Effectiveness of Therapeutical Interventions on the Scapulothoracic Complex in the Management of Patients with Subacromial Impingement and Frozen Shoulder: A Systematic Review
Abstract
1. Introduction
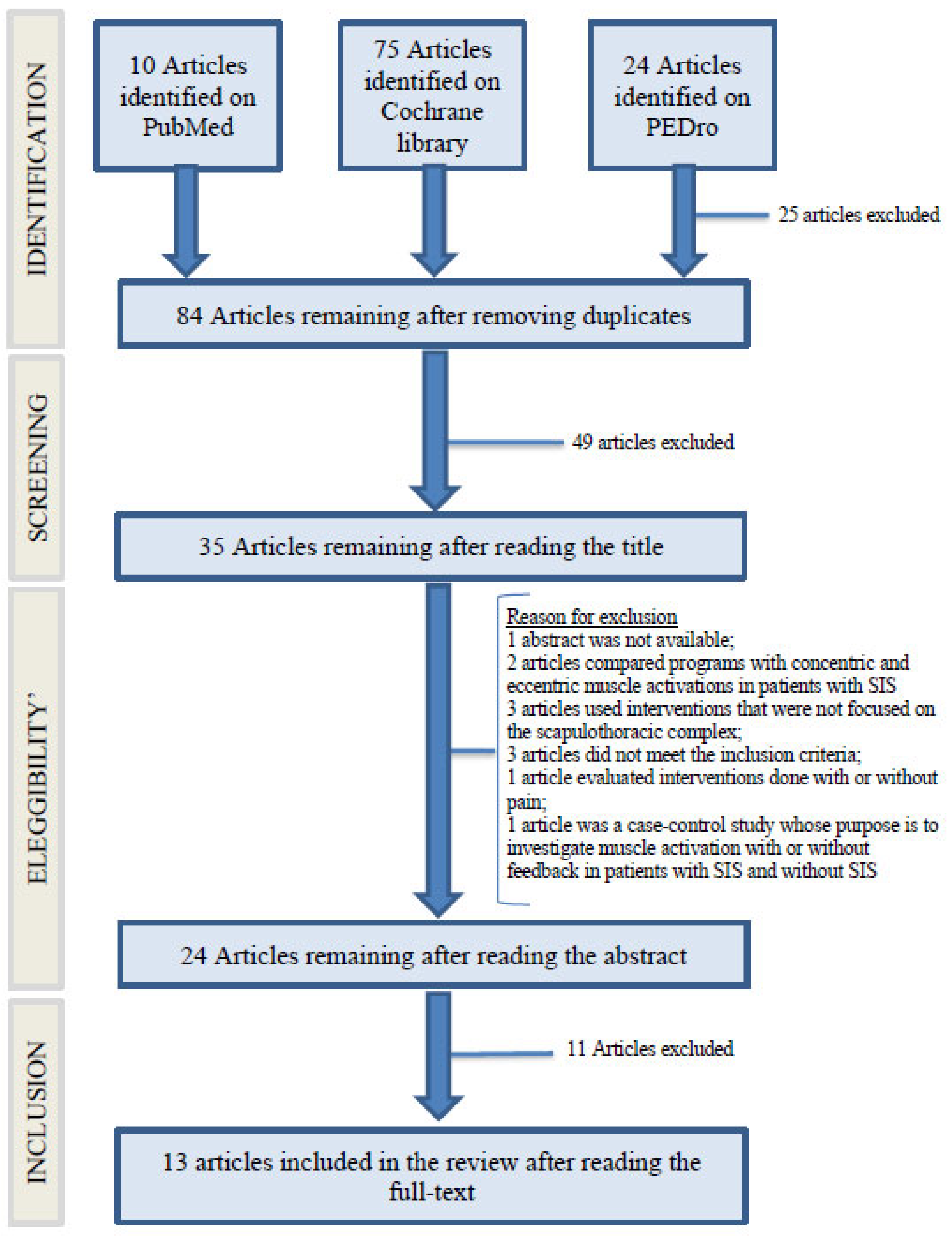
2. Materials and Methods
- PubMed: (Shoulder pain) AND ((Scapular kinematic) AND ((shoulder impingement) OR (Frozen Shoulder)) AND ((manual therapy) OR (feedback) OR (exercise therapy));
- PEDro: Title and Abstract: (shoulder pain) AND (scapular function);Problem: pain;Part of the body: upper arm, shoulder or shoulder girdle;
- Subdiscipline: musculoskeletal;
- Method: clinical trial;
- Published since: 2011.
- Cochrane library: (scapular function) AND (shoulder pain) AND ((shoulder impingement) OR (frozen shoulder)).
