Development and Validation of the Short Form (JAEN-10) of the Joint Assessment of Equilibrium and Neuromotor Status Scale (JAEN-20)
Abstract
1. Introduction
2. Materials and Methods
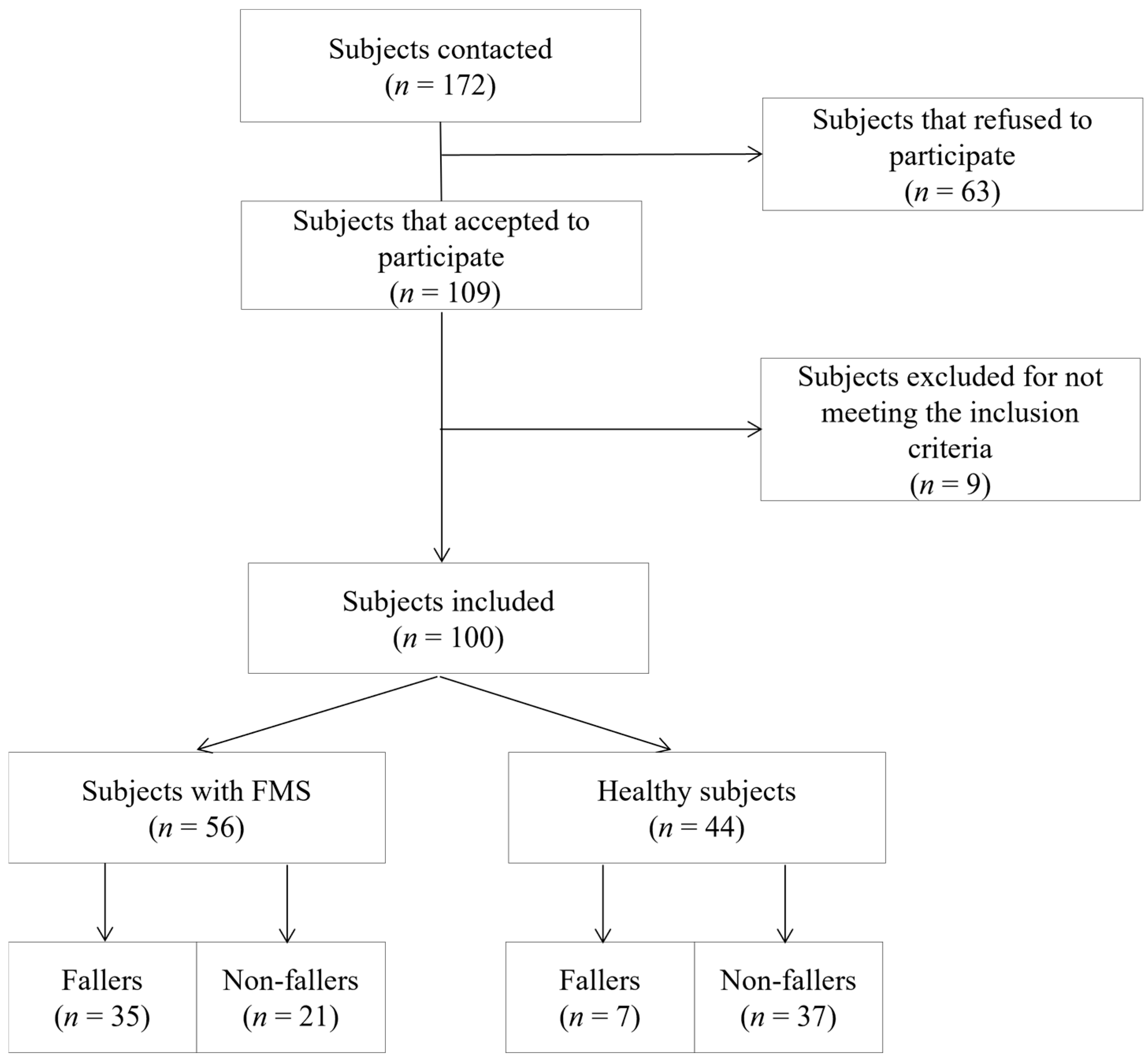
2.1. Study and Sample
2.2. Measurements
2.3. Items Reduction Procedure
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bennett, R.M. Emerging Concepts in the Neurobiology of Chronic Pain: Evidence of Abnormal Sensory Processing in Fibromyalgia. Mayo Clin. Proc. 1999, 74, 385–398. [Google Scholar] [CrossRef] [PubMed]
- Sarıhan, K.; Uzkeser, H.; Erdal, A. Evaluation of balance, fall risk, and related factors in patients with fibromyalgia syndrome. Turk. J. Phys. Med. Rehabil. 2021, 67, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.D.; Horak, F.B.; Winters-Stone, K.; Irvine, J.M.; Bennett, R.M. Fibromyalgia Is Associated With Impaired Balance and Falls. JCR J. Clin. Rheumatol. 2009, 15, 16–21. [Google Scholar] [CrossRef]
- Meireles, S.A.; Antero, D.C.; Kulczycki, M.M.; Skare, T.L. Prevalence of falls in fibromyalgia patients. Acta Ortop. Bras. 2014, 22, 163–166. [Google Scholar] [CrossRef]
- Pérez-De-Heredia-Torres, M.; Huertas-Hoyas, E.; Martínez-Piédrola, R.; Palacios-Ceña, D.; Alegre-Ayala, J.; Santamaría-Vázquez, M.; Fernández-De-Las-Peñas, C. Balance deficiencies in women with fibromyalgia assessed using computerised dynamic posturography: A cross-sectional study in Spain. BMJ Open 2017, 7, e016239. [Google Scholar] [CrossRef]
- Serrador, J.M.; Quigley, K.S.; Zhao, C.; Findley, T.; Natelson, B.H. Balance deficits in Chronic Fatigue Syndrome with and without fibromyalgia. NeuroRehabilitation 2018, 42, 235–246. [Google Scholar] [CrossRef]
- Reddy, R.S.; Tedla, J.S.; Dixit, S.; Raizah, A.; Al-Otaibi, M.L.; Gular, K.; Ahmad, I.; Sirajudeen, M.S. Cervical Joint Position Sense and Its Correlations with Postural Stability in Subjects with Fibromyalgia Syndrome. Life 2022, 12, 1817. [Google Scholar] [CrossRef]
- Demir-Göçmen, D.; Altan, L.; Korkmaz, N.; Arabacı, R. Effect of supervised exercise program including balance exercises on the balance status and clinical signs in patients with fibromyalgia. Rheumatol. Int. 2012, 33, 743–750. [Google Scholar] [CrossRef]
