Functional Recovery After Hip Arthroplasty with a Minimal Invasive or Classical Approach Eight Years After Intervention
Abstract
1. Introduction
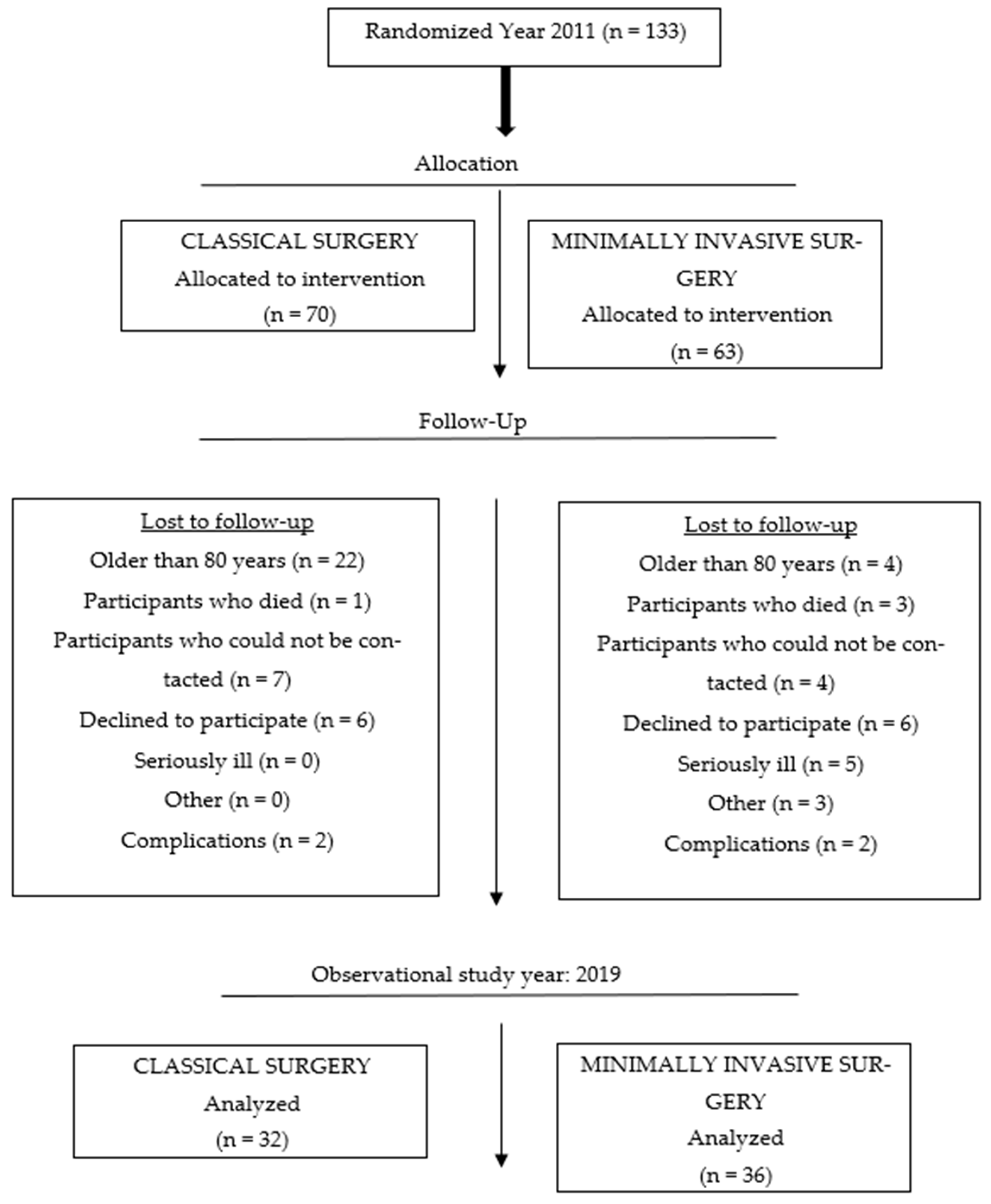
2. Materials and Methods
2.1. Participants
2.2. Surgical Technique
2.3. Study Design
2.4. Outcome Measures
2.4.1. Questionnaires
2.4.2. Motor Function Tests
2.4.3. Pain
2.4.4. Statistical Data Processing
3. Results
3.1. Demographic Characteristics
3.2. Harris Hip Score and Motor Function Tests
3.3. Relationship Between the Level of Physical Activity and Motor Functions
3.4. Correlation Between Body Mass Index and Motor Skills
3.5. The Relationship Between Age and Motor Skills
4. Discussion
4.1. Difference Between Groups in Motor Function Tests and Harris Hip Score
4.2. Correlation Between the Level of Physical Activity and Motor Skills
4.3. Correlation Between BMI and Motor Skills
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tudor, A.; Ruzic, L.; Vuckovic, M.; Prpic, T.; Rakovac, I.; Madjarevic, T.; Legovic, D.; Santic, V.; Mihelic, R.; Sestan, B. Functional Recovery after Muscle Sparing Total Hip Arthroplasty in Comparison to Classic Lateral Approach—A Three Years Follow-up Study. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2016, 21, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Roth, A. [The minimally invasive anterolateral approach. A review of the literature]. Orthopade 2012, 41, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Zhu, Q.; Han, Y.; Zhu, J.; Wang, H.; Cong, R.; Zhang, D. Minimally-Invasive Total Hip Arthroplasty Will Improve Early Postoperative Outcomes: A Prospective, Randomized, Controlled Trial. Ir. J. Med. Sci. 2010, 179, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Berry, D.J.; Berger, R.A.; Callaghan, J.J.; Dorr, L.D.; Duwelius, P.J.; Hartzband, M.A.; Lieberman, J.R.; Mears, D.C. Minimally Invasive Total Hip Arthroplasty. Development, Early Results, and a Critical Analysis. Presented at the Annual Meeting of the American Orthopaedic Association, Charleston, South Carolina, USA, June 14, 2003. J. Bone Jt. Surg. Am. 2003, 85, 2235–2246. [Google Scholar] [CrossRef]
- Woolson, S.T.; Mow, C.S.; Syquia, J.F.; Lannin, J.V.; Schurman, D.J. Comparison of Primary Total Hip Replacements Performed with a Standard Incision or a Mini-Incision. J. Bone Jt. Surg. Am. 2004, 86, 1353–1358. [Google Scholar] [CrossRef]
