Abstract
The assessment of balance among athletes is essential for training, prevention and rehabilitation of injuries resulting from postural instability. The purpose of the investigation was to validate the Sway Medical Balance Application (SMBA) against the Biodex Balance System (BBS) during the Balance Error Scoring System (BESS) protocol. One hundred and eighty-four Division-II male and female athletes from different sporting disciplines were evaluated using SMBA and BBS while performing all five testing conditions of the BESS. Pearson’s r correlations were used to determine the relationship between the two systems during each of the five conditions and an overall score. The significant relationship and very high correlation between the two systems validates the SMBA as a valid tool that can be used to assess balance in a time- and cost-effective manner in any setting with ease.
1. Introduction
Human balance is a measure of the postural control system that is responsible for the coordination of postural afferent and efferent impulses, to maintain the body’s center of mass (COM) over the base of support (BOS) [1,2,3,4]. The visual, vestibular, and somatosensory systems, are involved in preparing our movement responses in accordance with the afferent sensory information perceived from the position of the body segments with external objects and the environment [3,4,5]. The integration of these systems results in the central nervous system (CNS) protecting against imbalances through defensive reactions [3,4,6]. It has been reported that balance training for athletes could be beneficial both in the prevention and rehabilitation of musculoskeletal injuries [7,8], and assessments for balance performance is critical in such athletes [9]. However, different types of sports may place different demands on the postural control system [10]. Balance assessments and performance have already been well documented in multiple sporting disciplines such as in football, soccer, volleyball, basketball, gymnastics and track and field athletes [9]. In the sporting world, balance assessments are administered both at the sidelines, in the event of a suspected concussion in contact sports, and in clinical or laboratory settings for assessment and rehabilitation purposes. However, laboratory-based balance assessments involve the use of expensive equipment which is time consuming and difficult to move to the sidelines. Hence, there is a constant need for updated technology for balance assessments that could potentially be used anywhere, at a cost-effective and faster rate.
There have been various tests and measures to quantify balance, ranging from subjective measures such as the Berg Balance Scale and Romberg’s test to more modern and objective measures using dynamic posturography [9]. The Balance Error Scoring System (BESS) is a common clinical assessment that consists of five tests lasting 20 s each, performed on a firm and/or foam surface [11,12,13], used by sports medicine professionals. The BESS scores are subjective measures based on the number of errors across trials. Errors include moving the hands off the hips, stepping, stumbling, falling, lifting the forefoot or heel off the testing surface, or losing position for more than five seconds. This unreliable, subjective scoring system [14,15] has led sports medicine professionals to use an objective assessment tool for the BESS test for more reliability [12]. The Biodex Balance System SD (BBS) can be used to assess an individual’s balance based on their sway and has been shown to be a more reliable assessment tool for the BESS test [12]. Although the BESS test on the BBS is a reliable and valid test to measure balance, the equipment is large and difficult to implement outside of a clinical or laboratory setting. An exercise training smartphone application has been shown to be precise and highly accurate compared to the BBS [16].
An expansion in technology has brought more convenient, relatively inexpensive, and easily administered balance assessment tools that can readily be used with ease. The Sway Medical Balance Application (SMBA) is a concussion management program that can be administered on smartphones and encompasses accelerometers to measure the body’s sway [12,13,17]. Other research has been conducted, testing balance in a single-leg stance condition, with both devices [12], but not using all five conditions of the BESS test. There is currently no research on the validity of the SMBA with the BBS in athletes in all five BESS test conditions. This advancement has the ability to administer balance tests to identify any postural instability issues and potentially serve as a time- and cost-effective alternative to other balance assessments. Moreover, the literature on balance performance among different athletes that is sport-specific is constantly growing with the use of different tests, measures and tools. Subsequently, there is a constant need to develop and test different postural control and stability assessments conveniently among these different athletic populations. Therefore, the purpose of this research study was to investigate the validity of the SMBA compared to the BBS during the BESS in collegiate athletes from different sports disciplines.
2. Materials and Methods
2.1. Participants
One hundred and eighty-four Division-II male and female athletes (age 20.07 ± 1.67 years, height 175.54 ± 11.94 cm, weight 75.24 ± 14.20 kg) volunteered to complete a single testing session. Participating teams included collegiate women’s soccer, men’s soccer, women’s basketball, men’s basketball, women’s volleyball, softball, and baseball. Participants completed an Institutional Review Board (IRB) approved informed consent describing the protocol and a Physical Activity Readiness Questionnaire (PARQ). Athletes were healthy and had no history of any neurological or musculoskeletal disorder or a concussion.