- Duruturk, N.; Tuzun, E.H.; Culhaoglu, B. Is balance exercise training as effective as aerobic exercise training in fibromyalgia syndrome? Rheumatol. Int. 2014, 35, 845–854. [Google Scholar] [CrossRef]
- Peinado-Rubia, A.B.; Osuna-Pérez, M.C.; Cortés-Pérez, I.; Rojas-Navarrete, A.; Ibancos-Losada, M.d.R.; Lomas-Vega, R. Effectiveness of Vestibular Rehabilitation in Improving Health Status and Balance in Patients with Fibromyalgia Syndrome: A Single-Blind Randomized Controlled Trial. Biomedicines 2023, 11, 1297. [Google Scholar] [CrossRef]
- Kasapoğlu Aksoy, M.; Altan, L.; Ökmen Metin, B. The relationship between balance and vitamin 25(OH)D in fibromyalgia patients. Mod. Rheumatol. 2016, 27, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Ulus, Y.; Akyol, Y.; Tander, B.; Durmuş, D.; Bilgici, A.; Ömer, K.U. Is There a Balance Problem in Hypermobile Patients with Fibromyalgia? Turk. J. Rheumatol. 2013, 28, 10–15. [Google Scholar] [CrossRef]
- Ulus, Y.; Akyol, Y.; Tander, B.; Bilgici, A.; Kuru, O. Knee Proprioception and Balance in Turkish Women With and Without Fibromyalgia Syndrome. Turk. J. Phys. Med. Rehabil. 2013, 59, 128–132. [Google Scholar] [CrossRef]
- Lomas-Vega, R.; Rodríguez-Almagro, D.; Peinado-Rubia, A.B.; Zagalaz-Anula, N.; Molina, F.; Obrero-Gaitán, E.; Ibáñez-Vera, A.J.; Osuna-Pérez, M.C. Joint Assessment of Equilibrium and Neuromotor Function: A Validation Study in Patients with Fibromyalgia. Diagnostics 2020, 10, 1057. [Google Scholar] [CrossRef] [PubMed]
- Carrasco-Vega, E.; Martínez-Moya, M.; Barni, L.; Guiducci, S.; Nacci, F.; Gonzalez-Sanchez, M. Questionnaires for the subjective evaluation of patients with fibromyalgia: A systematic review. Eur. J. Phys. Rehabil. Med. 2023, 59, 353–363. [Google Scholar] [CrossRef]
- Hobart, J.C.; Cano, S.J.; Warner, T.T.; Thompson, A.J. What sample sizes for reliability and validity studies in neurology? J. Neurol. 2012, 259, 2681–2694. [Google Scholar] [CrossRef]
- Salgueiro, M.; García-Leiva, J.M.; Ballesteros, J.; Hidalgo, J.; Molina, R.; Calandre, E.P. Validation of a Spanish version of the Revised Fibromyalgia Impact Questionnaire (FIQR). Health Qual. Life Outcomes 2013, 11, 132. [Google Scholar] [CrossRef]
