Analysis of Dental Malocclusion and Neuromotor Control in Young Healthy Subjects through New Evaluation Tools
Abstract
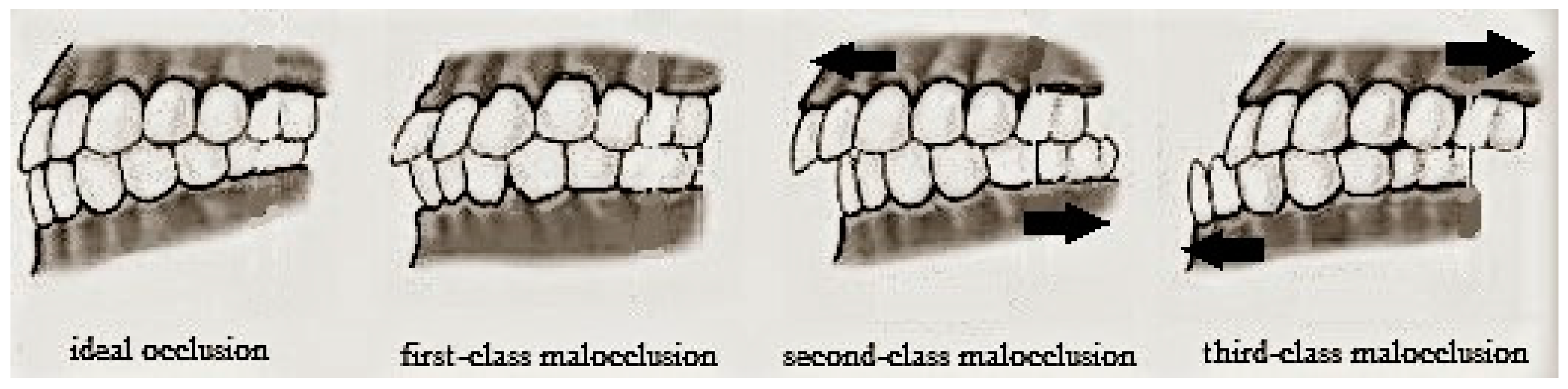
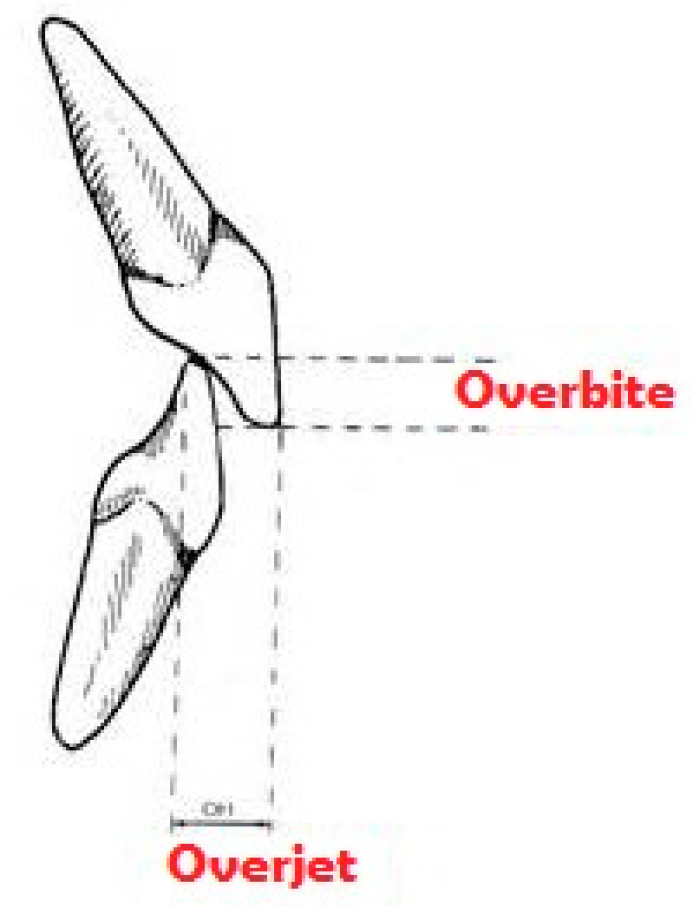
:1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Subject Examination
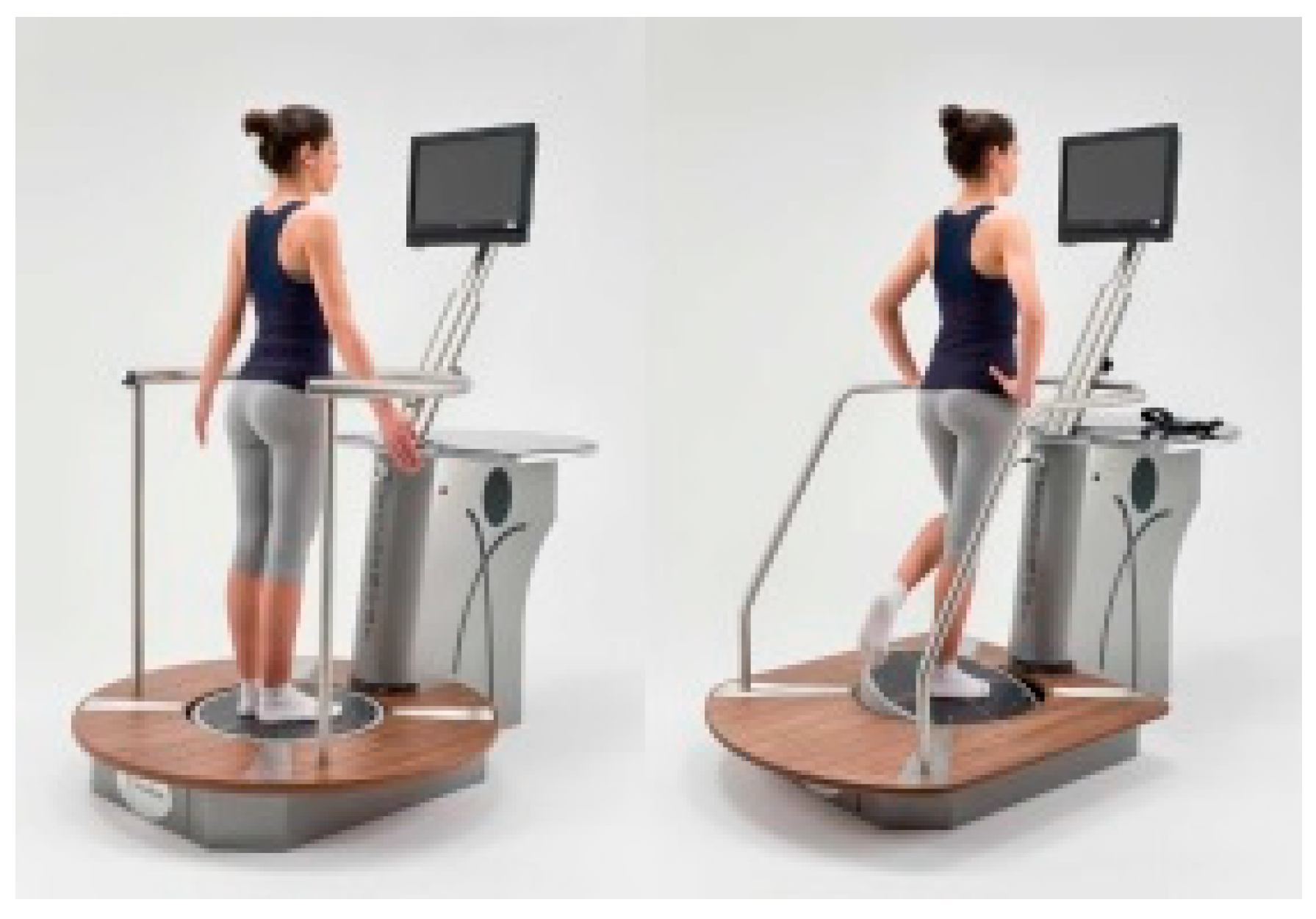
2.3. Instrumental Assessment of Neuromotor Control
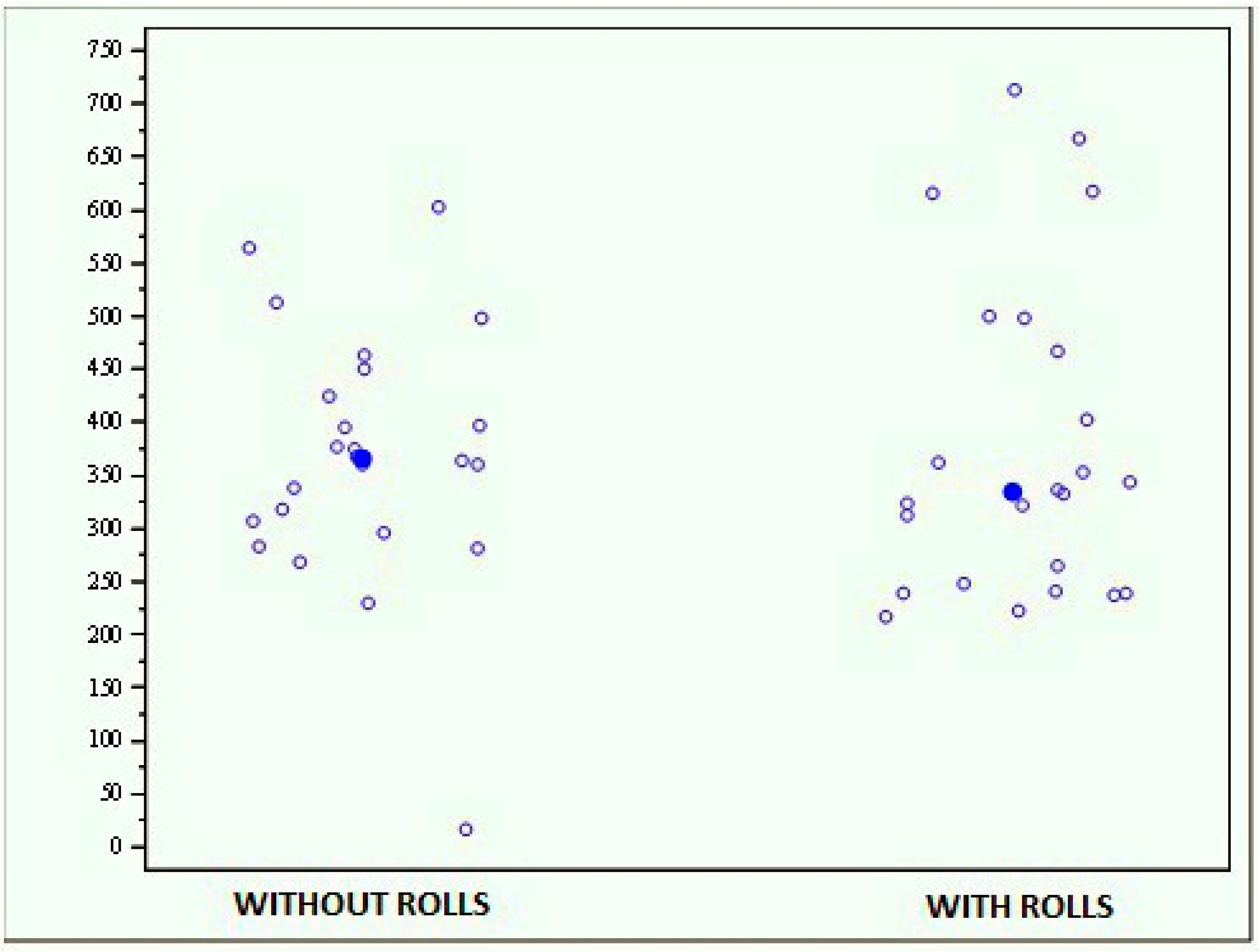
- A stabilometric test with open eyes (Romberg’s test) that consists of keeping on the standing station for 30 s while staring at a red spot on the monitor, during which it assesses the position of the body in space. The numerical value obtained is represented by the area described by the center of mass displacements (in mm2); the higher the value, the worse the test result.