2.1. Studies Selection
2.2. Studies Included
2.3. Study Design
2.4. Type of Participants
2.5. Type of Interventions
2.6. Type of Outcomes
3. Results
| Study | Outcome Measure Tool | Results | |||||
|---|---|---|---|---|---|---|---|
| Study [1] | NPRS | Pre-intervention | Post-intervention | ||||
| Thoracic thrust (average) | 3.5 | 2.6 | |||||
| Simulated thrust (average) | 3.6 | 2.4 | |||||
| Study [17] | Penn Shoulder Score | Median of changes | |||||
| Supine Thrust | Seated Thrust | Simulated Thrust | |||||
| 5.0 (2.0–7.0) | 5.0 (1.5–8.2) | 5.0 (2.0–9.8) | |||||
| Study [19] | NPRS | Pre-intervention | Post-intervention | ||||
| Thoracic thrust (average) | 3.3 | 2.4 | |||||
| Simulated Thrust (average) | 2.4 | 2.2 | |||||
| Study [20] | NPRS | Pre-intervention | 2 days pre-intervention | 2 days post-intervention | Follow-up | ||
| Thoracic thrust (average) | 3.3 | 2.5 | 2.4 | 2.4 | |||
| Simulated Thrust (average) | 2.7 | 2.4 | 2.4 | 2.9 | |||
| Study [22] | VAS at rest (from 0 to 100 mm) | Pre-intervention | Post-intervention | ||||
| Exercise plus manual therapy (average) | 19.3 ± 27.6 | 6.3 ± 11.6 | |||||
| Only exercise (average) | 10.3 ± 14.1 | 3.6 ± 6.1 | |||||
| Study [13] | VAS (on movement) | 0 week | 2 week | 3 week | 7 week | 11 week | |
| Scapular mobilization group (average) | 7.0 | 5.0 | 3.8 | 3.0 | 2.3 | ||
| False scapular mobilizations group (average) | 7.3 | 5.6 | 4.8 | 3.8 | 3.7 | ||
| Group with exercises under supervision (average) | 7.1 | 5.1 | 4.0 | 3.6 | 2.9 | ||
| Study [14] | VAS (during activity) | Pre-intervention | 6 week | 12 week | |||
| Intervention group (average) | 4.84 | 1.52 | 0.38 | ||||
| Control group (average) | 5.32 | 2.36 | 1.26 | ||||
| Study [15] | VAS (on movement) | Before treatment | After treatment | ||||
| Intervention group (average) | 5.7 ± 2.6 | 3.0 ± 1.9 | |||||
| Control group (average) | 6.3 ± 1.9 | 5.1 ± 2.0 | |||||
| Study [16] | NPRS | Pre-intervention | 4 week | 8 week | 16 week | ||
| Intervention group (average) | 3.9 | 1.5 | 1.3 | 1.2 | |||
| Control group (average) | 3.7 | 2.7 | 1.8 | 0.5 | |||
| Study [18] | VAS | Before treatment | Follow-up | ||||
| Treatment with feedback (average) | 6.4 | 2.4 | |||||
| Treatment without feedback (average) | 6.1 | 3.1 | |||||
| Control group (average) | 5.7 | 6.2 | |||||
| Study [21] | VAS | Before intervention | After intervention | ||||
| Scapular PNF (average) | 6.07 | 4.16 | |||||
| Classic exercises (average) | 4.67 | 3.97 | |||||
| Control group (average) | 6.55 | 4.22 | |||||
| Study [23] | NPRS | Before intervention | After intervention | ||||
| Intervention group (average) | 8.00 | 3.93 | |||||
| Control group (average) | 6.67 | 4.80 | |||||
3.1. Sample
3.1.1. Gender
3.1.2. Enrollment
3.1.3. Setting
3.1.4. Age
3.1.5. Diagnostic Criteria
3.2. Type of Interventions
3.3. Approaches
- Manual therapy in patients with SIS alone or performed in combination with stretching and strengthening exercises [22];
- Therapeutic exercise programs including interventions on the scapula-thoracic complex in patients with SIS [18];
- Therapeutic exercise programs including interventions on the scapula-thoracic complex in patients with frozen shoulder [21].
3.4. Contents of Therapeutic Interventions
3.4.1. Manual Therapy in Patients with Subacromial Impingement Syndrome (SIS)
3.4.2. Therapeutic Exercise Programs including Interventions on Scapulo-Thoracic Complex in Patients with SIS
- Exercises including isometry, isotonic, concentric and eccentric, and stretching, which were all focused on the scapula with tactile and verbal feedback [18];
- Manual mobilization, stretching, and training in motor control of the scapula [15];
- Strengthening exercises for the peri-scapular muscles combined with scapular stabilization exercises to emphasize scapular retraction and depression [16];
- A supervised combination of closed and open kinetic chain scapular stabilization exercises, with shoulder strengthening and stretching [14];
- Scapular mobilization, preceded by hot packs and TENS [13].
3.4.3. Therapeutic Exercise Programs including Interventions on the Scapulo-Thoracic Complex in Patients with Frozen Shoulder
- Warm compresses, TENS, and ultrasounds with scapular PNF (Proprioceptive Neuromuscular Facilitation) interventions [21];
- Standard treatment with passive mobilization, stretching and physical therapy in combination with scapular mobilization, and end range mobilization [10];
- Paraffin wax therapy, scapular mobilization, and home exercise program [23].
3.5. Professional Figures Involved
Type of Control Groups
- Isometric, isotonic in concentric, and eccentric exercise and stretching all focused on the scapula [18];
- Therapeutic exercises and manual therapy [15];
- Periscapular strengthening exercises [16];
- Shoulder stretching and strengthening exercises [14];
- In one group, false scapular mobilizations were performed, and in another one, strengthening and stretching exercises were performed under supervision [13].
3.6. Type of Outcome Measures
3.6.1. Shoulder Pain
- Penn Shoulder Score (PSS);
- Numeric pain rating scale (NPRS);
- Western Ontario rotator cuff index (WORC);
- Visual analog scale (VAS).
- Verbal numeric rating scale (VNRS);
- NPRS;
- VAS.
- NPRS;
- VAS.
3.6.2. Shoulder Function
- Penn Shoulder Score (PSS);
- Disability of the Arm, Shoulder and Hand (DASH), the normal and Brazilian versions;
- Global Rating of Change (GROC).
- Quick DASH Turkish version and DASH standard versions;
- Shoulder Pain and Disability index (SPADI-br), Turkish and standard versions;
- Shoulder disability questionnaire (SDQ).