- Bertin, K.C.; Röttinger, H. Anterolateral Mini-Incision Hip Replacement Surgery: A Modified Watson-Jones Approach. Clin. Orthop. 2004, 429, 248–255. [Google Scholar] [CrossRef]
- Dorr, L.D.; Maheshwari, A.V.; Long, W.T.; Wan, Z.; Sirianni, L.E. Early Pain Relief and Function after Posterior Minimally Invasive and Conventional Total Hip Arthroplasty. A Prospective, Randomized, Blinded Study. J. Bone Jt. Surg. Am. 2007, 89, 1153–1160. [Google Scholar] [CrossRef]
- Mow, C.S.; Woolson, S.T.; Ngarmukos, S.G.; Park, E.H.; Lorenz, H.P. Comparison of Scars from Total Hip Replacements Done with a Standard or a Mini-Incision. Clin. Orthop. 2005, 441, 80–85. [Google Scholar] [CrossRef]
- Ritter, M.A.; Meding, J.B. Total Hip Arthroplasty. Can the Patient Play Sports Again? Orthopedics 1987, 10, 1447–1452. [Google Scholar] [CrossRef]
- Russo, M.W.; Macdonell, J.R.; Paulus, M.C.; Keller, J.M.; Zawadsky, M.W. Increased Complications in Obese Patients Undergoing Direct Anterior Total Hip Arthroplasty. J. Arthroplast. 2015, 30, 1384–1387. [Google Scholar] [CrossRef]
- Foote, J.; Panchoo, K.; Blair, P.; Bannister, G. Length of Stay Following Primary Total Hip Replacement. Ann. R. Coll. Surg. Engl. 2009, 91, 500–504. [Google Scholar] [CrossRef]
- Inneh, I.A.; Iorio, R.; Slover, J.D.; Bosco, J.A. Role of Sociodemographic, Co-Morbid and Intraoperative Factors in Length of Stay Following Primary Total Hip Arthroplasty. J. Arthroplast. 2015, 30, 2092–2097. [Google Scholar] [CrossRef]
- Liu, W.; Wahafu, T.; Cheng, M.; Cheng, T.; Zhang, Y.; Zhang, X. The Influence of Obesity on Primary Total Hip Arthroplasty Outcomes: A Meta-Analysis of Prospective Cohort Studies. Orthop. Traumatol. Surg. Res. OTSR 2015, 101, 289–296. [Google Scholar] [CrossRef]
- Barrett, M.; Prasad, A.; Boyce, L.; Dawson-Bowling, S.; Achan, P.; Millington, S.; Hanna, S.A. Total Hip Arthroplasty Outcomes in Morbidly Obese Patients: A Systematic Review. EFORT Open Rev. 2018, 3, 507–512. [Google Scholar] [CrossRef]
- Haynes, J.; Nam, D.; Barrack, R.L. Obesity in Total Hip Arthroplasty: Does It Make a Difference? Bone Jt. J. 2017, 99-B, 31–36. [Google Scholar] [CrossRef]
- Sayed-Noor, A.S.; Mukka, S.; Mohaddes, M.; Kärrholm, J.; Rolfson, O. Body Mass Index Is Associated with Risk of Reoperation and Revision after Primary Total Hip Arthroplasty: A Study of the Swedish Hip Arthroplasty Register Including 83,146 Patients. Acta Orthop. 2019, 90, 220–225. [Google Scholar] [CrossRef]
