Insights into Non-Exercise Physical Activity on Control of Body Mass: A Review with Practical Recommendations
Abstract
1. Introduction
2. Methods
2.1. Information Sources
2.2. Search Strategy
2.3. Findings Presentation
3. Non-Exercise Physical Activity
4. Energy Expenditure from Non-Exercise Physical Activity
5. Promotion Strategies
6. Technological Monitoring of Non-Exercise Physical Activity
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hruby, A.; Hu, F.B. The Epidemiology of Obesity: A Big Picture. Pharmacoeconomics 2014, 33, 673–689. [Google Scholar] [CrossRef] [PubMed]
- Argilés, J.M.; Campos, N.; Lopez-Pedrosa, J.M.; Rueda, R.; Rodriguez-Mañas, L. Skeletal Muscle Regulates Metabolism via Interorgan Crosstalk: Roles in Health and Disease. J. Am. Med. Dir. Assoc. 2016, 17, 789–796. [Google Scholar] [CrossRef]
- Chakravarthy, M.V.; Booth, F.W. Eating, exercise, and “thrifty” genotypes: Connecting the dots toward an evolutionary understanding of modern chronic diseases. J. Appl. Physiol. 2004, 96, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, M.; Leibel, R.L. 20 years of leptin: Role of leptin in energy homeostasis in humans. J. Endocrinol. 2014, 223, T83–T96. [Google Scholar] [CrossRef] [PubMed]
- Sawamoto, R.; Nozaki, T.; Nishihara, T.; Furukawa, T.; Hata, T.; Komaki, G.; Sudo, N. Predictors of successful long-term weight loss maintenance: A two-year follow-up. BioPsychoSocial Med. 2017, 11, 14. [Google Scholar] [CrossRef]
- Kruger, J.; Blanck, H.M.; Gillespie, C. Dietary and physical activity behaviors among adults successful at weight loss maintenance. Int. J. Behav. Nutr. Phys. Act. 2006, 3, 17. [Google Scholar] [CrossRef]
- Laddu, D.; Paluch, A.E.; LaMonte, M.J. The role of the built environment in promoting movement and physical activity across the lifespan: Implications for public health. Prog. Cardiovasc. Dis. 2021, 64, 33–40. [Google Scholar] [CrossRef]
- Von Loeffelholz, C.; Birkenfeld, A. The role of non-exercise activity thermogenesis in human obesity. In Endotext; Feingold, F., Ed.; MDText.Com, Inc: South Dartmouth, MA, USA, 2018. [Google Scholar]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar] [PubMed]
- Castillo-Garzón, M.J.; Ruiz, J.R.; Ortega, F.B.; Gutiérrez, Á. Anti-aging therapy through fitness enhancement. Clin. Interv. Aging 2006, 1, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Kyu, H.H.; Bachman, V.F.; Alexander, L.T.; Mumford, J.E.; Afshin, A.; Estep, K.; Veerman, J.L.; Delwiche, K.; Iannarone, M.L.; Moyer, M.L.; et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: Systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. BMJ (Clin. Res. Ed.) 2016, 354, i3857. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.; Katikireddi, S.V.; Sowden, A.; Thomson, H. Lack of transparency in reporting narrative synthesis of quantitative data: A methodological assessment of systematic reviews. J. Clin. Epidemiol. 2019, 105, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Dixon-Woods, M.; Bonas, S.; Booth, A.; Jones, D.R.; Miller, T.; Sutton, A.J.; Shaw, R.L.; Smith, J.A.; Young, B. How can systematic reviews incorporate qualitative research? A critical perspective. Qual. Res. 2016, 6, 27–44. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Implement. 2021, 19, 3–10. [Google Scholar] [CrossRef]
- Lisy, K.; Porritt, K. Narrative Synthesis. Int. J. Evid.-Based Healthc. 2016, 14, 201. [Google Scholar] [CrossRef]
- World Health Organization. Physical Activity. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 14 January 2023).
- Westerterp, K. Physical Activity and Physical Activity Induced Energy Expenditure in Humans: Measurement, Determinants, and Effects. Front. Physiol. 2013, 4, 90. [Google Scholar] [CrossRef]
- American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2014. [Google Scholar]
- Wärnberg, J.; Cunningham, K.; Romeo, J.; Marcos, A. Physical activity, exercise and low-grade systemic inflammation. Proc. Nutr. Soc. 2010, 69, 400–406. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Glossary. Available online: https://www.cdc.gov/nchs/nhis/physical_activity/pa_glossary.htm (accessed on 14 January 2023).