- FLEX-SF;
- Shoulder Constant Score;
- Simple Shoulder test.
3.6.3. Scapular Kinematics
- Digital inclinometer;
- Flock of Birds hardware;
- Sistema 3SPACE FASTRAK.
- Electromagnetic tracking tools;
- Digital inclinometer;
- Infrared cameras.
- 3SPACE FASTRAK System;
- Lateral Scapular Slide Test.
3.7. Follow-Up
3.8. Qualitative Analysis on the Effectiveness of Interventions
3.9. Improvements as a Result of Manual Therapy Interventions on Pain, Function, and Scapular Kinematics in Patients with SIS
3.9.1. Efficacy of Manual Therapy in the Improvement of Shoulder Pain in Patients with SIS
3.9.2. Efficacy of Manual Therapy in Improving Shoulder Function in Patients with SIS
| Study | Outcome Measure Tool | Results | ||
|---|---|---|---|---|
| Study [1] | Penn Shoulder Score | Pre-intervention | Post-intervention | |
| Thoracic thrust (average) | 71.8 ± 11.1 | 80.4 ± 10.9 | ||
| Simulated Thrust (average) | 70.9 ± 12.5 | 80.2 ± 11.2 | ||
| Study [17] | Penn Shoulder Score | Median of changes | ||
| Supine Thrust | Seated Thrust | Simulated Thrust | ||
| 2.0 (1.0–5.0) | 2.6 (0.8–6.3) | 3.8 (0.0–8.7) | ||
| Study [20] | DASH | Differences between initial assessment and 2 day pre-intervention | Differences between initial assessment and follow-up | |
| Thoracic thrust (average) | −3.9 (−6.3 a −1.6) | −4.6 (−7.2 a −2.0) | ||
| Simulated Thrust (average) | −1.0 (0.8 a −2.9) | −4.7 (−2.1 a −7.4) | ||
| Study [22] | DASH | Pre intervento | Post-intervento | |
| Exercise + manual therapy (average) | 25.3 ± 16.1 | 12.4 ± 12.3 | ||
| Only exercise (average) | 20.8 ± 10.4 | 11.7 ± 9.5 | ||
3.9.3. Efficacy of Manual Therapy in Improving Scapular Kinematics in Patients with SIS
3.10. Improvements Obtained on Pain, Function, and Scapular Kinematics through Various Therapeutic Exercise Programs, in Patients with SIS
3.10.1. Efficacy of Various Therapeutic Exercises Programs in Patients with SIS in Improving Shoulder Pain
3.10.2. Effectiveness of Various Therapeutic Exercise Programs in Patients with SIS in Improving Shoulder Function
| Study | Outcome Measure Tools | Results | |||||
|---|---|---|---|---|---|---|---|
| Study [13] | DASH | 0 week | 2 week | 3 week | 7 week | 11 week | |
| Scapular mobilization group (average) | 41.4 | 32.1 | 29.7 | 19.5 | 28.5 | ||
| False scapular mobilizations group (average) | 41.7 | 31.0 | 25.6 | 18.8 | 24.3 | ||
| Group with supervised exercises (average) | 37.5 | 29.6 | 27.2 | 23.4 | 20.5 | ||
| Study [14] | SPADI (disability) | Pre-intervention | 6 week | 12 week | |||
| Intervention group (average) | 36.08 ± 22.23 | 16.82 ± 19.59 | 7.00 ± 10.34 | ||||
| Control group (average) | 41.58 ± 22.96 | 24.12 ± 17.26 | 19.42 ± 20.16 | ||||
| Study [15] | SDQ | Before treatment | After treatment | ||||
| Intervention group (average) | 55.9 ± 14.6 | 35.0 ± 14.0 | |||||
| Control group (average) | 50.9 ± 11.9 | 48.7 ± 11.3 | |||||
| Study [16] | SPADI-br | Pre-interv | 4 week | 8 week | 16 week | ||
| Intervention group (average) | 65.7 | 43.5 | 39.7 | 34.2 | |||
| Control group (average) | 63.3 | 49.8 | 37.1 | 32.8 | |||
| Study [18] | DASH | Before treatment | Follow-up | ||||
| Treatment with feedback (average) | 26.4 | 13.2 | |||||
| Treatment without feedback (average) | 24.4 | 17.3 | |||||
| Control group (average) | 23.1 | 25.0 | |||||
3.10.3. Efficacy of Various Therapeutic Exercise Programs in Improving Scapular Kinematics in Patients with SIS
- Ref. [14] Greater external rotation and scapular posterior tilt were observed in the group who performed scapular stabilizations than those in the control group. Furthermore, at follow-ups there were slight improvements in both groups in scapular rotation above 60°–90°–120° of humeral elevation and 90° of humeral lowering. The most significant improvements were noted in scapular rotation above 30° of humeral elevation and 60° of humeral lowering in the intervention group (Table 1).
3.11. Improvements Obtained on Pain, Function, and Scapular Kinematics in Various Programs with Therapeutic Exercises in Patients with Frozen Shoulder
3.11.1. Efficacy of Various Therapeutic Exercises Programs in Patients with Frozen Shoulder in Improving Shoulder Pain
- Ref. [21], the pain improved in all three groups, but there was a greater improvement in the group treated with scapular PNFs and physical therapy and in the group treated with physical therapy compared with that of the control group treated with classical exercises and physical therapy. An explanation of these results may be due to the fact that the intensity of pain measured before the interventions was greater in the two groups in which greater improvements were found than that in the third group (Table 2).
