What Is the Evidence on Which Physicians Can Rely to Advise Patients When They May Resume Driving after TKA? A Systematic Literature Review
Abstract
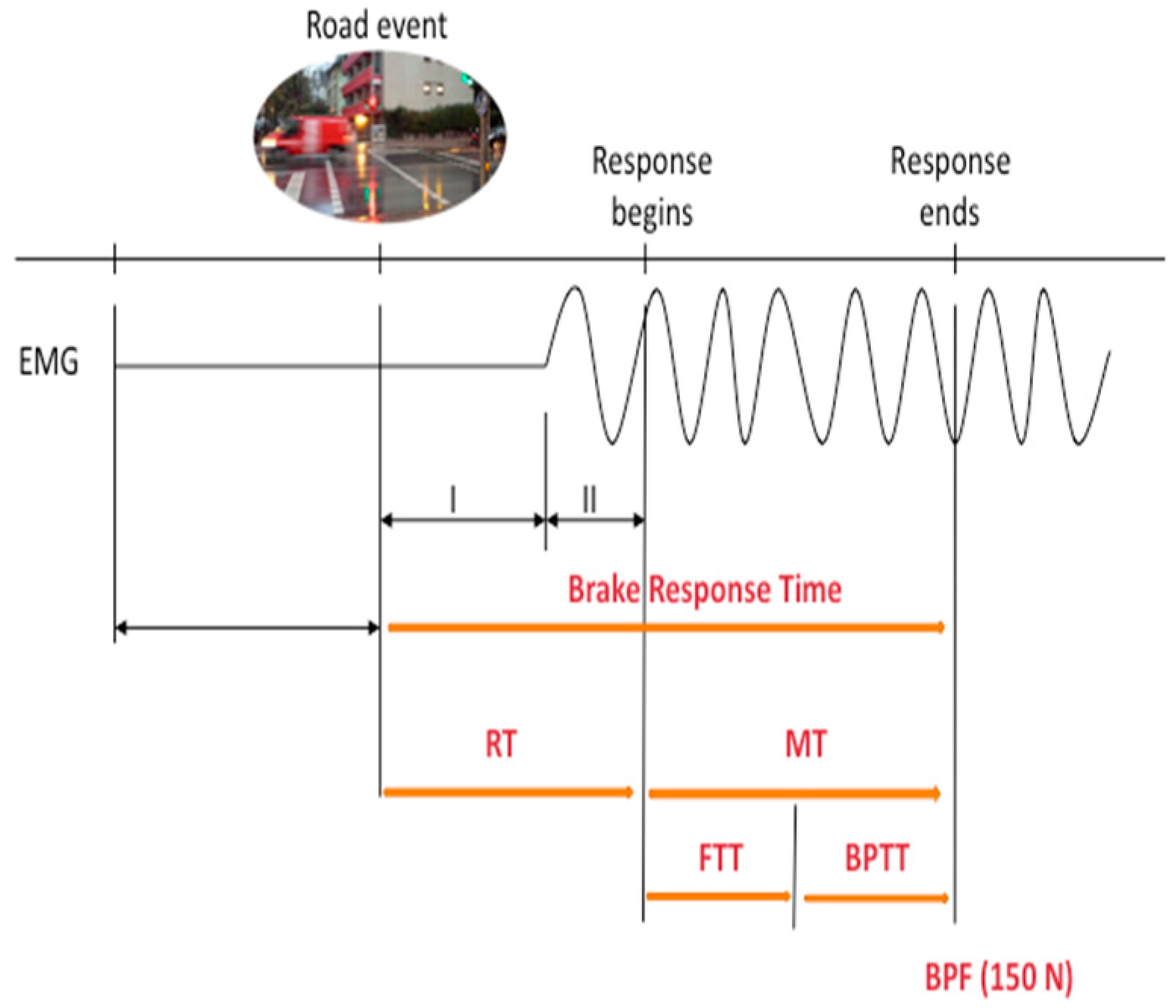
:1. Introduction
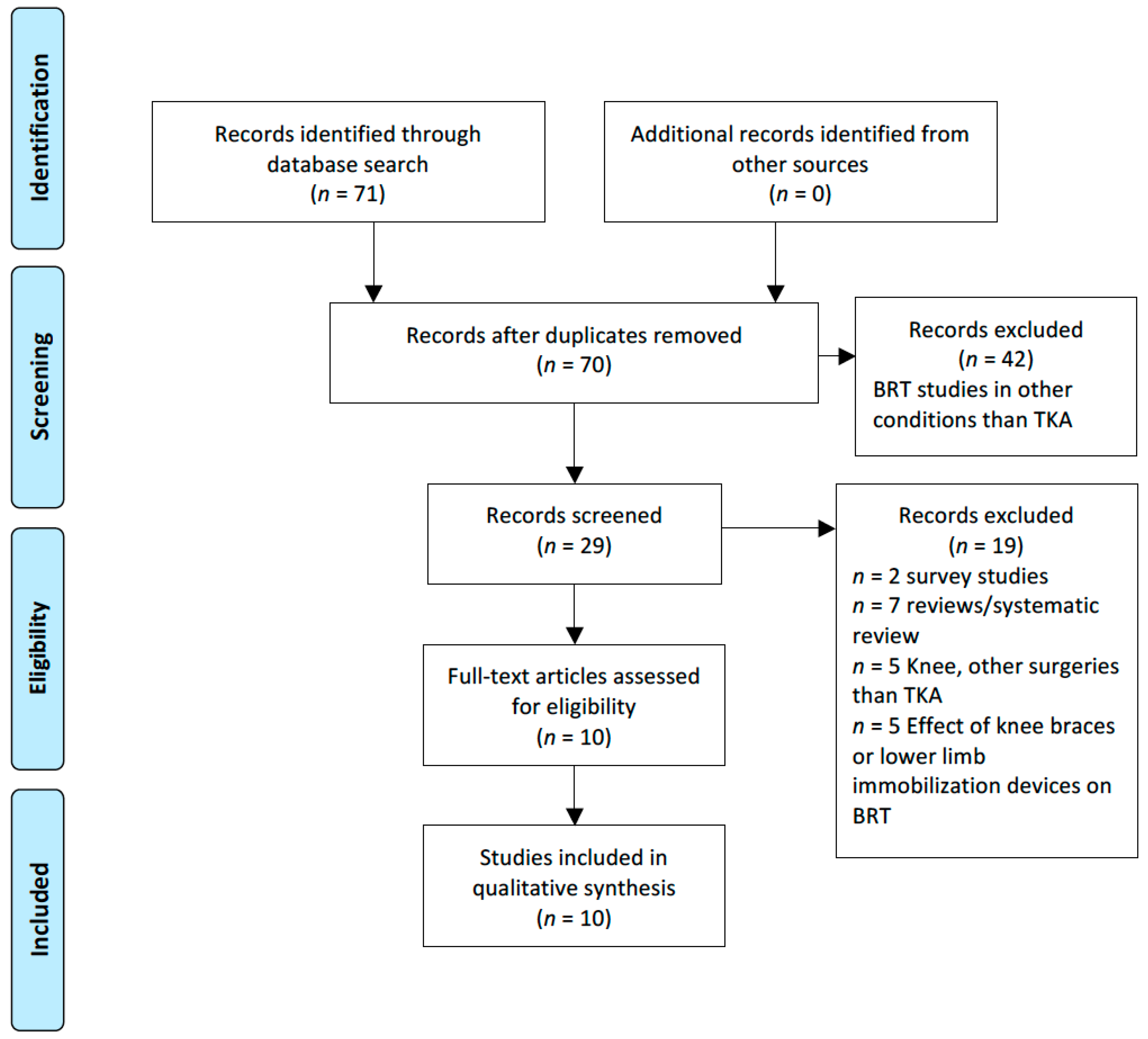
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria and Study Selection
2.3. Risk of Bias Assessment
2.4. Data Collection Process
2.5. Statistical Analysis
3. Results
3.1. Quality Assessment of the Included Studies
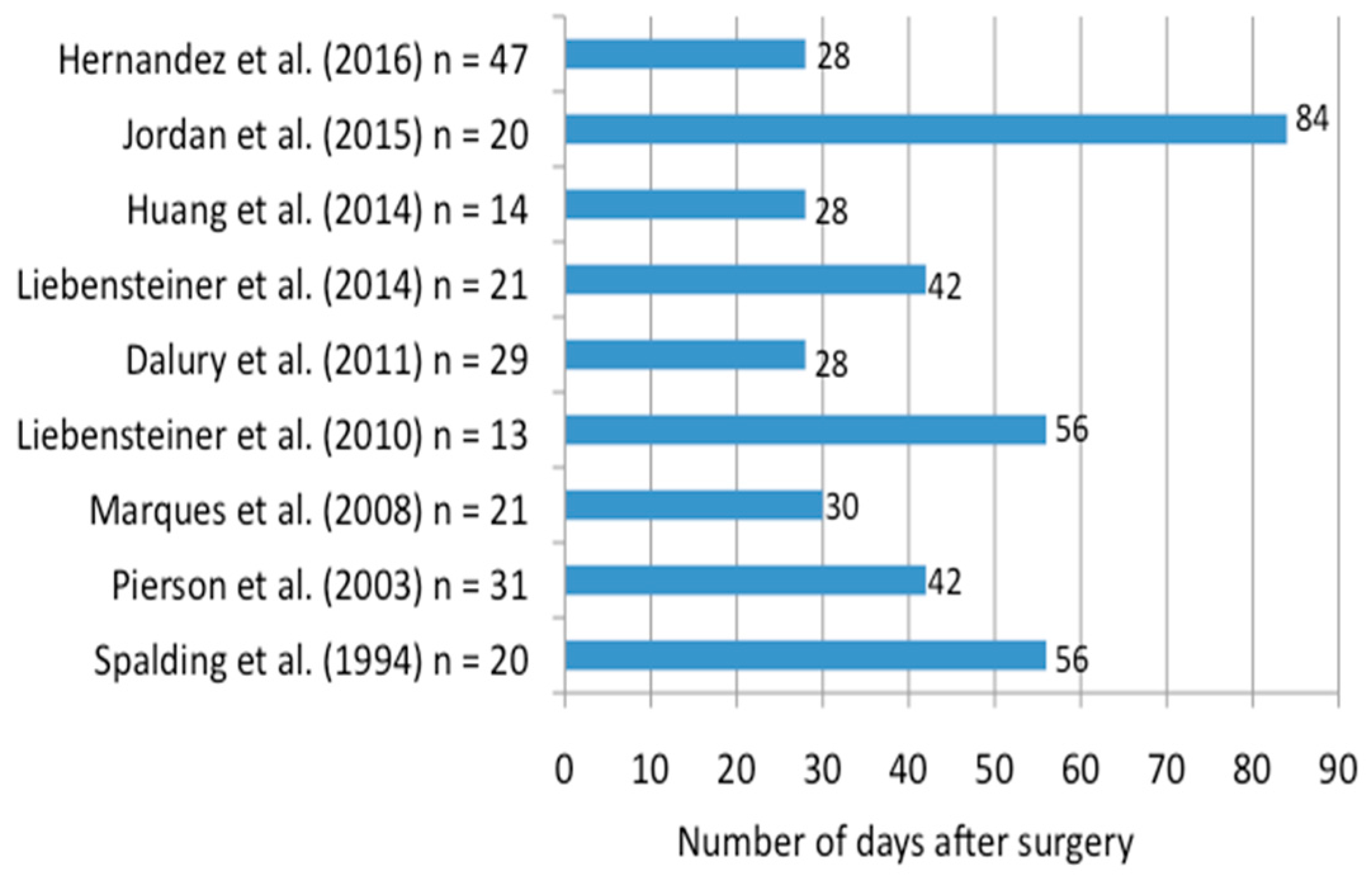
3.2. When Does the BRT of the Right Leg Return to Baseline Values after Right TKA?
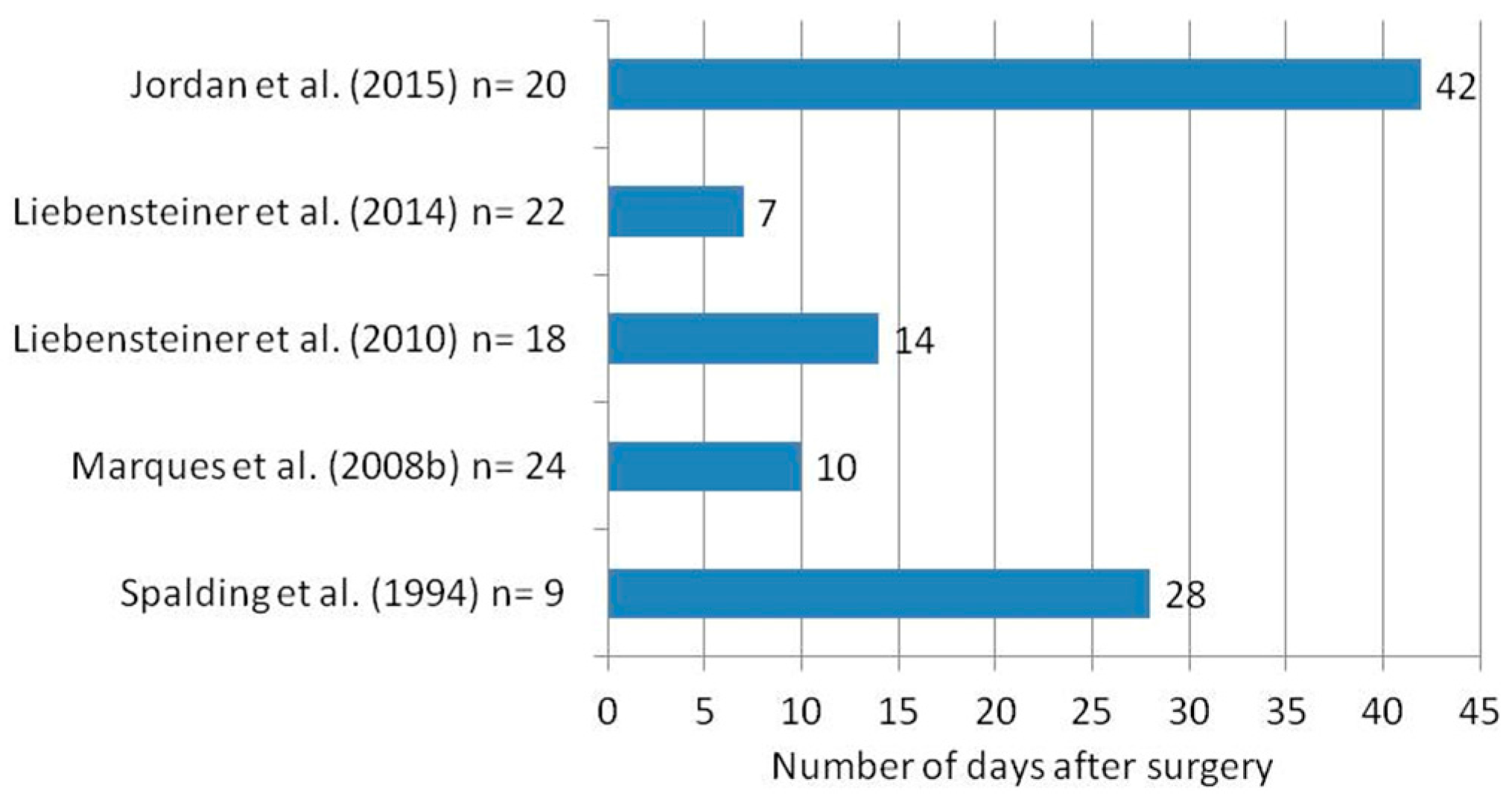
3.3. When Does the BRT of the Right Leg Return to Baseline Values after Left TKA?
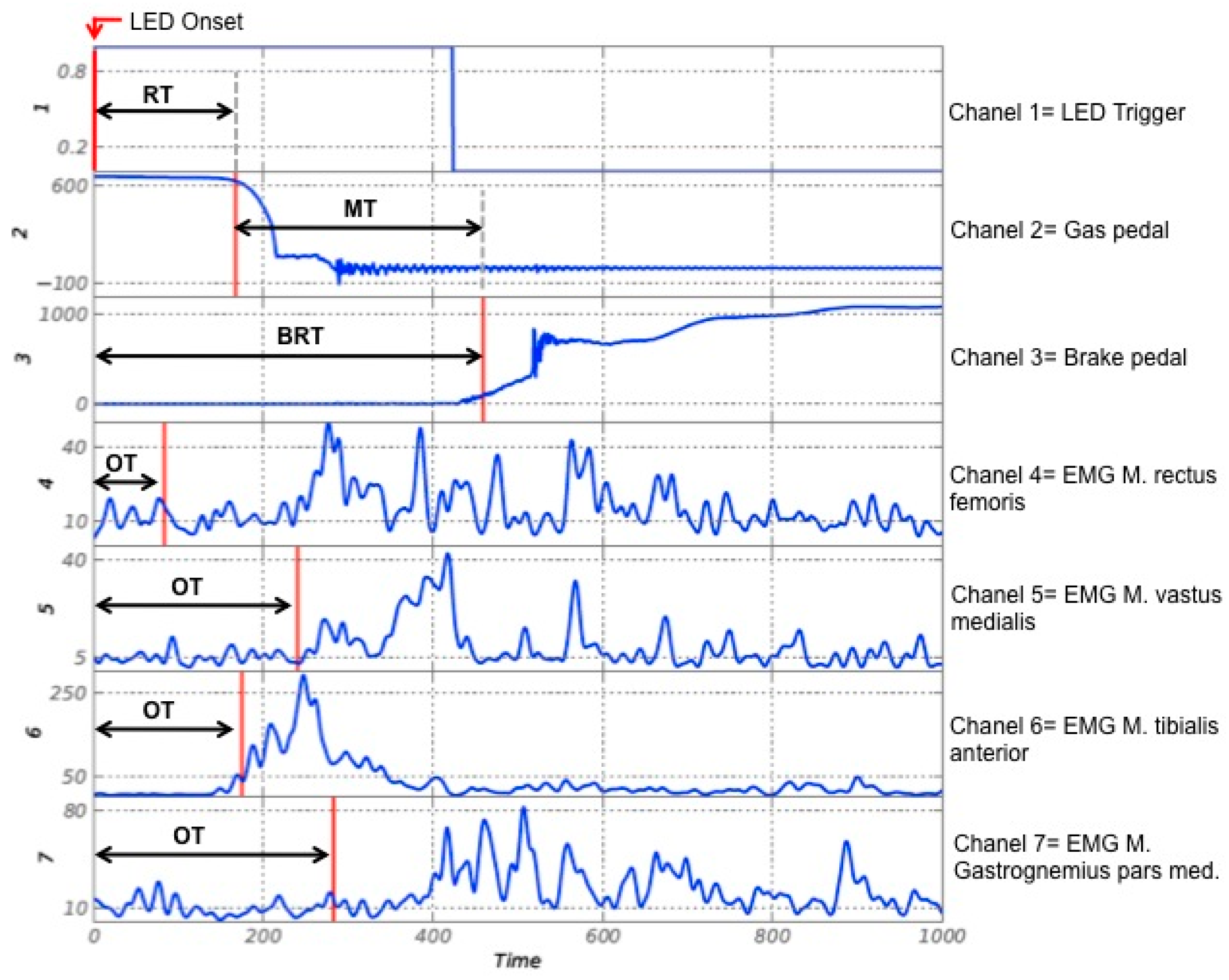
3.4. Are BRT Components, RT and MT, Equally Affected after TKA?
3.5. Are There Gender Differences Regarding the Influence of TKA on BRT and Its Recovery?
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A. Search Strategy
| #1 | Total knee replacement OR Total knee arthroplasty |
| #2 | Knee replacement |
| #3 | Knee prosthesis |
| #4 | Arthroplasty |
| #5 | #1 OR #2 OR #3 OR #4 |
| #6 | Brake response time |
| #7 | Car driving |
| #8 | Automobile driving |
| #9 | Reaction time |
| #10 | Movement time |
| #11 | Braking |
| #12 | #6 OR #7 OR #8 OR #9 OR #10 OR #11 |
| #13 | #5 AND #12 |
| #1 | Brake response time |
| #2 | Braking |
| #3 | Automobile driving |
| #4 | Movement time |
| #5 | Arthroplasty, replacement, knee |
| #6 | Total knee arthroplasty |
| #7 | Reaction time |
| #8 | #1 AND #6 |
| #9 | #3 AND #6 |
| #10 | #6 AND #7 |
| #11 | #7 OR #4 OR #3 OR #2 OR #1 |
| #12 | #6 AND #11 |
| #1 | Total knee replacement (MeSH) |
| #2 | Knee joint (MeSH) |
| #3 | Arthroplasty (MeSH) |
| #4 | Knee prosthesis (MeSH) |
| #5 | #1 OR #2 OR #3 OR #4 |
| #6 | Automobile driving (MeSH) |
| #7 | Braking |
| #8 | Reaction time (MeSH) |
| #9 | Movement time |
| #10 | #6 OR #7 OR #8 OR #9 |
| #11 | #5 AND #10 |
Appendix B
| References | Dependent Variables | Measurement Times (Weeks or Days) | Sample Size (n) | Mean Age (Years) | Main Results (* = Particularities) | |||
|---|---|---|---|---|---|---|---|---|
| BRT | RT | MT | Force | |||||
| Spalding, T.J.W. et al. (1994) | Yes | Yes | Yes | Yes | Before, 4, 6, 8, and 10 weeks after | n = 29 (18 drivers; 11 non-drivers) 20 right TKA 9 left TKA | 74 (61–83) | Right TKA: -RT remained unchanged at 4 weeks. -MT was 50% increased at 4 weeks; at 8 weeks returned to pre-op values. Left TKA: -BRT, RT, and MT remained unchanged 4 weeks after surgery. * High dropout rates: 27.5% started the study but did not finish it. * From 29 subjects included for analysis, 11 had been non-drivers. |