- Piggin, J. What Is Physical Activity? A Holistic Definition for Teachers, Researchers and Policy Makers. Front. Sport. Act. Living 2020, 2, 72. [Google Scholar] [CrossRef] [PubMed]
- Organización Mundial de la Salud. Estrategia Mundial Sobre Régimen Alimentario, Actividad Física y Salud. Actividad Física. Available online: https://www.who.int/dietphysicalactivity/pa/es/ (accessed on 14 January 2023).
- Beltaifa, L.; Chaouachi, A.; Zérifi, R.; Boussaidi, L.; Bouzrati, I.; Abid, A.; Elkhadi, A.; Chamari, K.; Raies, A. Walk-Run Transition Speed Training as an Efficient Exercise Adjunct to Dietary Restriction in the Management of Obesity: A Prospective Intervention Pilot Study. Obes. Facts 2011, 4, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Villareal, D.T.; Aguirre, L.; Gurney, A.B.; Waters, D.L.; Sinacore, D.R.; Colombo, E.; Armamento-Villareal, R.; Qualls, C. Aerobic or Resistance Exercise, or Both, in Dieting Obese Older Adults. N. Engl. J. Med. 2017, 376, 1943–1955. [Google Scholar] [CrossRef]
- Cauza, E.; Hanusch-Enserer, U.; Strasser, B.; Ludvik, B.; Metz-Schimmerl, S.; Pacini, G.; Wagner, O.; Georg, P.; Prager, R.; Kostner, K.; et al. The Relative Benefits of Endurance and Strength Training on the Metabolic Factors and Muscle Function of People With Type 2 Diabetes Mellitus. Arch. Phys. Med. Rehabil. 2005, 86, 1527–1533. [Google Scholar] [CrossRef] [PubMed]
- Görner, K.; Reineke, A. The influence of endurance and strength training on body composition and physical fitness in female students. J. Phys. Educ. Sport 2020, 2020, 8. [Google Scholar] [CrossRef]
- World Health Organization. Noncommunicable Diseases Country Profiles 2014; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour: At a Glance; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
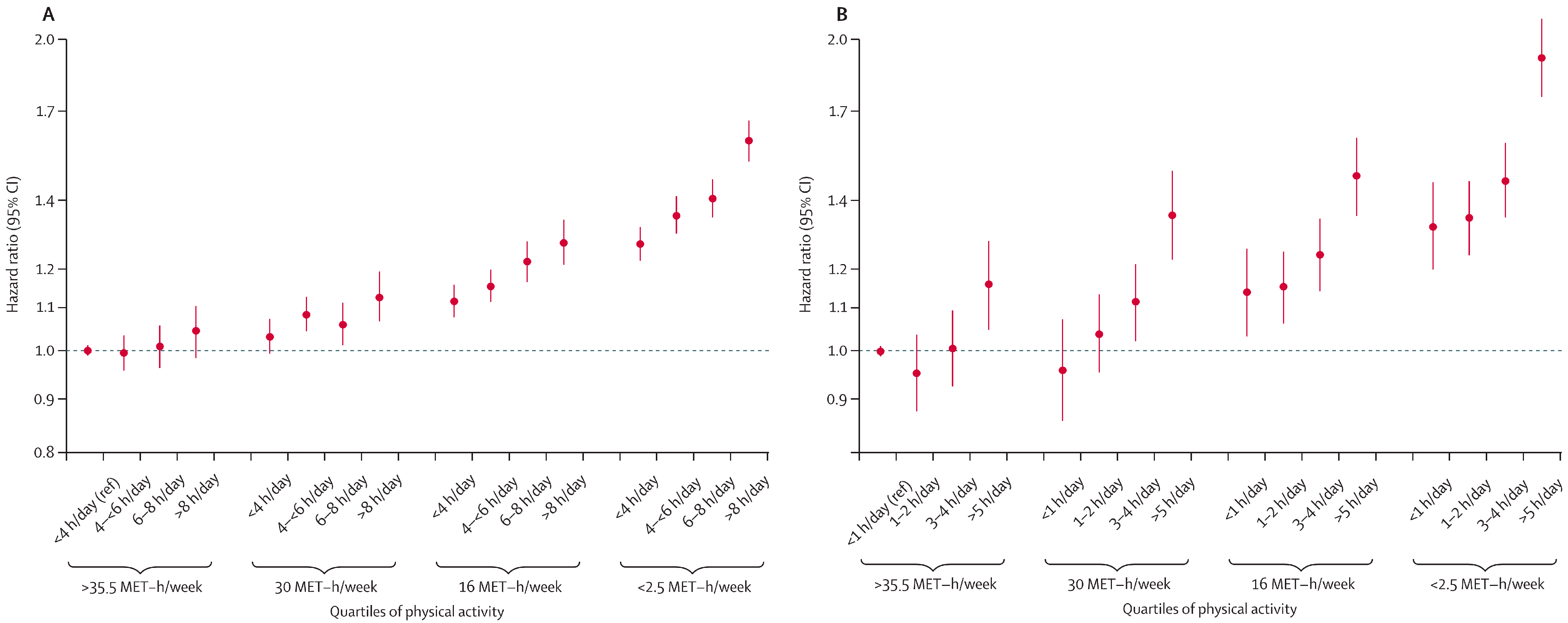
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.; Lee, I.M. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef] [PubMed]
- Aragon, A.A.; Schoenfeld, B.J.; Wildman, R.; Kleiner, S.; VanDusseldorp, T.; Taylor, L.; Earnest, C.P.; Arciero, P.J.; Wilborn, C.; Kalman, D.S.; et al. International society of sports nutrition position stand: Diets and body composition. J. Int. Soc. Sport. Nutr. 2017, 14, 16. [Google Scholar] [CrossRef] [PubMed]
- Herrera-Amante, C.A.; Ramos-Garcia, C.O.; Alacid, F.; Quiroga-Morales, L.A.; Martinez-Rubio, A.J.; Bonilla, D.A. Development of alternatives to estimate resting metabolic rate from anthropometric variables in paralympic swimmers. J. Sport. Sci. 2021, 39, 2133–2143. [Google Scholar] [CrossRef] [PubMed]
- Granata, G.P.; Brandon, L.J. The thermic effect of food and obesity: Discrepant results and methodological variations. Nutr. Rev. 2002, 60, 223–233. [Google Scholar] [CrossRef] [PubMed]
- Levine, J.A.; Lanningham-Foster, L.M.; McCrady, S.K.; Krizan, A.C.; Olson, L.R.; Kane, P.H.; Jensen, M.D.; Clark, M.M. Interindividual Variation in Posture Allocation: Possible Role in Human Obesity. Science 2005, 307, 584–586. [Google Scholar] [CrossRef]
- Levine, J.A.; Vander, M.W.; Hill, J.O.; Klesges, R.C. Non-Exercise Activity Thermogenesis. Arterioscler. Thromb. Vasc. Biol. 2006, 26, 729–736. [Google Scholar] [CrossRef]
- Chung, N.; Park, M.-Y.; Kim, J.; Park, H.-Y.; Hwang, H.; Lee, C.-H.; Han, J.-S.; So, J.; Park, J.; Lim, K. Non-exercise activity thermogenesis (NEAT): A component of total daily energy expenditure. J. Exerc. Nutr. Biochem. 2018, 22, 23–30. [Google Scholar] [CrossRef]