- Shen, J.; Chen, D. Recent Progress in Osteoarthritis Research. J. Am. Acad. Orthop. Surg. 2014, 22, 467–468. [Google Scholar] [CrossRef]
- Perruccio, A.V.; Young, J.J.; Wilfong, J.M.; Power, J.D.; Canizares, M.; Badley, E.M. Osteoarthritis Year in Review 2023: Epidemiology & Therapy. Osteoarthr. Cartil. 2024, 32, 159–165. [Google Scholar] [CrossRef]
- Rosenlund, S.; Broeng, L.; Holsgaard-Larsen, A.; Jensen, C.; Overgaard, S. Patient-Reported Outcome after Total Hip Arthroplasty: Comparison between Lateral and Posterior Approach. Acta Orthop. 2017, 88, 239–247. [Google Scholar] [CrossRef]
- Liljensøe, A.; Laursen, J.O.; Søballe, K.; Mechlenburg, I. Is High Body Mass Index a Potential Risk Factor for Poor Outcome after Hip Arthroplasty? A Cohort Study of 98 Patients 1 Year after Surgery. Acta Orthop. Belg. 2019, 85, 91–99. [Google Scholar]
- D’Arrigo, C.; Speranza, A.; Monaco, E.; Carcangiu, A.; Ferretti, A. Learning Curve in Tissue Sparing Total Hip Replacement: Comparison between Different Approaches. J. Orthop. Traumatol. Off. J. Ital. Soc. Orthop. Traumatol. 2009, 10, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Leuchte, S.; Luchs, A.; Wohlrab, D. [Measurement of ground reaction forces after total hip arthroplasty using different surgical approaches]. Z. Orthop. Ihre Grenzgeb. 2007, 145, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Inaba, Y.; Kobayashi, N.; Yukizawa, Y.; Ishida, T.; Iwamoto, N.; Saito, T. Little Clinical Advantage of Modified Watson-Jones Approach over Modified Mini-Incision Direct Lateral Approach in Primary Total Hip Arthroplasty. J. Arthroplast. 2011, 26, 1117–1122. [Google Scholar] [CrossRef] [PubMed]
- Godoy-Monzon, D.; Buttaro, M.; Comba, F.; Piccaluga, F.; Cid-Casteulani, A.; Ordas, A. Comparative Study of Radiological and Functional Outcomes Following a Direct Anterior Approach versus to a Posterolateral Approach to the Hip. Rev. Esp. Cir. Ortop. Traumatol. 2019, 63, 370–375. [Google Scholar] [CrossRef]
- Jianbo, J.; Ying, J.; Xinxin, L.; Lianghao, W.; Baoqing, Y.; Rongguang, A. Hip Hemiarthroplasty for Senile Femoral Neck Fractures: Minimally Invasive SuperPath Approach versus Traditional Posterior Approach. Injury 2019, 50, 1452–1459. [Google Scholar] [CrossRef]
- STROBE. Available online: https://www.strobe-statement.org/ (accessed on 1 February 2024).