| Pierson, J.L. et al. (2003) | Yes | No | No | No | Before, 3, 6, and 9 weeks after | n = 31 (17M; 14W) 13 bilateral TKA 18 unilateral TKA: −12 right TKA −6 left TKA | 68.6 (±7.6) | BRT: -12.5% quicker response at 6 weeks -17.5% quicker response at 9 weeks * Since 3 × 4 ANOVA revealed no significant differences in average BRT x laterality of TKA, the authors collapsed all patients across the variable “side of surgery” for all statistical analysis. For this reason, the results are probably biased. |
| Marques, C.J. et al. (2008) | Yes | Yes | Yes | No | Before, 10 and 30 days after | n = 21 21 right TKA: (9 M; 12 W) | 69.1 (±7.8) | Right BRT: -was 9.01% increased at 10 days -was still 1.7% increased at 30 days (statistically not significant) RT: -no significant differences across the measurements MT: -was significantly increased at 10 days -at 30 days it was still significantly increased -high dropout rates (22% were not assessed at the 3rd measurement) |
| Marques, C.J. et al. (2008) | Yes | Yes | Yes | No | Before, 10 and 30 days after | n = 24 24 left TKA (13 M; 11 W) | 63.2 (±8.5) | Left TKA: -BRT, RT, and MT were not affected 10 days after surgery |
| Liebensteiner, M.C. et al. (2010) | Yes | No | No | No | Before, 2 and 8 weeks after | n = 31 (14M, 17W) 13 right TKA 18 left TKA Control group n = 31 (12 M; 19 W) | 65.7 (±10.2) | Right TKA: -BRT was not significant increased at 2 weeks -BRT decreased significantly from 2 to 8 weeks. Left TKA: -BRT was not significantly increased at 2 weeks -Significant decrease between 2 and 8 weeks * High drop-out rates between Pre-Op and 2 weeks due to discomfort while sitting in the car simulator. * Control group was not age and gender matched. |
| Dalury, D.F. et al. (2011) | Yes | Yes | Yes | No | Before, 4, 6, and 8 weeks after | n = 29 29 right TKA | 66 (47–81) | -At 4 weeks all patients performed faster than preoperatively -RT: significantly faster at 4 weeks -FTT: no significant difference at 4 weeks |
| Liebensteiner, M.C. et al. (2014) | Yes | No | No | No | Before, 1 and 6 weeks | n = 43 (22 M; 21 W) 21 right TKA 22 left TKA | 59.8 (±7.5) | Right UKA (Unicompartmental knee arthroplasty): -BRT was significant increased at 1 week. -Baseline values were achieved at week 6 Left UKA: -BRT was not significantly changed at 1 week * High dropout rates: 26% of the patients assessed preoperatively dropped out at 6 weeks. |
