Associations between Dietary Intake and Cardiovascular Disease Risk in American Career Firefighters: An Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Experimental Design
2.2. Participants
2.3. Food Frequency and Health Questionnaire
2.4. CVD Risk
2.5. Anthropometrics and Physical Assessment
2.6. Statistical Analysis
3. Results
3.1. Statistical Analysis
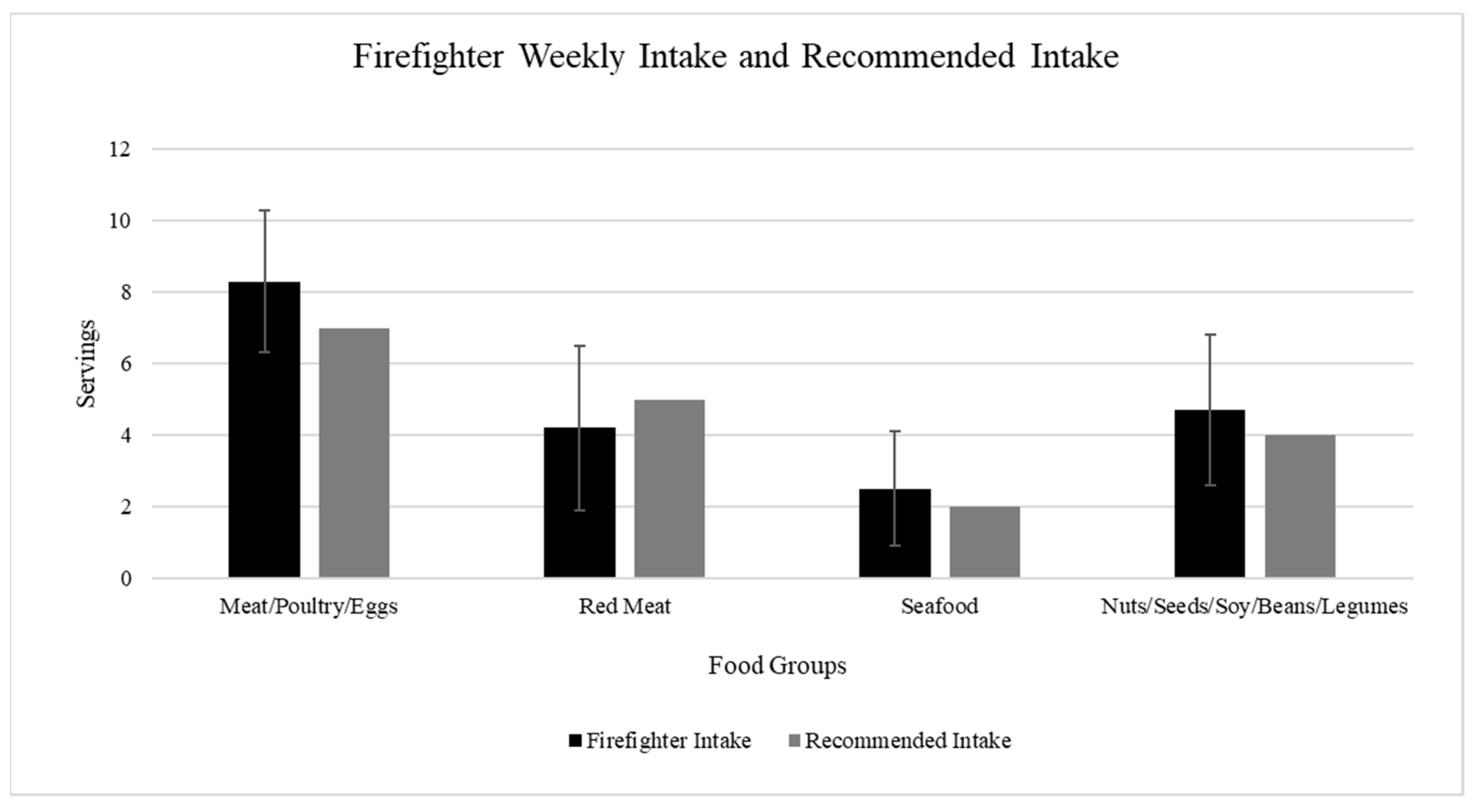
3.2. Dietary Intake
3.3. CVD Risk
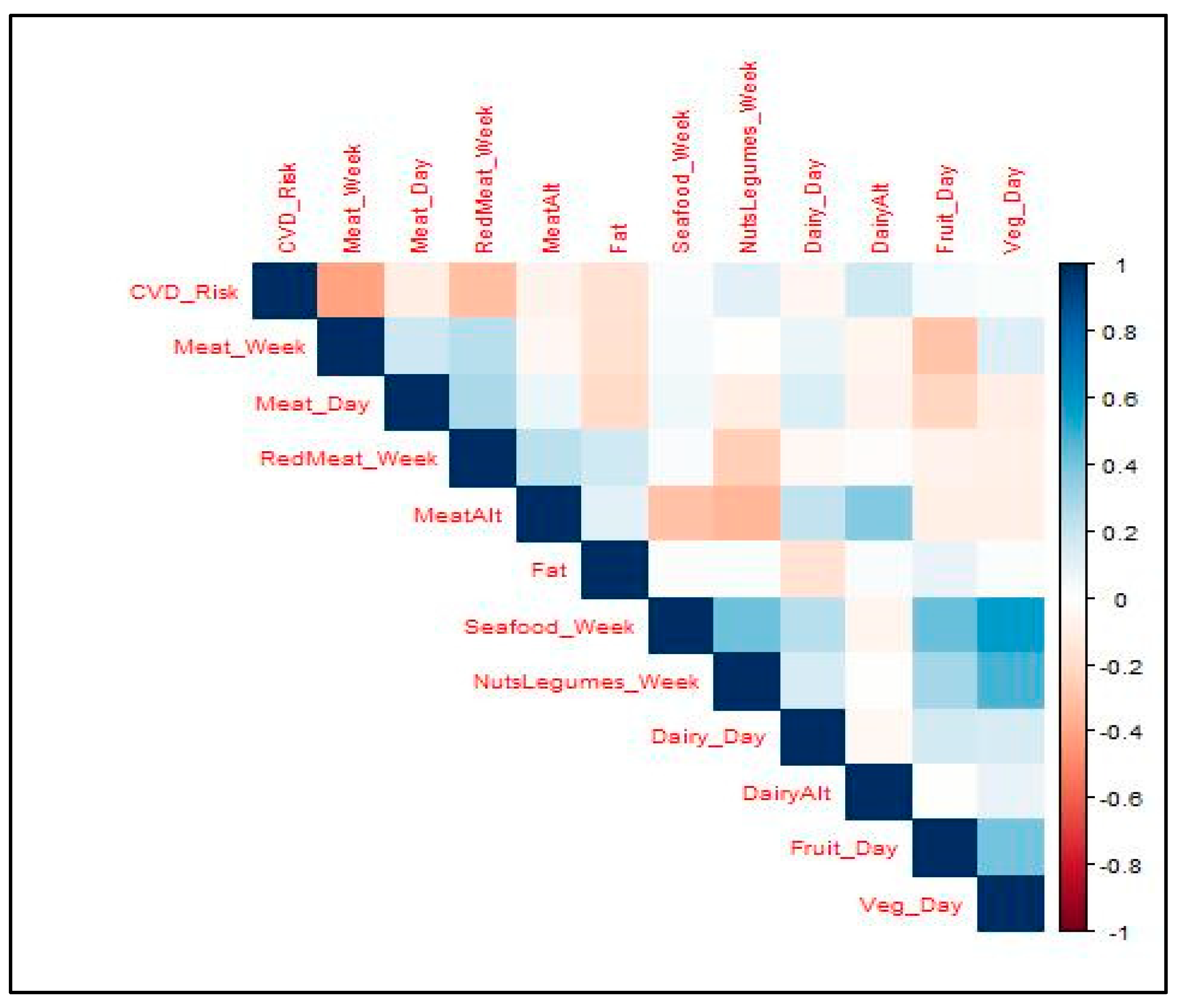
3.4. Associations between Dietary Intake and Cardiovascular Disease Risk
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Storer, T.W.; Dolezal, B.A.; Abrazado, M.L.; Smith, D.L.; Batalin, M.A.; Tseng, C.-H.; Cooper, C.B.; Group, T.P.S. Firefighter Health and Fitness Assessment: A Call to Action. J. Strength Cond. Res. 2014, 28, 661. [Google Scholar] [CrossRef]
- Gledhill, N.; Jamnik, V.K. Characterization of the Physical Demands of Firefighting. Can. J. Sport Sci. 1992, 17, 207–213. [Google Scholar]
- Kivimäki, M.; Head, J.; Ferrie, J.E.; Shipley, M.J.; Brunner, E.; Vahtera, J.; Marmot, M.G. Work Stress, Weight Gain and Weight Loss: Evidence for Bidirectional Effects of Job Strain on Body Mass Index in the Whitehall II Study. Int. J. Obes. 2006, 30, 982–987. [Google Scholar] [CrossRef]
- Dimsdale, J.E. Psychological Stress and Cardiovascular Disease. J. Am. Coll. Cardiol. 2008, 51, 1237–1246. [Google Scholar] [CrossRef]
- Puttonen, S.; Härmä, M.; Hublin, C. Shift Work and Cardiovascular Disease—Pathways from Circadian Stress to Morbidity. Scand. J. Work. Environ. Health 2010, 36, 96–108. [Google Scholar] [CrossRef]
- Albert, C.M.; Mittleman, M.A.; Chae, C.U.; Lee, I.-M.; Hennekens, C.H.; Manson, J.E. Triggering of Sudden Death from Cardiac Causes by Vigorous Exertion. N. Engl. J. Med. 2000, 343, 1355–1361. [Google Scholar] [CrossRef]
- Soteriades, E.S.; Smith, D.L.; Tsismenakis, A.J.; Baur, D.M.; Kales, S.N. Cardiovascular Disease in US Firefighters: A Systematic Review. Cardiol. Rev. 2011, 19, 202. [Google Scholar] [CrossRef]
- Firefighter Fatalities in the United States. Available online: https://www.usfa.fema.gov/statistics/reports/firefighters-departments/firefighter-fatalities.html (accessed on 19 June 2024).
