Antibiotic-Coated Nail in Open Tibial Fracture: A Retrospective Case Series
Abstract
:1. Introduction
- (a)
- bacteria can colonize the implant surface forming biofilm (glycocalyx) that protects them from the action of systemic antibiotic
- (b)
- vascular damage does not allow systemic antibiotics to reach high local concentrations.
2. Materials and Methods
2.1. Setting
2.2. Surgical Technique and Post-Operative Treatment
2.3. Outcome Measurements
2.4. Statistical Analysis
3. Results
3.1. Patients and Demographic Data
3.2. Surgical Data
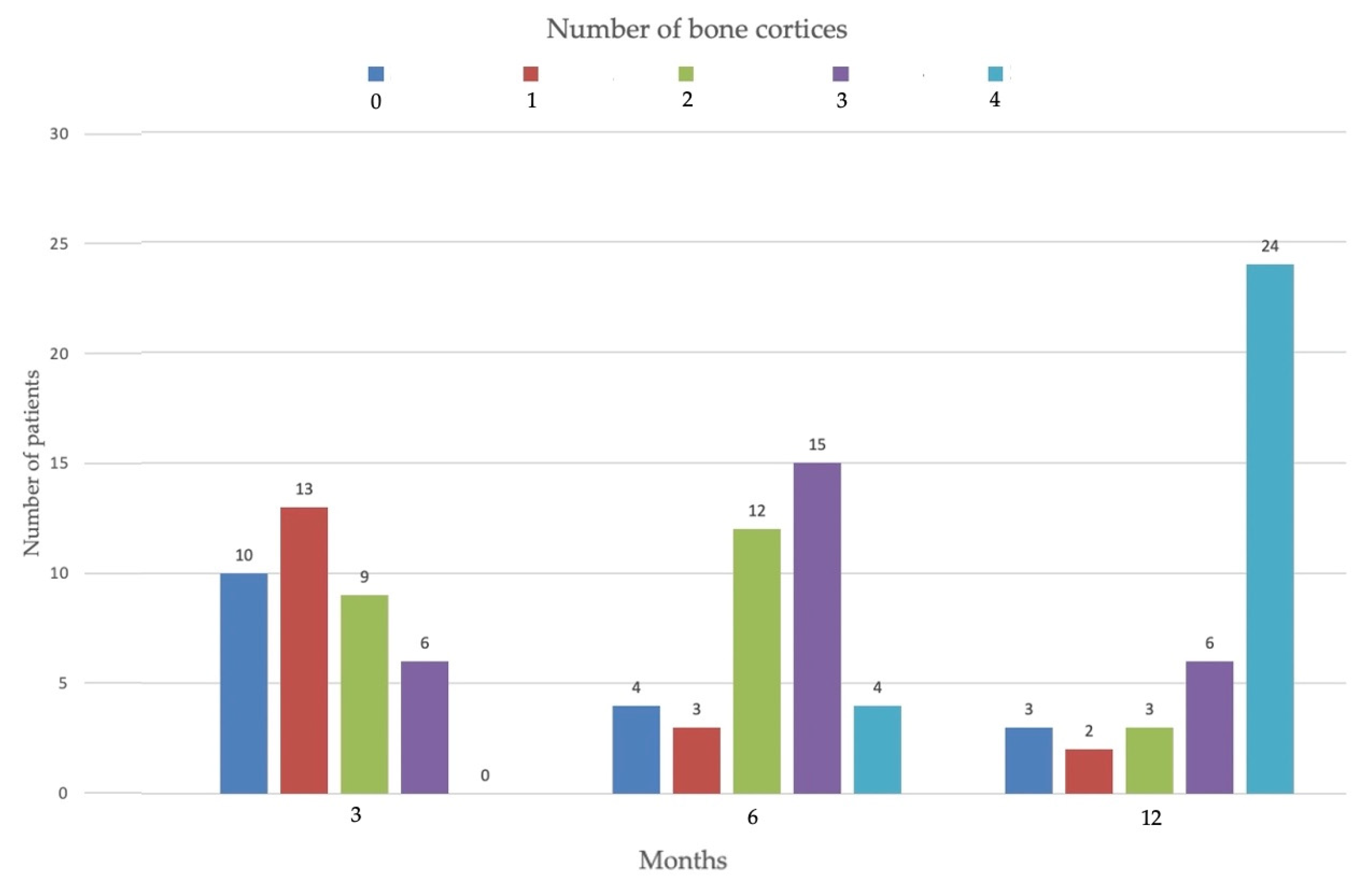
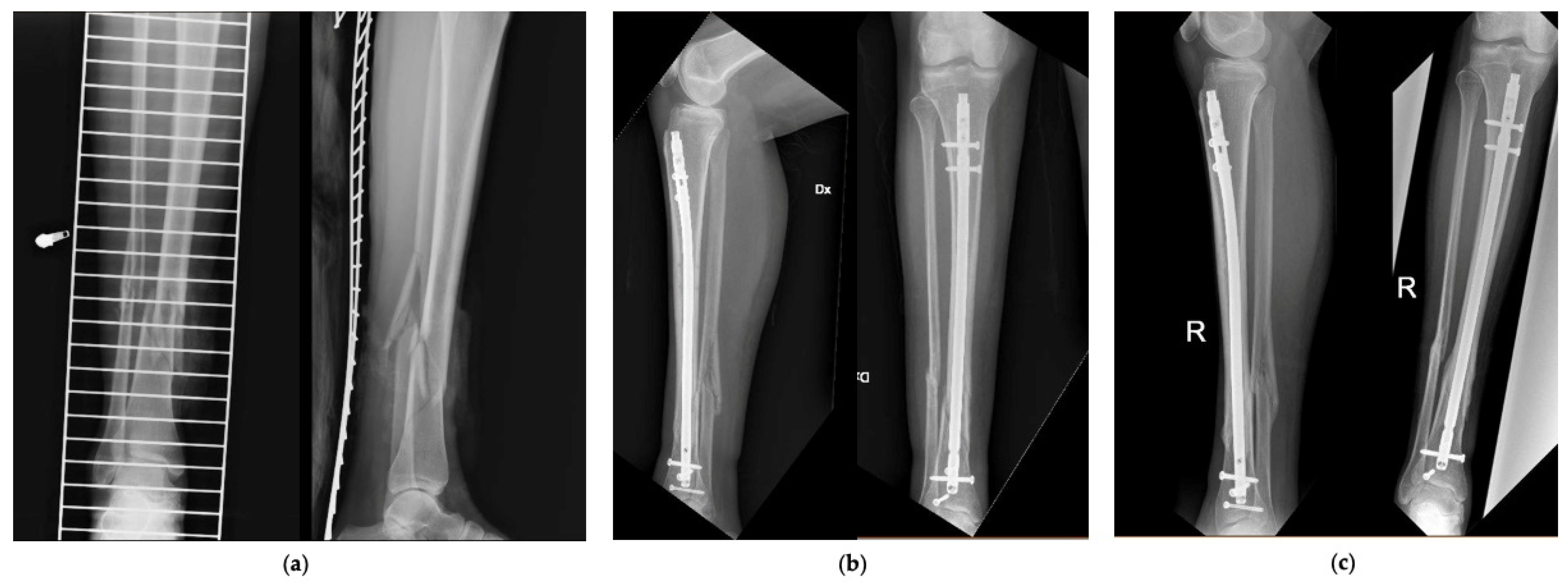
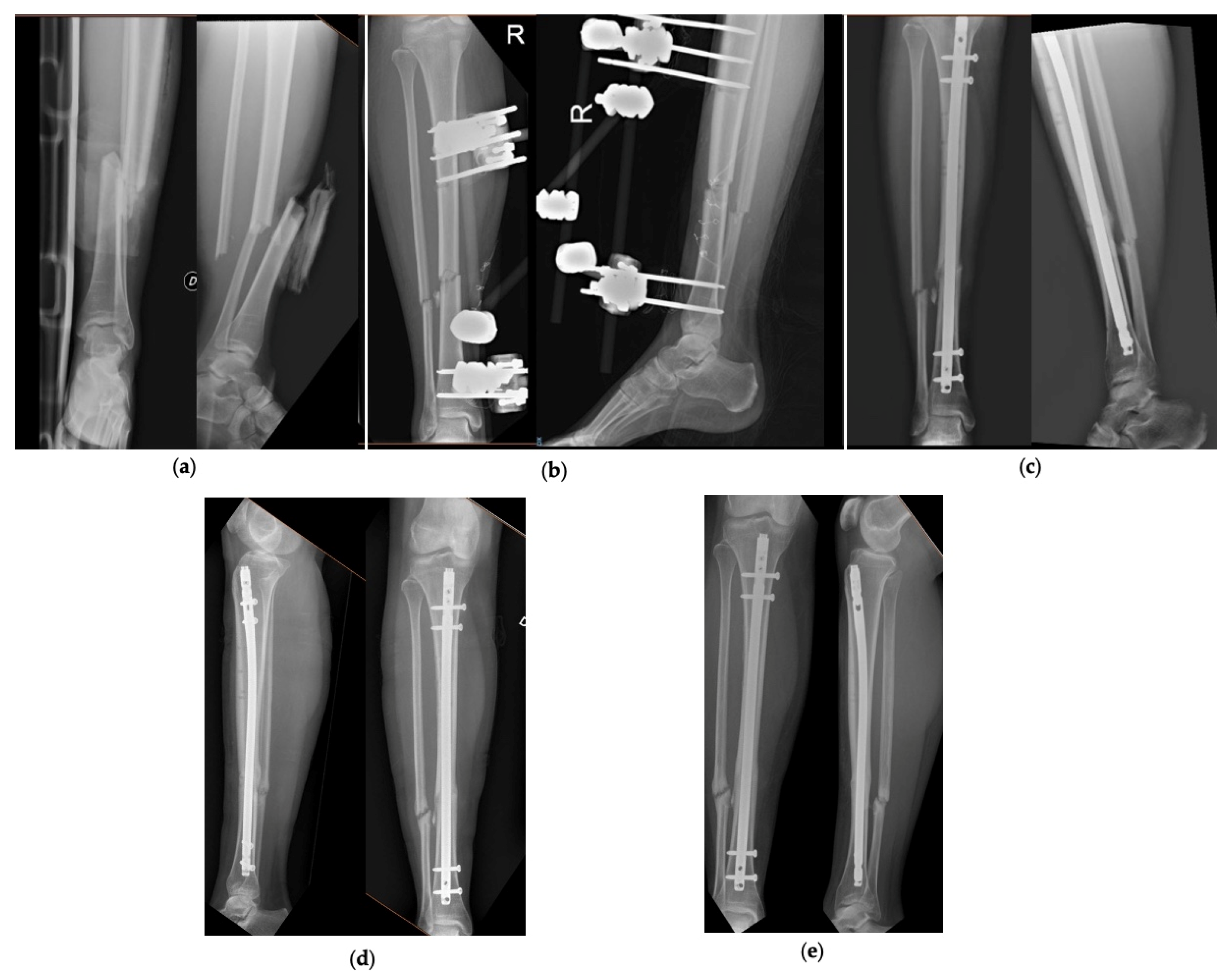
3.3. Radiographic and Clinical Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Periti, P.; Stringa, G.; Mini, E. Comparative multicenter trial of teicoplanin versus cefazolin for antimicrobial prophylaxis in prosthetic joint implant surgery. Italian Study Group for Antimicrobial Prophylaxis in Orthopedic Surgery. Eur. J. Clin. Microbiol. Infect. Dis. 1999, 18, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Diefenbeck, M.; Mückley, T.; Hofmann, G.O. Prophylaxis and treatment of implant-related infections by local application of antibiotics. Injury 2006, 37 (Suppl. S2), S95–S104. [Google Scholar] [CrossRef] [PubMed]
- Ostermann, P.A.; Henry, S.L.; Seligson, D. Timing of wound closure in severe compound fractures. Orthopedics 1994, 17, 397–399. [Google Scholar] [CrossRef]
- Craig, J.; Fuchs, T.; Jenks, M.; Fleetwood, K.; Franz, D.; Iff, J.; Raschke, M. Systematic review and meta-analysis of the additional benefit of local prophylactic antibiotic therapy for infection rates in open tibia fractures treated with intramedullary nailing. Int. Orthop. 2014, 38, 1025–1030. [Google Scholar] [CrossRef] [Green Version]
- Gustilo, R.B.; Anderson, J.T. JSBS classics. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones. Retrospective and prospective analyses. J. Bone Jt. Surg. Am. 2002, 84, 682. [Google Scholar] [CrossRef]