- Vilagut, G.; Valderas, J.M.; Ferrer, M.; Garin, O.; López-García, E.; Alonso, J. Interpretation of SF-36 and SF-12 questionnaires in Spain: Physical and mental components. Med. Clin. 2008, 130, 726–735. [Google Scholar] [CrossRef]
- Pérez, N.; Garmendia, I.; García-Granero, M.; Martin, E.; García-Tapia, R. Factor analysis and correlation between Dizziness Handicap Inventory and Dizziness Characteristics and Impact on Quality of Life Scales. Acta Oto-Laryngol. 2001, 545, 145–154. [Google Scholar] [CrossRef]
- Montilla-Ibáñez, A.; Martínez-Amat, A.; Lomas-Vega, R.; Cruz-Díaz, D.; De la Torre-Cruz, M.J.; Casuso-Pérez, R.; Hita-Contreras, F. The Activities-specific Balance Confidence scale: Reliability and validity in Spanish patients with vestibular disorders. Disabil. Rehabil. 2016, 39, 697–703. [Google Scholar] [CrossRef]
- Lomas-Vega, R.; Hita-Contreras, F.; Mendoza, N.; Martínez-Amat, A. Cross-cultural adaptation and validation of the Falls Efficacy Scale International in Spanish postmenopausal women. Menopause 2012, 19, 904–908. [Google Scholar] [CrossRef] [PubMed]
- Lamb, S.E.; Jørstad-Stein, E.C.; Hauer, K.; Becker, C. Development of a Common Outcome Data Set for Fall Injury Prevention Trials: The Prevention of Falls Network Europe Consensus. J. Am. Geriatr. Soc. 2005, 53, 1618–1622. [Google Scholar] [CrossRef] [PubMed]
- Moreira, N.B.; Bento, P.C.B.; Vieira, E.; da Silva, J.L.P.; Rodacki, A.L.F. Comparison of the Clinical-Functional Vulnerability Index and the frailty phenotype for the identification of falls in older individuals: A cross-sectional study. Ann. Phys. Rehabil. Med. 2022, 66, 101675. [Google Scholar] [CrossRef] [PubMed]
- Cortina, J.M. What Is Coefficient Alpha? An Examination of Theory and Applications. J. Appl. Psychol. 1993, 78, 98–104. [Google Scholar] [CrossRef]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef]
- Karna, D.K.; Mishra, C.; Dash, S.K.; Acharya, A.P.; Panda, S.; Chinnareddyvari, C.S. Exploring body morphometry and weight prediction in Ganjam goats in India through principal component analysis. Trop. Anim. Health Prod. 2024, 56, 298. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988. [Google Scholar]
- Zweig, M.H.; Campbell, G. Receiver-operating characteristic (ROC) plots: A fundamental evaluation tool in clinical medicine. Clin. Chem. 1993, 39, 561–577. [Google Scholar] [CrossRef]
