Comparing the Effects of Multicomponent and Concurrent Exercise Protocols on Muscle Strength in Older Adults
Abstract
:1. Introduction
2. Materials and Methods
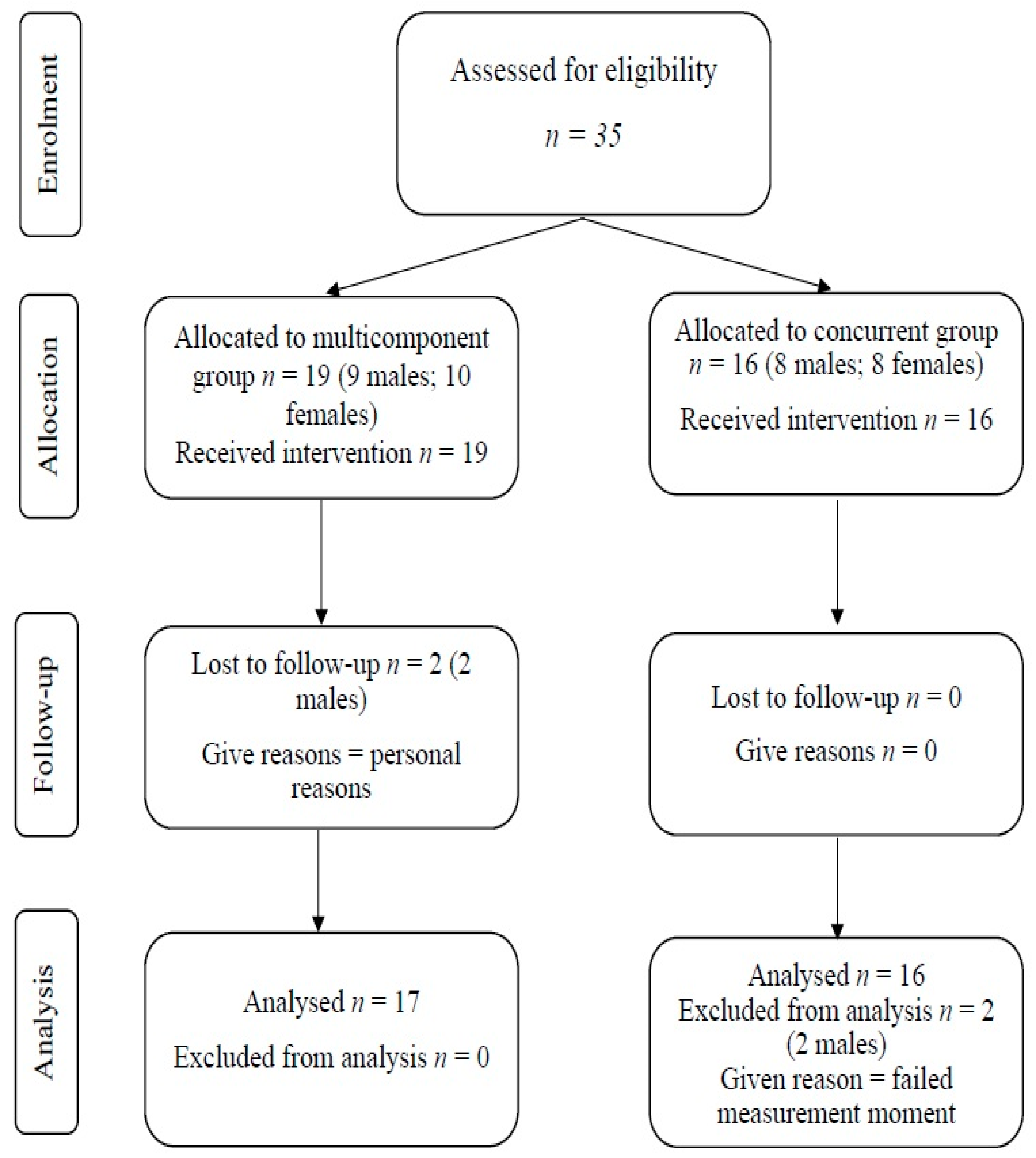
2.1. Participants
2.2. Procedures
2.3. Intervention
2.4. Outcomes
2.5. Statistical Analyses
3. Results
4. Discussion
Limitations and Agenda for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Marques, D.L.; Neiva, H.P.; Marinho, D.A.; Marques, M.C. Manipulating the Resistance Training Volume in Middle-Aged and Older Adults: A Systematic Review with Meta-Analysis of the Effects on Muscle Strength and Size, Muscle Quality, and Functional Capacity. Sports Med. 2022, 53, 503–518. [Google Scholar] [CrossRef] [PubMed]
- Di Lorito, C.; Long, A.; Byrne, A.; Harwood, R.H.; Gladman, J.R.F.; Schneider, S.; Logan, P.; Bosco, A.; van der Wardt, V. Exercise Interventions for Older Adults: A Systematic Review of Meta-Analyses. J. Sport. Health Sci. 2021, 10, 29–47. [Google Scholar] [CrossRef] [PubMed]
- Fien, S.; Linton, C.; Mitchell, J.S.; Wadsworth, D.P.; Szabo, H.; Askew, C.D.; Schaumberg, M.A. Characteristics of Community-Based Exercise Programs for Community-Dwelling Older Adults in Rural/Regional Areas: A Scoping Review. Aging Clin. Exp. Res. 2022, 34, 1511–1528. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, F.; Amaro, N.; Matos, R.; Mendes, D.; Monteiro, D.; Morouço, P. The Impact of an Exercise Intervention Using Low-Cost Equipment on Functional Fitness in the Community-Dwelling Older Adults: A Pilot Study. Front. Physiol. 2022, 13, 1039131. [Google Scholar] [CrossRef] [PubMed]
- Killingback, C.; Tsofliou, F.; Clark, C. Older People’s Adherence to Community-Based Group Exercise Programmes: A Multiple-Case Study. BMC Public Health 2017, 17, 115. [Google Scholar] [CrossRef] [PubMed]
- Izquierdo, M.; Merchant, R.A.; Morley, J.E.; Anker, S.D.; Aprahamian, I.; Arai, H.; Aubertin-Leheudre, M.; Bernabei, R.; Cadore, E.L.; Cesari, M.; et al. International Exercise Recommendations in Older Adults (ICFSR): Expert Consensus Guidelines. J. Nutr. Health Aging 2021, 25, 824–853. [Google Scholar] [CrossRef] [PubMed]
- da Silva, N.M.; de França, M.S.; de Almeida, D.K.F.H.; de Lima, E.S.G.; dos Santos, V.H.B.; Souza, J.V.d.A.; Larrad, A.R.; Aloise, D.d.A.; Lima, N.M.F.V. Effects of a Multicomponent Exercise Program on Groups of Community-Dwelling Older Adults with Low Schooling: A Pilot Study. J. Aging Res. 2021, 2021, 8829332. [Google Scholar] [CrossRef]