3.11.2. Efficacy of Various Therapeutic Exercises Programs in Patients with Frozen Shoulder in Improving Shoulder Function
| Study | Outcome Measure Tool | Results | |||
|---|---|---|---|---|---|
| Study [10] | FLEX-SF | Pre-intervention | 4 week | 8 week | |
| Intervention group with criterion (average) | 31.7 | 32.7 | 39.8 | ||
| Control group with criterion (average) | 30.8 | 31.6 | 32.1 | ||
| Control group without criterion (average) | 32.8 | 34.5 | 37.2 | ||
| Study [21] | Simple Shoulder Test | Pre-intervention | Post-intervention | ||
| Scapular PNF (average) | 6.77 | 8.16 | |||
| Classic exercises (average) | 6.94 | 8.47 | |||
| Control group (average) | 5.94 | 7.11 | |||
| Study [23] | Constant score | Pre-intervention | Post-intervention | ||
| Intervention group (average) | 48.69 | 78.13 | |||
| Control group (average) | 48.81 | 67.16 | |||
3.11.3. Efficacy of Various Therapeutic Exercises Programs in Patients with Frozen Shoulder in Improving Shoulder Kinematics
4. Discussion
4.1. Pain and Function Outcomes
4.2. Scapular Kinematics Outcomes
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kardouni, J.R.; Pidcoe, P.E.; Shaffer, S.W.; Finucane, S.D.; Cheatham, S.A.; Sousa, C.O.; Michener, L.A. Thoracic Spine Manipulation in Individuals With Subacromial Impingement Syndrome Does Not Immediately Alter Thoracic Spine Kinematics, Thoracic Excursion, or Scapular Kinematics: A Randomized Controlled Trial. J. Orthop. Sports Phys. Ther. 2015, 45, 527–538. [Google Scholar] [CrossRef] [PubMed]
- Garving, C.; Jakob, S.; Bauer, I.; Nadjar, R.; Brunner, U.H. Impingement Syndrome of the Shoulder. Dtsch. Ärztebl. Int. 2017, 114, 765. [Google Scholar] [CrossRef] [PubMed]
- Linaker, C.H.; Walker-Bone, K. Shoulder disorders and occupation. Best Pract. Res. Clin. Rheumatol. 2015, 29, 405–423. [Google Scholar] [CrossRef] [PubMed]
- Umer, M.; Qadir, I.; Azam, M. Subacromial impingement syndrome. Orthop. Rev. 2012, 4, 18. [Google Scholar] [CrossRef]
- Habermeyer, P.; Lichtenberg, S.; Loew, W.; Magosch, P.; Martetschläger, F.; Tauber, M. Schulterchirurgie; Elsevier: Berlin, Germany, 2017. [Google Scholar]
- Page, P. Shoulder muscle imbalance and subacromial impingement syndrome in overhead athletes. Int. J. Sports Phys. Ther. 2011, 6, 51–58. [Google Scholar]
- Ludewig, P.M.; Reynolds, J.F. The Association of Scapular Kinematics and Glenohumeral Joint Pathologies. J. Orthop. Sports Phys. Ther. 2009, 39, 90–104. [Google Scholar] [CrossRef]
- Alizadehkhaiyat, O.; Roebuck, M.M.; Makki, A.T.; Frostick, S.P. Postural alterations in patients with subacromial impingement syndrome. Int. J. Sports Phys. Ther. 2017, 12, 1111–1120. [Google Scholar] [CrossRef]
- Neumann, D.A. Kinesiology of the Musculoskeletal System; Elsevier: Maryland Heights, MO, USA, 2016. [Google Scholar]
- Yang, J.; Jan, M.-H.; Chang, C.; Lin, J. Effectiveness of the end-range mobilization and scapular mobilization approach in a subgroup of subjects with frozen shoulder syndrome: A randomized control trial. Man. Ther. 2012, 17, 47–52. [Google Scholar] [CrossRef]
- PRISMA-P Group; Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1–9. [Google Scholar] [CrossRef]
- Schardt, C.; Adams, M.B.; Owens, T.; Keitz, S.; Fontelo, P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med. Inform. Decis. Mak. 2007, 7, 1–6. [Google Scholar] [CrossRef]
- Aytar, A.; Baltaci, G.; Uhl, T.; Tuzun, H.; Oztop, P.; Karatas, M. The Effects of Scapular Mobilization in Patients With Subacromial Impingement Syndrome: A randomized, double-blind, placebo-controlled clinical trial. J. Sport Rehabil. 2015, 24, 116–129. [Google Scholar] [CrossRef]
- Turgut, E.; Duzgun, I.; Baltaci, G. Effects of Scapular Stabilization Exercise Training on Scapular Kinematics, Disability, and Pain in Subacromial Impingement: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2017, 98, 1915–1923.e3. [Google Scholar] [CrossRef]
- Struyf, F.; Nijs, J.; Mollekens, S.; Jeurissen, I.; Truijen, S.; Mottram, S.; Meeusen, R. Scapular-focused treatment in patients with shoulder impingement syndrome: A randomized clinical trial. Clin. Rheumatol. 2013, 32, 73–85. [Google Scholar] [CrossRef]
- Hotta, G.H.; de Assis Couto, A.G.; Cools, A.M.; McQuade, K.J.; de Oliveira, A.S. Effects of adding scapular stabilization exercises to a periscapular strengthening exercise program in patients with subacromial pain syndrome: A randomized controlled trial. Musculoskelet. Sci. Pract. 2020, 49, 102171. [Google Scholar] [CrossRef]
- Grimes, D.T. Making and breaking symmetry in development, growth and disease. Development 2019, 146, dev170985. [Google Scholar] [CrossRef]
- Moslehi, M.; Letafatkar, A.; Miri, H. Feedback improves the scapular-focused treatment effects in patients with shoulder impingement syndrome. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 2281–2288. [Google Scholar] [CrossRef]
- Haik, M.N.; Alburquerque-Sendín, F.; Silva, C.Z.; Siqueira-Junior, A.L.; Ribeiro, I.L.; Camargo, P.R. Scapular Kinematics Pre– and Post–Thoracic Thrust Manipulation in Individuals With and Without Shoulder Impingement Symptoms: A Randomized Controlled Study. J. Orthop. Sports Phys. Ther. 2014, 44, 475–487. [Google Scholar] [CrossRef]
- Haik, M.N.; Alburquerque-Sendín, F.; Camargo, P.R. Short-Term Effects of Thoracic Spine Manipulation on Shoulder Impingement Syndrome. Arch. Phys. Med. Rehabil. 2017, 98, 1594–1605. [Google Scholar] [CrossRef]
- Balcı, N.C.; Yuruk, Z.O.; Zeybek, A.; Gulsen, M.; Tekindal, M.A. Acute effect of scapular proprioceptive neuromuscular facilitation (PNF) techniques and classic exercises in adhesive capsulitis: A randomized controlled trial. J. Phys. Ther. Sci. 2016, 28, 1219–1227. [Google Scholar] [CrossRef]