- Malaeb, S.; Perez-Leighton, C.E.; Noble, E.E.; Billington, C. A “NEAT” Approach to Obesity Prevention in the Modern Work Environment. Workplace Health Saf. 2019, 67, 102–110. [Google Scholar] [CrossRef]
- Silva, A.M.; Judice, P.B.; Carraca, E.V.; King, N.; Teixeira, P.J.; Sardinha, L.B. What is the effect of diet and/or exercise interventions on behavioural compensation in non-exercise physical activity and related energy expenditure of free-living adults? A systematic review. Br. J. Nutr. 2018, 119, 1327–1345. [Google Scholar] [CrossRef]
- Liu, X.M.; Wang, K.; Zhu, Z.; Cao, Z.B. Compensatory effects of different exercise durations on non-exercise physical activity, appetite, and energy intake in normal weight and overweight adults. Front. Physiol. 2022, 13, 932846. [Google Scholar] [CrossRef] [PubMed]
- Castro, E.A.; Peinado, A.B.; Benito, P.J.; Galindo, M.; Gonzalez-Gross, M.; Cupeiro, R.; Group, P.S. What is the most effective exercise protocol to improve cardiovascular fitness in overweight and obese subjects? J. Sport Health Sci. 2017, 6, 454–461. [Google Scholar] [CrossRef] [PubMed]
- Romero Moraleda, B.; Morencos, E.; Peinado, A.B.; Bermejo, L.; Gomez Candela, C.; Benito, P.J.; on behalf of the PRONAF Study Group. Can the exercise mode determine lipid profile improvements in obese patients? Nutr. Hosp. 2013, 28, 607–617. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Miranda, L.M.; Briones-Villalba, R.A.; Ortiz-Ortiz, M.; Aburto-Corona, J.A.; Bonilla, D.A.; Pozos-Parra, P.; Espinoza-Gutierrez, R.; Calleja-Nunez, J.J.; Moncada-Jimenez, J.; Hernandez-Lepe, M.A. Association between Body Mass Index with Sugar-Sweetened and Dairy Beverages Consumption in Children from the Mexico-USA Border. Int. J. Environ. Res. Public Health 2022, 19, 6403. [Google Scholar] [CrossRef]
- Harris, J.L.; Bargh, J.A.; Brownell, K.D. Priming effects of television food advertising on eating behavior. Health Psychol. 2009, 28, 404–413. [Google Scholar] [CrossRef]
- Brown, V.; Moodie, M.; Cobiac, L.; Mantilla Herrera, A.M.; Carter, R. Obesity-related health impacts of fuel excise taxation- an evidence review and cost-effectiveness study. BMC Public Health 2017, 17, 359. [Google Scholar] [CrossRef]
- Courtemanche, C. A Silver Lining? The Connection between Gasoline Prices and Obesity. Econ. Inq. 2011, 49, 935–957. [Google Scholar] [CrossRef]
- Hou, N.; Popkin, B.M.; Jacobs, D.R.; Song, Y.; Guilkey, D.K.; He, K.; Lewis, C.E.; Gordon-Larsen, P. Longitudinal trends in gasoline price and physical activity: The CARDIA study. Prev. Med. 2011, 52, 365–369. [Google Scholar] [CrossRef]
- Booth, F.W.; Laye, M. Lack of adequate appreciation of physical exercise’s complexities can pre-empt appropriate design and interpretation in scientific discovery. J. Physiol. 2009, 587, 5527–5539. [Google Scholar] [CrossRef] [PubMed]
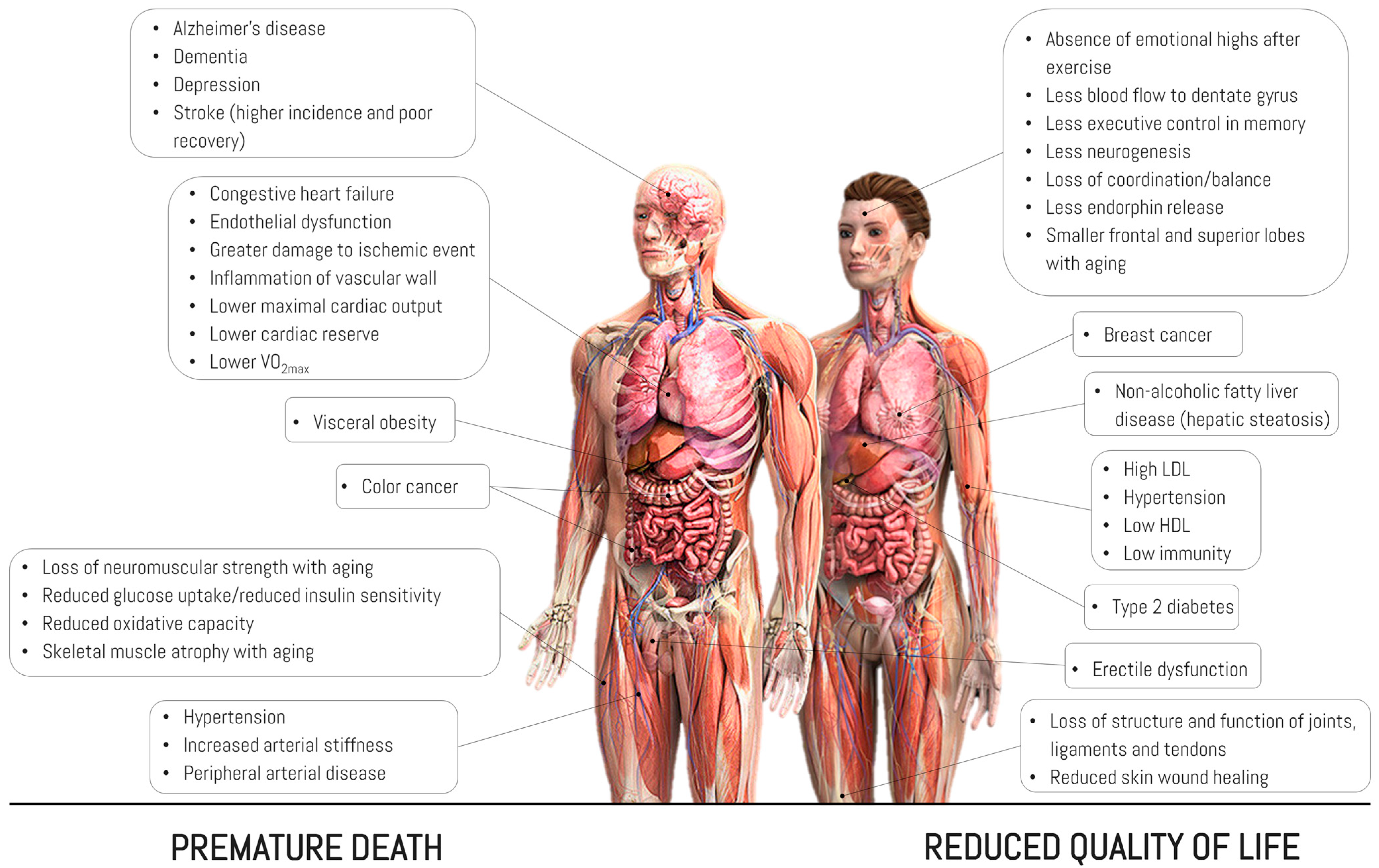
- Booth, F.W.; Roberts, C.K.; Thyfault, J.P.; Ruegsegger, G.N.; Toedebusch, R.G. Role of Inactivity in Chronic Diseases: Evolutionary Insight and Pathophysiological Mechanisms. Physiol. Rev. 2017, 97, 1351–1402. [Google Scholar] [CrossRef]
- Abi-Jaoude, E.; Naylor, K.T.; Pignatiello, A. Smartphones, social media use and youth mental health. CMAJ 2020, 192, E136–E141. [Google Scholar] [CrossRef]
