Immediate Effects of Isolated Lumbar Extension Resistance Exercise (ILEX) on Spine Posture and Mobility Measured with the IDIAG Spinal Mouse System
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Study Context and Ethical Considerations
2.3. Scanning Device and Outcome Parameters
2.4. Scanning Procedure
2.5. Machine Settings (ILEX Device) and Exercise Procedure
2.6. Statistical Analysis
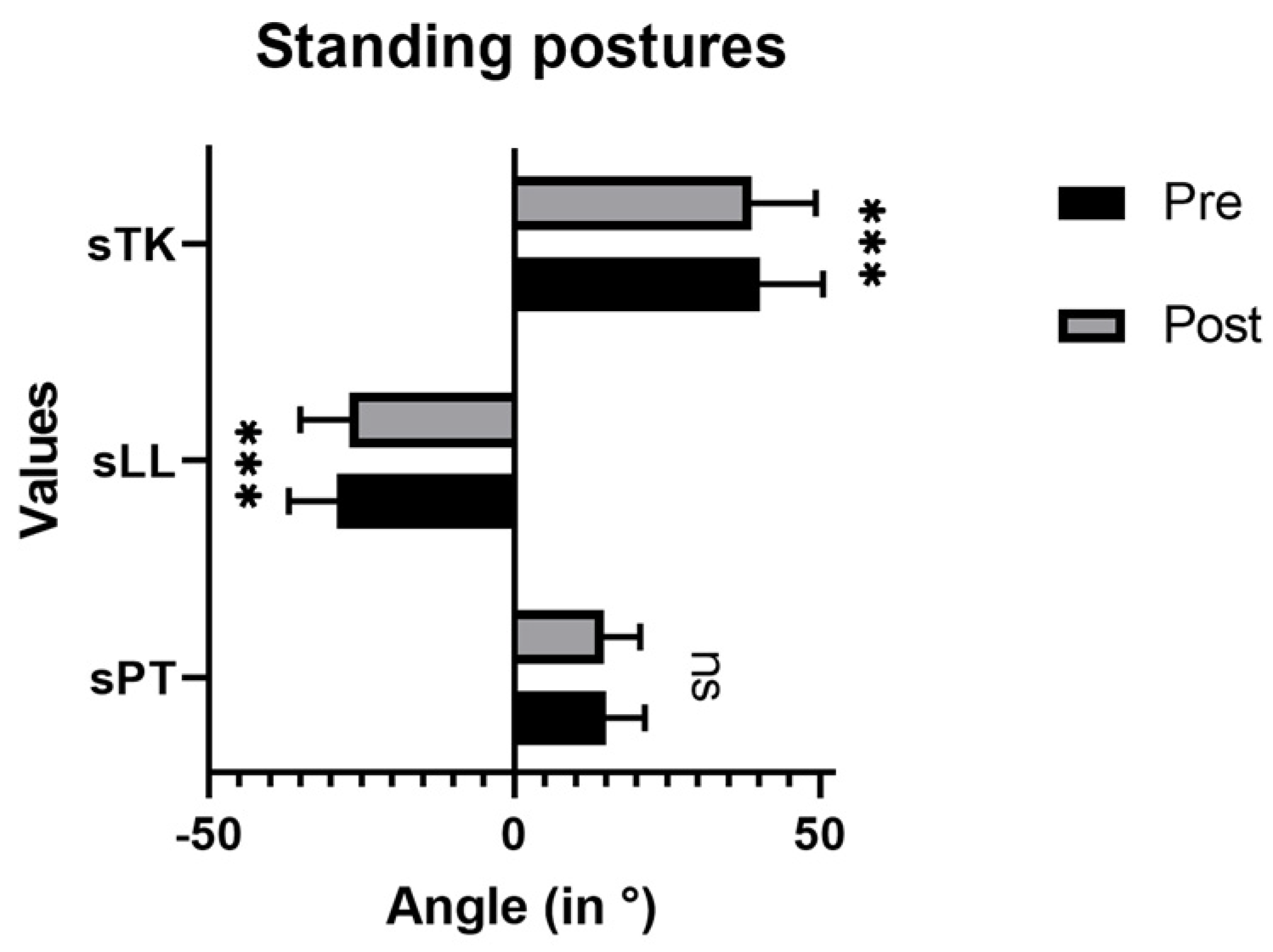
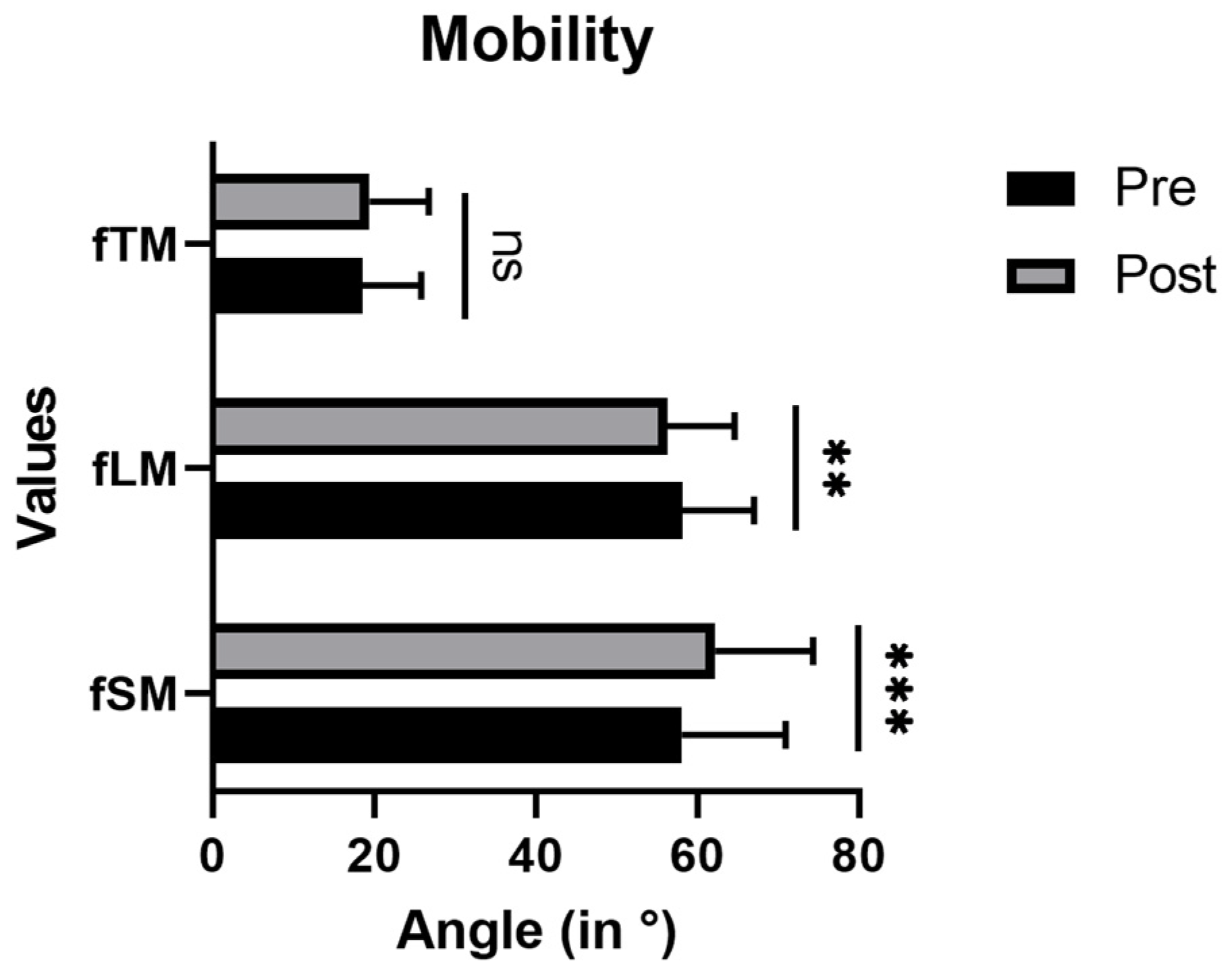
3. Results
4. Discussion
4.1. Immediate Effects on Posture
4.2. Immediate Effects on Mobility
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Panjabi, M.M. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J. Spinal Disord. 1992, 5, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Christie, H.J.; Kumar, S.; Warren, S.A. Postural aberrations in low back pain. Arch. Phys. Med. Rehabil. 1995, 76, 218–224. [Google Scholar] [CrossRef]
- Been, E.; Kalichman, L. Lumbar lordosis. Spine J. 2014, 14, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Czaprowski, D.; Stoliński, Ł.; Tyrakowski, M.; Kozinoga, M.; Kotwicki, T. Non-structural misalignments of body posture in the sagittal plane. Scoliosis Spinal Disord. 2018, 13, 6. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; McClure, P.W.; Pratt, N. The Effect of hamstring muscle stretching on standing posture and on lumbar and hip motions during forward bending. Phys. Ther. 1996, 76, 836–845. [Google Scholar] [CrossRef] [PubMed]
- Sadler, S.G.; Spink, M.J.; Ho, A.; Jonge, X.J.; de Chuter, V.H. Restriction in lateral bending range of motion, lumbar lordosis, and hamstring flexibility predicts the development of low back pain: A systematic review of prospective cohort studies. BMC Musculoskelet. Disord. 2017, 18, 179. [Google Scholar] [CrossRef]
- Lim, J.K.; Kim, S.M. Comparison of sagittal spinopelvic alignment between lumbar degenerative spondylolisthesis and degenerative spinal stenosis. J. Korean Neurosurg. Soc. 2014, 55, 331–336. [Google Scholar] [CrossRef]
- Sparrey, C.J.; Bailey, J.F.; Safaee, M.; Clark, A.J.; Lafage, V.; Schwab, F.; Smith, J.S.; Ames, C.P. Etiology of lumbar lordosis and its pathophysiology: A review of the evolution of lumbar lordosis, and the mechanics and biology of lumbar degeneration. Neurosurg. Focus 2014, 36, e1. [Google Scholar] [CrossRef]
