Short-Term Benefits from Manual Therapy as an Adjunct Treatment for Persistent Postural-Perceptual Dizziness Symptoms: A Preliminary Prospective Case Series
Abstract
1. Introduction
2. Case Presentations
2.1. Case Series Study Design
2.2. Subjects: Cases
2.3. Examination: Outcome Measures
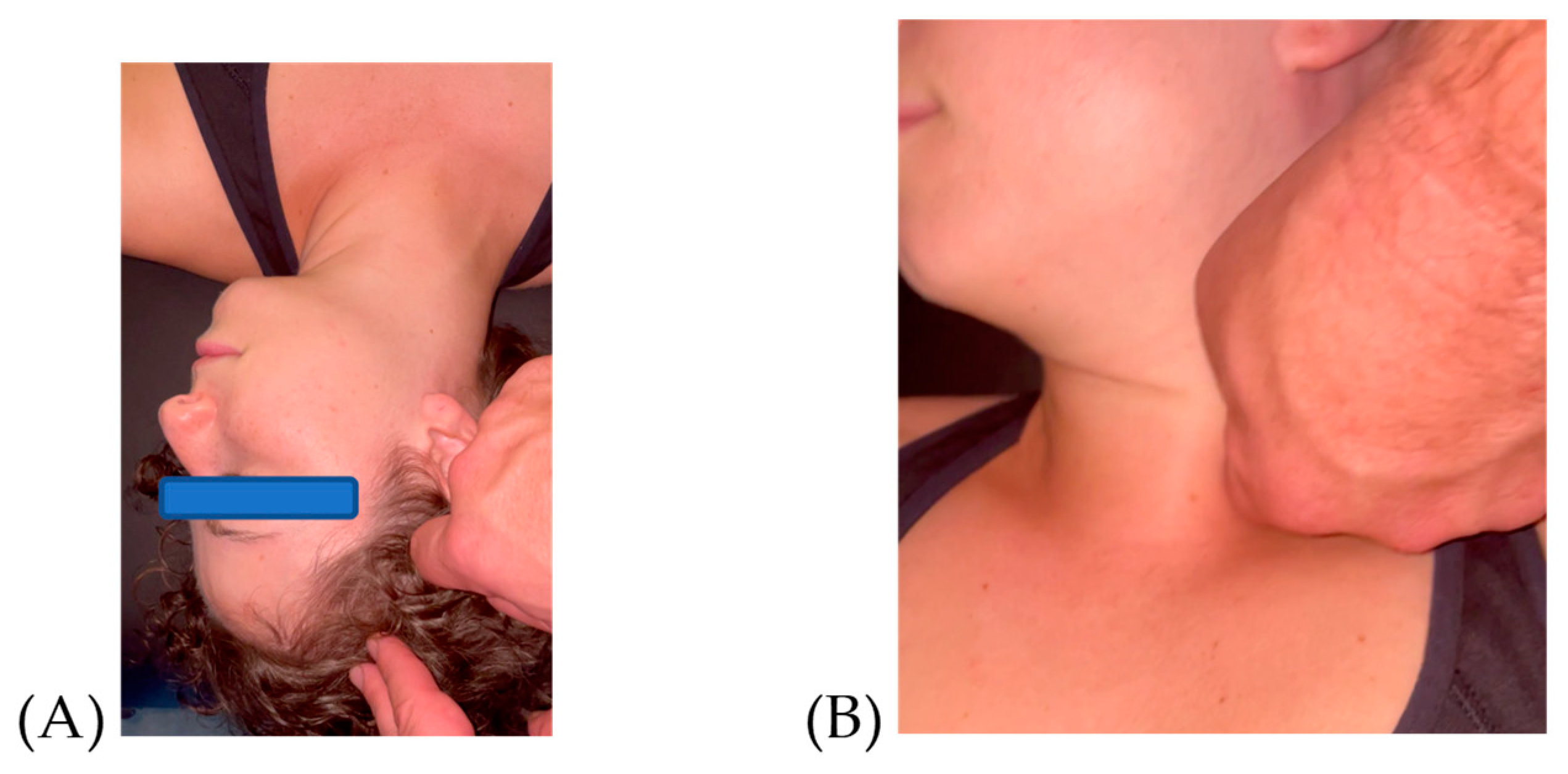
2.4. Plan of Care: Manual Therapy Intervention
2.5. Plan of Care: Home Exercise Program
2.6. Statistical Analysis
3. Case Presentations: Outcomes before and after Intervention
3.1. Subjects: Cases
3.2. Number of Visits
3.3. Dizziness Handicap Inventory
3.4. Timed up and Go
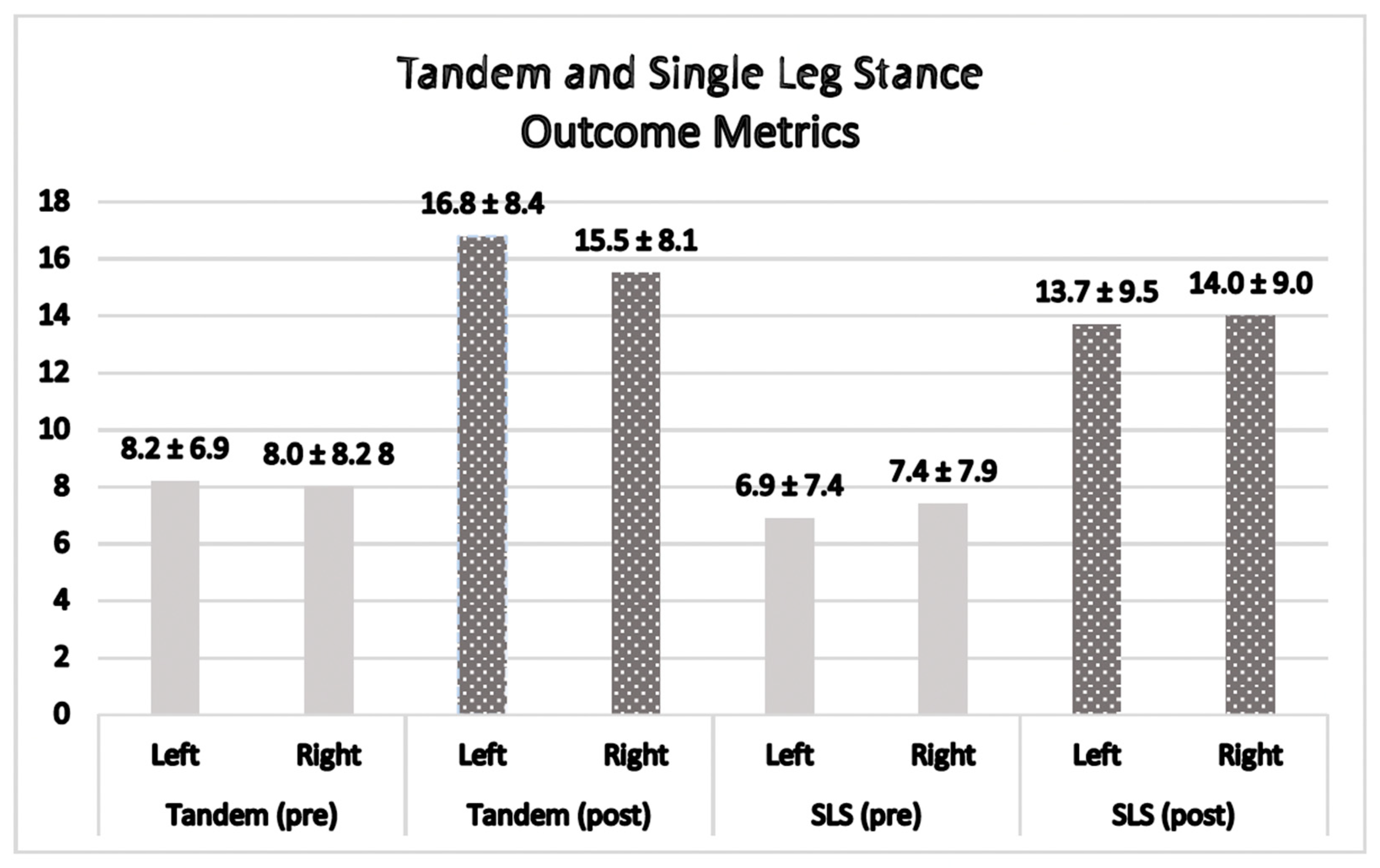
3.5. Tandem Stance
3.6. Single Limb Stance
4. Discussion
4.1. The Effect of Manual Therapy on Each Metric in This Case Series
4.2. Importance of Adding Non-Pharmacological Interventions for 3PD
4.3. Value of Clinical Balance Assessments
4.4. Prior Research Supporting the Soft Tissue Intervention
4.5. How Changes Might Have Occurred after FM®
4.6. Limiting other Potential Pain Generators for Continued Symptoms
4.7. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| PPPD: A chronic vestibular disorder defined by the five criteria items below. All five must be met to make the diagnosis. |
|
|
|
|
|
Appendix B
- Appendix B. Constructs of the Fascial Manipulation® Method of Soft Tissue Tangential Oscillations.