- Jones, L.W.; Kwan, M.L.; Weltzien, E.; Chandarlapaty, S.; Sternfeld, B.; Sweeney, C.; Bernard, P.S.; Castillo, A.; Habel, L.A.; Kroenke, C.H.; et al. Exercise and Prognosis on the Basis of Clinicopathologic and Molecular Features in Early-Stage Breast Cancer: The LACE and Pathways Studies. Cancer Res. 2016, 76, 5415–5422. [Google Scholar] [CrossRef]
| Variables | Healthy | n = 44 | FMS | n = 56 | p-Value |
|---|---|---|---|---|---|
| Statistics | Mean | SD | Mean | SD | t-test |
| Age | 61.00 | 10.69 | 57.75 | 7.61 | 0.082 |
| Height | 1.60 | 0.06 | 1.60 | 0.06 | 0.665 |
| Weight | 68.18 | 10.45 | 73.70 | 14.78 | 0.052 |
| Body Mass Index | 26.91 | 4.35 | 28.68 | 5.25 | 0.093 |
| Years since diagnosis | 14.00 | 9.28 | |||
| Falls in the last year | 0.55 | 2.33 | 1.23 | 1.25 | 0.062 |
| Physical Component Summary SF-12 | 49.35 | 8.67 | 30.74 | 5.81 | <0.001 |
| Mental Component Summary SF-12 | 47.04 | 9.89 | 32.86 | 10.26 | <0.001 |
| Dizziness Handicap Inventory Emotional | 2.73 | 5.96 | 15.11 | 8.29 | <0.001 |
| Dizziness Handicap Inventory Functional | 5.09 | 7.92 | 18.98 | 8.88 | <0.001 |
| Dizziness Handicap Inventory Physical | 7.50 | 8.25 | 19.27 | 5.36 | <0.001 |
| Dizziness Handicap Inventory Total Score | 15.32 | 19.38 | 53.36 | 20.47 | <0.001 |
| Activities Balance Confidence Scale | 85.15 | 13.42 | 58.19 | 22.55 | <0.001 |
| Falls Efficacy Scale | 22.12 | 6.05 | 34.46 | 10.78 | <0.001 |
| Mean of the Scale If the Element Is Deleted | Scale Variance If the Element Is Removed | Corrected Total Element Correlation | Multiple Squared Correlation | Cronbach’s Alpha If Element Is Deleted | |
|---|---|---|---|---|---|
| Romberg test | 13.08 | 48.499 | 0.505 | 0.341 | 0.903 |
| One Leg Left (Eyes Closed) | 10.80 | 51.253 | 0.289 | 0.470 | 0.914 |
| One Leg Right (Eyes Closed) | 10.76 | 50.406 | 0.365 | 0.478 | 0.910 |
| Rotational head shaking test (Eyes Closed) | 13.31 | 43.792 | 0.803 | 0.773 | 0.885 |
| Head shaking test on the left-right diagonal (Eyes Open) | 13.26 | 42.699 | 0.808 | 0.859 | 0.884 |
| Head shaking test on the left-right diagonal (Eyes Closed) | 13.01 | 42.050 | 0.820 | 0.819 | 0.883 |
| Head shaking test on the right-left diagonal (Eyes Open) | 13.24 | 43.134 | 0.820 | 0.866 | 0.884 |