- Diebo, B.G.; Varghese, J.J.; Lafage, R.; Schwab, F.J.; Lafage, V. Sagittal alignment of the spine: What do you need to know? Clin. Neurol. Neurosurg. 2015, 139, 295–301. [Google Scholar] [CrossRef]
- Jentzsch, T.; Geiger, J.; König, M.A.; Werner, C.M.L. Hyperlordosis is associated with facet joint pathology at the lower lumbar spine. Clin. Spine Surg. 2017, 30, 129–135. [Google Scholar] [CrossRef]
- Chun, S.W.; Lim, C.Y.; Kim, K.; Hwang, J.; Chung, S.G. The relationships between low back pain and lumbar lordosis. A systematic review and meta-analysis. Spine J. 2017, 17, 1180–1191. [Google Scholar] [CrossRef] [PubMed]
- Katzman, W.B.; Vittinghoff, E.; Lin, F.; Schafer, A.; Long, R.K.; Wong, S.; Gladin, A.; Fan, B.; Allaire, B.; Kado, D.M.; et al. Targeted spine strengthening exercise and posture training program to reduce hyperkyphosis in older adults: Results from the study of hyperkyphosis, exercise, and function (SHEAF) randomized controlled trial. Osteoporos. Int. 2017, 28, 2831–2841. [Google Scholar] [CrossRef] [PubMed]
- González-Gálvez, N.; Gea-García, G.M.; Marcos-Pardo, P.J. Effects of exercise programs on kyphosis and lordosis angle: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0216180. [Google Scholar] [CrossRef]
- Ponzano, M.; Tibert, N.; Bansal, S.; Katzman, W.; Glangregorio, L. Exercise for improving age-related hyperkyphosis: A systematic review and meta-analysis with GRADE assessment. Arch. Osteoporos. 2021, 16, 140. [Google Scholar] [CrossRef] [PubMed]
- Seichert, N.; Baumann, M.; Senn, E.; Zuckriegl, H. The “back mouse”—An analog-digital measuring device to record the sagittal outline of the back. Phys. Med. Rehabil. Kurortmed. 1994, 4, 35–43. [Google Scholar] [CrossRef]
- Mannion, A.F.; Knecht, K.; Balaban, G.; Dvorak, J.; Grob, D. A new skin-surface device for measuring the curvature and global and segmental ranges of motion of the spine: Reliability of measurement and comparison with data reviewed from the literature. Eur. Spine J. 2004, 13, 122–136. [Google Scholar] [CrossRef]
- Demir, E.; Guezel, N.A.; Cobanoglu, G.; Kafa, N. The reliability of measurements with the spinal mouse device in frontal and sagittal planes in asymptomatic female adolescents. Ann. Clin. Anal. Med. 2020, 11, 146–149. [Google Scholar] [CrossRef]