- Chen, L.; Shi, J. Reducing Harm From Media: A Meta-Analysis of Parental Mediation. J. Mass Commun. Q. 2018, 96, 173–193. [Google Scholar] [CrossRef]
- Ochs, C.; Sauer, J. Curtailing smartphone use: A field experiment evaluating two interventions. Behav. Inf. Technol. 2021, 41, 3598–3616. [Google Scholar] [CrossRef]
- Myers, E.; Drees, E.T.; Cain, J. An Intervention Utilizing the Salience Principle to Reduce Pharmacy Students’ Psychological Attraction to Smartphones. Am. J. Pharm. Educ. 2022, 86, 8717. [Google Scholar] [CrossRef]
- Choksi, S.T. A Study to Find Out the Correlation of Mobile Phone Addiction with Anxiety, Depression, Stress and Sleep Quality in the College Students of Surat City. Int. J. Curr. Res. Rev. 2021, 13, 137–142. [Google Scholar] [CrossRef]
- Oswald, T.K.; Rumbold, A.R.; Kedzior, S.G.E.; Moore, V.M. Psychological impacts of “screen time” and “green time” for children and adolescents: A systematic scoping review. PLoS ONE 2020, 15, e0237725. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Hatano, Y.; Pangrazi, R.P.; Kang, M. Revisiting “How Many Steps Are Enough?”. Med. Sci. Sport. Exerc. 2008, 40, S537–S543. [Google Scholar] [CrossRef] [PubMed]
- Warburton, D.E.R.; Bredin, S.S.D. Health benefits of physical activity: A systematic review of current systematic reviews. Curr. Opin. Cardiol. 2017, 32, 541–556. [Google Scholar] [CrossRef] [PubMed]
- Organización Mundial de la Salud. Actividad Física para la Salud: Más Personas Activas para un Mundo más Sano: Proyecto de Plan de Acción Mundial sobre Actividad Física 2018–2030: Informe del Director General; Organización Mundial de la Salud: Geneva, Switzerland, 2018. [Google Scholar]
- Hansen, M.M.; Jones, R.; Tocchini, K. Shinrin-Yoku (Forest Bathing) and Nature Therapy: A State-of-the-Art Review. Int. J. Environ. Res. Public Health 2017, 14, 851. [Google Scholar] [CrossRef] [PubMed]
- Marselle, M.R.; Stadler, J.; Korn, H.; Irvine, K.N.; Bonn, A. Biodiversity and Health in the Face of Climate Change; Springer: Cham, Switzerland, 2019. [Google Scholar]
- Després, C.; Larivière-Lajoie, A.A.; Tremblay-Lemieux, S.; Legault, M.; Piché, D. Healthy Schools, Healthy Lifestyles: Literature Review. In Health and Well-Being for Interior Architecture, 1st ed.; Kopec, D., Ed.; Routledge: Oxfordshire, UK, 2017; pp. 123–136. [Google Scholar]
- Sanford, J.A.; Hernandez, S.C. Universal design, design for aging in place, and habilitative design in residential environments. In Health and Well-Being for Interior Architecture, 1st ed.; Kopec, D., Ed.; Routledge: Oxfordshire, UK, 2017; pp. 137–147. [Google Scholar]
- Coughlin, S.S.; Whitehead, M.; Sheats, J.Q.; Mastromonico, J.; Smith, S. A Review of Smartphone Applications for Promoting Physical Activity. Jacobs J. Community Med. 2016, 2, 021. [Google Scholar]
- Sallis, J.F.; Saelens, B.E. Assessment of Physical Activity by Self-Report: Status, Limitations, and Future Directions. Res. Q. Exerc. Sport 2015, 71, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Thakkar, H.K.; Chowdhury, S.R.; Bhoi, A.K.; Barsocchi, P. Applications of wearable technologies in healthcare: An analytical study. In 5G IoT and Edge Computing for Smart Healthcare; Kumar Bhoi, A., Nath Sur, S., Costa de Albuquerque, V.H., Barsocchi, P., Eds.; Academic Press: London, UK, 2022; Volume 1, pp. 279–299. [Google Scholar]
