Effects of Oral Lactate Supplementation on Acid–Base Balance and Prolonged High-Intensity Interval Cycling Performance
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Experimental Design
2.3. Equipment and Measurements
2.4. Cardio Pulmonary Exercise Test (CPET)
2.5. Supplementation Strategy
2.6. Dietary Control
2.7. Exercise Protocol
2.8. Statistical Analysis
3. Results
3.1. Acid–Base Balance and Metabolic Measurements Pre and Post Supplementation
3.2. Performance Data
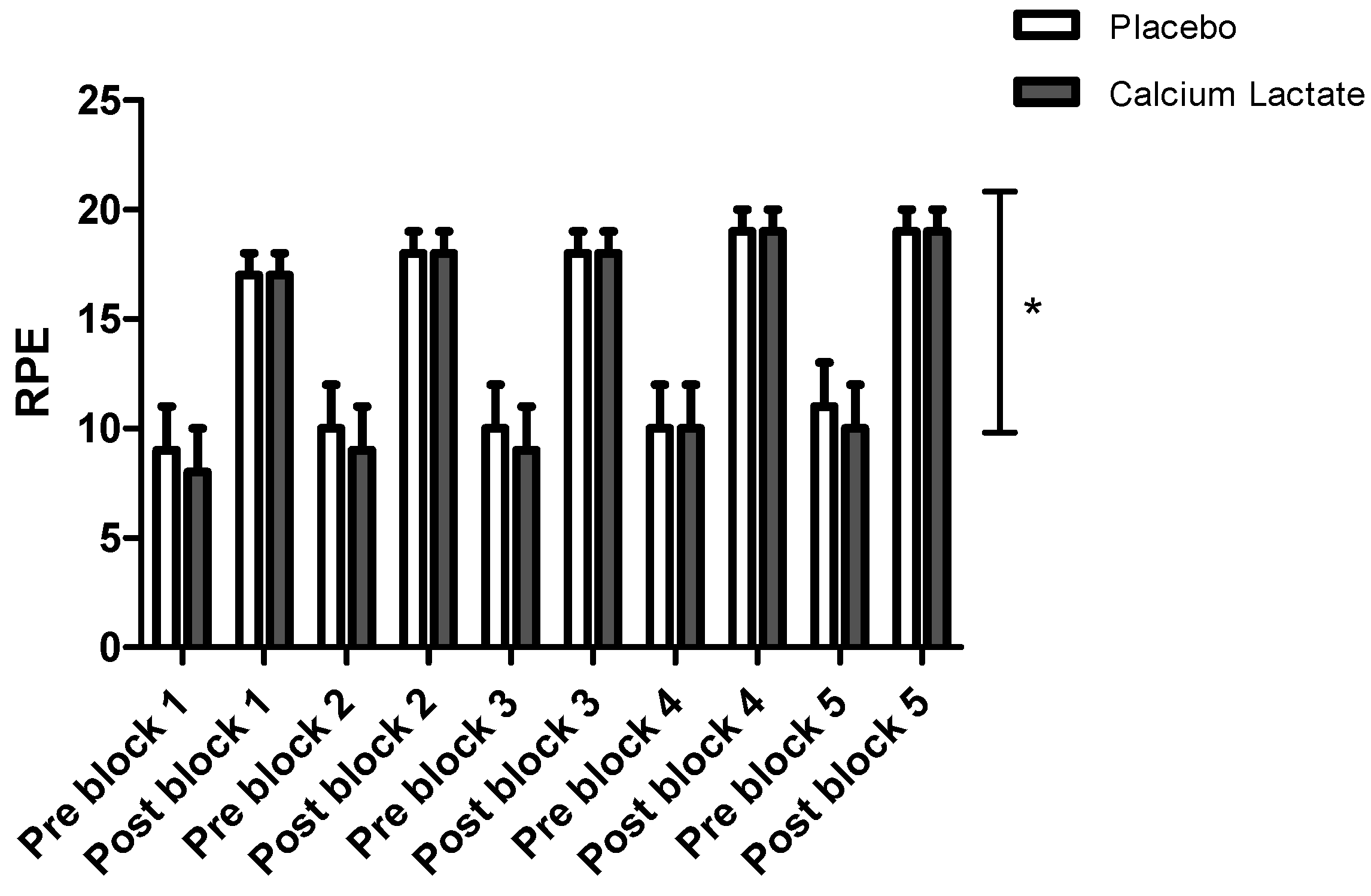
3.3. Heart Rate and Perceived Exertion
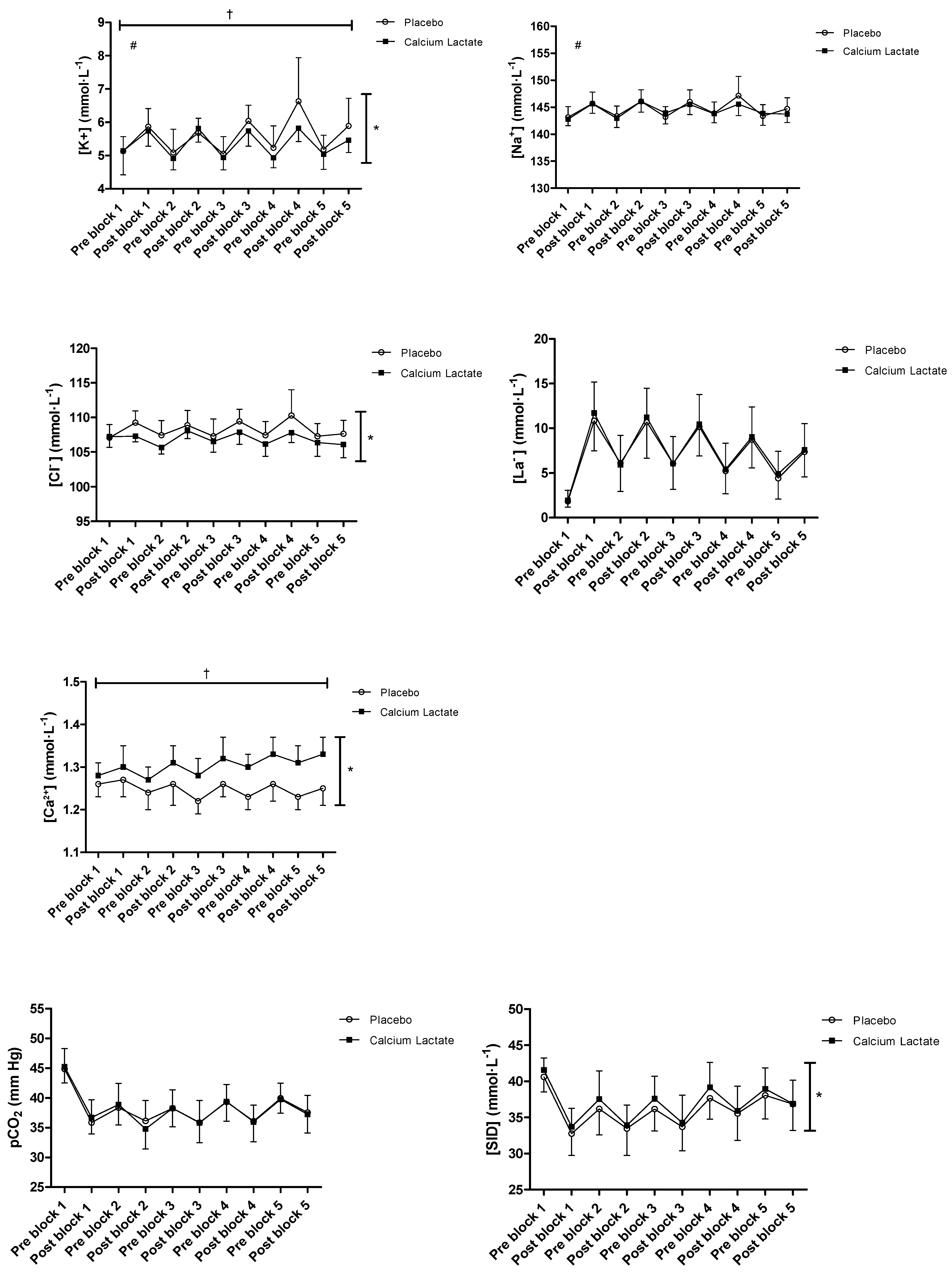
3.4. Acid–Base Balance and Metabolic Measurements during Exercise
3.5. Gastro-Intestinal Tolerance
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gladden, L.B. Lactate metabolism: A new paradigm for the third millennium. J. Physiol. 2004, 558, 5–30. [Google Scholar] [CrossRef] [PubMed]
- Hall, M.M.; Rajasekaran, S.; Thomsen, T.W.; Peterson, A.R. Lactate: Friend or Foe. PM&R 2016, 8, S8–S15. [Google Scholar]
- Rabinowitz, J.D.; Enerbäck, S. Lactate: The ugly duckling of energy metabolism. Nat. Metab. 2020, 2, 566–571. [Google Scholar] [CrossRef] [PubMed]
- Morris, D. Effects of oral lactate consumption on metabolism and exercise performance. Curr. Sports Med. Rep. 2012, 11, 185–188. [Google Scholar] [CrossRef] [PubMed]
- Morris, D.M.; Beloni, R.K.; Wofford, H.; Roslanova, E. Metabolic and exercise performance responses to Two different oral Doses of Calcium Lactate. Sports Nutr. Ther. 2016, 1, 117. [Google Scholar] [CrossRef]
- Jacobs, R.A.; Meinild, A.K.; Nordsborg, N.B.; Lundby, C. Lactate oxidation in human skeletal muscle mitochondria. Am. J. Physiol.-Endocrinol. Metab. 2013, 304, E686–E694. [Google Scholar] [CrossRef] [PubMed]
- Hostetler, K.Y.; Williams, H.R.; Shreeve, W.W.; Landau, B.R. Conversion of specifically 14 C-labelled lactate and pyruvate to glucose in man. J. Biol. Chem. 1969, 244, 2075–2077. [Google Scholar] [CrossRef] [PubMed]
- Brooks, G.A. The lactate shuttle during exercise and recovery. Med. Sci. Sports Exerc. 1986, 18, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Brooks, G.A.; Arevalo, J.A.; Osmond, A.D.; Leija, R.G.; Curl, C.C.; Tovar, A.P. Lactate in contemporary biology: A phoenix risen. J. Physiol. 2021, 600, 1229–1251. [Google Scholar]