- Kopp, W. How Western Diet And Lifestyle Drive The Pandemic Of Obesity And Civilization Diseases. DMSO 2019, 12, 2221–2236. [Google Scholar] [CrossRef]
- Manzel, A.; Muller, D.N.; Hafler, D.A.; Erdman, S.E.; Linker, R.A.; Kleinewietfeld, M. Role of “Western Diet” in Inflammatory Autoimmune Diseases. Curr. Allergy Asthma Rep. 2013, 14, 404. [Google Scholar] [CrossRef]
- Grotto, D.; Zied, E. The standard American diet and its relationship to the health status of Americans. Nutr. Clin. Pract. 2010, 25, 603–612. [Google Scholar] [CrossRef]
- Kales, S.N.; Tsismenakis, A.J.; Zhang, C.; Soteriades, E.S. Blood pressure in firefighters, police officers, and other emergency responders. Am. J. Hypertens. 2009, 22, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Carey, M.G.; Al-Zaiti, S.S.; Dean, G.E.; Sessanna, L.; Finnell, D.S. Sleep Problems, Depression, Substance Use, Social Bonding, and Quality of Life in Professional Firefighters. J. Occup. Environ. Med. 2011, 53, 928. [Google Scholar] [CrossRef] [PubMed]
- Garbarino, S.; de Carli, F.; Nobili, L.; Mascialino, B.; Squarcia, S.; Penco, M.A.; Beelke, M.; Ferrillo, F. Sleepiness and Sleep Disorders in Shift Workers: A Study on a Group of Italian Police Officers. Sleep 2002, 25, 642–647. [Google Scholar] [CrossRef]
- Paoli, A.; Tinsley, G.; Bianco, A.; Moro, T. The Influence of Meal Frequency and Timing on Health in Humans: The Role of Fasting. Nutrients 2019, 11, 719. [Google Scholar] [CrossRef] [PubMed]
- Panda, S. Circadian physiology of metabolism. Science 2016, 354, 1008–1015. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Ramsey, K.M.; Marcheva, B.; Bass, J. Circadian Rhythms, Sleep, and Metabolism. J. Clin. Investig. 2011, 121, 2133–2141. [Google Scholar] [CrossRef] [PubMed]
- Eckel-Mahan, K.; Sassone-Corsi, P. Metabolism and the Circadian Clock Converge. Physiol. Rev. 2013, 93, 107–135. [Google Scholar] [CrossRef] [PubMed]
- Lowden, A.; Moreno, C.; Holmbäck, U.; Lennernäs, M.; Tucker, P. Eating and shift work—Effects on habits, metabolism, and performance. Scand. J. Work Enviorn. Health. 2010, 36, 150–162. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Martínez-González, M.Á.; Corella, D.; Salas-Salvadó, J.; Ruiz-Gutiérrez, V.; Covas, M.I.; Fiol, M.; Gómez-Gracia, E.; López-Sabater, M.C.; Vinyoles, E.; et al. Effects of a Mediterranean-Style Diet on Cardiovascular Risk Factors. Ann. Intern. Med. 2006, 145, 1–11. [Google Scholar] [CrossRef]