- Western, M.J.; Peacock, O.J.; Stathi, A.; Thompson, D. The understanding and interpretation of innovative technology-enabled multidimensional physical activity feedback in patients at risk of future chronic disease. PLoS ONE 2015, 10, e0126156. [Google Scholar] [CrossRef]
- Patel, M.S.; Asch, D.A.; Volpp, K.G. Wearable devices as facilitators, not drivers, of health behavior change. JAMA 2015, 313, 459–460. [Google Scholar] [CrossRef] [PubMed]
- Freedson, P.S.; Miller, K. Objective monitoring of physical activity using motion sensors and heart rate. Res. Q. Exerc. Sport 2000, 71, S21–S29. [Google Scholar] [CrossRef] [PubMed]
- Broderick, J.M.; Ryan, J.; O’Donnell, D.M.; Hussey, J. A guide to assessing physical activity using accelerometry in cancer patients. Support. Care Cancer 2014, 22, 1121–1130. [Google Scholar] [CrossRef]
- Robertson, W.; Stewart-Brown, S.; Wilcock, E.; Oldfield, M.; Thorogood, M. Utility of accelerometers to measure physical activity in children attending an obesity treatment intervention. J. Obes. 2011, 2011, 398918. [Google Scholar] [CrossRef]
- Hills, A.P.; Mokhtar, N.; Byrne, N.M. Assessment of physical activity and energy expenditure: An overview of objective measures. Front. Nutr. 2014, 1, 5. [Google Scholar] [CrossRef]
- Yang, Y.; Schumann, M.; Le, S.; Cheng, S. Reliability and validity of a new accelerometer-based device for detecting physical activities and energy expenditure. PeerJ 2018, 6, e5775. [Google Scholar] [CrossRef]
- Yang, C.; Hsu, Y. A Review of Accelerometry-Based Wearable Motion Detectors for Physical Activity Monitoring. Sensors 2010, 10, 7772–7788. [Google Scholar] [CrossRef]
- Golbus, J.R.; Pescatore, N.A.; Nallamothu, B.K.; Shah, N.; Kheterpal, S. Wearable device signals and home blood pressure data across age, sex, race, ethnicity, and clinical phenotypes in the Michigan Predictive Activity & Clinical Trajectories in Health (MIPACT) study: A prospective, community-based observational study. Lancet Digit. Health 2021, 3, e707–e715. [Google Scholar] [CrossRef]
- Pennestri, F.; Banfi, G.; Tomaiuolo, R. Remote decentralized clinical trials: A new opportunity for laboratory medicine. Clin. Chem. Lab. Med. 2023; Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Ali, Z.; Valk, T.J.; Bjerre-Christensen, T.; Brandt, S.; Isberg, A.P.; Jensen, M.L.; Helledi, L.S.; Kaas, A.; Thomsen, S.F.; Andersen, A.D.; et al. Exploring Decentralized Glucose and Behaviometric Monitoring of Persons with Type 2 Diabetes in the Setting of a Clinical Trial. J. Diabetes Sci. Technol. 2023, 17, 117–124. [Google Scholar] [CrossRef]
- Hartung, V.; Sarshar, M.; Karle, V.; Shammas, L.; Rashid, A.; Roullier, P.; Eilers, C.; Maurer, M.; Flachenecker, P.; Pfeifer, K.; et al. Validity of Consumer Activity Monitors and an Algorithm Using Smartphone Data for Measuring Steps during Different Activity Types. Int. J. Environ. Res. Public Health 2020, 17, 9314. [Google Scholar] [CrossRef]