| Huang, Hsuan-Ti et al. (2014) | Yes | Yes | Yes | No | Before, 2 and 4 weeks | n = 14 14 right TKA: (4 M; 10 W) | 63.1 (±6.6) | Right TKA: -BRT returned to baseline at 4 weeks at a driving speed of 50 and 70 km/h -At a driving speed of 90 km/h the BRT was still significantly increased at 4 weeks. * Minimally invasive surgery (MIS) was used for all surgeries. All subjects were tested at three different speeds (50, 70, and 90 km/h). The order of performing at different speeds was not randomized. Are the patients performing at a 90 km/h speed slower as an effect of fatigue? |
| Jordan, M. et al. (2015) | Yes | Yes | Yes | Yes | Before, 8 days, and 6, 12, and 52 weeks | n = 40 20 right TKA: (10 M; 10 W) 20 left TKA: (8 M; 12 W) | 69 (right TKA) 73 (left TKA) | Right TKA: -BRT was significantly increased at 8 days by 30% -Brake Force (BF) was significantly decreased by 35% -Baseline values were reached at week 12 Left TKA: -BRT was not significant increased at 8 days (2%) -BF was significantly decreased by 25% at 8 days -BRT below baseline at week 6 -11% were lost to follow-up |
| Hernandez, V.H. et al. (2016) | Yes | No | No | No | Before, 2, 4, and 6 weeks | n = 47 47 right TKA (48.3% M; 61.7% W) | 67.5 (±10.0) | -BRT of 39 patients (80%) was at baseline by 2 weeks -20% reached baseline by 4 weeks * All patients managed with spinal anesthesia. Multimodal pain management and rapid mobilization physical therapy protocol were used. |
References
- Ranawat, C.S.; Flynn, W.F., Jr.; Saddler, S.; Hansraj, K.K.; Maynard, M.J. Long-term results of the total condylar knee arthroplasty. A 15-year survivorship study. Clin. Orthop. Relat. Res. 1993, 286, 94–102. [Google Scholar]
- Sabouret, P.; Lavoie, F.; Cloutier, J.M. Total knee replacement with retention of both cruciate ligaments: A 22-year follow-up study. Bone Joint J. 2013, 95-B, 917–922. [Google Scholar] [CrossRef] [PubMed]
- Inacio, M.C.S.; Paxton, E.W.; Graves, S.E.; Namba, R.S.; Nemes, S. Projected increase in total knee arthroplasty in the United States—An alternative projection model. Osteoarthr. Cartil. 2017, 25, 1797–1803. [Google Scholar] [CrossRef] [PubMed]
- Kehlet, H. Fast-track hip and knee arthroplasty. Lancet 2013, 381, 1600–1602. [Google Scholar] [CrossRef]
- Kehlet, H.; Thienpont, E. Fast-track knee arthroplasty—Status and future challenges. Knee 2013, 20, S29–S33. [Google Scholar] [CrossRef]