References
- Agrawal, Y.; Carey, J.P.; Della Santina, C.C.; Schubert, M.C.; Minor, L.B. Disorders of balance and vestibular function in US adults: Data from the National Health and Nutrition Examination Survey, 2001–2004. Arch. Intern. Med. 2009, 169, 938–944. [Google Scholar] [CrossRef] [PubMed]
- Bisdorff, A.; Von Brevern, M.; Lempert, T.; Newman-Toker, D.E. Classification of vestibular symptoms: Towards an international classification of vestibular disorders. J. Vestib. Res. 2009, 19, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Staab, J.P. Chronic subjective dizziness. Continuum 2012, 18, 1118–1141. [Google Scholar] [CrossRef] [PubMed]
- Azzi, J.L.; Khoury, M.; Séguin, J.; Rourke, R.; Hogan, D.; Tse, D.; Lelli, D.A. Characteristics of persistent postural perceptual dizziness patients in a multidisciplinary dizziness clinic. J. Vestib. Res. 2022, 32, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Holle, D.; Schulte-Steinberg, B.; Wurthmann, S.; Naegel, S.; Ayzenberg, I.; Diener, H.C.; Katsarava, Z.; Obermann, M. Persistent Postural-Perceptual Dizziness: A Matter of Higher, Central Dysfunction? PLoS ONE 2015, 10, e0142468. [Google Scholar] [CrossRef] [PubMed]
- Staab, J.P.; Eckhardt-Henn, A.; Horii, A.; Jacob, R.; Strupp, M.; Brandt, T.; Bronstein, A. Diagnostic criteria for persistent postural-perceptual dizziness (PPPD): Consensus document of the committee for the Classification of Vestibular Disorders of the Barany Society. J. Vestib. Res. 2017, 27, 191–208. [Google Scholar] [CrossRef] [PubMed]
- Popkirov, S.; Stone, J.; Holle-Lee, D. Treatment of Persistent Postural-Perceptual Dizziness (PPPD) and Related Disorders. Curr. Treat. Options Neurol. 2018, 20, 50. [Google Scholar] [CrossRef] [PubMed]
- Popkirov, S.; Staab, J.P.; Stone, J. Persistent postural-perceptual dizziness (PPPD): A common, characteristic and treatable cause of chronic dizziness. Pract. Neurol. 2018, 18, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Si, L.; Cui, B.; Ling, X.; Shen, B.; Yang, X. Altered spontaneous functional activity of the right precuneus and cuneus in patients with persistent postural-perceptual dizziness. Brain Imaging Behav. 2020, 14, 2176–2186. [Google Scholar] [CrossRef]
- Staab, J.P. Persistent Postural-Perceptual Dizziness. Semin. Neurol. 2020, 40, 130–137. [Google Scholar] [CrossRef]
- Muelleman, T.; Shew, M.; Subbarayan, R.; Shum, A.; Sykes, K.; Staecker, H.; Lin, J. Epidemiology of Dizzy Patient Population in a Neurotology Clinic and Predictors of Peripheral Etiology. Otol. Neurotol. 2017, 38, 870–875. [Google Scholar] [CrossRef] [PubMed]
- Staibano, P.; Lelli, D.; Tse, D. A retrospective analysis of two tertiary care dizziness clinics: A multidisciplinary chronic dizziness clinic and an acute dizziness clinic. J. Otolaryngol. Head Neck Surg. 2019, 48, 11. [Google Scholar] [CrossRef] [PubMed]
- Gazzola, J.M.; Gananca, F.F.; Aratani, M.C.; Perracini, M.R.; Gananca, M.M. Circumstances and consequences of falls in elderly people with vestibular disorder. Braz. J. Otorhinolaryngol. 2006, 72, 388–392. [Google Scholar] [CrossRef] [PubMed]
- Baloh, R.W. Vestibular and auditory disorders. Curr. Opin. Neurol. 1996, 9, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Brandt, T.; Daroff, R.B. Physical therapy for benign paroxysmal positional vertigo. Arch. Otolaryngol. 1980, 106, 484–485. [Google Scholar] [CrossRef] [PubMed]