- Van Montforrt, M.C.E.; Van Dieren, L.; Hopkins, W.G.; Shearman, J.P. Effects of Ingestion of Bicarbonate, Citrate, Lactate, and Chloride on Sprint Running. Med. Sci. Sports Exerc. 2004, 36, 1239–1243. [Google Scholar] [CrossRef] [PubMed]
- Bryner, R.W.; Hornsby, W.G.; Chetlin, R.; Ullrich, I.H.; Yeater, R.A. Effect of lactate consumption on exercise performance. J. Sports Med. Phys. Fit. 1998, 38, 116–123. [Google Scholar] [CrossRef]
- Swensen, T.; Crater, G.; Bassett, D.; Howley, E. Adding Polylactate to a Glucose Polymer Solution Does not Improve Endurance. Int. J. Sports Med. 1994, 15, 430–434. [Google Scholar] [CrossRef] [PubMed]
- Morris, D.M.; Shafer, R.S.; Fairbrother, K.R.; Woodall, M.W. Effects of Lactate Consumption on Blood Bicarbonate Levels and Performance during High-Intensity Exercise. Int. J. Sport Nutr. Exerc. Metab. 2011, 21, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Northgraves, M.J.; Peart, D.J.; Jordan, C.A.; Vince, R.V. Effect of Lactate Supplementation and Sodium Bicarbonate on 40-km Cycling Time Trial Performance. J. Strength Cond. Res. 2013, 28, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, L.F.; de Salles Painelli, V.; Nemezio, K.; Gonçalves, L.S.; Yamaguchi, G.; Saunders, B.; Gualano, B.; Artioli, G.G. Chronic lactate supplementation does not improve blood buffering capacity and repeated high-intensity exercise. Scand. J. Med. Sci. Sports 2016, 27, 1231–1239. [Google Scholar] [CrossRef]
- Peveler, W.W.; Palmer, T.G. Effect of Magnesium Lactate Dihydrate and Calcium Lactate Monohydrate on 20-km Cycling Time Trial Performance. J. Strength Cond. Res. 2012, 26, 1149–1153. [Google Scholar] [CrossRef]
- Russ, A.E.; Schifino, A.G.; Leong, C.-H. Effect of lactate supplementation on VO2peak and onset of blood lactate accumulation: A double blind, placebo-controlled trial. Acta Gymnica 2019, 49, 51–57. [Google Scholar] [CrossRef]
- de Salles Painelli, V.; da Silva, R.P.; de Oliveira, O.M.; de Oliveira, L.F.; Benatti, F.B.; Rabelo, T.; Guilherme, J.P.L.F.; Junior, A.H.L.; Artioli, G.G. The Effects of Two Different Doses of Calcium Lactate on Blood pH, Bicarbonate, and Repeated High-Intensity Exercise Performance. Int. J. Sport Nutr. Exerc. Metab. 2014, 24, 286–295. [Google Scholar] [CrossRef]