- Trombetti, A.; Reid, K.F.; Hars, M.; Herrmann, F.R.; Pasha, E.; Phillips, E.M.; Fielding, R.A. Age-Associated Declines in Muscle Mass, Strength, Power, and Physical Performance: Impact on Fear of Falling and Quality of Life. Osteoporos. Int. 2016, 27, 463–471. [Google Scholar] [CrossRef]
- Rodrigues, G.d.S.; Rodrigues, K.P.; de Almeida, M.L.; Sobrinho, A.C.d.S.; Noronha, N.Y.; Benjamim, C.J.R.; da Silva, S.; Rodrigues, J.A.L.; Júnior, C.R.B. Comparing Fourteen Weeks of Multicomponent Training Versus Combined Training in Physically Inactive Older Women: A Randomized Trial. Int. J. Environ. Res. Public Health 2023, 20, 2699. [Google Scholar] [CrossRef]
- Hurst, C.; Weston, K.L.; McLaren, S.J.; Weston, M. The Effects of Same-Session Combined Exercise Training on Cardiorespiratory and Functional Fitness in Older Adults: A Systematic Review and Meta-Analysis. Aging Clin. Exp. Res. 2019, 31, 1701–1717. [Google Scholar] [CrossRef]
- Sousa, N.; Mendes, R.; Abrantes, C.; Sampaio, J.; Oliveira, J. Effectiveness of Combined Exercise Training to Improve Functional Fitness in Older Adults: A Randomized Controlled Trial. Geriatr. Gerontol. Int. 2014, 14, 892–898. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, K.P.; Prado, L.; de Almeida, M.L.; Yamada, A.K.; Finzeto, L.C.; Bueno Júnior, C.R. Effects of Combined Versus Multicomponent Training in Physically Active Women Aged 50–75 Years. Res. Q. Exerc. Sport. 2022, 93, 710–717. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. World Medical Association World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Fiatarone Singh, M.A.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S. Exercise and Physical Activity for Older Adults. Med. Sci. Sports Exerc. 2009, 41, 1510. [Google Scholar] [CrossRef] [PubMed]
- Rikli, R.E.; Jones, C.J. Development and Validation of Criterion-Referenced Clinically Relevant Fitness Standards for Maintaining Physical Independence in Later Years. Gerontol. 2013, 53, 255–267. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, F.; Teixeira, J.E.; Forte, P. The Reliability of the Timed Up and Go Test among Portuguese Elderly. Healthcare 2023, 11, 928. [Google Scholar] [CrossRef] [PubMed]
- Jakobsen, L.H.; Rask, I.K.; Kondrup, J. Validation of Handgrip Strength and Endurance as a Measure of Physical Function and Quality of Life in Healthy Subjects and Patients. Nutrition 2010, 26, 542–550. [Google Scholar] [CrossRef]