- Khan, S.K.; Malviya, A.; Muller, S.D.; Carluke, I.; Partington, P.F.; Emmerson, K.P.; Reed, M.R. Reduced short-term complications and mortality following Enhanced Recovery primary hip and knee arthroplasty: Results from 6,000 consecutive procedures. Acta Orthop. 2014, 85, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Savaridas, T.; Serrano-Pedraza, I.; Khan, S.K.; Martin, K.; Malviya, A.; Reed, M.R. Reduced medium-term mortality following primary total hip and knee arthroplasty with an enhanced recovery program. A study of 4,500 consecutive procedures. Acta Orthop. 2013, 84, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Husted, H.; Jensen, C.M.; Solgaard, S.; Kehlet, H. Reduced length of stay following hip and knee arthroplasty in Denmark 2000–2009: From research to implementation. Arch. Orthop. Trauma Surg. 2012, 132, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Husted, H.; Lunn, T.H.; Troelsen, A.; Gaarn-Larsen, L.; Kristensen, B.B.; Kehlet, H. Why still in hospital after fast-track hip and knee arthroplasty? Acta Orthop. 2011, 82, 679–684. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.; Hau, R.; Bartlett, J. Driving reaction time before and after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2000, 8, 226–230. [Google Scholar] [CrossRef] [PubMed]
- Talusan, P.G.; Miller, C.P.; Save, A.V.; Reach, J.S., Jr. Driving reaction times in patients with foot and ankle pathology before and after image-guided injection: Pain relief without improved function. Foot Ankle Spec. 2015, 8, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Thaler, M.; Lechner, R.; Foedinger, B.; Haid, C.; Kavakebi, P.; Galiano, K.; Obwegeser, A. Driving reaction time before and after surgery for lumbar disc herniation in patients with radiculopathy. Eur. Spine J. 2012, 21, 2259–2264. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. March 2014. Available online: https://www.nhlbi.nih.gov/health-topics/study-qulaity-assessment-tools (accessed on 17 Febbruary 2016).
- Ellanti, P.; Raval, P.; Harrington, P. Return to driving after total knee arthroplasty. Acta Orthop. Traumatol. Turc. 2015, 49, 593–596. [Google Scholar] [CrossRef] [PubMed]
- Lewis, C.; Mauffrey, C.; Hull, P.; Brooks, S. Knee arthroscopy and driving. Results of a prospective questionnaire survey and review of the literature. Acta Orthop. Belg. 2011, 77, 336–338. [Google Scholar] [PubMed]
- Argintar, E.; Williams, A.; Kaplan, J.; Hall, M.P.; Sanders, T.; Yalamanchili, R.; Hatch, G.F., 3rd. Recommendations for driving after right knee arthroscopy. Orthopedics 2013, 36, 659–665. [Google Scholar] [CrossRef] [PubMed]