- Kao, C.L.; Hsieh, W.L.; Chern, C.M.; Chen, L.K.; Lin, M.H.; Chan, R.C. Clinical features of benign paroxysmal positional vertigo (BPPV) in Taiwan: Differences between young and senior age groups. Arch. Gerontol. Geriatr. 2009, 49 (Suppl. S2), S50–S54. [Google Scholar] [CrossRef] [PubMed]
- Axer, H.; Finn, S.; Wassermann, A.; Guntinas-Lichius, O.; Klingner, C.M.; Witte, O.W. Multimodal treatment of persistent postural-perceptual dizziness. Brain Behav. 2020, 10, e01864. [Google Scholar] [CrossRef]
- Pfeiffer, C.; Serino, A.; Blanke, O. The vestibular system: A spatial reference for bodily self-consciousness. Front. Integr. Neurosci. 2014, 8, 31. [Google Scholar] [CrossRef]
- Wiesmeier, I.K.; Dalin, D.; Maurer, C. Elderly Use Proprioception Rather than Visual and Vestibular Cues for Postural Motor Control. Front. Aging Neurosci. 2015, 7, 97. [Google Scholar] [CrossRef]
- Mense, S. Innervation of the thoracolumbar fascia. Eur. J. Transl. Myol. 2019, 29, 8297. [Google Scholar] [CrossRef]
- Stecco, C.; Pirri, C.; Fede, C.; Fan, C.; Giordani, F.; Stecco, L.; Foti, C.; De Caro, R. Dermatome and fasciatome. Clin. Anat. 2019, 32, 896–902. [Google Scholar] [CrossRef] [PubMed]
- Stecco, C.; Porzionato, A.; Lancerotto, L.; Stecco, A.; Macchi, V.; Day, J.A.; De Caro, R. Histological study of the deep fasciae of the limbs. J. Bodyw. Mov. Ther. 2008, 12, 225–230. [Google Scholar] [CrossRef]
- Chu, E.C.P.; Chin, W.L.; Bhaumik, A. Cervicogenic dizziness. Oxf. Med. Case Reports 2019, 2019, 476–478. [Google Scholar] [CrossRef] [PubMed]
- Reiley, A.S.; Vickory, F.M.; Funderburg, S.E.; Cesario, R.A.; Clendaniel, R.A. How to diagnose cervicogenic dizziness. Arch. Physiother. 2017, 7, 12. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, G.P.; Newman, C.W. The development of the Dizziness Handicap Inventory. Arch. Otolaryngol. Head Neck Surg. 1990, 116, 424–427. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, G.P.; Calder, J.H. A screening version of the Dizziness Handicap Inventory (DHI-S). Am. J. Otol. 1998, 19, 804–808. [Google Scholar]
- Steffen, T.M.; Hacker, T.A.; Mollinger, L. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys. Ther. 2002, 82, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Lin, M.R.; Hwang, H.F.; Hu, M.H.; Wu, H.D.; Wang, Y.W.; Huang, F.C. Psychometric comparisons of the timed up and go, one-leg stand, functional reach, and Tinetti balance measures in community-dwelling older people. J. Am. Geriatr. Soc. 2004, 52, 1343–1348. [Google Scholar] [CrossRef]
- Franchignoni, F.; Tesio, L.; Martino, M.T.; Ricupero, C. Reliability of four simple, quantitative tests of balance and mobility in healthy elderly females. Aging (Milano) 1998, 10, 26–31. [Google Scholar] [CrossRef]
- Giorgetti, M.M.; Harris, B.A.; Jette, A. Reliability of clinical balance outcome measures in the elderly. Physiother. Res. Int. 1998, 3, 274–283. [Google Scholar] [CrossRef] [PubMed]
- Kozinc, Z.; Lofler, S.; Hofer, C.; Carraro, U.; Sarabon, N. Diagnostic Balance Tests for Assessing Risk of Falls and Distinguishing Older Adult Fallers and Non-Fallers: A Systematic Review with Meta-Analysis. Diagnostics 2020, 10, 667. [Google Scholar] [CrossRef] [PubMed]
- Hile, E.S.; Brach, J.S.; Perera, S.; Wert, D.M.; VanSwearingen, J.M.; Studenski, S.A. Interpreting the need for initial support to perform tandem stance tests of balance. Phys. Ther. 2012, 92, 1316–1328. [Google Scholar] [CrossRef] [PubMed]
- Stecco, L. Fascial Manipulation® Practical Part—First Level, 2nd ed.; Piccin: São Carlos, Brazil, 2018. [Google Scholar]