- Siervo, M.; Lara, J.; Chowdhury, S.; Ashor, A.; Oggioni, C.; Mathers, J.C. Effects of the Dietary Approach to Stop Hypertension (DASH) Diet on Cardiovascular Risk Factors: A Systematic Review and Meta-Analysis. Br. J. Nutr. 2015, 113, 1–15. [Google Scholar] [CrossRef]
- Lairon, D. Intervention Studies on Mediterranean Diet and Cardiovascular Risk. Mol. Nutr. Food Res. 2007, 51, 1209–1214. [Google Scholar] [CrossRef]
- Matthews, C.E.; Hebert, J.R.; Ockene, I.S.; Saperia, G.; Merriam, P.A. Relationship between Leisure-Time Physical Activity and Selected Dietary Variables in the Worcester Area Trial for Counseling in Hyperlipidemia. Med. Sci. Sports Exerc. 1997, 29, 1199–1207. [Google Scholar] [CrossRef]
- Eaton, C.B.; McPhillips, J.B.; Gans, K.M.; Garber, C.E.; Assaf, A.R.; Lasater, T.M.; Carleton, R.A. Cross-Sectional Relationship Between Diet and Physical Activity in Two Southeastern New England Communities. Am. J. Prev. Med. 1995, 11, 238–244. [Google Scholar] [CrossRef]
- D’Agostino Sr, R.B.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef]
- Liguori, G.; American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription, 11th ed.; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2021; 541p. [Google Scholar]
- Servings from Each Food Group. Available online: https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/nutrition-basics/suggested-servings-from-each-food-group. (accessed on 19 June 2024).
- Gendron, P.; Lajoie, C.; Laurencelle, L.; Trudeau, F. Cardiovascular disease risk factors in Québec male firefighters. J. Occup. Environ. Med. 2018, 60, e300–e306. [Google Scholar] [CrossRef]
- Bode, E.D.; Mathias, K.C.; Steward, D.F.; Moffatt, S.M.; Jack, K.; Smith, D.L. Cardiovascular disease risk factors by BMI and age in United States firefighters. Obesity 2021, 29, 1186–1194. [Google Scholar] [CrossRef]