- Bravata, D.M.; Smith-Spangler, C.; Sundaram, V.; Gienger, A.L.; Lin, N.; Lewis, R.; Stave, C.D.; Olkin, I.; Sirard, J.R. Using pedometers to increase physical activity and improve health: A systematic review. JAMA 2007, 298, 2296–2304. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Bassett, D.R. How Many Steps/Day Are Enough? Sport. Med. 2004, 34, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hultquist, C.N.; Albright, C.; Thompson, D.L. Comparison of walking recommendations in previously inactive women. Med. Sci. Sport. Exerc. 2005, 37, 676–683. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Ming, W.K.; You, J.H. The Cost-Effectiveness of Digital Health Interventions on the Management of Cardiovascular Diseases: Systematic Review. J. Med. Internet Res. 2019, 21, e13166. [Google Scholar] [CrossRef]
- Gentili, A.; Failla, G.; Melnyk, A.; Puleo, V.; Tanna, G.L.D.; Ricciardi, W.; Cascini, F. The cost-effectiveness of digital health interventions: A systematic review of the literature. Front. Public Health 2022, 10, 787135. [Google Scholar] [CrossRef] [PubMed]
- Mollee, J.S.; Middelweerd, A.; Kurvers, R.L.; Klein, M.C.A. What technological features are used in smartphone apps that promote physical activity? A review and content analysis. Pers. Ubiquitous Comput. 2017, 21, 633–643. [Google Scholar] [CrossRef]
- Kageyama, I.; Kurata, K.; Miyashita, S.; Lim, Y.; Sengoku, S.; Kodama, K. A Bibliometric Analysis of Wearable Device Research Trends 2001-2022-A Study on the Reversal of Number of Publications and Research Trends in China and the USA. Int. J. Environ. Res. Public Health 2022, 19, 16427. [Google Scholar] [CrossRef] [PubMed]
- Koyama, Y.; Nishiyama, M.; Watanabe, K. Physical activity recognition using hetero-core optical fiber sensors embedded in a smart clothing. In Proceedings of the 2018 IEEE 7th Global Conference on Consumer Electronics (GCCE), Nara, Japan, 9–12 October 2018; pp. 71–72. [Google Scholar]
- Wang, Z.; Yang, Z.; Dong, T. A Review of Wearable Technologies for Elderly Care that Can Accurately Track Indoor Position, Recognize Physical Activities and Monitor Vital Signs in Real Time. Sensors 2017, 17, 341. [Google Scholar] [CrossRef] [PubMed]
| Target | Components | Descriptions/Actions |
|---|---|---|
| Creating physically active societies | Social norms and attitudes | To achieve a paradigm shift throughout society by improving the knowledge, understanding, and appreciation of the multiple benefits of regular physical activity according to ability and at all ages. |
| Creating active environments | Spaces and places | To create and maintain environments that promote and safeguard the rights of all people, of all ages, to enjoy equitable access to safe places and spaces in their cities and communities where they can engage in regular physical activity according to their abilities. |
| Promoting active populations | Programs and opportunities | To create and promote access to opportunities and programs, in multiple settings, to help people of all ages and abilities participate regularly in physical activity, either alone or with their families and communities. |
| Creating active systems | Governance and policy enablers | To enable elements of governance and policy to build and strengthen leadership, governance, multisectoral partnerships, workforce capacities, advocacy, and information systems across sectors to achieve excellence in resource mobilization and the implementation of coordinated international, national, and subnational actions to increase physical activity and reduce sedentary lifestyles. |
| Device | Sensor | Sensor Location | Advantages/Disadvantages | Variables |
|---|---|---|---|---|