- Cotti, A.; Del Corso, M.; Diana, R.; Cornale, L.; Sudanese, A.; Stecco, A.; Branchini, M. Inter and Intra Operator Reliability of Motor and Palpation Evaluation in Fascial Manipulation in individuals with coxarthrosis. J. Man. Manip. Ther. 2020, 28, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Bertoldo, D.; Pirri, C.; Roviaro, B.; Stecco, L.; Day, J.A.; Fede, C.; Guidolin, D.; Stecco, C. Pilot Study of Sacroiliac Joint Dysfunction Treated with a Single Session of Fascial Manipulation((R)) Method: Clinical Implications for Effective Pain Reduction. Medicina 2021, 57, 691. [Google Scholar] [CrossRef] [PubMed]
- Day, J.A.; Copetti, L.; Rucli, G. From clinical experience to a model for the human fascial system. J. Bodyw. Mov. Ther. 2012, 16, 372–380. [Google Scholar] [CrossRef] [PubMed]
- Ercole, B.; Antonio, S.; Julie Ann, D.; Stecco, C. How much time is required to modify a fascial fibrosis? J. Bodyw. Mov. Ther. 2010, 14, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Day, J.A.; Stecco, C.; Stecco, A. Application of Fascial Manipulation technique in chronic shoulder pain--anatomical basis and clinical implications. J. Bodyw. Mov. Ther. 2009, 13, 128–135. [Google Scholar] [CrossRef]
- Harper, B.; Steinbeck, L.; Aron, A. Fascial manipulation vs. standard physical therapy practice for low back pain diagnoses: A pragmatic study. J. Bodyw. Mov. Ther. 2019, 23, 115–121. [Google Scholar] [CrossRef]
- Whitney, S.L.; Wrisley, D.M.; Brown, K.E.; Furman, J.M. Is perception of handicap related to functional performance in persons with vestibular dysfunction? Otol. Neurotol. 2004, 25, 139–143. [Google Scholar] [CrossRef]
- Gunter, K.B.; White, K.N.; Hayes, W.C.; Snow, C.M. Functional mobility discriminates nonfallers from one-time and frequent fallers. J. Gerontol. A Biol. Sci. Med. Sci. 2000, 55, M672–M676. [Google Scholar] [CrossRef]
- Brown, K.E.; Whitney, S.L.; Wrisley, D.M.; Furman, J.M. Physical therapy outcomes for persons with bilateral vestibular loss. Laryngoscope 2001, 111, 1812–1817. [Google Scholar] [CrossRef] [PubMed]
- Kear, B.M.; Guck, T.P.; McGaha, A.L. Timed Up and Go (TUG) Test: Normative Reference Values for Ages 20 to 59 Years and Relationships With Physical and Mental Health Risk Factors. J. Prim. Care Community Health 2017, 8, 9–13. [Google Scholar] [CrossRef]
- Goldberg, A.; Casby, A.; Wasielewski, M. Minimum detectable change for single-leg-stance-time in older adults. Gait Posture 2011, 33, 737–739. [Google Scholar] [CrossRef]
- Ries, J.D.; Echternach, J.L.; Nof, L.; Gagnon Blodgett, M. Test-retest reliability and minimal detectable change scores for the timed “up & go” test, the six-minute walk test, and gait speed in people with Alzheimer disease. Phys. Ther. 2009, 89, 569–579. [Google Scholar] [CrossRef] [PubMed]
- Marques, A.; Cruz, J.; Quina, S.; Regencio, M.; Jacome, C. Reliability, Agreement and Minimal Detectable Change of the Timed Up & Go and the 10-Meter Walk Tests in Older Patients with COPD. COPD 2016, 13, 279–287. [Google Scholar] [CrossRef]
- Quinn, G.; Comber, L.; McGuigan, C.; Galvin, R.; Coote, S. Discriminative ability and clinical utility of the Timed Up and Go (TUG) in identifying falls risk in people with multiple sclerosis: A prospective cohort study. Clin. Rehabil. 2019, 33, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Nigro, S.; Indovina, I.; Riccelli, R.; Chiarella, G.; Petrolo, C.; Lacquaniti, F.; Staab, J.P.; Passamonti, L. Reduced cortical folding in multi-modal vestibular regions in persistent postural perceptual dizziness. Brain Imaging Behav. 2019, 13, 798–809. [Google Scholar] [CrossRef]