- Smith, D.L.; Fehling, P.C.; Frisch, A.; Haller, J.M.; Winke, M.; Dailey, M.W. The Prevalence of Cardiovascular Disease Risk Factors and Obesity in Firefighters. J. Obes. 2012, 2012, 908267. [Google Scholar] [CrossRef]
- Fahs, C.A.; Smith, D.L.; Horn, G.P.; Agiovlasitis, S.; Rossow, L.M.; Echols, G.; Heffernan, K.S.; Fernhall, B. Impact of Excess Body Weight on Arterial Structure, Function, and Blood Pressure in Firefighters. Am. J. Cardiol. 2009, 104, 1441–1445. [Google Scholar] [CrossRef]
- Garver, J.N.; Jankovitz, K.Z.; Danks, J.M.; Fittz, A.A.; Smith, H.S.; Davis, S.C. PHYSICAL FITNESS OF AN INDUSTRIAL FIRE DEPARTMENT VS. A MUNICIPAL FIRE DEPARTMENT. J. Strength Cond. Res. 2005, 19, 310. [Google Scholar]
- Kales, S.N.; Aldrich, J.M.; Polyhronopoulos, G.N.; Leitao, E.O.; Artzerounian, D.; Gassert, T.H.; Hu, H.; Kelsey, K.T.; Sweet, C.; Christiani, D.C. Correlates of fitness for duty in hazardous materials firefighters. Am. J. Ind. Med. 1999, 36, 618–629. [Google Scholar] [CrossRef]
- Lemon, P.W.R.; Hermiston, R.T. Physiological Profile of Professional Fire Fighters. J. Occup. Med. 1977, 19, 337–340. [Google Scholar]
- Poston, W.S.C.; Haddock, C.K.; Jahnke, S.A.; Jitnarin, N.; Tuley, B.C.; Kales, S.N. The Prevalence of Overweight, Obesity, and Substandard Fitness in a Population-Based Firefighter Cohort. J. Occup. Environ. Med. 2011, 53, 266. [Google Scholar] [CrossRef]
- Iqbal, R.; Dehghan, M.; Mente, A.; Rangarajan, S.; Wielgosz, A.; Avezum, A.; Seron, P.; AlHabib, K.F.; Lopez-Jaramillo, P.; Swaminathan, S.; et al. Associations of Unprocessed and Processed Meat Intake with Mortality and Cardiovascular Disease in 21 Countries [Prospective Urban Rural Epidemiology (PURE) Study]: A Prospective Cohort Study. Am. J. Clin. Nutr. 2021, 114, 1049–1058. [Google Scholar] [CrossRef]
- Jakobsen, M.U.; Bysted, A.; Mejborn, H.; Stockmarr, A.; Trolle, E. Intake of Unprocessed and Processed Meat and the Association with Cardiovascular Disease: An Overview of Systematic Reviews. Nutrients 2021, 13, 3303. [Google Scholar] [CrossRef]
- O’Connor, L.E.; Kim, J.E.; Campbell, W.W. Total Red Meat Intake of ≥0.5 Servings/d Does Not Negatively Influence Cardiovascular Disease Risk Factors: A Systemically Searched Meta-Analysis of Randomized Controlled Trials12. Am. J. Clin. Nutr. 2017, 105, 57–69. [Google Scholar] [CrossRef]