- Cianni, L.; Bocchi, M.B.; Vitiello, R.; Greco, T.; De Marco, D.; Masci, G.; Maccauro, G.; Pitocco, D.; Perisano, C. Arthrodesis in the Charcot foot: A systematic review. Orthop. Rev. 2020, 12, 8670. [Google Scholar] [CrossRef] [PubMed]
- Greco, T.; Polichetti, C.; Cannella, A. Ankle hemophilic arthropathy: Literature review. Am. J. Blood Res. 2021, 11, 206. [Google Scholar]
- Metsemakers, W.J.; Reul, M.; Nijs, S. The use of gentamicin-coated nails in complex open tibia fracture and revision cases: A retrospective analysis of a single centre case series and review of the literature. Injury 2015, 46, 2433–2437. [Google Scholar] [CrossRef]
- Greco, T.; Cianni, L.; Polichetti, C.; Inverso, M.; Maccauro, G.; Perisano, C. Uncoated vs. Antibiotic-Coated Tibia Nail in Open Diaphyseal Tibial Fracture (42 according to AO Classification): A Single Center Experience. BioMed Res. Int. 2021, 2021, 7421582. [Google Scholar] [CrossRef]
- Lillo, M.; Ezzo, O.E.; Cauteruccio, M.; Ziranu, A.; Santis, V.D.; Maccauro, G. Infections in primary intramedullary nailing of open tibial fractures: A review article. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 195–200. [Google Scholar]
- Gosselin, R.A.; Roberts, I.; Gillespie, W.J. Antibiotics for preventing infection in open limb fractures. Cochrane Database Syst. Rev. 2004, CD003764. [Google Scholar] [CrossRef]
- Nizegorodcew, T.; Palmieri, G.; Marzetti, E. Antibiotic-Coated Nails in Orthopedic and Trauma Surgery: State of the Art. Int. J. Immunopathol. Pharmacol. 2011, 24, 125–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McKee, M.D.; Li-Bland, E.A.; Wild, L.M.; Schemitsch, E.H. A prospective, randomized clinical trial comparing an antibiotic-impregnated bioabsorbable bone substitute with standard antibiotic-impregnated cement beads in the treatment of chronic osteomyelitis and infected nonunion. J. Orthop. Trauma 2010, 24, 483–490. [Google Scholar] [CrossRef]