| SenseWear, BodyMedia Inc. (CAM) | 2-axis accelerometer | Upper arm | High concordance to assess PA and EE. Requires specific software to interpret data. Low sensitivity in subjects with functional mobility limitations. | Acceleration and EE (METs). |
| CT1/RT3, StayHealthy Inc. (CAM/ RGAM) | 3-axis accelerometer | Wrist or hip (RT3) | Detailed information on activities of daily living. May present difficulties in manipulation (switching on/off) in older individuals or persons with disabilities or mobility difficulties. | Activities of daily living (NEPA) and displacements (as vector magnitude units). |
| AMP331, Dynastream Innovations Inc. (CAM) | 2-axis accelerometer | Ankle | Due to its dimensions, it is comfortable to use for several consecutive days. Useful to control the intensity of physical exercise. | Activities of daily living (NEPA), vertical and horizontal accelerations, number of steps, frequency and stride speed, and EE. |
| wGT3X-BT, Actigraph LLC (RGAM) | 3-axis accelerometer, time-of-use sensor, ambient light sensor | Wrist or hip | High concordance to assess PA and EE. Small device and easy location. Requires specific software to interpret data. Overestimates EE when using motor vehicle transportation. | Acceleration (as vector magnitude units) and EE. |
| StepWatch, Orthocare Innovations (CAM) | 2-axis accelerometer | Ankle | Portable device designed to track and monitor physical activity. Useful for persons with lower-limb disabilities or mobility difficulties. High precision and measures PA on different surfaces such as soil, grass, carpets, etc. High cost compared to other devices. It needs to be calibrated to ensure accurate results. Some people find it uncomfortable to wear the device on their ankle or wrist all day. | Activities of daily living, duration and pause time between them (walking, jogging, running or sprinting, and sitting or standing), EE, steps per minute, moderate-to-vigorous PA, and total PA. |
| activPAL, PAL Technologies Ltd. (CAM) | Accelerometer | Thigh | Useful for different populations (children, older adults, and patients with chronic diseases) and more user-friendly. Expensive device. Must be placed on upper thigh, which is uncomfortable for some users. Not water-resistant. | Activities of daily living (NEPA) and displacements (body inclinations in degrees). Light and moderate-to- vigorous PA. |
| IDEEA, MiniSun (CAM) | 2-axis accelerometer | Chest, thigh, or ankle | Uses several sensors on different parts of the body at the same time (foot, ankle, thigh, and chest). Requires constant adjustment of the sensors to avoid loss of information. Underestimates EE in continuous static arm activities such as cycling or arm exercises and slow walking. Slightly overestimates EE in other NEPA activities. Not water-resistant. | Activities of daily living (NEPA), HR, EE, and acceleration. |
| Inspire, Fitbit Inc. (CAM) | 3-Axis Accelerometer | Wrist or hip | Compatible with a variety of applications (apps) and fitness platforms. Low cost. Not very accurate in PA measurement and does not measure HR continuously, limiting the measurement of moderate-to-vigorous PA. Low battery life. | Activities of daily living, duration and pause time between them (walking, jogging, running or sprinting, and sitting or standing), and EE. |