- Camargo, P.R.; Alburquerque-Sendín, F.; Avila, M.A.; Haik, M.N.; Vieira, A.; Salvini, T.F. Effects of Stretching and Strengthening Exercises, With and Without Manual Therapy, on Scapular Kinematics, Function, and Pain in Individuals With Shoulder Impingement: A Randomized Controlled Trial. J. Orthop. Sports Phys. Ther. 2015, 45, 984–997. [Google Scholar] [CrossRef]
- Pragassame, S.A.; Kurup, V.M.; Kifayathunnisa, A. Effectiveness of Scapular Mobilisation in the Management of Patients with Frozen Shoulder—A Randomised Control Trial. J. Clin. Diagn. Res. 2019, 13, 5–9. [Google Scholar] [CrossRef]
| Author and Year of Publication | Study Design and Level of Evidence (E) | Number (N) of Patients and Their Characteristics | Intervention Groups, Control Groups and Number of Treatments | Objectives | Evaluation & Follow-Up | Results |
|---|---|---|---|---|---|---|
| Joseph R. Kardouni et al., 2015 [1] | RCT E = 1b | Patients with impingement; N = 52; Females = 24; Males = 28; Age (years); Experimental group = 18–59 (average 30.8); Control group = 18–59 (average 33.2). | Experimental group n = 26. 3 high-speed, low-amplitude thrusts, one for the low, one for the middle, and one for the high thoracic spine, each performed 2 times. Control group n = 26. Same thoracic thrust, but simulated. | Thoracic and shoulder kinematics during limb elevation: 3SPACE FASTRAK, which is an electromagnetic tracking tool; Pain: numeric pain-rating scale (NPRS); Thoracic exursion: electromagnetic capture system; Function: Penn Shoulder Score (PSS). | Immediately before and immediately after treatment, thoracic and scapula kinematics and NPRS were evaluated. From 24 to 48 h later, NPRS, PSS, and global change rating (GROC) were assessed. | Thoracic and scapula kinematics: no change in the two groups. Scapulo-thoracic excursion: no change in the two groups. Pain: similar improvements in both groups. Function: Similar improvements in both groups |
| Jing-Ian Yang et al., 2012 [10] | RCT | Patients with Frozen Shoulder N = 34 (2 did not complete treatment); Males = 12; Females = 22; Age (years); Criterion intervention group= average age 56.8; Criterion control group = average age 54.9; Control group = average age 54.3. | Intervention group with criterion n = 10; passive mobilizations, stretching in flexion and abduction of the shoulder, physical therapy, active exercises, end range mobilizations, and scapula mobilization; Control group of criterion n = 12 passive mobilizations, stretching in flexion and abduction of the shoulder, physical therapy, and active exercises; Control group n = 10 passive mobilizations, stretching in flexion and abduction of the shoulder, physical therapy, and active exercises; All patients were treated twice weekly for 8 weeks. | ROM: measurements made using a standard inclinometer; Disability: completion of a self-administered questionnaire specific to the shoulder, with a fixed index of items, called FLEX-SF. Kinematics of the shoulder: FASTAK motility analysis system. | Evaluations were made before treatment at 4 weeks, and finally, at 8 weeks. | ROM: From 4 and 8 weeks, the humeral external rotation and the ability to put the hand behind the back improved in the control group compared to that of the control group with criterion; at 4 weeks, the ability to put the hand behind the back improved in the intervention group with criterion compared to that of the control group; at 8 weeks, both the ability to put the hand behind the back and the external humeral rotation improved. There were no significant differences between the control group and the criterion and intervention groups. Disability: At 8 weeks, the questionnaire score was better in the control group than that in the criterion control group; at 8 weeks, the questionnaire score was better in the criterion intervention group than that in the criterion control group, while there were no significant differences between the control group and the criterion intervention group. Shoulder kinematics: From 4 and 8 weeks, the upward rotation of the scapula, the posterior tilt and the scapulohumeral rhythm improved in the control group compared to those of the criterion control group; at 8 weeks, the posterior scapula tilt and humeral scapular rhythm improved in the criterion intervention group compared to those of the criterion control group; there were no significant differences between the criterion intervention group and the control group. |
| Aydan Aytar et al., 2015 [13] | RCT | Patients with SIS N = 66; Males = 15; Females = 51; Age (years); Group treated with scapular mobilizations (GMS) = average age 52; Group treated with false scapular mobilizations (GFMS) = average age 52; Group treated with exercises (GE) = mean age 51. | GMT n = 22 treated with scapula mobilizations; GFMT n = 22 treated with false scapula mobilizations; GE n = 22 treated with muscle strengthening and stretching exercises. In all groups, before performing the listed interventions, patients were received warm compresses and TENS. Treatments were performed for 3 weeks, 3 times a week. After 3 weeks, all groups were instructed to perform GE exercises at home. | Primary Function: Quick DASH Questionnaire; Pain: VAS, evaluated at rest, during the night and during activity. Secondary ROM: measured the active ROM with a protractor; Satisfaction of the participants: Likert scale. | All assessments were made before the interventions, after two weeks, after three weeks, after seven weeks, and after eleven weeks. The satisfaction questionnaire was administered at the end of the three weeks of treatment. | Pain: there were similar improvements in all three groups. Function: similar improvement to the assessment after the third week, while in subsequent evaluations, it worsened in GMS and GFMS. ROM: similar improvements in all three groups. Participant satisfaction: was greater in GMS and GE. |