- Schmidmaier, G.; Lucke, M.; Wildemann, B.; Haas, N.P.; Raschke, M. Prophylaxis and treatment of implant-related infections by antibiotic-coated implants: A review. Injury 2006, 37 (Suppl. S2), S105–S112. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, T.; Schmidmaier, G.; Raschke, M.J.; Stange, R. Bioactive-Coated Implants in Trauma Surgery. Eur. J. Trauma Emerg. Surg. 2008, 34, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Schmidmaier, G.; Wildemann, B.; Stemberger, A.; Haas, N.P.; Raschke, M. Biodegradable poly(D,L-lactide) coating of implants for continuous release of growth factors. J. Biomed. Mater. Res. 2001, 58, 449–455. [Google Scholar] [CrossRef]
- Govoni, M.; Lamparelli, E.P.; Ciardulli, M.C.; Santoro, A.; Oliviero, A.; Palazzo, I.; Reverchon, E.; Vivarelli, L.; Maso, A.; Storni, E.; et al. Demineralized bone matrix paste formulated with biomimetic PLGA microcarriers for the vancomycin hydrochloride controlled delivery: Release profile, citotoxicity and efficacy against S. aureus. Int. J. Pharm. 2020, 582, 119322. [Google Scholar] [CrossRef]
- Winkler, H.; Kaudela, K.; Stoiber, A.; Menschik, F. Bone grafts impregnated with antibiotics as a tool for treating infected implants in orthopedic surgery—One stage revision results. Cell Tissue Bank 2006, 7, 319–323. [Google Scholar] [CrossRef]
- Peeters, A.; Putzeys, G.; Thorrez, L. Current Insights in the Application of Bone Grafts for Local Antibiotic Delivery in Bone Reconstruction Surgery. J. Bone Jt. Infect. 2019, 4, 245–253. [Google Scholar] [CrossRef]
- Walter, N.; Popp, D.; Freigang, V.; Nerlich, M.; Alt, V.; Rupp, M. Treatment of severely open tibial fractures, non-unions, and fracture-related infections with a gentamicin-coated tibial nail—Clinical outcomes including quality of life analysis and psychological ICD-10-based symptom rating. J. Orthop. Surg. Res. 2021, 16, 270. [Google Scholar] [CrossRef]