| VivoFit 4, Garming Ltd. (CAM) | Accelerometer | Wrist | Compatible with the Garmin Connect app and is water-resistant. No GPS and no HR. | Activities of daily living (NEPA), sleep quality, EE, and total PA. |
| Vivomove HR, Garming Ltd. (CAM) | Accelerometer, barometer, photoplethysmography, ambient light sensor | Wrist | Compatible with the Garmin Connect app, long battery life, and water-resistant. | Activities of daily living (NEPA), EE and total PA, and sleep monitoring. |
| Mi Band 3, Xiami Corp. (CAM) | 3-axis accelerometer, photoplethysmography | Wrist | Compatible with the Mi Fit app, water-resistant, and affordable price. No GPS and no HR. | Activities of daily living (NEPA), EE, and total PA. |
| Pulse HR, Withings (CAM) | 3-axis accelerometer, photoplethysmography, ambient light sensor | Wrist | Multisport tracking, connected GPS, and an OLED screen that displays full smartphone notifications for calls, texts, events, and all of your favorite apps. | HR, training zones, and sleep quality. |
| Steel HR, Withings (CAM) | 3-axis accelerometer, day and night motion sensor | Wrist | Compatible with the Health Mate app, water-resistant, and call and message notification. | Activities of daily living (NEPA), EE and total PA, sleep monitoring, EE, and HR. |
| TriTrac-R3D, Madison, WI, USA | 3-Axis Accelerometer | Hip | Good concordance to assess PA and EE during physical exercise. Very high correlation when evaluating HR in children. Does not show good accuracy in sedentary individuals. Requires software to estimate total EE (kJ/min). | Activities of daily living (NEPA), EE, and acceleration. |
| Steps per Day | Physical Activity Level |
|---|---|
| <5000 | Insufficiently active |
| 5000–7499 | Somewhat active |
| 7500–9999 | Moderately active |
| >10,000 | Active |
| >12,500 | Highly active |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bonilla, D.A.; Peralta-Alzate, J.O.; Bonilla-Henao, J.A.; Cannataro, R.; Cardozo, L.A.; Vargas-Molina, S.; Stout, J.R.; Kreider, R.B.; Petro, J.L. Insights into Non-Exercise Physical Activity on Control of Body Mass: A Review with Practical Recommendations. J. Funct. Morphol. Kinesiol. 2023, 8, 44. https://doi.org/10.3390/jfmk8020044
Bonilla DA, Peralta-Alzate JO, Bonilla-Henao JA, Cannataro R, Cardozo LA, Vargas-Molina S, Stout JR, Kreider RB, Petro JL. Insights into Non-Exercise Physical Activity on Control of Body Mass: A Review with Practical Recommendations. Journal of Functional Morphology and Kinesiology. 2023; 8(2):44. https://doi.org/10.3390/jfmk8020044
Chicago/Turabian StyleBonilla, Diego A., Javier O. Peralta-Alzate, Jhonny A. Bonilla-Henao, Roberto Cannataro, Luis A. Cardozo, Salvador Vargas-Molina, Jeffrey R. Stout, Richard B. Kreider, and Jorge L. Petro. 2023. "Insights into Non-Exercise Physical Activity on Control of Body Mass: A Review with Practical Recommendations" Journal of Functional Morphology and Kinesiology 8, no. 2: 44. https://doi.org/10.3390/jfmk8020044
APA StyleBonilla, D. A., Peralta-Alzate, J. O., Bonilla-Henao, J. A., Cannataro, R., Cardozo, L. A., Vargas-Molina, S., Stout, J. R., Kreider, R. B., & Petro, J. L. (2023). Insights into Non-Exercise Physical Activity on Control of Body Mass: A Review with Practical Recommendations. Journal of Functional Morphology and Kinesiology, 8(2), 44. https://doi.org/10.3390/jfmk8020044