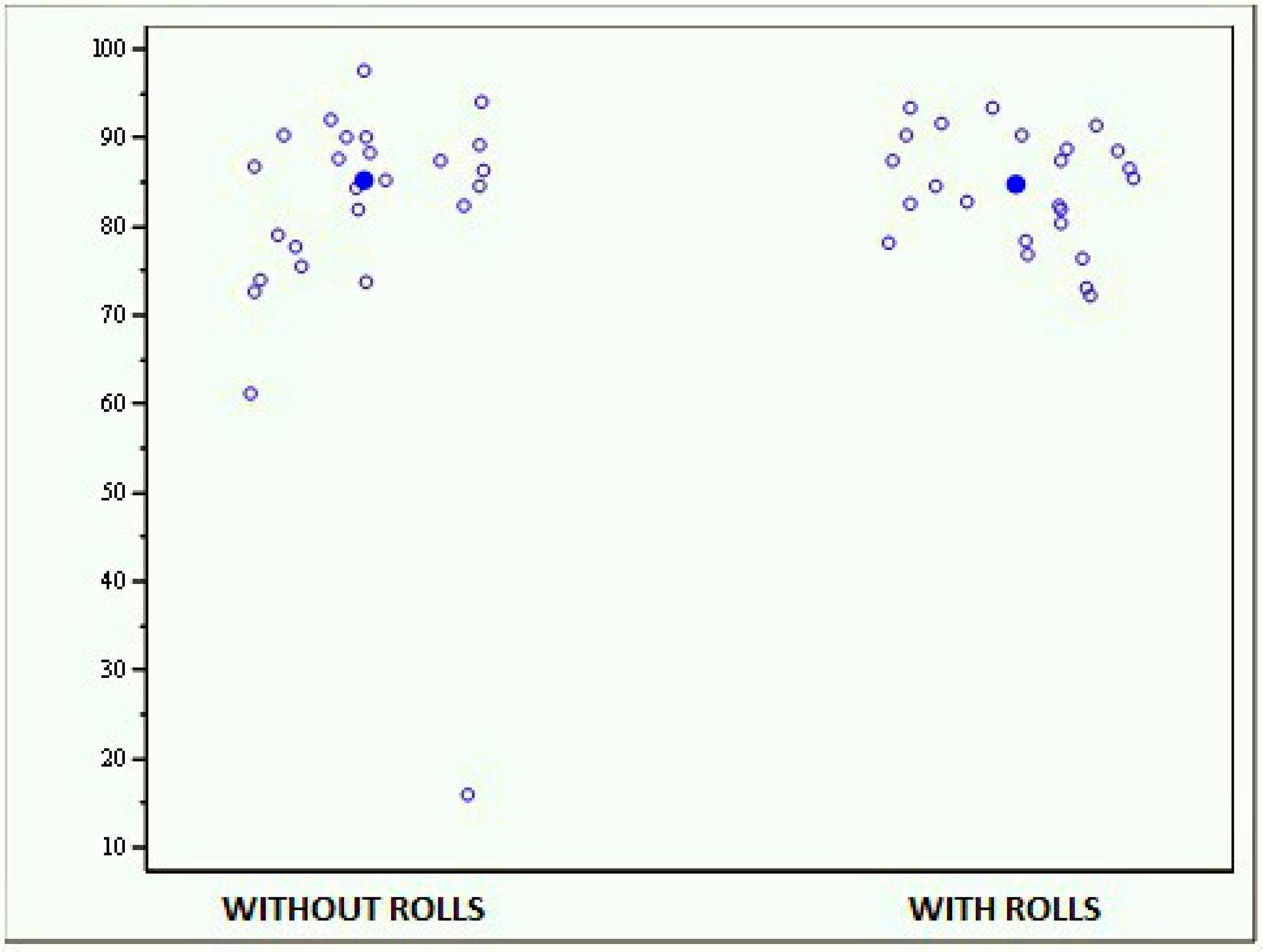
- A test for the evaluation of the stability limit, in which the task is to move the center of gravity towards a point indicated in the monitor; this test is useful for evaluating spatial exploration capacity. The value obtained represents the displacement of the center of mass, expressed as a percentage of the total displacement provided by the software according to the height of the subject (more than 75% is considered normal).
- Two comparative stability tests, including a bipodalic test with open and closed eyes, and a monopodalic test comparing the balance between the right and left foot. The scores are expressed as the area described by the center of mass displacements (in mm2); the higher the value, the worse the test result.
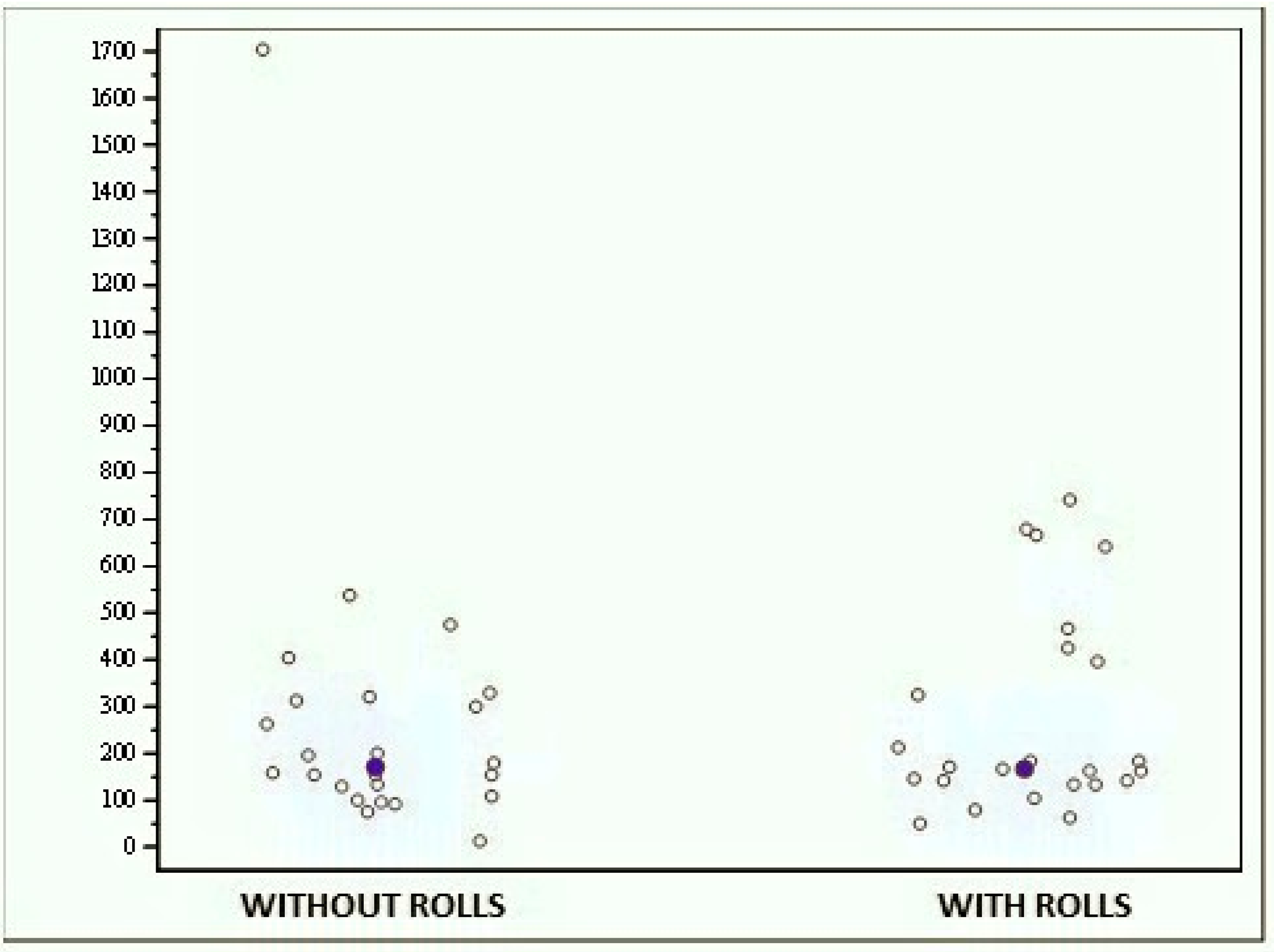