- Franz, D.; Raschke, M.; Giannoudis, P.V.; Leliveld, M.; Metsemakers, W.J.; Verhofstad, M.H.J.; Craig, J.A.; Shore, J.; Smith, A.; Muehlendyck, C.; et al. Use of antibiotic coated intramedullary nails in open tibia fractures: A European medical resource use and cost-effectiveness analysis. Injury 2021, 52, 1951–1958. [Google Scholar] [CrossRef]
- Expert Tibial Nail (ETN)|With PROtect. Available online: https://www.jnjmedicaldevices.com/de-DE/product/expert-tibial-nail-etn (accessed on 25 November 2021).
- Muller, M.E.; Nazarian, S.; Koch, P.; Schatzker, J. The AO Classification of Fractures of Long Bones; Springer: Berlin/Heidelberg, Germany, 1990. [Google Scholar]
- Johnson, E.E.; Urist, M.R.; Finerman, G.A. Repair of segmental defects of the tibia with cancellous bone grafts augmented with human bone morphogenetic protein. A preliminary report. Clin. Orthop. Relat. Res. 1988, 236, 249–257. [Google Scholar] [CrossRef]
- Horan, T.C.; Andrus, M.; Dudeck, M.A. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am. J. Infect. Control 2008, 36, 309–332. [Google Scholar] [CrossRef]
- Holcomb, T.M.; Temple, E.W.; Barp, E.A.; Smith, H.L. Surgical Correction of Checkrein Deformity after Malunited Distal Tibia Fracture: A Case Report. J. Foot Ankle Surg. 2014, 53, 631–634. [Google Scholar] [CrossRef]
- Careri, S.; Vitiello, R.; Oliva, M.S.; Ziranu, A.; Maccauro, G.; Perisano, C. Masquelet technique and osteomyelitis: Innovations and literature review. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Greco, T.; Vitiello, R.; Cazzato, G.; Cianni, L.; Malerba, G.; Maccauro, G.; Perisano, C. Intramedullary antibiotic coated nail in tibial fracture: A systematic review. J. Biol. Regul. Homeost. Agents 2020, 34, 63–69. [Google Scholar] [PubMed]
- Basilico, M.; Vitiello, R.; Oliva, M.S.; Covino, M.; Greco, T.; Cianni, L.; Dughiero, G.; Ziranu, A.; Perisano, C.; Maccauro, G. Predictable risk factors for infections in proximal femur fractures. J. Biol. Regul. Homeost. Agents 2020, 34, 77–81. [Google Scholar] [PubMed]