- Smith, D.; Bissell, G.; Bruce-Low, S.; Wakefield, C. The effect of lumbar extension training with and without pelvic restraint on lumbar strength and low back pain. J. Back Musculoskelet. Rehabil. 2011, 24, 241–249. [Google Scholar] [CrossRef]
- Steele, J.; Bruce-Low, S.; Smith, D. A review of the specificity of exercises designed for conditioning the lumbar extensors. Br. J. Spors Med. 2015, 49, 291–297. [Google Scholar] [CrossRef]
- Graves, J.E.; Webb, D.C.; Pollock, M.L.; Matkozich, J.; Leggett, S.H.; Carpenter, D.M.; Foster, D.N.; Cirulli, J. Pelvic stabilization during resistance training: Its effect on the development of lumbar extension strength. Arch. Phys. Med. Rehabil. 1994, 75, 210–215. [Google Scholar] [CrossRef]
- Steele, J.; Bruce-Low, S.; Smith, D. A review of the clinical value of isolated lumbar extension resistance training for chronic low back pain. PMR 2015, 7, 169–187. [Google Scholar] [CrossRef] [PubMed]
- Golonka, W.; Raschka, C.; Harandi, V.M.; Domokos, B.; Alfredson, H.; Alfen, F.M.; Spang, C. Isolated lumbar extension resistance exercise in limited range of motion for patients with lumbar radiculopathy and disk herniation—Clinical outcome and influencing factors. J. Clin. Med. 2021, 10, 2430. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Minaro, P.A.; Muyor, J.M.; Belmonte, F.; Alacid, F. Acute effects of hamstring stretching on sagittal spinal curvatures and pelvic tilt. J. Hum. Kinet. 2012, 31, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Takihara, Y.; Urabe, Y.; Nishiwaki, G.A.; Tanaka, K.; Miyashita, K. How back-muscle fatigue influences lumbar curvature. J. Sport Rehabil. 2009, 19, 327–336. [Google Scholar] [CrossRef] [PubMed]
- IDIAG Ag. IDIAG M360. Software Handbuch; IDIAG Ag: Zürich, Switzerland, 2018. [Google Scholar]
- Malai, S.; Pichaiyongwongdee, S.; Sakulsriprasert, P. Immediate effect of hold-relax stretching of iliopsoas muscle on transversus abdominis muscles activation in chronic non-specific low back pain with lumbar hyperlordosis. J. Med. Assoc. Thai. 2015, 98 (Suppl. 5), 6–11. [Google Scholar]
- Koo, D.K.; Nam, S.M.; Kwon, J.W. Immediate effects of the reverse plank exercise on muscle thickness and postural angle in individuals with the forward shoulder posture. J. Funct. Morphol. Kinesiol. 2022, 7, 82. [Google Scholar] [CrossRef]