| Elif Turgut et al., 2017 [14] | RCT | Individuals with SIS and scapular dyskinesia participated in the study. N = 30; Males = 16; Females = 14; Age (years); Intervention group (GI): average age 33.4; Control group (GC): average age 39.5 | GC n = 15 patients treated with strengthening muscle exercises and stretching; GI n = 15 patients treated with scapular stabilization exercises, followed by shoulder strengthening and stretching exercises. The two intervention programs lasted 12 weeks, monitored weekly by physiotherapist. | Kinematics of the scapula and humerus: measured with an electromagnetic tracking instrument, with measurements made during the elevation and lowering of the arm on the sagittal plane; Function: Turkish version of the Shoulder Pain and Disability Index (SPADI); Pain: VAS, at rest, during the night and during activities. | Assessments were made before intervention, after the sixth week, and immediately after the end of treatments. | Kinematics of the scapula and humerus: increased external scapular rotation during the elevation and lowering of the arm in the GI; increased upward scapular rotation in the GI after 12 weeks; increased rear tilt in the GI; Function: improvements in questionnaire scores at the end of all interventions, but between the two groups there were no significant differences; Pain: decreased pain in the two groups, but without significant differences. |
| F. Struyf et al., 2012 [15] | RCT | Patients with impingement N = 22; Males = 10; Females = 12; Age (years); Experimental group = 46.2 average age; Control group = 45.4 average age. | Experimental group n = 10 manual mobilizations, stretching, and training on the motor control of the scapula. Control group n = 12. Exercises for strength in eccentric for the muscles of the rotator cuff, manual therapy with multidirectional gleno-humeral mobilizations and ultrasound. Patients in both groups were treated with 9 and 30 min therapy sessions at a frequency of 1–3 per week. | Primary Function: Shoulder Disability Questionnaire (SDQ). Secondary Pain: verbal numeric rating scale from 0 to 10 (VNRS) for impingement tests and VAS scale for pain at rest and during activity; Scapula measurements Visual observation of any winged scapula; Shoulder anteposition: distance between the posterior edge of the acromion and the table in supine patient; Length of the small pectoral muscle; upward rotation of the scapula: inclinometer; motor control of the scapula: kinetic test of internal rotation; isometric force of elevation: dynamometer in the position of the Jobe test. | Assessments were made before treatment, immediately after treatment, and three months after treatment. | Function: significant improvements in the experimental group compared to that of the control group, maintained even in the 3 month follow-up. Pain: reduction of pain in the experimental group at rest, during movement, and also during the Neer test. Scapula position: no change, not even in follow-up. |
| Gisele Harumi Hotta et al., 2020 [16] | RCT | Patients with subacromial pain N = 60; Males = 18; Females = 42; Age (years); Group with periscapular reinforcement (GRP) = average age 47; Scapular stabilization group (GSS)= average age 51. | GRP n = 30. They were treated with 6 progressive reinforcement exercises for the descending, middle, and ascending trapezius muscles and the anterior serratus muscle; all exercises were performed with progressive loads; GSS n = 30. Same exercises performed by the group as before with in addition six scapular stabilization exercises to emphasize retraction and scapular depression. Treatments in both groups were performed for 8 weeks 3 times a week on non-consecutive days. | Primary Function: shoulder pain and disability index (SPADI-Br) questionnaire. Secondary Pain: numeric pain rating scale (NPRS); perception of the effect of treatment: scale of the perceived overall effect; Satisfaction: MedRisk questionnaire; Chisesiophobia: Tampa scale; Force in isometry: hand dynamometer; ROM and scapula position; digital inclinometer. | Assessments were made: before intervention, at 4 weeks, at 8 weeks and 16 weeks. | This study showed that a protocol of progressive periscapular muscle strengthening exercises, with or without scapular stabilization exercises, improved all the parameters that were evaluated, but there were no differences in improvements between the two groups. The only thing that improved the most in the GSS was the upward scapula rotation at 90° of humeral elevation. |
| Jason K. Grimes et al., 2019 [17] | RCT E = 1 | Patients with sub-acromial pain N = 60; Males = 37; Females = 23; Age (years); Group treated with supine thrust (GTSU)= average age 37.6; Group treated with seated thrust (GTSE) = average age 35.6; Group treated with simulated thrust (GTF) = mean age 36.5. | GTSU n = 20 treated with a thrust for the upper portion of the thoracic spine in supine position; GTSE n = 20 treated with a thrust for the upper portion of the thoracic spine while seated; GTF n = 20 treated with a simulated thrust performed while seated. All types of interventions were performed twice. | Pain and function: Penn Shoulder Score (PSS) questionnaire; Evaluation of mobility: inclinometer to measure the various scapular movements both passively and actively, during the elevation of the arm on the scapular plane; the active elevation of the shoulder on the scapular plane was measured using a protractor; Length of the small pectoral muscle: measured with a tape taking reference points; Shoulder strength: measured with a hand dynamometer the strength of the middle trapezius muscle, ascending trapezius muscle, and anterior serratus muscle. | Evaluation of motility, pectoral muscle length, and shoulder strength were evaluated before treatment and immediately after treatment; PSS was administered before treatment and 48 h after treatment. | Pain and function: the PSS improved in all three groups, but between the groups, there were no major differences. Motility: there were no differences between the 3 groups, both for scapular and humeral movements. Length of the pectoral small muscle: there were no significant differences between the 3 groups. Shoulder strength: there were no statistically significant increases in strength after thoracic thrust; no significant differences in strength were observed between the 3 groups. |