- Rodrigues, F.; Domingos, C.; Monteiro, D.; Morouço, P. A Review on Aging, Sarcopenia, Falls, and Resistance Training in Community-Dwelling Older Adults. Int. J. Environ. Res. Public Health 2022, 19, 874. [Google Scholar] [CrossRef]
- Baker, B.S.; Miller, K.; Weitzel, K.J.; Duren, D.L.; Gammon, R.; Mills-Gray, S.; Ball, S.D. Resistance Training Reduces Age- and Geography-Related Physical Function Discrepancies in Older Adults. Gerontol. Geriatr. Med. 2021, 7. [Google Scholar] [CrossRef]
- Baker, B.S.; Miller, K.; Weitzel, K.J.; Duren, D.L.; Gammon, R.; Mills-Gray, S.; Ball, S.D. Acute Resistance Training May Have Lasting Benefit to Middle-Aged Adults. Gerontol. Geriatr. Med. 2021, 7. [Google Scholar] [CrossRef]
- Crowe, E.M.; Ball, S.D. Effectiveness of Advanced Stay Strong, Stay Healthy in Community Settings. Gerontol. Geriatr. Med. 2015, 1. [Google Scholar] [CrossRef] [PubMed]
- Ball, S.; Gammon, R.; Kelly, P.J.; Cheng, A.-L.; Chertoff, K.; Kaume, L.; Abreu, E.L.; Brotto, M. Outcomes of Stay Strong, Stay Healthy in Community Settings. J. Aging Heal. 2013, 25, 1388–1397. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Shinkai, S. Prevalence of Muscle Weakness Based on Different Diagnostic Criteria in Community-Dwelling Older Adults: A Comparison of Grip Strength Dynamometers. Geriatr. Gerontol. Int. 2017, 17, 2089–2095. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Liu, Y.; Lin, T.; Hou, L.; Song, Q.; Ge, N.; Yue, J. Reliability and Validity of Two Hand Dynamometers When Used by Community-Dwelling Adults Aged over 50 Years. BMC Geriatr. 2022, 22, 580. [Google Scholar] [CrossRef]
- Abe, T.; Loenneke, J.P.; Thiebaud, R.S.; Loftin, M. The Bigger the Hand, the Bigger the Difference? Implications for Testing Strength With 2 Popular Handgrip Dynamometers. J. Sport Rehabil. 2019, 28, 278–282. [Google Scholar] [CrossRef]
- Guerra, R.S.; Amaral, T.F.; Sousa, A.S.; Fonseca, I.; Pichel, F.; Restivo, M.T. Comparison of Jamar and Bodygrip Dynamometers for Handgrip Strength Measurement. J. Strength Cond. Res. 2017, 31, 1931. [Google Scholar] [CrossRef]
| Variables | Units | Multicomponent Group | Concurrent Group | ||||||
|---|---|---|---|---|---|---|---|---|---|
| MT0 | SDT0 | MT1 | SDT1 | MT0 | SDT0 | MT1 | SDT1 | ||
| 30 s chair stand | Repetitions | 14.15 | 5.03 | 17.22 | 5.37 | 15.58 | 4.52 | 16.73 | 4.66 |
| 30 s arm curl | Repetitions | 19.84 | 6.39 | 24.53 | 5.73 | 22.37 | 2.63 | 23.28 | 7.33 |