- The first test consists of maintaining the bipodalic equilibrium on the unstable platform with visual feedback, which is useful for identifying the directions of the subject’s imbalance. The value provided by the device is the stability index, that is the distance (expressed in cm) between the center of the platform and the average coordinates of the positions assumed by the center of mass; lower scores correspond to greater stability.
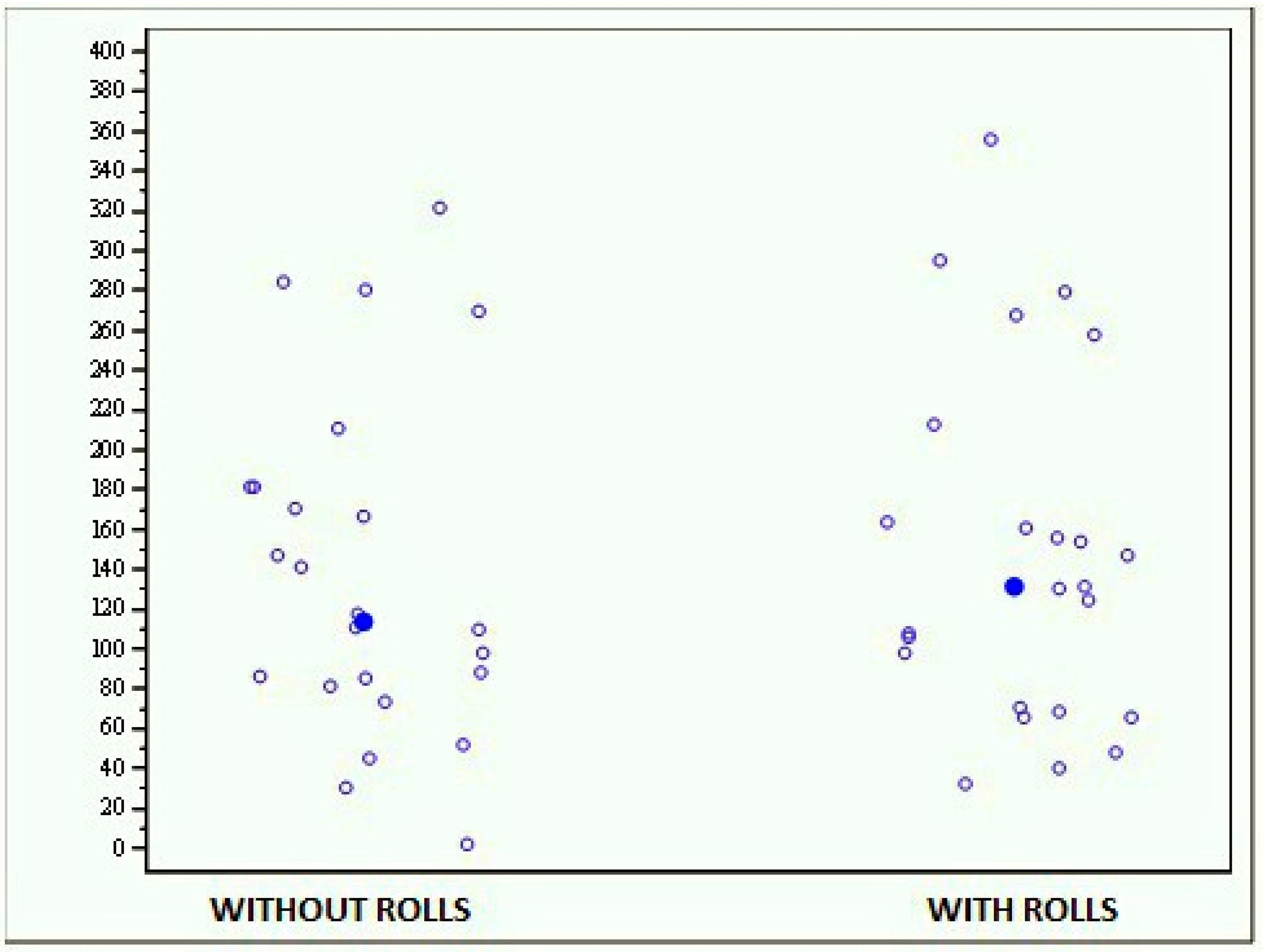
- A second comparative proprioceptive test gives information about body control whilst performing a fine motor skill, in this case represented by tracking a circular trace on the monitor, either with the right foot (clockwise) or with the left foot (anti-clockwise). The result of this test is expressed as an “average trace error”, which indicates the deviation of the subject from the optimal trace, expressed as a percentage; a low value corresponds to a trace close to the ideal line, thus meaning good motor and perceptive capacity.