- DiSilvestro, K.J.; Santoro, A.J.; Tjoumakaris, F.P.; Levicoff, E.A.; Freedman, K.B. When can i drive after orthopaedic surgery? A Systematic Review. Clin. Orthop. Relat. Res. 2016, 474, 2557–2570. [Google Scholar] [CrossRef] [PubMed]
- Giddins, G.E.; Hammerton, A. “Doctor, when can I drive?”: A medical and legal view of the implications of advice on driving after injury or operation. Injury 1996, 27, 495–497. [Google Scholar] [CrossRef]
- Goodwin, D.; Baecher, N.; Pitta, M.; Letzelter, J.; Marcel, J.; Argintar, E. Driving after orthopedic surgery. Orthopedics 2013, 36, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Hartman, J.; Thornley, P.; Oreskovich, S.; Adili, A.; Bedi, A.; Khan, M. Braking time following total knee arthroplasty: A systematic review. J. Arthroplast. 2017, 33, 284–290. [Google Scholar] [CrossRef] [PubMed]
- MacLeod, K.; Lingham, A.; Chatha, H.; Lewis, J.; Parkes, A.; Grange, S.; Smitham, P.J. “When can I return to driving?”: A review of the current literature on returning to driving after lower limb injury or arthroplasty. Bone Joint J. 2013, 95-B, 290–294. [Google Scholar] [CrossRef] [PubMed]
- Van der Velden, C.A.; Tolk, J.J.; Janssen, R.P.A.; Reijman, M. When is it safe to resume driving after total hip and total knee arthroplasty? a meta-analysis of literature on post-operative brake reaction times. Bone Joint. J. 2017, 99-B, 566–576. [Google Scholar] [CrossRef] [PubMed]
- Gotlin, R.S.; Sherman, A.L.; Sierra, N.; Kelly, M.; Scott, W.N. Measurement of brake response time after right anterior cruciate ligament reconstruction. Arthroscopy 2000, 16, 151–155. [Google Scholar] [CrossRef]
- Gotlin, R.S.; Sherman, A.L.; Sierra, N.; Kelly, M.A.; Pappas, Z.; Scott, W.N. Measurement of brake response time after right anterior cruciate ligament reconstruction. Arch. Phys. Med. Rehabil. 2000, 81, 201–204. [Google Scholar] [CrossRef]
- Hau, R.; Csongvay, S.; Bartlett, J. Driving reaction time after right knee arthroscopy. Knee Surg. Sports Traumatol. Arthrosc. 2000, 8, 89–92. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, U.K.; Jordan, M.; Rondak, I.; Wolf, P.; Kluba, T.; Ipach, I. Osteoarthritis of the knee or hip significantly impairs driving ability (cross-sectional survey). BMC Musculoskelet. Disord. 2014, 15, 20. [Google Scholar] [CrossRef] [PubMed]
- Dammerer, D.; Giesinger, J.M.; Biedermann, R.; Haid, C.; Krismer, M.; Liebensteiner, M. Effect of knee brace type on braking response time during automobile driving. Arthroscopy 2015, 31, 404–409. [Google Scholar] [CrossRef] [PubMed]