- Azevedo, J.L.; Tietz, E.; Two-Feathers, T.; Paull, J.; Chapman, K. Lactate, Fructose and Glucose Oxidation Profiles in Sports Drinks and the Effect on Exercise Performance. PLoS ONE 2007, 2, e927. [Google Scholar] [CrossRef]
- Sanders, D.; Heijboer, M. Physical demands and power profile of different stage types within a cycling grand tour. Eur. J. Sport Sci. 2018, 19, 736–744. [Google Scholar] [CrossRef]
- Vogt, S.; Heinrich, L.; Schumacher, Y.O.; Blum, A.; Roecker, K.; Dickhuth, H.-H.; Schmid, A. Power Output during Stage Racing in Professional Road Cycling. Med. Sci. Sports Exerc. 2006, 38, 147–151. [Google Scholar] [CrossRef]
- Jacobs, I.; Kaiser, P.; Tesch, P. Muscle strength and fatigue after selective glycogen depletion in human skeletal muscle fibers. Eur. J. Appl. Physiol. Occup. Physiol. 1981, 46, 47–53. [Google Scholar] [CrossRef]
- Ørtenblad, N.; Westerblad, H.; Nielsen, J. Muscle glycogen stores and fatigue. J. Physiol. 2013, 591, 4405–4413. [Google Scholar] [CrossRef]
- Amann, M.; Wan, H.Y.; Thurston, T.S.; Georgescu, V.P.; Weavil, J.C. On the Influence of Group III/IV Muscle Afferent Feedback on Endurance Exercise Performance. Exerc. Sport Sci. Rev. 2020, 48, 209–216. [Google Scholar] [CrossRef]
- Péronnet, F.; Burelle, Y.; Massicotte, D.; Lavoie, C.; Hillaire-Marcel, C. Respective oxidation of13C-labeled lactate and glucose ingested simultaneously during exercise. J. Appl. Physiol. 1997, 82, 440–446. [Google Scholar] [CrossRef][Green Version]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Johnson, M.A.; Mills, D.E.; Brown, P.I.; Sharpe, G.R. Prior upper body exercise reduces cycling work capacity but not critical power. Med. Sci. Sports Exerc. 2014, 46, 802–808. [Google Scholar] [CrossRef]
- Stickland, M.K.; Lindinger, M.I.; Olfert, I.M.; Heigenhauser, G.J.F.; Hopkins, S.R. Pulmonary gas exchange and acid–base balance during exercise. Compr. Physiol. 2013, 3, 693–739. [Google Scholar]
- Harrison, M.H. Effects on thermal stress and exercise on blood volume in humans. Physiol. Rev. 1985, 65, 149–209. [Google Scholar] [CrossRef]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef]
- Carr, A.J.; Slater, G.J.; Gore, C.J.; Dawson, B.; Burke, L.M. Effect of sodium bicarbonate on [HCO3−], pH, and gastrointestinal symptoms. Int. J. Sport Nutr. Exerc. Metab. 2011, 21, 189–194. [Google Scholar] [CrossRef]