- Wasko, M.K.; Borens, O. Antibiotic cement nail for the treatment of posttraumatic intramedullary infections of the tibia: Midterm results in 10 cases. Injury 2013, 44, 1057–1060. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Open tibial fractures treated with antibiotic-coated nail | Open tibial fractures not treated with antibiotic-coated nail |
| At least 18 months follow-up | Less than 18 months follow-up |
| Informed consent to treatment | Pre-trauma gait deficit |
| Neurological pathologies |
| ETN PROtectTM (38 Patients) | |
|---|---|
| Age (Mean ± DS, range) | 44.7 ± 16.6 (18–78) |
| Gender | |
| Male | 29 |
| Female | 9 |
| Voluptuous habits | |
| Smokers | 9 |
| Drug addicts | 3 |
| ETN ProtectTM indication | |
| Acute fracture | 34 |
| Revision surgery | 4 |
| AO Classification | |
| 42A | 12 |
| 42B | 17 |
| 42C | 7 |
| 43A | 1 |
| Gustilo-Anderson Classification | |
| I | 6 |
| II | 15 |
| III | 17 (8 IIIA; 5 IIIB; 4 IIIC) |
| Polytrauma | |
| Yes | 28 |
| No | 10 |
| Fractured Fibula | 35 |
| EF/TT/VAC Therapy | 31 EF; 1 TT; 8 VAC |
| Plastic Surgery | 9 |
| Skin grafts | 5 |
| Sural flaps | 4 |
| TTN days (Mean ± DS, range) | 16.5 ± 15.3 (2–54) |
| Hospital Stay days (Mean ± DS, range) | 28.2 ± 26.9 (4–128) |
| Bone union | 34 |
| Within 12 months | 29 |
| After 12 months | 5 |
| Non-union | 4 |
| Total complications | 13 |
| Delay consolidation | 5 |
| Non-union | 4 (2 infected non-union) |
| Surgical site infection | 4 |
| Other treatment | 12 |
| Nail Dynamization | 5 |
| Wound debridement + targeted antibiotic therapy | 3 |
| Revision osteosynthesis | 3 |
| Nail removal and TAT | 1 |
| Follow-up months (Mean ± DS, range) | 24.1 ± 6.1 (18–43) |
| N° | Age | Sex | AO Tibia | Ga | Fractured Fibula | AO Fibula | Polytrauma | Voluptuous Habits | EF/TT/VAC Therapy |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 20 | M | 42B3 | 2 | Yes | 4F2B | Yes | Smoking, DA | EF |
| 2 | 53 | M | 42C3 | 2 | Yes | 4F2B | Yes | - | EF |
| 3 | 24 | M | 42B3 | 1 | - | - | Yes | Smoking | - |
| 4 | 67 | F | 42B3 | 3A | Yes | 4F2B | - | - | EF |
| 5 | 68 | F | 42B2 | 3A | Yes | 4F3A | - | - | EF, VAC |