- Murray, J.C.; Tremblay, M.A.; Corriveau, H.; Hamel, M.; Cabana, F. Effects of right lower limb orthopedic immobilization on braking function: An on-the-road experimental study with healthy volunteers. J. Foot Ankle Surg. 2015, 54, 554–558. [Google Scholar] [CrossRef] [PubMed]
- Nunn, T.; Baird, C.; Robertson, D.; Gray, I.; Gregori, A. Fitness to drive in a below knee plaster? An evidence based response. Injury 2007, 38, 1305–1307. [Google Scholar] [CrossRef] [PubMed]
- Sansosti, L.E.; Rocha, Z.M.; Lawrence, M.W.; Meyr, A.J. Effect of variable lower extremity immobilization devices on emergency brake response driving outcomes. J. Foot Ankle Surg. 2016, 55, 999–1002. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.A.; Corriveau, H.; Boissy, P.; Smeesters, C.; Hamel, M.; Murray, J.C.; Cabana, F. Effects of orthopaedic immobilization of the right lower limb on driving performance: An experimental study during simulated driving by healthy volunteers. J. Bone Joint. Surg. Am. 2009, 91, 2860–2866. [Google Scholar] [CrossRef] [PubMed]
- Dalury, D.F.; Tucker, K.K.; Kelley, T.C. When can I drive?: Brake response times after contemporary total knee arthroplasty. Clin. Orthop. Relat. Res. 2011, 469, 82–86. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.T.; Liang, J.M.; Hung, W.T.; Chen, Y.Y.; Guo, L.Y.; Wu, W.L. Timeframe for return to driving for patients with minimally invasive knee arthroplasty is associated with knee performance on functional tests. BMC Musculoskelet. Disord. 2014, 15, 198. [Google Scholar] [CrossRef] [PubMed]
- Jordan, M.; Hofmann, U.K.; Rondak, I.; Gotze, M.; Kluba, T.; Ipach, I. Brake response time is significantly impaired after total knee arthroplasty: investigation of performing an emergency stop while driving a car. Am. J. Phys. Med. Rehabil. 2015, 94, 665–676. [Google Scholar] [CrossRef] [PubMed]
- Liebensteiner, M.C.; Kern, M.; Haid, C.; Kobel, C.; Niederseer, D.; Krismer, M. Brake response time before and after total knee arthroplasty: A prospective cohort study. BMC Musculoskelet. Disord. 2010, 11, 267. [Google Scholar] [CrossRef] [PubMed]
- Liebensteiner, M.C.; Rochau, H.; Renz, P.; Smekal, V.; Rosenberger, R.; Birkfellner, F.; Haid, C.; Krismer, M. Brake response time returns to the pre-surgical level 6 weeks after unicompartmental knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1926–1931. [Google Scholar] [CrossRef] [PubMed]