- A third comparative monopodalic equilibrium test consists in maintaining the dynamic equilibrium in a monopodalic position, first with the right foot and then with the left. The result is expressed as a stability index—that is, the distance (in cm) between the center of the platform and the average coordinates of the positions assumed by the center of mass; the lower the score, the greater the stability.
2.4. Statistical Analysis
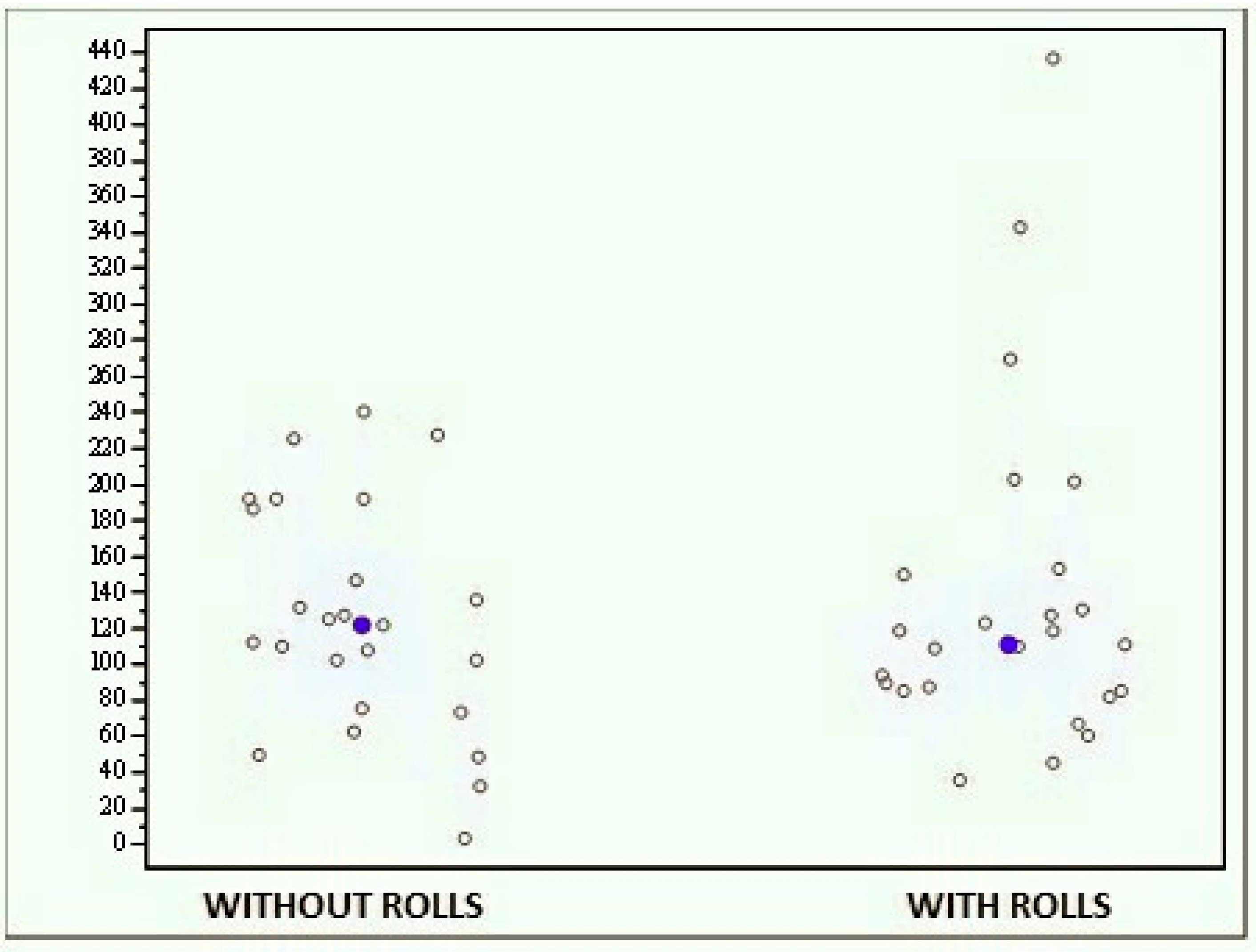
3. Results
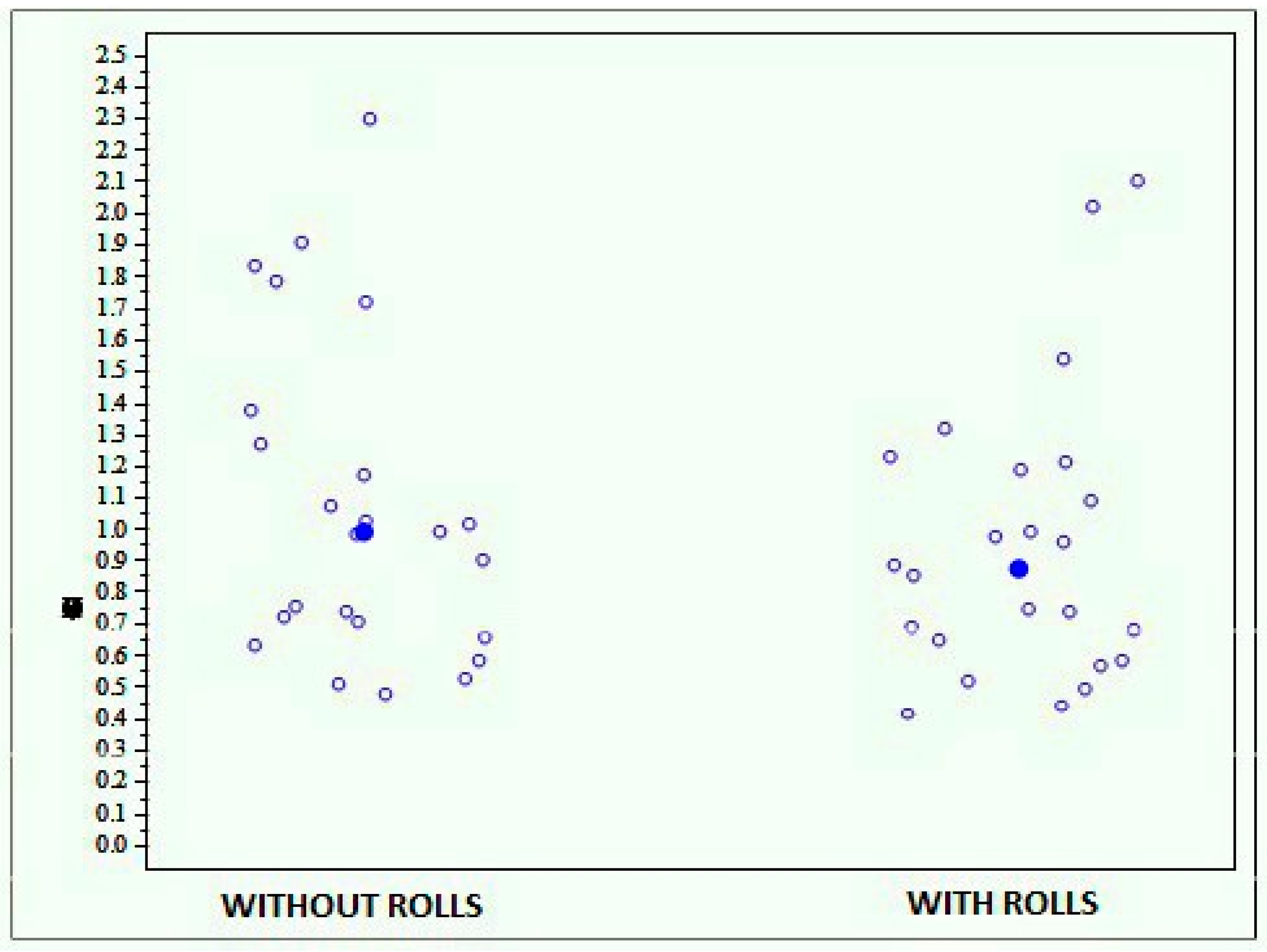
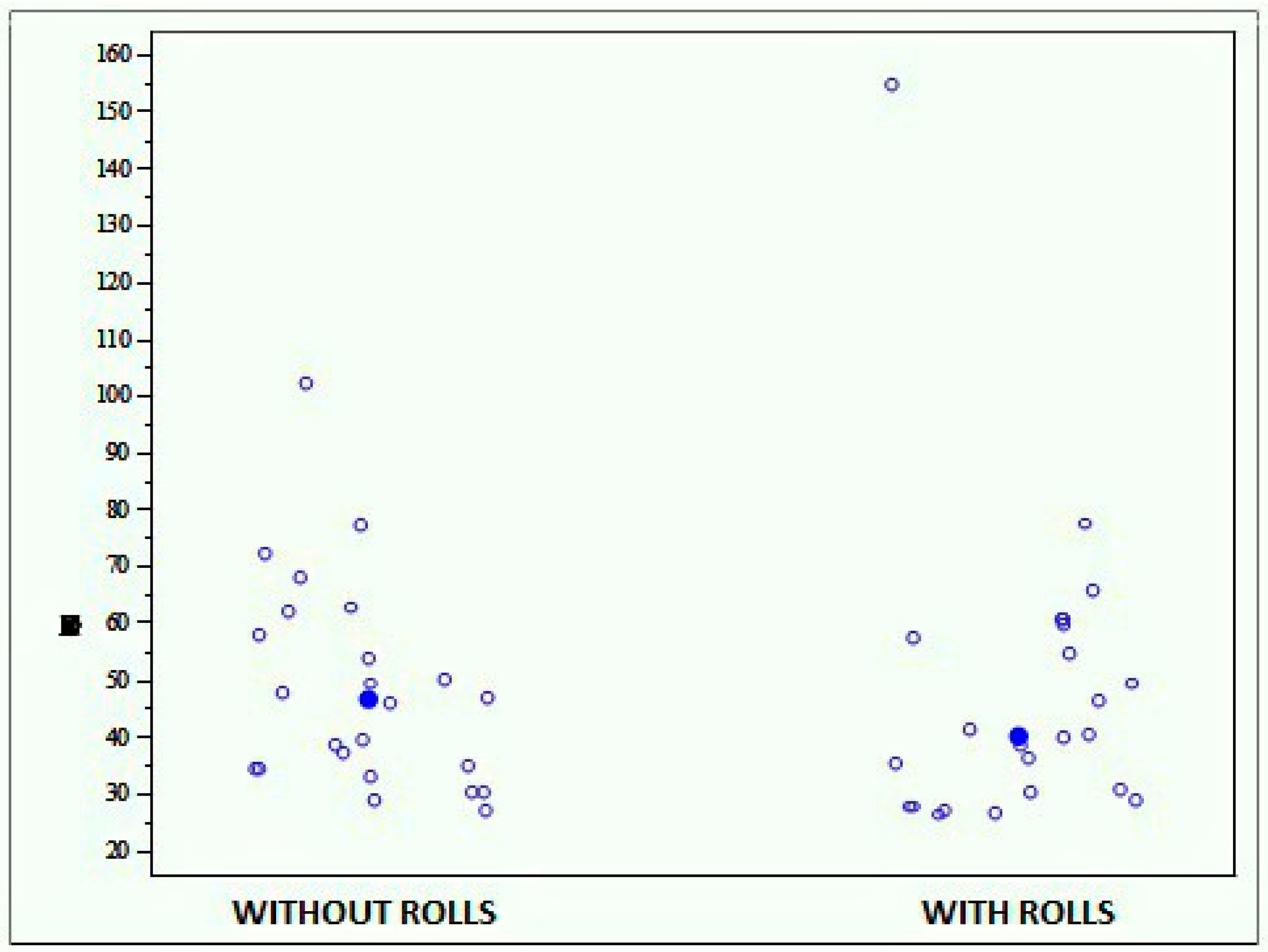
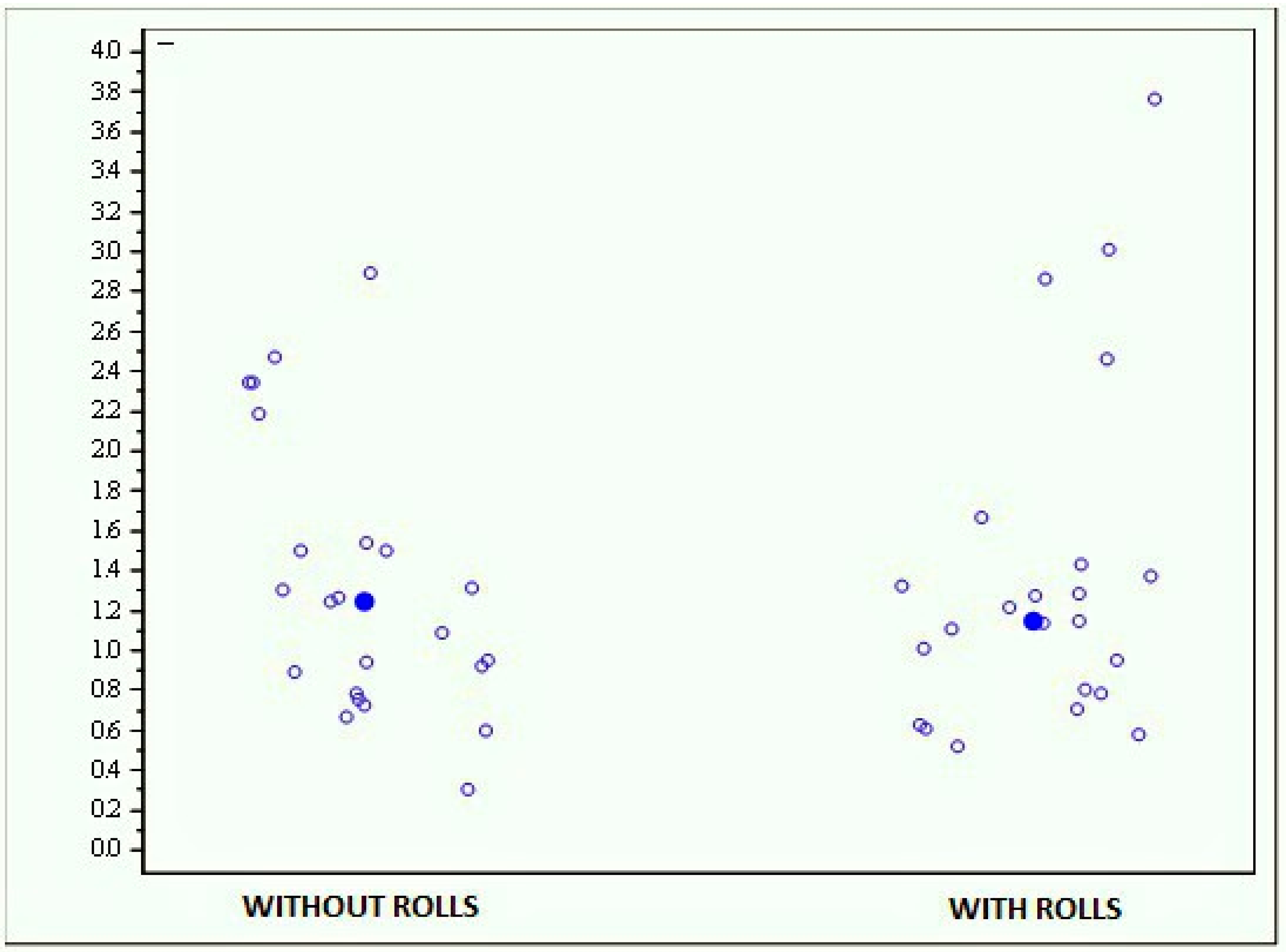
3.1. MF-Stability
3.2. Prokin-B
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Scharnweber, B.; Adjami, F.; Schuster, G.; Kopp, S.; Natrup, J.; Erbe, C.; Ohlendorf, D. Influence of dental occlusion on postural control and plantar pressure distribution. Cranio 2017, 35, 358–366. [Google Scholar] [CrossRef] [PubMed]
- Lacour, M.; Bernard-Demanze, L.; Dumitrescu, M. Posture control, aging, and attention resources: Models and posture-analysis methods. Neurophysiol. Clin. 2008, 38, 411–421. [Google Scholar] [CrossRef] [PubMed]
- Ivanenko, Y.; Gurfinkel, V.S. Human Postural Control. Front. Neurosci. 2018, 12, 171. [Google Scholar] [CrossRef] [PubMed]
- Hugel, F.; Cadopi, M.; Kohler, F.; Perrin, P. Postural control of ballet dancers: A specific use of visual input for artistic purposes. Int. J. Sports Med. 1999, 20, 86–92. [Google Scholar] [CrossRef]
- Ben Achour Lebib, S.; Missaoui, B.; Miri, I.; Ben Salah, F.Z.; Dziri, C. Role of the Neurocom Balance Master in assessment of gait problems and risk of falling in elderly people. Ann. Readapt. Med. Phys. 2006, 49, 210–217. [Google Scholar] [CrossRef]
- Faraldo García, A.; Soto Varela, A.; Santos Pérez, S. Is it possible to shorten examination time in posture control studies? Acta Otorrinolaringol. Esp. 2015, 66, 154–158. [Google Scholar] [CrossRef] [PubMed]
