CHOROIDAL VASCULOPATHY IN WHITE PATIENTS WITH EXUDATIVE AGE-RELATED MACULAR DEGENERATION: Systematic Review and Meta-Analysis. Retina 2018, 38, 2363–2371. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.W.; Wong, T.Y.; Cheung, C.M. Polypoidal Choroidal Vasculopathy in Asians. J. Clin. Med. 2015, 4, 782–821. [Google Scholar] [CrossRef]
- Sho, K.; Takahashi, K.; Yamada, H.; Wada, M.; Nagai, Y.; Otsuji, T.; Nishikawa, M.; Mitsuma, Y.; Yamazaki, Y.; Matsumura, M.; et al. Polypoidal choroidal vasculopathy: Incidence, demographic features, and clinical characteristics. Arch. Ophthalmol. 2003, 121, 1392–1396. [Google Scholar] [CrossRef] [Green Version]
- Kikushima, W.; Sakurada, Y.; Sugiyama, A.; Tanabe, N.; Kume, A.; Iijima, H. Comparison of initial treatment between 3-monthly intravitreal aflibercept monotherapy and combined photodynamic therapy with single intravitreal aflibercept for polypoidal choroidal vasculopathy. Graefe’s Arch. Clin. Exp. Ophthalmol. 2017, 255, 311–316. [Google Scholar] [CrossRef]
- Lee, J.E.; Shin, J.P.; Kim, H.W.; Chang, W.; Kim, Y.C.; Lee, S.J.; Chung, I.Y.; Lee, J.E. VAULT study group Efficacy of fixed-dosing aflibercept for treating polypoidal choroidal vasculopathy: 1-year results of the VAULT study. Graefe’s Arch. Clin. Exp. Ophthalmol. 2017, 255, 493–502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gharehbagh, S.S.; Subhi, Y.; Sørensen, T.L. Efficacy of aflibercept for polypoidal choroidal vasculopathy in Caucasians. Acta Ophthalmol. 2018, 96, e94–e95. [Google Scholar] [CrossRef] [Green Version]
- Kondo, N.; Honda, S.; Ishibashi, K.; Tsukahara, Y.; Negi, A. Elastin gene polymorphisms in neovascular age-related macular degeneration and polypoidal choroidal vasculopathy. Investig. Ophthalmol. Vis. Sci. 2008, 49, 1101–1105. [Google Scholar] [CrossRef] [PubMed]
- Yamashiro, K.; Mori, K.; Nakata, I.; Tsuchihashi, T.; Horie-Inoue, K.; Nakanishi, H.; Tsujikawa, A.; Saito, M.; Iida, T.; Yamada, R.; et al. Association of elastin gene polymorphism to age-related macular degeneration and polypoidal choroidal vasculopathy. Investig. Ophthalmol. Vis. Sci. 2011, 52, 8780–8784. [Google Scholar] [CrossRef] [PubMed]
- Lima, L.H.; Merriam, J.E.; Freund, K.B.; Barbazetto, I.A.; Spaide, R.F.; Yannuzzi, L.A.; Allikmets, R. Elastin rs2301995 polymorphism is not associated with polypoidal choroidal vasculopathy in caucasians. Ophthalmic Genet. 2011, 32, 80–82. [Google Scholar] [CrossRef]
- Zeng, R.; Wen, F.; Zhang, X.; Su, Y. Serum levels of matrix metalloproteinase 2 and matrix metalloproteinase 9 elevated in polypoidal choroidal vasculopathy but not in age-related macular degeneration. Mol. Vis. 2013, 19, 729–736. [Google Scholar] [PubMed]