- Zhong, V.W.; Van Horn, L.; Greenland, P.; Carnethon, M.R.; Ning, H.; Wilkins, J.T.; Lloyd-Jones, D.M.; Allen, N.B. Associations of Processed Meat, Unprocessed Red Meat, Poultry, or Fish Intake With Incident Cardiovascular Disease and All-Cause Mortality. JAMA Intern. Med. 2020, 180, 503–512. [Google Scholar] [CrossRef]
- Gonzalez, D.E.; McAllister, M.J.; Waldman, H.S.; Ferrando, A.A.; Joyce, J.; Barringer, N.D.; Dawes, J.J.; Kieffer, A.J.; Harvey, T.; Kerksick, C.M.; et al. International society of sports nutrition position stand: Tactical athlete nutrition. J. Int. Soc. Sports Nutr. 2022, 19, 267–315. [Google Scholar] [CrossRef]
- Korre, M.; Sotos-Prieto, M.; Kales, S.N. Survival Mediterranean style: Lifestyle changes to improve the health of the US fire service. Public Health Front. 2017, 5, 331. [Google Scholar] [CrossRef]
- Sotos-Prieto, M.; Cash, S.B.; Christophi, C.A.; Folta, S.; Moffatt, S.; Muegge, C.; Korre, M.; Mozaffarian, D.; Kales, S.N. Rationale and Design of Feeding America’s Bravest: Mediterranean Diet-Based Intervention to Change Firefighters’ Eating Habits and Improve Cardiovascular Risk Profiles. Contemp. Clin. Trials 2017, 61, 101–107. [Google Scholar] [CrossRef]
- Gill, R.; Superko, H.R.; McCarthy, M.M.; Jack, K.; Jones, B.; Ghosh, D.; Richards, S.; Gleason, J.A.; Williams, P.T.; Dansinger, M. Cardiovascular Risk Factor Reduction in First Responders Resulting From an Individualized Lifestyle and Blood Test Program: A Randomized Controlled Trial. J. Occup. Environ. Med. 2019, 61, 183. [Google Scholar] [CrossRef]
- Bailey, R.L. Overview of dietary assessment methods for measuring intakes of foods, beverages, and dietary supplements in research studies. Curr. Opin. Biotechnol. 2021, 70, 91–96. [Google Scholar] [CrossRef]
- Hong, O.; Fiola, L.A.; Feld, J. Challenges and successes in recruiting firefighters for hearing loss prevention research. Workplace Health Saf. 2013, 61, 257–263. [Google Scholar] [CrossRef]

| Firefighters (Mean ± SD) (n = 46) | |
|---|---|
| Age (years) | 41.2 ± 11.2 |
| Years of Service (years) | 16.9 ± 10.2 |
| BMI (kg/m2) | 29.2 ± 4.1 |
| Body Fat (%) | 21.7 ± 6.1 |
| Resting Blood Pressure | |