- Deng, H.B.; Macfarlane, D.J.; Thomas, G.N.; Lao, X.Q.; Jiang, C.Q.; Cheng, K.K.; Lam, T.H. Reliability and Validity of the IPAQ-Chinese: The Guangzhou Biobank Cohort Study. Med. Sci. Sports Exerc. 2008, 40, 303–307. [Google Scholar] [CrossRef]
- Macfarlane, D.J.; Lee, C.C.Y.; Ho, E.Y.K.; Chan, K.L.; Chan, D.T.S. Reliability and Validity of the Chinese Version of IPAQ (Short, Last 7 Days). J. Sci. Med. Sport 2007, 10, 45–51. [Google Scholar] [CrossRef]
- Vandelanotte, C.; Bourdeaudhuij, I.; Philippaerts, R.; Sjostrom, M.; Sallis, J. Reliability and Validity of a Computerized and Dutch Version of the International Physical Activity Questionnaire (IPAQ). J. Phys. Act Health 2005, 2, 63–75. [Google Scholar] [CrossRef]
- Mišigoj-Duraković, M. Tjelesno Vježbanje i Zdravlje, 2nd ed.; Znanje d.o.o.: Zagreb, Croatia, 2018; ISBN 978-953-343-702-6. [Google Scholar]
- Singh, J.A.; Schleck, C.; Harmsen, S.; Lewallen, D. Clinically Important Improvement Thresholds for Harris Hip Score and Its Ability to Predict Revision Risk after Primary Total Hip Arthroplasty. BMC Musculoskelet. Disord. 2016, 17, 256. [Google Scholar] [CrossRef]
- Nilsdotter, A.; Bremander, A. Measures of Hip Function and Symptoms: Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score (HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopedic Surgeons (AAOS) Hip and Knee Questionnaire. Arthritis Care Res. 2011, 63 (Suppl. 11), S200–S207. [Google Scholar] [CrossRef]
- Harris Hip Score—Orthopaedic Scores. Available online: https://www.orthopaedicscore.com/scorepages/harris_hip_score.html (accessed on 23 April 2024).
- Heller, G.Z.; Manuguerra, M.; Chow, R. How to Analyze the Visual Analogue Scale: Myths, Truths and Clinical Relevance. Scand. J. Pain 2016, 13, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Lenhard, W.; Lenhard, A. Computation of Effect Sizes; Psychometrica: Dettelbach, Germany, 2017; p. 2024. [Google Scholar]
- Srikanth, V.K.; Fryer, J.L.; Zhai, G.; Winzenberg, T.M.; Hosmer, D.; Jones, G. A Meta-Analysis of Sex Differences Prevalence, Incidence and Severity of Osteoarthritis. Osteoarthr. Cartil. 2005, 13, 769–781. [Google Scholar] [CrossRef] [PubMed]
- Hughes-Oliver, C.N.; Srinivasan, D.; Schmitt, D.; Queen, R.M. Gender and Limb Differences in Temporal Gait Parameters and Gait Variability in Ankle Osteoarthritis. Gait Posture 2018, 65, 228–233. [Google Scholar] [CrossRef]
- Conaghan, P.G. Osteoarthritis in 2012: Parallel Evolution of OA Phenotypes and Therapies. Nat. Rev. Rheumatol. 2013, 9, 68–70. [Google Scholar] [CrossRef]
- Crawford, R.W.; Murray, D.W. Total Hip Replacement: Indications for Surgery and Risk Factors for Failure. Ann. Rheum. Dis. 1997, 56, 455–457. [Google Scholar] [CrossRef]