| Timed Up and Go test | Seconds | 4.89 | 0.64 | 4.79 | 0.89 | 5.08 | 0.46 | 4.60 | 0.46 |
| Handgrip strength | Kilograms | 30.95 | 9.39 | 32.80 | 10.35 | 31.12 | 6.84 | 30.91 | 6.88 |
| Variables | Mean Square | F | df1 | df2 | p | η2p | Pairwise Comparisons |
|---|---|---|---|---|---|---|---|
| 30 s chair stand | |||||||
| Time | 2.503 | 0.170 | 1 | 15 | 0.686 | 0.011 | ns |
| Group | 81.732 | 66.596 | 1 | 15 | ≤0.001 | 0.816 | 1 ≠ 2 |
| Time*group | 77.931 | 16.953 | 1 | 15 | ≤0.001 | 0.531 | 1 ≠ 2 |
| 30 s arm curl | |||||||
| Time | 51.01 | 1.31 | 1 | 15 | 0.269 | 0.081 | ns |
| Group | 435.11 | 19.28 | 1 | 15 | ≤0.001 | 0.562 | 1 ≠ 2 |
| Time*group | 10.84 | 0.181 | 1 | 15 | 0.677 | 0.012 | ns |
| Timed Up and Go test | |||||||
| Time | 0.209 | 0.593 | 1 | 15 | 0.453 | 0.038 | ns |
| Group | 1.45 | 35.561 | 1 | 15 | ≤0.001 | 0.703 | 1 ≠ 2 |
| Time*group | 2.14 | 11.687 | 1 | 15 | 0.004 | 0.438 | 1 ≠ 2 |
| Handgrip strength | |||||||
| Time | 1.683 | 0.027 | 1 | 15 | 0.871 | 0.002 | ns |
| Group | 17.621 | 2.62 | 1 | 15 | 0.126 | 0.149 | ns |
| Time*group | 101.635 | 5.19 | 1 | 15 | 0.038 | 0.257 | 1 ≠ 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodrigues, F.; Jacinto, M.; Antunes, R.; Monteiro, D.; Mendes, D.; Matos, R.; Amaro, N. Comparing the Effects of Multicomponent and Concurrent Exercise Protocols on Muscle Strength in Older Adults. J. Funct. Morphol. Kinesiol. 2024, 9, 3. https://doi.org/10.3390/jfmk9010003
Rodrigues F, Jacinto M, Antunes R, Monteiro D, Mendes D, Matos R, Amaro N. Comparing the Effects of Multicomponent and Concurrent Exercise Protocols on Muscle Strength in Older Adults. Journal of Functional Morphology and Kinesiology. 2024; 9(1):3. https://doi.org/10.3390/jfmk9010003
Chicago/Turabian StyleRodrigues, Filipe, Miguel Jacinto, Raul Antunes, Diogo Monteiro, Diogo Mendes, Rui Matos, and Nuno Amaro. 2024. "Comparing the Effects of Multicomponent and Concurrent Exercise Protocols on Muscle Strength in Older Adults" Journal of Functional Morphology and Kinesiology 9, no. 1: 3. https://doi.org/10.3390/jfmk9010003
APA StyleRodrigues, F., Jacinto, M., Antunes, R., Monteiro, D., Mendes, D., Matos, R., & Amaro, N. (2024). Comparing the Effects of Multicomponent and Concurrent Exercise Protocols on Muscle Strength in Older Adults. Journal of Functional Morphology and Kinesiology, 9(1), 3. https://doi.org/10.3390/jfmk9010003