| Systolic (mmHg) | 140.2 ± 14.1 |
| Diastolic (mmHg) | 82.5 ± 10.9 |
| Dietary Intake (n = 46) | Mean ± SD or Percentage (%) |
|---|---|
| Servings of Meat per Week | 8.3 ± 2.0 |
| Servings of Meat per Day | 3.6 ± 1.4 |
| Servings of Red Meat per Week | 4.2 ± 2.3 |
| Servings of Seafood per Week | 2.5 ± 1.6 |
| Servings of Nuts/Seeds/Legumes per Week | 4.7 ± 2.1 |
| Servings of Dairy per Day | 2.1 ± 0.7 |
| Servings of Fruit per Day | 2.7 ± 1.1 |
| Servings of Vegetables per Day | 3.4 ± 1.2 |
| Plant vs. Animal Cooking Fat | 89.1% Animal |
| CVD Risk Components (n = 46) | Mean ± SD or Percentage (%) |
|---|---|
| CVD Risk (%) | 9.7% ± 6.5% |
| Vascular Age (years) | 49.7 ± 12.5 |
| CVD Risk Category | |
| Low | 60.0% |
| Moderate | 33.3% |
| High | 6.7% |
| Independent Variables | β | βstd 1 | p-Value |
|---|---|---|---|
| Y-Intercept | 26.6 | 5.3 | <0.000 |
| Servings of Meat per Week | −1.4 | 0.4 | 0.003 |
| Plant vs. Animal Cooking Fat | −4.6 | −1.6 | 0.111 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simonson, A.P.; Zera, J.N.; Banerjee, P.; Baker, B.M. Associations between Dietary Intake and Cardiovascular Disease Risk in American Career Firefighters: An Observational Study. J. Funct. Morphol. Kinesiol. 2024, 9, 132. https://doi.org/10.3390/jfmk9030132
Simonson AP, Zera JN, Banerjee P, Baker BM. Associations between Dietary Intake and Cardiovascular Disease Risk in American Career Firefighters: An Observational Study. Journal of Functional Morphology and Kinesiology. 2024; 9(3):132. https://doi.org/10.3390/jfmk9030132
Chicago/Turabian StyleSimonson, Anna Peluso, Jacquelyn N. Zera, Paromita Banerjee, and Brianne M. Baker. 2024. "Associations between Dietary Intake and Cardiovascular Disease Risk in American Career Firefighters: An Observational Study" Journal of Functional Morphology and Kinesiology 9, no. 3: 132. https://doi.org/10.3390/jfmk9030132
APA StyleSimonson, A. P., Zera, J. N., Banerjee, P., & Baker, B. M. (2024). Associations between Dietary Intake and Cardiovascular Disease Risk in American Career Firefighters: An Observational Study. Journal of Functional Morphology and Kinesiology, 9(3), 132. https://doi.org/10.3390/jfmk9030132