- Miller, P.; Robinson, A.L.; Sparks, S.A.; Bridge, C.A.; Bentley, D.J.; McNaughton, L.R. The Effects of Novel Ingestion of Sodium Bicarbonate on Repeated Sprint Ability. J. Strength Cond. Res. 2016, 30, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Vanhatalo, A.; Black, M.I.; DiMenna, F.J.; Blackwell, J.R.; Schmidt, J.F.; Thompson, C.; Wylie, L.J.; Mohr, M.; Bangsbo, J.; Krustrup, P.; et al. The mechanistic bases of the power-time relationship: Muscle metabolic responses and relationships to muscle fibre type. J. Physiol. 2016, 594, 4407–4423. [Google Scholar] [CrossRef] [PubMed]
- Committee on Medical Aspects of Food Policy (COMA). 41 Dietary Reference Values for Food Energy and Nutrients for the United Kingdom; Report on Health and Social Subjects; HMSO: London, UK, 1991. [Google Scholar]
- Burke, L.M.; Hawley, J.A.; Schabort, E.J.; Gibson, A.S.C.; Mujika, I.; Noakes, T.D. Carbohydrate loading failed to improve 100-km cycling performance in a placebo-controlled trial. J. Appl. Physiol. 2000, 88, 1284–1290. [Google Scholar] [CrossRef]
- Jeacocke, N.A.; Burke, L.M. Methods to standardize dietary intake before performance testing. Int. J. Sport Nutr. Exerc. Metab. 2010, 20, 87–103. [Google Scholar] [CrossRef] [PubMed]
- Tomcik, K.A.; Camera, D.M.; Bone, J.L.; Ross, M.L.; Jeacocke, N.A.; Tachtsis, B.; Senden, J.; VAN Loon, L.J.C.; Hawley, J.A.; Burke, L.M. Effects of Creatine and Carbohydrate Loading on Cycling Time Trial Performance. Med. Sci. Sports Exerc. 2018, 50, 141–150. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioural Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1998. [Google Scholar]
- Fahey, T.D.; Larsen, J.D.; Brooks, G.A.; Colvin, W.; Henderson, S.; Lary, D. The Effects of Ingesting Polylactate or Glucose Polymer Drinks during Prolonged Exercise. Int. J. Sport Nutr. 1991, 1, 249–256. [Google Scholar] [CrossRef]
- Peacock, C.A.; Pollock, B.S.; Burns, K.L.; Sanders, G.J.; Glickman, E.L. Improving Cardiovascular Performance and Decreasing Perceived Exertion with Lactate Supplement. NSUWorks. 2017. Available online: https://nsuworks.nova.edu/hpd_hhp_facarticles/34/ (accessed on 15 February 2023).
- Lindinger, M.I.; Heigenhauser, G.J.; McKelvie, R.S.; Jones, N.L. Blood ion regulation during repeated maximal exercise and recovery in humans. Am. J. Physiol. 1992, 262, R126–R136. [Google Scholar] [CrossRef]