- Marques, C.J.; Barreiros, J.; Cabri, J.; Carita, A.I.; Friesecke, C.; Loehr, J.F. Does the brake response time of the right leg change after left total knee arthroplasty? A prospective study. Knee 2008, 15, 295–298. [Google Scholar] [CrossRef] [PubMed]
- Marques, C.J.; Cabri, J.; Barreiros, J.; Carita, A.I.; Friesecke, C.; Loehr, J.F. The effects of task complexity on brake response time before and after primary right total knee arthroplasty. Arch. Phys. Med. Rehabil. 2008, 89, 851–855. [Google Scholar] [CrossRef] [PubMed]
- Pierson, J.L.; Earles, D.R.; Wood, K. Brake response time after total knee arthroplasty: When is it safe for patients to drive? J. Arthroplast. 2003, 18, 840–843. [Google Scholar] [CrossRef]
- Spalding, T.J.; Kiss, J.; Kyberd, P.; Turner-Smith, A.; Simpson, A.H. Driver reaction times after total knee replacement. J. Bone Joint. Surg. Br. 1994, 76, 754–756. [Google Scholar] [PubMed]
- Hernandez, V.H.; Ong, A.; Orozco, F.; Madden, A.M.; Post, Z. When is it safe for patients to drive after right total hip arthroplasty? J. Arthroplast. 2015, 30, 627–630. [Google Scholar] [CrossRef] [PubMed]
- Warshawsky-Livne, L.; Shinar, D. Effects of uncertainty, transmission type, driver age and gender on brake reaction and movement time. J. Saf. Res. 2002, 33, 117–128. [Google Scholar] [CrossRef]
- Montgomery, J.; Kusano, K.D.; Gabler, H.C. Age and gender differences in time to collision at braking from the 100-Car Naturalistic Driving Study. Traffic Inj. Prev. 2014, 15, S15–S20. [Google Scholar] [CrossRef] [PubMed]
- Davies, B.T.; Watts, J.M., Jr. Preliminary investigation of movement time between brake and accelerator pedals in automobiles. Hum. Factors 1969, 11, 407–409. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, E.R. Accelerator-to-brake movement times. Ergonomics 1991, 34, 277–287. [Google Scholar] [CrossRef]
- Liebensteiner, M.C.; Birkfellner, F.; Thaler, M.; Haid, C.; Bach, C.; Krismer, M. Driving reaction time before and after primary fusion of the lumbar spine. Spine 2010, 35, 330–335. [Google Scholar] [CrossRef] [PubMed]
- Scott, P.A.; Candler, P.D.; Li, J.-C. Stature and seat position as factors affecting fractionated response time in motor vehicle drivers. Appl. Ergon. 1996, 27, 411–416. [Google Scholar] [CrossRef]
| Criteria | Included Studies | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Spalding, T.J.W. et al. (1994) | Pierson, J.L. et al. (2003) | Marques, C.J. et al. (2008a) | Marques, C.J. et al. (2008b) | Liebensteiner, M.C. et al. (2010) | Dalury, F.D. et al. (2011) | Liebensteiner, M.C. et al. (2014) | Huang, H.-T. et al. (2014) | Jordan, M. et al. (2015) | Hernandez, V.H. et al. (2016) | |