| Head shaking test on the right-left diagonal (Eyes Closed) | 13.15 | 42.412 | 0.853 | 0.878 | 0.881 |
| Walk Shaking Neck Flexion (Eyes Open) | 13.06 | 46.097 | 0.664 | 0.675 | 0.894 |
| Walk Shaking Neck Rotation (Eyes Open) | 12.69 | 45.772 | 0.617 | 0.649 | 0.897 |
| Component | Initial Eigenvalues | Sums of the Squared Saturations of the Extraction | Sum of the Squared Saturations of the Rotation | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | % of Variance | % Accumulated | Total | % of Variance | % Accumulated | Total | % of Variance | % Accumulated | |
| 1 | 5.552 | 55.524 | 55.524 | 5.552 | 55.524 | 55.524 | 5.162 | 51.624 | 51.624 |
| 2 | 1.684 | 16.839 | 72.363 | 1.684 | 16.839 | 72.363 | 2.074 | 20.739 | 72.363 |
| 3 | 0.968 | 9.678 | 82.040 | ||||||
| 4 | 0.622 | 6.221 | 88.262 | ||||||
| 5 | 0.346 | 3.456 | 91.718 | ||||||
| 6 | 0.254 | 2.536 | 94.254 | ||||||
| 7 | 0.211 | 2.114 | 96.368 | ||||||
| 8 | 0.179 | 1.790 | 98.158 | ||||||
| 9 | 0.117 | 1.165 | 99.323 | ||||||
| 10 | 0.068 | 0.677 | 100.000 | ||||||
| Component | ||
|---|---|---|
| 1 | 2 | |
| Romberg test | 0.578 | |
| One Leg Left (Eyes Closed) | 0.874 | |
| One Leg Right (Eyes Closed) | 0.874 | |
| Rotational head shaking test (Eyes Closed) | 0.893 | |
| Head shaking test on the left-right diagonal (Eyes Open) | 0.920 | |
| Head shaking test on the left-right diagonal (Eyes Closed) | 0.889 | |
| Head shaking test on the right-left diagonal (Eyes Open) | 0.917 | |
| Head shaking test on the right-left diagonal (Eyes Closed) | 0.926 | |
| Walk Shaking Neck Flexion (Eyes Open) | 0.682 | |
| Walk Shaking Neck Rotation (Eyes Open) | 0.636 | |
| JAEN 10-ITEMS | JAEN 20-ITEMS | |||
|---|---|---|---|---|
| r Pearson | Correlation | r Pearson | Correlation | |
| Fibromyalgia Impact Questionnaire | 0.398 | Moderate | 0.450 | Moderate |
| Physical Component Summary of SF-12 | −0.658 | Strong | −0.653 | Strong |
| Mental Component Summary SF-12 | −0.441 | Moderate | −0.439 | Moderate |
| Dizziness Handicap Inventory emotional | 0.599 | Strong | 0.576 | Strong |
| Dizziness Handicap Inventory functional | 0.662 | Strong | 0.652 | Strong |
| Dizziness Handicap Inventory physical | 0.687 | Strong | 0.704 | Strong |