- Trinidade, A.; Goebel, J.A. Persistent Postural-Perceptual Dizziness-A Systematic Review of the Literature for the Balance Specialist. Otol. Neurotol. 2018, 39, 1291–1303. [Google Scholar] [CrossRef]
- Pedrelli, A.; Stecco, C.; Day, J.A. Treating patellar tendinopathy with Fascial Manipulation. J. Bodyw. Mov. Ther. 2009, 13, 73–80. [Google Scholar] [CrossRef]
- Stecco, A.; Stecco, C.; Macchi, V.; Porzionato, A.; Ferraro, C.; Masiero, S.; De Caro, R. RMI study and clinical correlations of ankle retinacula damage and outcomes of ankle sprain. Surg. Radiol. Anat. 2011, 33, 881–890. [Google Scholar] [CrossRef] [PubMed]
- Picelli, A.; Ledro, G.; Turrina, A.; Stecco, C.; Santilli, V.; Smania, N. Effects of myofascial technique in patients with subacute whiplash associated disorders: A pilot study. Eur. J. Phys. Rehabil. Med. 2011, 47, 561–568. [Google Scholar] [PubMed]
- Gdowski, G.T.; McCrea, R.A. Integration of vestibular and head movement signals in the vestibular nuclei during whole-body rotation. J. Neurophysiol. 1999, 82, 436–449. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Arumugam, K.; Harikesavan, K. Effectiveness of fascial manipulation on pain and disability in musculoskeletal conditions. A systematic review. J. Bodyw. Mov. Ther. 2021, 25, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Brandolini, S.; Lugaresi, G.; Santagata, A.; Ermolao, A.; Zaccaria, M.; Marchand, A.M.; Stecco, A. Sport injury prevention in individuals with chronic ankle instability: Fascial Manipulation((R)) versus control group: A randomized controlled trial. J. Bodyw. Mov. Ther. 2019, 23, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Espi-Lopez, G.V.; Lopez-Martinez, S.; Ingles, M.; Serra-Ano, P.; Aguilar-Rodriguez, M. Effect of manual therapy versus proprioceptive neuromuscular facilitation in dynamic balance, mobility and flexibility in field hockey players. A randomized controlled trial. Phys. Ther. Sport. 2018, 32, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Sawamura, S.; Mikami, A. Effect of fascial Manipulation(R) on reaction time. J. Bodyw. Mov. Ther. 2020, 24, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Foster, C.A.; Jabbour, P. Barre-Lieou syndrome and the problem of the obsolete eponym. J. Laryngol. Otol. 2007, 121, 680–683. [Google Scholar] [CrossRef]
- Brandt, T.; Bronstein, A.M. Cervical vertigo. J. Neurol. Neurosurg. Psychiatry 2001, 71, 8–12. [Google Scholar] [CrossRef]
- Brandt, T. Cervical vertigo--reality or fiction? Audiol. Neurootol. 1996, 1, 187–196. [Google Scholar] [CrossRef]
- Willard, F.H.; Vleeming, A.; Schuenke, M.D.; Danneels, L.; Schleip, R. The thoracolumbar fascia: Anatomy, function and clinical considerations. J. Anat. 2012, 221, 507–536. [Google Scholar] [CrossRef]
- Schilder, A.; Hoheisel, U.; Magerl, W.; Benrath, J.; Klein, T.; Treede, R.D. Sensory findings after stimulation of the thoracolumbar fascia with hypertonic saline suggest its contribution to low back pain. Pain 2014, 155, 222–231. [Google Scholar] [CrossRef]
- Stecco, C.; Stern, R.; Porzionato, A.; Macchi, V.; Masiero, S.; Stecco, A.; De Caro, R. Hyaluronan within fascia in the etiology of myofascial pain. Surg. Radiol. Anat. 2011, 33, 891–896. [Google Scholar] [CrossRef]
- Amir, A.; Kim, S.; Stecco, A.; Jankowski, M.P.; Raghavan, P. Hyaluronan homeostasis and its role in pain and muscle stiffness. PM&R 2022, 14, 1490–1496. [Google Scholar] [CrossRef] [PubMed]