| Mahsa Moslehi et al., 2020 [18] | RCT E = 2 | Patients with impingement N = 75; Males = 25; Females = 50; Age (years); Scapula-focused treatment group with feedback (GTSF) = 34.6–42 (38.3 average); Scapula-focused treatment group (GTS) = 33.4–45.5 (37.5 average); Control group = 36.1–40.3 (38.2 average). | GTS n = 25 training on shoulder positioning (first week), strengthening of the rotator cuff muscles (second, third, fifth, sixth, and seventh week), and exercises on flexibility (fourth and eighth weeks); GTSF n = 25 exercises focused on the scapula with tactile and verbal feedback; Control group n = 25 no intervention. The groups were treated for 8 weeks. | Primary Pain: VAS. Secondary Function: questionnaire Disability of the Arm, Shoulder and Hand (DASH); Scapular kinematics: infrared cameras. | Assessments were made before treatment and at the end of 8 weeks. | Pain: in both groups the VAS values improved, but the improvement was more significant in the GTSF. Function: in both groups it has improved, but the improvement is more significant in the GTSF. Scapular kinematics: after 8 weeks, the upward rotation of the scapula and the posterior tilt increased in GTSF, while there were no differences in the control group and in the GTS. |
| Melina N.Haik et al., 2014 [19] | RCT E = 4 | Patients with impingement (PI) and patients without impingement (PSI) N = 97; Age (years); Impingement patients treated with thrust (PIT)= 33.8 average age; Patients with impingement treated with simulated thrusts (PIFT) = 29.7 average age; Patients without impingement treated with a thrust (PSIT) = 25.5 average age; Patients without impingement treated with simulated thrusts (PSIFT) = 26.1 average age. | PI n = 50; PSI n = 47: these two groups of patients were each divided into two groups. PIT n = 25 treated with thrust aimed to the intermediate thoracic tract; PIFT (with SIS) n = 25 treated with a simulated thrust; PSIT (without SIS) n = 24 treated with thrust aimed to the intermediate thoracic tract; PSIFT n = 23 treated with a simulated thrust. | Primary Pain: Western Ontario Rotator cuff index (WORC) and NPRS questionnaire to assess pain during arm elevation and lowering; Function: DASH questionnaire; Scapular kinematics: evaluated using an electromagnetic tracking system during an elevation of the arm on the sagittal plane (Flock of Birds hardware). Secondary Effects on scapular kinematics in groups formed by individuals without impingement. | Assessments were made before intervention and immediately after intervention. | Pain: Improved after thrust in both PIT and PIFT, but the biggest increase was in PIT. Scapular kinematics in the 2 groups of patients with impingement: a few changes were observed, e.g., there was an increase in the degree of the upward rotation of the scapula during arm elevation in the PIT and a slight increase in the degree of internal rotation in the PIT and PIFT. Scapular kinematics in the two groups of patients without impingement: increase in the degree of the upward rotation of the scapula during arm elevation in both groups, more significant in PSIT; a slight increase in the degree of anterior tilt was also observed during arm elevation in the PSIT. |
| Melina N. Haik et al., 2017 [20] | RCT | The study involved people diagnosed with SIS N = 61; Males = 38; Females = 23; Age (years); Group treated with thoracic manipulation (GMT) = 32.5 average age; Group treated with false thoracic manipulation (GFMT) = 31.3 average age. | GMT n = 30: thoracic thrust to seated patient; GFMT n = 31: similar technique was used, but with thrust applied in different patient position. All operations were performed twice after 3–4 days. | Pain: NPRS and administration of the WORC questionnaire; Function: administration of the DASH questionnaire; Scapular kinematics: measured by a computerized system during the complete elevation and lowering of the limb on the sagittal plane. Muscle activation: measured the activity of the ascending, middle and descending trapezius muscle and the anterior serratus muscle with electromyography. | Evaluations were made before the first intervention, before the second intervention, immediately after the second intervention, and then, 3–4 days after the second intervention. | Pain: a decrease in pain was observed in GMT before the second intervention and immediately after the second intervention; there were minimal improvements in the WORC and no difference between the two groups. Function: minimal improvements and no difference between the two groups; Scapular kinematics: in the GMT after the two interventions, there was an increase in the degrees of upward rotation and scapular tilt, while in the GFMT, the anterior scapular tilt increased after the second intervention; 3–4 days after the interventions, the difference between the two groups in the upward scapular rotation was maintained, even if it was minimal. Muscle activation: activation of the descending trapezius after intervention increased in GFMT, while activity of the middle and ascending trapezius and anterior serratus decreased in both groups. |