- Lorentzen, T.D.; Subhi, Y.; Sørensen, T.L. Presenting characteristics and prevalence of polypoidal choroidal vasculopathy in Scandinavian patients with treatment-naïve exudative age-related macular degeneration. Acta Ophthalmol. 2018, 96, 475–480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rifai, N.; Ridker, P.M. Proposed cardiovascular risk assessment algorithm using high-sensitivity C-reactive protein and lipid screening. Clin. Chem. 2001, 47, 28–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Subhi, Y.; Sørensen, T.L. Physical activity patterns in patients with early and late age-related macular degeneration. Dan. Med. J. 2016, 63, A5303. [Google Scholar]
- Kumar, S.; Nakashizuka, H.; Jones, A.; Lambert, A.; Zhao, X.; Shen, M.; Parker, M.; Wang, S.; Berriochoa, Z.; Fnu, A.; et al. Proteolytic Degradation and Inflammation Play Critical Roles in Polypoidal Choroidal Vasculopathy. Am. J. Pathol. 2017, 187, 2841–2857. [Google Scholar] [CrossRef] [Green Version]
- Okubo, A.; Sameshima, M.; Uemura, A.; Kanda, S.; Ohba, N. Clinicopathological correlation of polypoidal choroidal vasculopathy revealed by ultrastructural study. Br. J. Ophthalmol. 2002, 86, 1093–1098. [Google Scholar] [CrossRef] [Green Version]
- Lafaut, B.A.; Aisenbrey, S.; Van den Broecke, C.; Bartz-Schmidt, K.U.; Heimann, K. Polypoidal choroidal vasculopathy pattern in age-related macular degeneration: A clinicopathologic correlation. Retina 2000, 20, 650–654. [Google Scholar] [CrossRef]
- Moussa, K.; Bloomer, M.M.; Schwartz, D.M.; Pan, C.K.; Toy, B.C.; Crawford, J.B.; Afshar, A.R. POLYPOIDAL CHOROIDAL VASCULOPATHY: A CLINICOPATHOLOGIC STUDY. Retin. Cases Brief Rep. Winter 2017, 11 (Suppl. 1), S128–S131. [Google Scholar] [CrossRef] [PubMed]
- Nakashizuka, H.; Mitsumata, M.; Okisaka, S.; Shimada, H.; Kawamura, A.; Mori, R.; Yuzawa, M. Clinicopathologic findings in polypoidal choroidal vasculopathy. Investig. Ophthalmol. Vis. Sci. 2008, 49, 4729–4737. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tso, M.O.M.; Suarez, M.J.; Eberhart, C.G. Pathologic study of early manifestations of polypoidal choroidal vasculopathy and pathogenesis of choroidal neovascularization. Am. J. Ophthalmol. Case. Rep. 2017, 11, 176–180. [Google Scholar] [CrossRef] [PubMed]
- Subhi, Y.; Krogh Nielsen, M.; Molbech, C.R.; Oishi, A.; Singh, A.; Nissen, M.H.; Sørensen, T.L. Polypoidal Choroidal Vasculopathy Associate With Diminished Regulatory T Cells That Are Polarized Into a T Helper 2-Like Phenotype. Investig. Ophthalmol. Vis. Sci. 2019, 60, 2583–2590. [Google Scholar] [CrossRef] [Green Version]
- Subhi, Y.; Krogh Nielsen, M.; Molbech, C.R.; Oishi, A.; Singh, A.; Nissen, M.H.; Sørensen, T.L. CD11b and CD200 on Circulating Monocytes Differentiate Two Angiographic Subtypes of Polypoidal Choroidal Vasculopathy. Investig. Ophthalmol. Vis. Sci. 2017, 58, 5242–5250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Subhi, Y.; Krogh Nielsen, M.; Molbech, C.R.; Sørensen, T.L. Altered proportion of CCR2+ and CX3CR1+ circulating monocytes in neovascular age-related macular degeneration and polypoidal choroidal vasculopathy. Clin. Exp. Ophthalmol. 2018, 46, 661–669. [Google Scholar] [CrossRef]