| 1. Was the research question clearly stated? | ||||||||||
| 2. Was the study population clearly defined? | ||||||||||
| 3. Were inclusion and exclusion criteria well described? | ||||||||||
| 4. Were key potential confounding factors (e.g., age and gender) balanced? | ||||||||||
| 5. Was patient recruitment period and flow well described? | ||||||||||
| 6. Was a sample size justification, power description, or variance and effect estimates provided? | ||||||||||
| 7. Were the timeframes between the repeated measures sufficient to detect changes from baseline? | ||||||||||
| 8. Were the dependent variables (BRT, RT, MT) clearly defined? | ||||||||||
| 9. Were the materials used to access the dependent variables (car simulator) well described, inclusive pedal layout description? | ||||||||||
| 10. Were any measures taken to filter the data and remove possible outliers? | ||||||||||
| 11. Was loss to follow-up after baseline 20% or less? | NR | NR | NR | NR | NR | |||||
| 12. Are reports of the study free of suggestion of selective outcome reporting? | ||||||||||
| Quality scores | 3 | 5 | 9 | 9 | 9 | 5 | 9 | 5 | 10 | 7 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marques, C.; Barreiros, J.; Cabri, J. What Is the Evidence on Which Physicians Can Rely to Advise Patients When They May Resume Driving after TKA? A Systematic Literature Review. J. Funct. Morphol. Kinesiol. 2018, 3, 8. https://doi.org/10.3390/jfmk3010008
Marques C, Barreiros J, Cabri J. What Is the Evidence on Which Physicians Can Rely to Advise Patients When They May Resume Driving after TKA? A Systematic Literature Review. Journal of Functional Morphology and Kinesiology. 2018; 3(1):8. https://doi.org/10.3390/jfmk3010008
Chicago/Turabian StyleMarques, Carlos, João Barreiros, and Jan Cabri. 2018. "What Is the Evidence on Which Physicians Can Rely to Advise Patients When They May Resume Driving after TKA? A Systematic Literature Review" Journal of Functional Morphology and Kinesiology 3, no. 1: 8. https://doi.org/10.3390/jfmk3010008
APA StyleMarques, C., Barreiros, J., & Cabri, J. (2018). What Is the Evidence on Which Physicians Can Rely to Advise Patients When They May Resume Driving after TKA? A Systematic Literature Review. Journal of Functional Morphology and Kinesiology, 3(1), 8. https://doi.org/10.3390/jfmk3010008