- Namdar, N.; Arazpour, M.; Bani, M.A. Comparison of the immediate efficacy of the Spinomed back orthosis and posture training support on walking ability in elderly people with thoracic kyphosis. Disabil. Rehabil. Assist. Technol. 2019, 14, 2217–2220. [Google Scholar] [CrossRef]
- Shum, G.L.; Tsung, B.Y.; Lee, R.Y. The immediate effect of posteroanterior mobilization on reducing back pain and the stifness of the lumbar spine. Arch. Phys. Med. Rhebil. 2013, 94, 673–679. [Google Scholar] [CrossRef]
- Villers, J.; Cardenas, A.; Gipson, T.; Man, E. The immediate effect of adding lumbar mobilization to a static stretching program on hamstrings range of motion: An exploratory study. J. Sports Sci. Med. 2022, 21, 253–259. [Google Scholar] [CrossRef]
- Grieve, R.; Goodwin, F.; Alfaki, M.; Bourton, A.J.; Jeffries, C. The immediate effect of bilateral self myofascial release on the plantar surface of the feet on hamstring and lumbar spine flexibility: A pilot randomized controlled trial. J. Bodyw. Mov. Ther. 2015, 19, 544–552. [Google Scholar] [CrossRef]
- Iorio, J.A.; Jakoi, A.M.; Singla, A. Biomechanics of degenerative spinal disorders. Asian Spine J. 2016, 10, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Dolan, P.; Adams, M.A. Influence of lumbar and hip mobility on the bending stresses acting on the lumbar spine. Clin. Biomech. 1993, 8, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Ko, K.J.; Ha, G.C.; Yook, Y.S.; Kang, S.J. Effects of 12-week lumbar stabilization exercise and sling exercise on lumbosacral region angle, lumbar muscle strength, and pain scale of patients with chronic low back pain. J. Phys. Ther. Sci. 2018, 30, 18–22. [Google Scholar] [CrossRef]
- Zwierzchowska, A.; Tuz, J. Evaluation of the impact of sagittal spinal curvatures on musculoskeletal disorders in young people. Med. Pr. 2018, 69, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Greig, A.M.; Bennell, K.L.; Briggs, A.M.; Hodges, P.W. Postural taping decreases thoracic kyphosis but does not influence trunk muscle electromyographic activity or balance in women with osteoporosis. Man. Ther. 2008, 13, 249–257. [Google Scholar] [CrossRef] [PubMed]



| Women | Men | Total | |
|---|---|---|---|
| n | 16 | 17 | 33 |
| Age (years) | 28.2 ± 8.3 | 31.6 ± 4.6 | 29.9 ± 6.8 |
| Height (cm) | 167.6 ± 7.4 | 183.9 ± 4.6 | 176.0 ± 10.2 |