| 6 | 63 | M | 42B2 | 2 | Yes | 4F3B | Yes | - | - |
| 7 | 75 | M | 42A1 | 3B | Yes | 4F2B | Yes | - | EF |
| 8 * | 63 | M | 42A2 | 3A | Yes | 4F2A | Yes | - | EF |
| 9 | 29 | M | 42B3 | 3A | Yes | 4F2B | Yes | - | EF, VAC |
| 10 | 30 | M | 42C3 | 2 | Yes | 4F2B | Yes | - | EF |
| 11 | 46 | F | 42A1 | 1 | - | - | - | - | - |
| 12 | 52 | F | 42B3 | 2 | Yes | 4F24 | - | Smoking | EF |
| 13 | 43 | M | 42A2 | 2 | Yes | 4F2B | Yes | - | EF |
| 14 | 30 | M | 42B2 | 2 | Yes | 4F2B | Yes | - | VAC |
| 15 | 57 | M | 42A2 | 3A | Yes | 4F2B | Yes | - | EF, VAC |
| 16 | 22 | M | 42A3 | 3C | Yes | 4F2B | Yes | Smoking | EF |
| 17 | 62 | M | 42C3 | 2 | Yes | 4F2B | Yes | - | EF |
| 18 | 50 | M | 42A1 | 3C | Yes | 4F2A | Yes | - | EF, VAC |
| 19 | 45 | F | 42A2 | 3B | Yes | 4F2A | - | - | EF, VAC |
| 20 | 65 | F | 42A2 | 1 | Yes | 4F2A | - | - | - |
| 21 | 47 | M | 42C3 | 3A | Yes | 4F3B | Yes | Smoking | EF, VAC |
| 22 | 57 | M | 42B2 | 2 | Yes | 4F2B | Yes | - | EF |
| 23 * | 46 | M | 42B2 | 3B | Yes | 4F2A | Yes | - | EF |
| 24 | 26 | F | 42B3 | 3B | Yes | 4F2A | - | - | EF |
| 25 | 28 | M | 42B3 | 3A | Yes | 4F2B | Yes | - | EF |
| 26 | 31 | M | 42C3 | 3A | Yes | 4F2A | Yes | - | EF |
| 27 | 49 | F | 42B3 | 2 | Yes | 4F2B | - | - | EF |
| 28 | 18 | M | 42B3 | 2 | - | - | Yes | - | - |
| 29 | 25 | M | 42B3 | 1 | Yes | 4F2B | Yes | - | EF |
| 30 | 53 | M | 42C2 | 1 | Yes | 4F2B | Yes | Smoking, DA | EF |
| 31 | 36 | F | 42C3 | 3C | Yes | 4F2B | - | - | EF, VAC |
| 32 * | 40 | M | 42B3 | 3B | Yes | 4F2A | Yes | - | EF, VAC |
| 33 * | 52 | M | 43A3 | 3C | Yes | 4F3B | Yes | Smoking | EF |
| 34 | 42 | M | 42A2 | 2 | Yes | 4F2A | Yes | Smoking | EF |
| 35 | 78 | M | 42A1 | 2 | Yes | 4F2A | Yes | - | EF |
| 36 | 22 | M | 42A3 | 1 | Yes | 4F2B | Yes | - | TT |
| 37 | 58 | M | 42A3 | 2 | Yes | 4F2B | Yes | - | EF |
| 38 | 28 | M | 42B3 | 2 | Yes | 4F1A | Yes | Smoking, DA | EF |
| N° | TTN (days) | Nail Length × Diameter (mm) | HS | Bone Union (Number of Cortices at 3–6–12 Months) | Complications | Other Treatments | Follow-Up (Months) |