- Miller, B.F.; Lindinger, M.I.; Fattor, J.A.; Jacobs, K.A.; LeBlanc, P.J.; Duong, M.; Heigenhauser, G.J.F.; Brooks, G.A. Hematological and acid-base changes in men during prolonged exercise with and without sodium-lactate infusion. J. Appl. Physiol. 2005, 98, 856–865. [Google Scholar] [CrossRef]
- Hostrup, M.; Cairns, S.P.; Bangsbo, J. Muscle Ionic Shifts during Exercise: Implications for Fatigue and Exercise Performance. Compr. Physiol. 2021, 11, 1895–1959. [Google Scholar]
- Hureau, T.J.; Romer, L.M.; Amann, M. The ‘sensory tolerance limit’: A hypothetical construct determining exercise performance? Eur. J. Sport Sci. 2018, 18, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.A.; Sharpe, G.R.; Williams, N.C.; Hannah, R. Locomotor muscle fatigue is not critically regulated after prior upper body exercise. J. Appl. Physiol. 2015, 119, 840–850. [Google Scholar] [CrossRef] [PubMed]
- Hebestreit, H.; Meyer, F.; Htay-Htay; Heigenhauser, G.J.F.; Bar-Or, O. Plasma metabolites, volume and electrolytes following 30-s high-intensity exercise in boys and men. Eur. J. Appl. Physiol. Occup. Physiol. 1996, 72, 563–569. [Google Scholar] [CrossRef] [PubMed]
- Brooks, G.A. What the Lactate Shuttle Means for Sports Nutrition. Nutrients 2023, 15, 2178. [Google Scholar] [CrossRef] [PubMed]
- Ganapathy, V.; Thangaraju, M.; Gopal, E.; Martin, P.M.; Itagaki, S.; Miyauchi, S.; Prasad, P.D. Sodium-coupled monocarboxylate transporters in normal tissues and in cancer. AAPS J. 2008, 10, 193–199. [Google Scholar] [CrossRef] [PubMed]


| Pre Supplementation | Post Supplementation | Δ | |
|---|---|---|---|
| Treatment | |||
| Calcium Lactate | |||
| [K+] mmol·−1 | 4.91 (4.62, 5.20) | 4.81 (4.62, 5.00) | −0.10 (−0.38, 0.18) |
| [Na+] mmol·L−1 | 143 (142, 143) | 142 (141, 143) | −0.57 (−1.52, 0.38) |
| [Cl−] mmol·L−1 | 107 (106, 108) | 105 (105, 106) | −2.07 (−2.77, −1.37) * |
| [La−] mmol·L−1 | 2.14 (1.78, 2.50) | 1.86 (1.63, 2.10) | −0.27 (−0.59, 0.05) |
| [Ca2+] mmol·L−1 | 1.24 (1.22, 1.26) | 1.26 (1.25, 1.28) | 0.02 (0.01, 0.03) |
| pCO2 mm Hg | 41.31 (39.84, 42.77) | 42.68 (41.60, 43.76) | 1.37 (0.01, 2.73) |
| [SID] mmol·L−1 | 39.44 (38.61, 40.28) | 41.14 (40.12, 42.15) | 1.69 (0.29, 3.10) * |