- von Rottkay, E.; Rackwitz, L.; Rudert, M.; Nöth, U.; Reichert, J.C. Function and Activity after Minimally Invasive Total Hip Arthroplasty Compared to a Healthy Population. Int. Orthop. 2018, 42, 297–302. [Google Scholar] [CrossRef]
- Judge, A.; Batra, R.N.; Thomas, G.E.; Beard, D.; Javaid, M.K.; Murray, D.W.; Dieppe, P.A.; Dreinhoefer, K.E.; Peter-Guenther, K.; Field, R.; et al. Body Mass Index Is Not a Clinically Meaningful Predictor of Patient Reported Outcomes of Primary Hip Replacement Surgery: Prospective Cohort Study. Osteoarthr. Cartil. 2014, 22, 431–439. [Google Scholar] [CrossRef]
- McCalden, R.W.; Charron, K.D.; MacDonald, S.J.; Bourne, R.B.; Naudie, D.D. Does Morbid Obesity Affect the Outcome of Total Hip Replacement?: An Analysis of 3290 THRs. J. Bone Jt. Surg. Br. 2011, 93, 321–325. [Google Scholar] [CrossRef]
- Abdulla, I.; Mahdavi, S.; Khong, H.; Gill, R.; Powell, J.; Johnston, K.D.; Sharma, R. Does Body Mass Index Affect the Rate of Adverse Outcomes in Total Hip and Knee Arthroplasty? A Retrospective Review of a Total Joint Replacement Database. Can. J. Surg. J. Can. Chir. 2020, 63, E142–E149. [Google Scholar] [CrossRef]
- Mouchti, S.; Whitehouse, M.R.; Sayers, A.; Hunt, L.P.; MacGregor, A.; Blom, A.W. The Association of Body Mass Index with Risk of Long-Term Revision and 90-Day Mortality Following Primary Total Hip Replacement: Findings from the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. J. Bone Jt. Surg. Am. 2018, 100, 2140–2152. [Google Scholar] [CrossRef]
- Courtine, M.; Bourredjem, A.; Gouteron, A.; Fournel, I.; Bartolone, P.; Baulot, E.; Ornetti, P.; Martz, P. Functional Recovery after Total Hip/Knee Replacement in Obese People: A Systematic Review. Ann. Phys. Rehabil. Med. 2023, 66, 101710. [Google Scholar] [CrossRef]
| Variables | CS M (SD) or n (%) | MIS M (SD) or n (%) |
|---|---|---|
| Age | 68.25 (8.06) | 69.94 (7.3) |
| Gender | n (%) | n (%) |
| Female | 24 (75) | 26 (72) |
| Male | 8 (25) | 10 (28) |
| Body mass index | M (SD) | M (SD) |
| Female | 27.16 (4.38) | 29.11 (4.95) |
| Male | 28 (4.69) | 28.9 (3.44) |
| Clinical status | n (%) | n (%) |
| Healthy | 12 (37.5) | 9 (25) |
| Cardiovascular diseases | 7 (22) | 10 (27.77) |
| Musculoskeletal disease | 1 (3.1) | 0 |
| Endocrine, nutritional, and metabolic diseases | 2 (6.25) | 1 (2.77) |
| Diseases of the respiratory system | 1 (3.1) | 1 (2.77) |
| Diseases of the genital and urinary system | 1 (3.1) | 0 |
| Neoplasms | 1 (3.1) | 1 (2.77) |
| Eye diseases | 0 | 1 (2.77) |
| Diseases of the digestive system | 0 | 1 (2.77) |
| Two comorbidities | 6 (18.75) | 11 (30.55) |
| Three comorbidities | 1 (3.1) | 1 (2.77) |
| Operated side | n (%) | n (%) |
| Left side | 17 (53) | 17 (47) |
| Right side | 15 (47) | 19 (53) |
| Variables | CS C (25–75 Percentile) N = 32 | MIS C (25–75 Percentile) N = 36 | U p * | Effect Size η2 d |
|---|---|---|---|---|