- Ferrario, V.F.; Sforza, C.; Schmitz, J.H.; Taroni, A. Occlusion and center of foot pressure variation: Is there a relationship? J. Prosthet. Dent. 1996, 76, 302–308. [Google Scholar] [CrossRef]
- Ferrario, V.F.; Sforza, C.; Serrao, G.; Fragnito, N.; Grassi, G. The influence of different jaw positions on the endurance and electromyographic pattern of the biceps brachii muscle in young adults with different occlusal characteristics. J. Oral Rehabil. 2001, 28, 732–739. [Google Scholar] [CrossRef]
- Fujimoto, M.; Hayakawa, L.; Hirano, S.; Watanabe, I. Changes in gait stability induced by alteration of mandibular position. J. Med. Dent. Sci. 2001, 48, 131–136. [Google Scholar]
- Armijo Olivo, S.; Magee, D.J.; Parfitt, M.; Major, P.; Thie, N.M. The association between the cervical spine, the stomatognathic system, and craniofacial pain: A critical review. J. Orofac. Pain 2006, 20, 271–287. [Google Scholar]
- Perinetti, G.; Contardo, L.; Silvestrini-Biavati, A.; Perdoni, L.; Castaldo, A. Dental malocclusion and body posture in young subjects: A multiple regression study. Clinics (Sao Paulo) 2010, 65, 689–695. [Google Scholar] [CrossRef] [PubMed]
- Gangloff, P.; Louis, J.P.; Perrin, P.P. Dental occlusion modifies gaze and posture stabilization in human subjects. Neurosci. Lett. 2000, 293, 203–206. [Google Scholar] [CrossRef]
- Hanke, B.A.; Motschall, E.; Türp, J.C. Association between orthopedic and dental findings: What level of evidence is available? J. Orofac. Orthop. 2007, 68, 91–107. [Google Scholar] [CrossRef]
- Bracco, P.; Deregibus, A.; Piscetta, R. Effects of different jaw relations on postural stability in human subjects. Neurosci. Lett. 2004, 356, 228–230. [Google Scholar] [CrossRef] [PubMed]
- Huggare, J. Postural disorders and dentofacial morphology. Acta Odontol. Scand. 1998, 56, 383–386. [Google Scholar] [CrossRef] [PubMed]