| [HCO3−] mmol·L−1 | 25.79 (25.11, 26.46) | 26.68 (26.14, 27.22) | 0.89 (0.07, 1.71) * |
| [H+] nmol·L−1 | 38.52 (37.29, 39.75) | 38.06 (36.98, 39.14) | −0.46 (−1.50, 0.59) |
| [Glucose] mmol·L−1 | 5.11 (4.80, 5.43) | 5.11 (4.77, 5.46) | 0.00 (−0.48, 0.48) |
| Placebo | |||
| [K+] mmol·L−1 | 4.94 (4.60, 5.27) | 4.97 (4.76, 5.18) | 0.03 (−0.40, 0.47) |
| [Na+] mmol·L−1 | 143 (142, 144) | 142 (141, 143) | −1.00 (−1.78, −0.22) |
| [Cl−] mmol·L−1 | 107 (106, 108) | 106 (105, 107) | −0.64 (−1.42, 0.14) |
| [La−] mmol·L−1 | 2.08 (1.76, 2.40) | 1.73 (1.42, 2.05) | −0.34 (−0.73, 0.04) |
| [Ca2+] mmol·L−1 | 1.25 (1.23, 1.26) | 1.25 (1.24, 1.26) | 0.00 (−0.01, 0.02) |
| pCO2 mm Hg | 41.88 (40.91, 42.86) | 42.70 (41.40, 44.00) | 0.82 (−0.45, 2.08) |
| [SID] mmol·L−1 | 40.19 (39.16, 41.21) | 40.20 (39.21, 41.20) | 0.02 (−0.94, 0.97) |
| [HCO3−] mmol·L−1 | 25.95 (25.40, 26.49) | 25.76 (25.21, 26.32) | −0.18 (−0.74, 0.38) |
| [H+] nmol·L−1 | 38.62 (37.80, 39.44) | 39.30 (38.21, 40.39) | 0.68 (−0.51, 1.88) |
| [Glucose] mmol·L−1 | 5.62 (5.27, 5.97) | 5.29 (5.01, 5.58) | −0.32 (−0.86, 0.21) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bordoli, C.; Varley, I.; Sharpe, G.R.; Johnson, M.A.; Hennis, P.J. Effects of Oral Lactate Supplementation on Acid–Base Balance and Prolonged High-Intensity Interval Cycling Performance. J. Funct. Morphol. Kinesiol. 2024, 9, 139. https://doi.org/10.3390/jfmk9030139
Bordoli C, Varley I, Sharpe GR, Johnson MA, Hennis PJ. Effects of Oral Lactate Supplementation on Acid–Base Balance and Prolonged High-Intensity Interval Cycling Performance. Journal of Functional Morphology and Kinesiology. 2024; 9(3):139. https://doi.org/10.3390/jfmk9030139
Chicago/Turabian StyleBordoli, Claire, Ian Varley, Graham R. Sharpe, Michael A. Johnson, and Philip J. Hennis. 2024. "Effects of Oral Lactate Supplementation on Acid–Base Balance and Prolonged High-Intensity Interval Cycling Performance" Journal of Functional Morphology and Kinesiology 9, no. 3: 139. https://doi.org/10.3390/jfmk9030139
APA StyleBordoli, C., Varley, I., Sharpe, G. R., Johnson, M. A., & Hennis, P. J. (2024). Effects of Oral Lactate Supplementation on Acid–Base Balance and Prolonged High-Intensity Interval Cycling Performance. Journal of Functional Morphology and Kinesiology, 9(3), 139. https://doi.org/10.3390/jfmk9030139