- Subhi, Y.; Krogh Nielsen, M.; Molbech, C.R.; Krüger Falk, M.; Singh, A.; Hviid, T.V.F.; Nissen, M.H.; Sørensen, T.L. Association of CD11b+ Monocytes and Anti-Vascular Endothelial Growth Factor Injections in Treatment of Neovascular Age-Related Macular Degeneration and Polypoidal Choroidal Vasculopathy. JAMA Ophthalmol. 2019, 137, 515–522. [Google Scholar] [CrossRef]
- Subhi, Y.; Krogh Nielsen, M.; Molbech, C.R.; Oishi, A.; Singh, A.; Nissen, M.H.; Sørensen, T.L. Plasma markers of chronic low-grade inflammation in polypoidal choroidal vasculopathy and neovascular age-related macular degeneration. Acta Ophthalmol. 2019, 97, 99–106. [Google Scholar] [CrossRef] [Green Version]
- Subhi, Y.; Nielsen, M.K.; Molbech, C.R.; Liisborg, C.; Søndergaard, H.B.; Sellebjerg, F.; Sørensen, T.L. The transcriptome of peripheral blood mononuclear cells in patients with clinical subtypes of late age-related macular degeneration. Immun. Ageing 2019, 16, 20. [Google Scholar] [CrossRef]
- Thrailkill, K.; Cockrell, G.; Simpson, P.; Moreau, C.; Fowlkes, J.; Bunn, R.C. Physiological matrix metalloproteinase (MMP) concentrations: Comparison of serum and plasma specimens. Clin. Chem. Lab. Med. 2006, 44, 503–504. [Google Scholar] [CrossRef] [Green Version]
- Jung, K. Serum or plasma: What kind of blood sample should be used to measure circulating matrix metalloproteinases and their inhibitors? J. Neuroimmunol. 2005, 162, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Mannello, F.; Jung, K.; Tonti, G.A.; Canestrari, F. Heparin affects matrix metalloproteinases and tissue inhibitors of metalloproteinases circulating in peripheral blood. Clin. Biochem. 2008, 41, 1466–1473. [Google Scholar] [CrossRef] [PubMed]
- Mannello, F.; Tonti, G.A. Gelatinase concentrations and zymographic profiles in human breast cancer: Matrix metalloproteinases circulating in plasma are better markers for the subclassification and early prediction of cancer: The coagulation/fibrinolysis pathways alter the release, activation and recovery of different gelatinases in serum. Int. J. Cancer 2007, 121, 216–218. [Google Scholar] [CrossRef] [PubMed]
- Nascimento Dda, C.; Durigan Rde, C.; Tibana, R.A.; Durigan, J.L.; Navalta, J.W.; Prestes, J. The response of matrix metalloproteinase-9 and -2 to exercise. Sports Med. 2015, 45, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Subhi, Y.; Singh, A.; Falk, M.K.; Sørensen, T.L. In patients with neovascular age-related macular degeneration, physical activity may influence C-reactive protein levels. Clin. Ophthalmol. 2014, 8, 15–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Characteristics | Patients with PCV (n = 26) | Healthy Controls (n = 34) | p-Value |
|---|---|---|---|
| Age, years, mean (SD) | 72 (7) | 74 (8) | 0.4 † |
| Gender, males:females, n | 11:15 | 15:19 | 0.9 ‡ |
| Cardiovascular disease, n (%) | 5 (19) | 5 (15) | 0.6 ‡ |
| Hypertension, n (%) | 10 (39) | 11 (32) | 0.6 ‡ |
| Hypercholesterolemia, n (%) | 9 (35) | 12 (35) | 1.0 ‡ |
| Type 2 diabetes mellitus, n (%) | 3 (12) | 0 (0) | 0.08 § |
| Alcohol consumption, units, median (IQR) | 4 (1 to 13) | 4 (2 to 7) | 0.8 ¶ |
| Body mass index, mean (SD) | 25 (4) | 25 (3) | 1.0 † |