- Milani, R.S.; De Perière, D.D.; Lapeyre, L.; Pourreyron, L. Relationship between dental occlusion and posture. Cranio 2000, 18, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Nobili, A.; Adversi, R. Relationship between posture and occlusion: A clinical and experimental investigation. Cranio 1996, 14, 274–285. [Google Scholar] [CrossRef]
- Funakoshi, T.; David, K.L. Physiognomy in the Classification of Individuals with a Lateral Preference in Mastication. J. Orofac. Pain 1976, 8, 61–72. [Google Scholar]
- Martensmeir, I.; Dietrich, P. Which correlations between cervical posture and malocclusions. Fortschr Kieferothop 1992, 52, 26–32. [Google Scholar]
- Tardieu, C.; Dumitrescu, M.; Giraudeau, A.; Blanc, J.L.; Cheynet, F.; Borel, L. Dental occlusion and postural control in adults. Neurosci. Lett. 2009, 450, 221–224. [Google Scholar] [CrossRef]
- Michelotti, A.; Manzo, P.; Farella, M.; Martina, R. Occlusion and posture: Is there evidence of correlation? Miner. Stomatol. 1999, 48, 525–534. [Google Scholar]
- Perinetti, G. Dental occlusion and body posture: No detectable correlation. Gait Posture 2006, 24, 165–168. [Google Scholar] [CrossRef]
- Michelotti, A.; Buonocore, G.; Manzo, P.; Pellegrino, G.; Farella, M. Dental occlusion and posture: An overview. Prog. Orthod. 2011, 12, 53–58. [Google Scholar] [CrossRef]
- Birinci, T.; Demirbas, S.B. Relationship between the mobility of medial longitudinal arch and postural control. Acta Orthop. Traumatol. Turc. 2017, 51, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Saadat, M.; Salehi, R.; Negahban, H.; Shaterzadeh, M.J.; Mehravar, M.; Hessam, M. Postural stability in patients with non-specific chronic neck pain: A comparative study with healthy people. Med. J. Islam. Repub. Iran 2018, 32, 33. [Google Scholar] [CrossRef] [PubMed]