|---|---|---|---|---|---|---|---|
| 1 | 27 | 360 × 11 | 34 | Yes # (0-2-2) | Consolidation delay | Dynamization | 18 |
| 2 | 6 | 375 × 12 | 9 | Yes (1-3-3) | - | - | 25 |
| 3 | 8 | 345 × 10 | 12 | Yes (3-3-3) | - | - | 18 |
| 4 | 7 | 330 × 10 | 12 | Yes (3-4-4) | - | - | 19 |
| 5 | 54 | 315 × 11 | 91 | Yes (2-2-3) | - | - | 18 |
| 6 | 2 | 375 × 11 | 10 | Yes (2-3-3) | - | - | 26 |
| 7 | 10 | 315 × 10 | 26 | Yes (2-3-4) | - | - | 21 |
| 8* | 104 | 330 × 11 | 55 | Yes # (1-2-2) | Consolidation delay | Dynamization + check-rein deformity correction | 24 |
| 9 | 52 | 345 × 11 | 128 | Yes (2-3-4) | - | 22 | |
| 10 | 6 | 340 × 9 | 12 | No (0-0-0) | Non-union, coronal malalignment | Revision osteosynthesis (plate and screws) | 43 |
| 11 | 12 | 285 × 9 | 59 | Yes (3-3-4) | - | - | 27 |
| 12 | 11 | 330 × 11 | 12 | Yes (1-3-4) | - | - | 25 |
| 13 | 20 | 375 × 12 | 26 | Yes (2-2-4) | - | - | 26 |
| 14 | 9 | 315 × 10 | 11 | Yes (1-3-4) | - | - | 26 |
| 15 | 9 | 360 × 10 | 54 | Yes (1-2-4) | - | - | 28 |
| 16 | 16 | 345 × 10 | 31 | No (0-0-0) | Infected non-union | Nail removal, fistulectomy, debridement, curettage, Masquelet | 29 |
| 17 | 9 | 330 × 9 | 12 | Yes (0-1-4) | Superficial surgical site infection | Wound debridement + targeted antibiotic therapy | 29 |
| 18 | 48 | 340 × 11 | 77 | Yes (0-2-4) | - | - | 34 |
| 19 | 47 | 285 × 9 | 56 | Yes # (0-0-1) | Consolidation delay | Dynamization | 34 |
| 20 | 2 | 315 × 10 | 7 | Yes (1-3-4) | - | - | 36 |
| 21 | 48 | 375 × 10 | 57 | Yes (0-2-4) | - | - | 36 |
| 22 | 9 | 375 × 10 | 12 | Yes # (1-2-2) | Consolidation delay | Dynamization | 18 |
| 23* | 331 | 360 × 11 | 13 | Yes (1-2-4) | Superficial surgical site infection | Wound debridement + targeted antibiotic therapy | 18 |
| 24 | 8 | 315 × 9 | 14 | Yes (2-3-4) | Superficial surgical site infection | Wound debridement + targeted antibiotic therapy | 18 |
| 25 | 7 | 345 × 10 | 7 | Yes (3-3-4) | - | - | 18 |