| Weight (kg) | 59.7 ± 6.2 | 83.4 ± 12.8 | 71.9 ± 15.6 |
| BMI (kg/m2) | 21.3 ± 1.9 | 24.7 ± 4.1 | 23.0 ± 3.6 |
| Mean ± SD in ° | p | ICC (95% CI) | SEM (95% CI) | ||
|---|---|---|---|---|---|
| M1 | M2 | ||||
| Standing Postition | |||||
| sTK | 40.82 ± 10.43 | 40.26 ± 10.56 | 0.342 | 0.977 (0.951–0.989) | 0.581 (−0.627–1.749) |
| sLL | −28.18 ± 7.86 | −26.42 ± 13.54 | 0.359 | 0.722 (0.419–0.867) | 1.887 (−5.620–2.100) |
| sPT | 14.85 ± 5.94 | 15.19 ± 6.66 | 0.372 | 0.974 (0.946–0.988) | 0.369 (−1.088–0.420) |
| Mobility | |||||
| fTM | 17.11 ± 7.33 | 17.21 ± 7.72 | 0.912 | 0.883 (0.753–0.944) | 0.901 (−1.944–1.742) |
| fLM | 56.71 ± 8.14 | 56.85 ± 8.34 | 0.726 | 0.983 (0.964–0.992) | 0.396 (−0.949–0.669) |
| fSM | 58.62 ± 16.23 | 62.43 ± 12.81 | 0.040 * | 0.863 (0.703–0.936) | 1.774 (−7.438–−0.182) |
| Standing Posture | |||
| sTK | sLL | sPT | |
| sTK | −0.385 * | 0.089 | |
| sLL | −0.826 *** | ||
| Mobility | |||
| fTM | fLM | fSM | |
| fTM | −0.169 | 0.349 | |
| fLM | −0.287 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Domokos, B.; Beer, L.; Reuther, S.; Raschka, C.; Spang, C. Immediate Effects of Isolated Lumbar Extension Resistance Exercise (ILEX) on Spine Posture and Mobility Measured with the IDIAG Spinal Mouse System. J. Funct. Morphol. Kinesiol. 2023, 8, 60. https://doi.org/10.3390/jfmk8020060
Domokos B, Beer L, Reuther S, Raschka C, Spang C. Immediate Effects of Isolated Lumbar Extension Resistance Exercise (ILEX) on Spine Posture and Mobility Measured with the IDIAG Spinal Mouse System. Journal of Functional Morphology and Kinesiology. 2023; 8(2):60. https://doi.org/10.3390/jfmk8020060
Chicago/Turabian StyleDomokos, Bruno, Lisa Beer, Stefanie Reuther, Christoph Raschka, and Christoph Spang. 2023. "Immediate Effects of Isolated Lumbar Extension Resistance Exercise (ILEX) on Spine Posture and Mobility Measured with the IDIAG Spinal Mouse System" Journal of Functional Morphology and Kinesiology 8, no. 2: 60. https://doi.org/10.3390/jfmk8020060
APA StyleDomokos, B., Beer, L., Reuther, S., Raschka, C., & Spang, C. (2023). Immediate Effects of Isolated Lumbar Extension Resistance Exercise (ILEX) on Spine Posture and Mobility Measured with the IDIAG Spinal Mouse System. Journal of Functional Morphology and Kinesiology, 8(2), 60. https://doi.org/10.3390/jfmk8020060