- Faraldo-García, A.; Santos-Pérez, S.; Crujeiras, R.; Labella-Caballero, T.; Soto-Varela, A. Comparative study of computerized dynamic posturography and the SwayStar system in healthy subjects. Acta Otolaryngol. 2012, 132, 271–276. [Google Scholar] [CrossRef]
- Pickerill, M.L.; Harter, R.A. Validity and reliability of limits-of-stability testing: A comparison of 2 postural stability evaluation devices. J. Athl. Train. 2011, 46, 600–606. [Google Scholar] [CrossRef] [PubMed]


© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Isaia, B.; Ravarotto, M.; Finotti, P.; Nogara, M.; Piran, G.; Gamberini, J.; Biz, C.; Masiero, S.; Frizziero, A. Analysis of Dental Malocclusion and Neuromotor Control in Young Healthy Subjects through New Evaluation Tools. J. Funct. Morphol. Kinesiol. 2019, 4, 5. https://doi.org/10.3390/jfmk4010005
Isaia B, Ravarotto M, Finotti P, Nogara M, Piran G, Gamberini J, Biz C, Masiero S, Frizziero A. Analysis of Dental Malocclusion and Neuromotor Control in Young Healthy Subjects through New Evaluation Tools. Journal of Functional Morphology and Kinesiology. 2019; 4(1):5. https://doi.org/10.3390/jfmk4010005
Chicago/Turabian StyleIsaia, Barbara, Martina Ravarotto, Paolo Finotti, Matteo Nogara, Giovanni Piran, Jacopo Gamberini, Carlo Biz, Stefano Masiero, and Antonio Frizziero. 2019. "Analysis of Dental Malocclusion and Neuromotor Control in Young Healthy Subjects through New Evaluation Tools" Journal of Functional Morphology and Kinesiology 4, no. 1: 5. https://doi.org/10.3390/jfmk4010005
APA StyleIsaia, B., Ravarotto, M., Finotti, P., Nogara, M., Piran, G., Gamberini, J., Biz, C., Masiero, S., & Frizziero, A. (2019). Analysis of Dental Malocclusion and Neuromotor Control in Young Healthy Subjects through New Evaluation Tools. Journal of Functional Morphology and Kinesiology, 4(1), 5. https://doi.org/10.3390/jfmk4010005