| Physically active, n (%) | 14 (54) | 22 (65) | 0.4 ‡ |
| Smoking, current:previous:never, n | 8:15:3 | 5:15:14 | 0.03 § |
| MMP-9 | TIMP-1 | MMP-9/TIMP-1 Ratio | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Univariate OR; CI95% | p-Value | Multivariate OR; CI95% | p-Value | Univariate OR; CI95% | p-Value | Multivariate OR; CI95% | p-Value | Univariate OR; CI95% | p-Value | |
| Retinal diagnosis | ||||||||||
| PCV | 0.65; 0.27–1.59 | 0.3 | 0.66; 0.27–1.61 | 0.4 | 0.93; 0.38–2.25 | 0.9 | 1.28; 0.52–3.11 | 0.6 | 0.67; 0.28–1.63 | 0.4 |
| Healthy | Ref. | Ref. | Ref. | Ref. | Ref. | |||||
| Participant characteristics included as co-variates | ||||||||||
| Age | 0.95; 0.99–1.12 | 0.09 | 1.15; 1.08–1.23 | <0.001 | 1.16; 1.08–1.24 | <0.001 | 0.99; 0.94–1.05 | 0.7 | ||
| Gender | ||||||||||
| Female | 0.36; 0.15–0.90 | 0.03 | 0.36; 0.14–0.90 | 0.03 | 0.48; 0.20–1.19 | 0.1 | 0.61; 0.25–1.49 | 0.3 | ||
| Male | Ref. | Ref. | Ref. | Ref. | ||||||
| Alcohol | 1.00; 0.94–1.06 | 0.9 | 0.97; 0.92–1.03 | 0.4 | 0.99; 0.93–1.05 | 0.8 | ||||
| BMI | 1.02; 0.90–1.14 | 0.8 | 1.08; 0.96–1.22 | 0.2 | 0.97; 0.86–2.41 | 0.6 | ||||
| PA | 1.03; 0.42–2.52 | 0.9 | 0.79; 0.32–1.93 | 0.6 | 1.01; 0.41–2.46 | 1.0 | ||||
| Smoking | ||||||||||
| Current | 1.84; 0.52–6.48 | 0.3 | 0.84; 0.24–2.92 | 0.8 | 1.94; 0.55–6.86 | 0.3 | ||||
| Previous | 1.65; 0.59–4.66 | 0.3 | 1.95; 0.69–5.52 | 0.2 | 0.99; 0.35–2.79 | 1.0 | ||||
| Never | Ref. | Ref. | Ref. | |||||||
| CVD | 1.14; 0.35–3.69 | 0.8 | 0.55; 0.17–1.79 | 0.3 | 1.52; 0.47–4.94 | 0.5 | ||||
| HT | 0.81; 0.32–2.02 | 0.6 | 1.59; 0.63–4.02 | 0.3 | 0.56; 0.22–1.42 | 0.2 | ||||
| HC | 0.76; 0.30–1.92 | 0.6 | 0.49; 0.19–1.26 | 0.1 | 1.15; 0.46–2.88 | 0.8 | ||||
| T2DM | 0.94; 0.13–7.02 | 1.0 | 3.13; 0.41–23.8 | 0.3 | 0.46; 0.06–3.47 | 0.5 | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sørensen, J.Ø.; Subhi, Y.; Molbech, C.R.; Krogh Nielsen, M.; Sørensen, T.L. Plasma Levels of Matrix Metalloprotease MMP-9 and Tissue Inhibitor TIMP-1 in Caucasian Patients with Polypoidal Choroidal Vasculopathy. Vision 2020, 4, 27. https://doi.org/10.3390/vision4020027
Sørensen JØ, Subhi Y, Molbech CR, Krogh Nielsen M, Sørensen TL. Plasma Levels of Matrix Metalloprotease MMP-9 and Tissue Inhibitor TIMP-1 in Caucasian Patients with Polypoidal Choroidal Vasculopathy. Vision. 2020; 4(2):27. https://doi.org/10.3390/vision4020027
Chicago/Turabian StyleSørensen, Jakob Ø., Yousif Subhi, Christopher R. Molbech, Marie Krogh Nielsen, and Torben L. Sørensen. 2020. "Plasma Levels of Matrix Metalloprotease MMP-9 and Tissue Inhibitor TIMP-1 in Caucasian Patients with Polypoidal Choroidal Vasculopathy" Vision 4, no. 2: 27. https://doi.org/10.3390/vision4020027
APA StyleSørensen, J. Ø., Subhi, Y., Molbech, C. R., Krogh Nielsen, M., & Sørensen, T. L. (2020). Plasma Levels of Matrix Metalloprotease MMP-9 and Tissue Inhibitor TIMP-1 in Caucasian Patients with Polypoidal Choroidal Vasculopathy. Vision, 4(2), 27. https://doi.org/10.3390/vision4020027