| 26 | 13 | 345 × 11 | 17 | No (0-0-0) | Infected non-union malalignment | Nail removal, Masquelet | 18 |
| 27 | 10 | 345 × 10 | 12 | Yes (3-4-4) | - | - | 19 |
| 28 | 5 | 375 × 10 | 6 | Yes (0-2-3) | - | - | 19 |
| 29 | 23 | 360 × 10 | 26 | Yes # (1-1-2) | Consolidation delay | Dynamization | 20 |
| 30 | 9 | 360 × 9 | 15 | No (0-1-1) | Non-union | Patient refused further treatment | 22 |
| 31 | 10 | 340 × 10 | 15 | Yes (2-4-4) | - | - | 24 |
| 32* | 41 | 375 × 12 | 42 | Yes (2-3-3) | - | - | 24 |
| 33* | 375 | 315 × 10 | 4 | Yes (1-2-4) | - | - | 24 |
| 34 | 8 | 330 × 10 | 10 | Yes (3-3-4) | Superficial surgical site infection | Nail removal, wound debridement, and targeted antibiotic therapy | 25 |
| 35 | 2 | 315 × 11 | 27 | Yes (2-2-4) | - | - | 20 |
| 36 | 22 | 360 × 10 | 20 | Yes (1-3-4) | - | - | 21 |
| 37 | 24 | 375 × 13 | 31 | Yes (1-3-4) | - | - | 19 |
| 38 | 10 | 345 × 8 | 13 | Yes (1-3-4) | - | - | 25 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perisano, C.; Greco, T.; Polichetti, C.; Inverso, M.; Maccauro, G. Antibiotic-Coated Nail in Open Tibial Fracture: A Retrospective Case Series. J. Funct. Morphol. Kinesiol. 2021, 6, 97. https://doi.org/10.3390/jfmk6040097
Perisano C, Greco T, Polichetti C, Inverso M, Maccauro G. Antibiotic-Coated Nail in Open Tibial Fracture: A Retrospective Case Series. Journal of Functional Morphology and Kinesiology. 2021; 6(4):97. https://doi.org/10.3390/jfmk6040097
Chicago/Turabian StylePerisano, Carlo, Tommaso Greco, Chiara Polichetti, Michele Inverso, and Giulio Maccauro. 2021. "Antibiotic-Coated Nail in Open Tibial Fracture: A Retrospective Case Series" Journal of Functional Morphology and Kinesiology 6, no. 4: 97. https://doi.org/10.3390/jfmk6040097
APA StylePerisano, C., Greco, T., Polichetti, C., Inverso, M., & Maccauro, G. (2021). Antibiotic-Coated Nail in Open Tibial Fracture: A Retrospective Case Series. Journal of Functional Morphology and Kinesiology, 6(4), 97. https://doi.org/10.3390/jfmk6040097