| Abductor muscle strength | 7.0 (3.0–9.0) | 8.0 (5.0–9.0) | 475.00 0.210 | 0.02 0.30 |
| Harris Hip Score | 86.3 (72.1–91.5) | 92.9 (90.05–95.75) | 264.00 <0.001 * | 0.22 1.05 |
| ROM-hip abduction | 10.0 (10.0–15.0) | 15.0 (10.0–20.0) | 318.00 <0.001 | 0.15 0.83 |
| ROM-hip flexion | 90.0 (75.0–100.0) | 95.0 (90.0–101.0) | 384.00 0.018 * | 0.08 0.60 |
| Walk for 50 m | 26.8 (23–32.6) | 23 (20.7–31.6) | 435.00 0.080 | 0.04 0.43 |
| IPAQ | 1389.0 (905.5–2006.0) | 1265.0 (672.0–1977.0) | 547.50 0.730 | 0.002 0.008 |
| Correlation of IPAQ with | CS (n = 32) rs p | MIS (n = 36) rs p |
|---|---|---|
| Abductor muscle strength | 0.43 0.011 * | 0.23 0.170 |
| Walk for 50 m | −0.16 0.368 | −0.33 0.052 |
| Harris Hip Score | 0.27 0.128 | 0.34 0.041 * |
| ROM-hip abduction | 0.05 0.762 | 0.03 0.878 |
| ROM-hip flexion | 0.31 0.082 | 0.13 0.439 |
| Correlation of BMI with | CS (n = 32) rs p * | MIS (n = 36) rs p * |
|---|---|---|
| Walk for 50 m | 0.39 0.027 * | 0.35 0.03 * |
| ROM-hip flexion | −0.21 0.257 | −0.37 0.020 * |
| ROM-hip abduction | −0.09 0.623 | −0.23 0.170 |
| Abductor muscle strength | −0.15 0.422 | −0.24 0.151 |
| IPAQ | −0.09 0.604 | −0.27 0.111 |
| Harris Hip Score | −0.06 0.733 | −0.26 0.121 |
| Correlation of Age with | CS (n = 32) rs p | MIS (n = 36) rs p |
|---|---|---|
| Harris Hip Score | −0.13 0.495 | −0.36 0.032 * |
| Walk for 50 m | 0.24 0.190 | 0.51 0.001 * |
| Abductor muscle strength | −0.14 0.451 | −0.44 0.007 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vuckovic, M.; Ruzic, L.; Tudor, K.; Prpic, T.; Jotanovic, Z.; Segulja, S.; Lekic, A.; Bazdaric, K. Functional Recovery After Hip Arthroplasty with a Minimal Invasive or Classical Approach Eight Years After Intervention. J. Funct. Morphol. Kinesiol. 2024, 9, 208. https://doi.org/10.3390/jfmk9040208
Vuckovic M, Ruzic L, Tudor K, Prpic T, Jotanovic Z, Segulja S, Lekic A, Bazdaric K. Functional Recovery After Hip Arthroplasty with a Minimal Invasive or Classical Approach Eight Years After Intervention. Journal of Functional Morphology and Kinesiology. 2024; 9(4):208. https://doi.org/10.3390/jfmk9040208
Chicago/Turabian StyleVuckovic, Mirela, Lana Ruzic, Karlo Tudor, Tomislav Prpic, Zdravko Jotanovic, Silvije Segulja, Andrica Lekic, and Ksenija Bazdaric. 2024. "Functional Recovery After Hip Arthroplasty with a Minimal Invasive or Classical Approach Eight Years After Intervention" Journal of Functional Morphology and Kinesiology 9, no. 4: 208. https://doi.org/10.3390/jfmk9040208
APA StyleVuckovic, M., Ruzic, L., Tudor, K., Prpic, T., Jotanovic, Z., Segulja, S., Lekic, A., & Bazdaric, K. (2024). Functional Recovery After Hip Arthroplasty with a Minimal Invasive or Classical Approach Eight Years After Intervention. Journal of Functional Morphology and Kinesiology, 9(4), 208. https://doi.org/10.3390/jfmk9040208