- Pavan, P.G.; Stecco, A.; Stern, R.; Stecco, C. Painful connections: Densification versus fibrosis of fascia. Curr. Pain. Headache Rep. 2014, 18, 441. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, B.; Li, Y.; Thayer, S.A. Inhibition of the plasma membrane Ca2+ pump by CD44 receptor activation of tyrosine kinases increases the action potential afterhyperpolarization in sensory neurons. J. Neurosci. 2011, 31, 2361–2370. [Google Scholar] [CrossRef]
- Kobayashi, T.; Chanmee, T.; Itano, N. Hyaluronan: Metabolism and Function. Biomolecules 2020, 10, 1525. [Google Scholar] [CrossRef] [PubMed]
- Valachova, K.; Soltes, L. Hyaluronan as a Prominent Biomolecule with Numerous Applications in Medicine. Int. J. Mol. Sci. 2021, 22, 7077. [Google Scholar] [CrossRef]
- Cowman, M.K.; Schmidt, T.A.; Raghavan, P.; Stecco, A. Viscoelastic Properties of Hyaluronan in Physiological Conditions. F1000Research 2015, 4, 622. [Google Scholar] [CrossRef]
- Raghavan, P.; Lu, Y.; Mirchandani, M.; Stecco, A. Human Recombinant Hyaluronidase Injections For Upper Limb Muscle Stiffness in Individuals With Cerebral Injury: A Case Series. EBioMedicine 2016, 9, 306–313. [Google Scholar] [CrossRef]
- Chaudhry, H.; Bukiet, B.; Roman, M.; Stecco, A.; Findley, T. Squeeze film lubrication for non-Newtonian fluids with application to manual medicine. Biorheology 2013, 50, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Roman, M.; Chaudhry, H.; Bukiet, B.; Stecco, A.; Findley, T.W. Mathematical analysis of the flow of hyaluronic acid around fascia during manual therapy motions. J. Am. Osteopath. Assoc. 2013, 113, 600–610. [Google Scholar] [CrossRef] [PubMed]
- Fraix, M.; Gordon, A.; Graham, V.; Hurwitz, E.; Seffinger, M.A. Use of the SMART Balance Master to quantify the effects of osteopathic manipulative treatment in patients with dizziness. J. Am. Osteopath. Assoc. 2013, 113, 394–403. [Google Scholar] [PubMed]
- Louw, A.; Puentedura, E.J.; Schmidt, S.; Zimney, K. Therapeutic Neuroscience Education: Teaching People about Pain, 2nd ed.; OPTP: Minneapolis, MN, USA, 2018. [Google Scholar]
- Vlaeyen, J.W.S.; Linton, S.J. Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain 2000, 85, 317–332. [Google Scholar] [CrossRef] [PubMed]
- Breinbauer, H.A.; Contreras, M.D.; Lira, J.P.; Guevara, C.; Castillo, L.; Ruedlinger, K.; Munoz, D.; Delano, P.H. Spatial Navigation Is Distinctively Impaired in Persistent Postural Perceptual Dizziness. Front. Neurol. 2019, 10, 1361. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harper, B.A.; Steinbeck, L. Short-Term Benefits from Manual Therapy as an Adjunct Treatment for Persistent Postural-Perceptual Dizziness Symptoms: A Preliminary Prospective Case Series. J. Funct. Morphol. Kinesiol. 2024, 9, 82. https://doi.org/10.3390/jfmk9020082
Harper BA, Steinbeck L. Short-Term Benefits from Manual Therapy as an Adjunct Treatment for Persistent Postural-Perceptual Dizziness Symptoms: A Preliminary Prospective Case Series. Journal of Functional Morphology and Kinesiology. 2024; 9(2):82. https://doi.org/10.3390/jfmk9020082
Chicago/Turabian StyleHarper, Brent A., and Larry Steinbeck. 2024. "Short-Term Benefits from Manual Therapy as an Adjunct Treatment for Persistent Postural-Perceptual Dizziness Symptoms: A Preliminary Prospective Case Series" Journal of Functional Morphology and Kinesiology 9, no. 2: 82. https://doi.org/10.3390/jfmk9020082
APA StyleHarper, B. A., & Steinbeck, L. (2024). Short-Term Benefits from Manual Therapy as an Adjunct Treatment for Persistent Postural-Perceptual Dizziness Symptoms: A Preliminary Prospective Case Series. Journal of Functional Morphology and Kinesiology, 9(2), 82. https://doi.org/10.3390/jfmk9020082