| Nilay Comuk Balci et al., 2016 [21] | RCT | The study involved patients with unilateral frozen shoulder N = 53; Males = 13; Females = 40; Age (years); PNF treatment group (GPNF) = 56.7 average age; Group treated with classical exercises (GEC) = average age 58.1; Control group (GC) = 58.6 average age | GC n = 17 patients were treated with warm compresses, TENS and ultrasound; GEC n = 18 group treated with the same interventions done in the GC plus stretching exercises such as Codman’s movements, and reinforcement exercises that include scapular elevation and scapular stabilization exercises; GPNF n = 18 patients were treated in the same way as GC, with additional scapular PNF techniques. The intervention lasted an hour. | Pain: VAS; Scapular dyskinesia: lateral scapular slide test; Active ROM: protractor to measure abduction and flexion in supine position; Function: Simple Shoulder test (SST), which is a questionnaire. | Assessments were made before the various interventions and immediately after the end of each treatment. | Pain: pain improved the most in GC and GPNF; Scapular dyskinesia: no improvements were found; Active ROM and Function: there were improvements in all three groups, without there being any significant differences between the groups. |
| Paula R. Camargo et al., 2015 [22] | RCT E = 1b | Patients with impingement N = 46; Males = 24; Females = 22; Age (years); Manual therapy intervention group (GITM): 35.96 average age; Intervention group (GI): 32.65 average age. | GI n = 233 strength exercises and 3 stretching exercises; GITM n = 23 same exercises performed by the GI with an additional 45 min of manual therapy. All patients were treated for 4 weeks. | Scapular kinematics: measurement made through a machine (Flock of Birds hardware) during the elevation of the arm on the scapular and sagittal plane; Function: Brazilian version of the DASH questionnaire; Pain: VAS scale; Mechanical sensitivity: threshold pressure point (point where pressure turns into pain). | The evaluations were made one week before the intervention, and at the end of the 4 weeks of intervention. | Scapular kinematics: there were no clinically relevant changes in any group. A noticeable increase in the degree of anterior tilt was observed after GITM intervention. Function: both groups had improvements in the questionnaire score, which were more relevant in the GITM. Pain: after the interventions, it improved in both groups, although the most significant improvement occurred in the GITM. Mechanical sensitivity: mechanical sensitivity in the shoulder region is improved in both groups after interventions. |
| S. Arul Pragassame et al., 2019 [23] | RCT | The study involved patients with unilateral frozen shoulder N = 30; Males = 19; Females = 11; Age (years); Group treated with scapula mobilizations (GMS): average age 51.73; Group treated with conventional therapy (GTC) = average age 51.40 | GTC n = 15: this group was treated with paraffin wax before each surgery, capsular stretching, and home exercises; GMS n = 15: this group was treated the same as the GTC group with the addition of scapular mobilizations. The total duration of both treatments was 10 days, one session per day. | Primary Pain: NPRS ROM: measured the active abduction and external rotation on the scapula plane with a protractor; Secondary Function: shoulder constant score, (a questionnaire to evaluate shoulder function). | Assessments were made before treatment and immediately after the 10 days of treatment. | Pain: pain improved significantly in both groups, but the improvement was most significant in GMS; ROM: both abduction and external roation improved in both groups, but more so in GMS; Function: improved in both groups but more in GMS. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferlito, R.; Testa, G.; McCracken, K.L.; Moscato, S.; Zerbito, G.M.; Panvini, F.M.C.; Blatti, C.; Pavone, V.; Sapienza, M. Effectiveness of Therapeutical Interventions on the Scapulothoracic Complex in the Management of Patients with Subacromial Impingement and Frozen Shoulder: A Systematic Review. J. Funct. Morphol. Kinesiol. 2023, 8, 38. https://doi.org/10.3390/jfmk8020038
Ferlito R, Testa G, McCracken KL, Moscato S, Zerbito GM, Panvini FMC, Blatti C, Pavone V, Sapienza M. Effectiveness of Therapeutical Interventions on the Scapulothoracic Complex in the Management of Patients with Subacromial Impingement and Frozen Shoulder: A Systematic Review. Journal of Functional Morphology and Kinesiology. 2023; 8(2):38. https://doi.org/10.3390/jfmk8020038
Chicago/Turabian StyleFerlito, Rosario, Gianluca Testa, Kathryn Louise McCracken, Salvatore Moscato, Giovanni Maria Zerbito, Flora Maria Chiara Panvini, Chiara Blatti, Vito Pavone, and Marco Sapienza. 2023. "Effectiveness of Therapeutical Interventions on the Scapulothoracic Complex in the Management of Patients with Subacromial Impingement and Frozen Shoulder: A Systematic Review" Journal of Functional Morphology and Kinesiology 8, no. 2: 38. https://doi.org/10.3390/jfmk8020038
APA StyleFerlito, R., Testa, G., McCracken, K. L., Moscato, S., Zerbito, G. M., Panvini, F. M. C., Blatti, C., Pavone, V., & Sapienza, M. (2023). Effectiveness of Therapeutical Interventions on the Scapulothoracic Complex in the Management of Patients with Subacromial Impingement and Frozen Shoulder: A Systematic Review. Journal of Functional Morphology and Kinesiology, 8(2), 38. https://doi.org/10.3390/jfmk8020038