| Dizziness Handicap Inventory Total Score | 0.695 | Strong | 0.689 | Strong |
| Activities Balance Confidence Scale | −0.542 | Strong | −0.607 | Strong |
| Falls Efficacy Scale International | 0.532 | Strong | 0.547 | Strong |
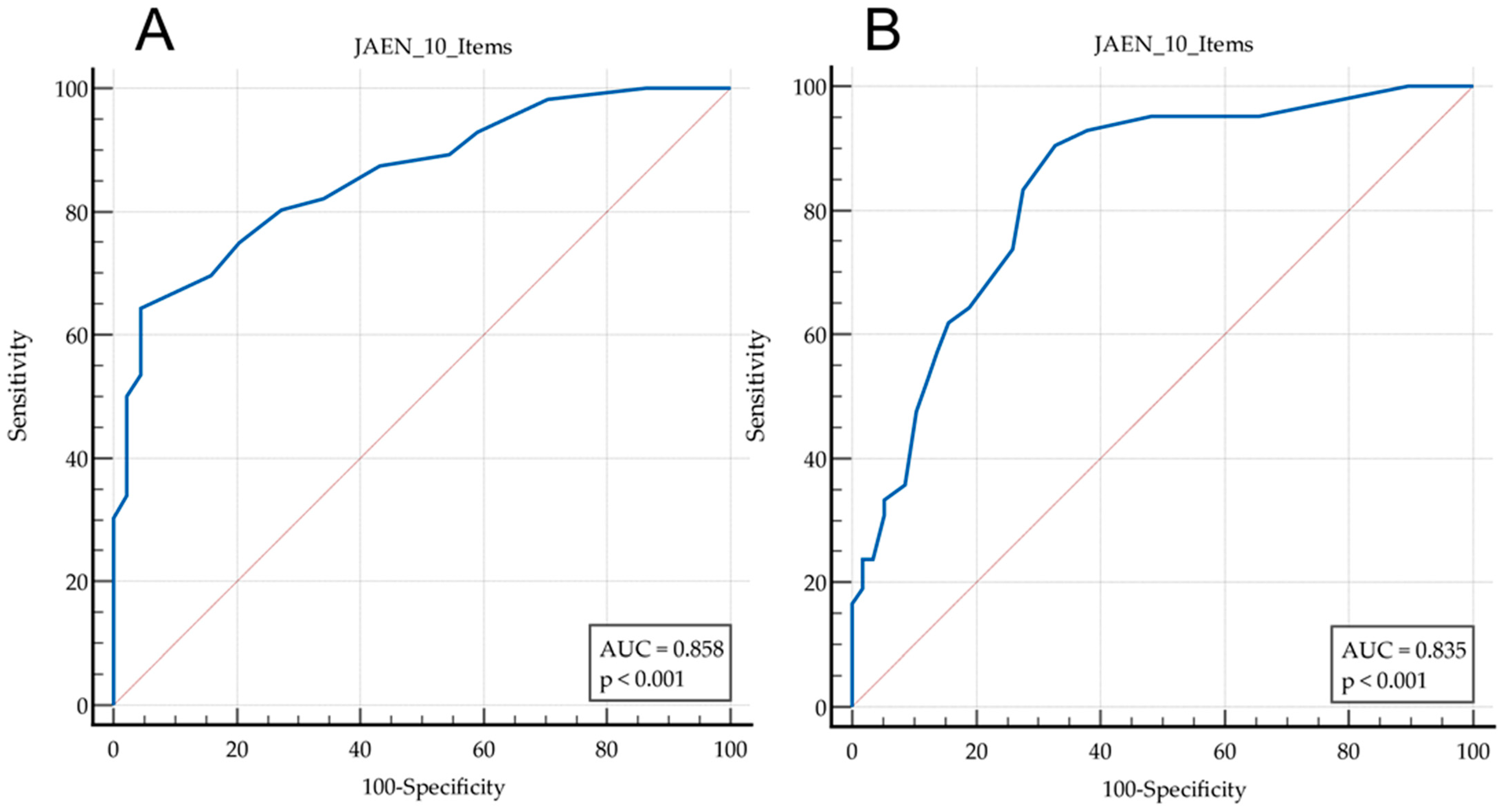
| Diagnostic | Criterion | Sen | 95% CI | Spe | 95% CI | +LR | 95% CI | −LR | 95% CI | +PV | 95% CI | −PV | 95% CI |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fibromyalgia | >14 | 64.29 | (50.4–76.6) | 95.45 | (84.5–99.4) | 14.14 | (3.60–55.55) | 0.37 | (0.26–0.53) | 94.7 | (82.1–98.6) | 67.7 | (59.5–75.0) |
| Falls | >11 | 90.48 | (77.4–97.3) | 67.24 | (53.7–79.0) | 2.76 | (1.89–4.04) | 0.14 | (0.055–0.37) | 66.7 | (57.7–74.5) | 90.7 | (79.1–96.2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peinado-Rubia, A.B.; Osuna-Pérez, M.C.; Núñez-Fuentes, D.; Rodríguez-Almagro, D.; Zagalaz-Anula, N.; Lomas-Vega, R. Development and Validation of the Short Form (JAEN-10) of the Joint Assessment of Equilibrium and Neuromotor Status Scale (JAEN-20). J. Funct. Morphol. Kinesiol. 2024, 9, 223. https://doi.org/10.3390/jfmk9040223
Peinado-Rubia AB, Osuna-Pérez MC, Núñez-Fuentes D, Rodríguez-Almagro D, Zagalaz-Anula N, Lomas-Vega R. Development and Validation of the Short Form (JAEN-10) of the Joint Assessment of Equilibrium and Neuromotor Status Scale (JAEN-20). Journal of Functional Morphology and Kinesiology. 2024; 9(4):223. https://doi.org/10.3390/jfmk9040223
Chicago/Turabian StylePeinado-Rubia, Ana Belén, María Catalina Osuna-Pérez, David Núñez-Fuentes, Daniel Rodríguez-Almagro, Noelia Zagalaz-Anula, and Rafael Lomas-Vega. 2024. "Development and Validation of the Short Form (JAEN-10) of the Joint Assessment of Equilibrium and Neuromotor Status Scale (JAEN-20)" Journal of Functional Morphology and Kinesiology 9, no. 4: 223. https://doi.org/10.3390/jfmk9040223
APA StylePeinado-Rubia, A. B., Osuna-Pérez, M. C., Núñez-Fuentes, D., Rodríguez-Almagro, D., Zagalaz-Anula, N., & Lomas-Vega, R. (2024). Development and Validation of the Short Form (JAEN-10) of the Joint Assessment of Equilibrium and Neuromotor Status Scale (JAEN-20). Journal of Functional Morphology and Kinesiology, 9(4), 223. https://doi.org/10.3390/jfmk9040223