2.2. Instrumentation
Balance measures were assessed with Sway Medical’s Concussion Management System Application (Sway Medical, Tulsa, OK, USA, version used) an application software that uses tri-axial accelerometers within the iOS mobile device to calculate postural sway during BESS. For the purposes of the study, SMBA was used on an iPhone fourth generation (Apple Inc., Cupertino, CA, USA). The system calculated a score on a scale from 0 to 100 where 100 meant completely stable and 0 meant completely unstable based on postural sway. The BioDex Balance System SD (Balance System™ SD, Shirley, NY, USA) platform was set to a static horizontal level and was able to record postural sway by generating an Anterior-Posterior Stability Index (APSI). The APSI calculates a score where zero represents complete stability; whereas the larger the deviation from zero translates into a larger amount of instability and postural sway. The BBS was programmed with the identical BESS concussion management protocol as the SMBA and used simultaneously during the BESS test. The five different stance conditions performed during the BESS test were double-leg (DL), tandem-left (TL), tandem right (TR), single-leg right (SLR), and single-leg left (SLL). Each condition was held with eyes closed for 10 s followed by a 10 s break where participants rested and transitioned into the next condition.
2.3. Procedures
All participants completed one testing session that included a familiarization and a testing condition for BESS test, using both the BBS and SMBA devices simultaneously (Figure 1). Anthropometrics were measured and all participants were familiarized with the BESS test by instruction and allowed to practice each of the five different stance conditions. Once the participants were comfortable with the protocol, the two pieces of equipment were incorporated in the testing phase. Since the SMBA and the BBS were programmed with identical BESS protocols, both pieces of equipment were used simultaneously. The iOS mobile device was secured to the chest harness permitting hands free testing. To ensure simultaneous testing, the start buttons on both pieces of equipment were pressed at the same time. One successful trial of the BESS protocol was completed for each subject. A trial was deemed successful if the subject did not have to take a step or hold onto the hand rails. If participants touched the safety rails or had adjusted foot placements, participants had to restart the testing protocol.
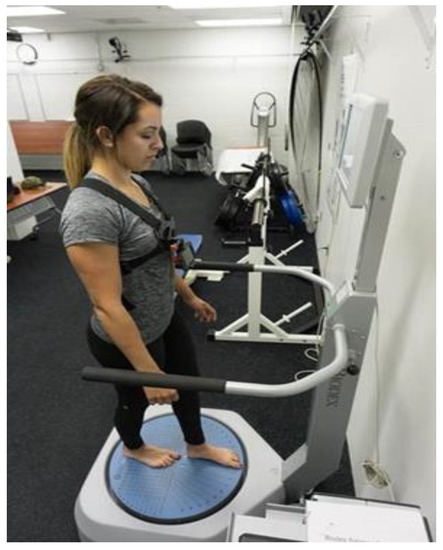
Figure 1.
Demonstration of using the Biodex Balance System SD while simultaneously using the Sway Medical Application on the iPod device during the Balance Error Scoring System test.
2.4. Statistical Analysis
Pearson’s r correlations were used to determine the relationship between the BBS and SMBA during each of the five conditions and an overall score. Correlational strengths were based on the following ranges: 0.0–0.1 is trivial or very small; 0.1–0.3 is small, low, or minor; 0.3–0.5 is moderate or medium; 0.5–0.7 is large, high, or major; 0.7–0.9 is very large or very high; and 0.9–1.0 is nearly perfect to perfect [18,19]. All raw values were converted into standardized z-scores due to the different scoring systems. Six paired-sample t-tests were conducted to compare mean differences between the standard scores of each device. Statistical significance was set a priori with a α level of p < 0.05 and all analyses were conducted using Statistical Package for the Social Sciences (SPSS) IBM 22.
3. Results
There were significant, moderate, and negative correlations for DL (p < 0.001, r = −0.32, R2 = 0.10) and TL (p ≤ 0.001, r = −0.32, R2 = 0.10). There was no significant correlation (p = 0.08, r = −0.13, R2 = 0.01) for TR. There were significant, high, and negative correlations for SLR (p < 0.001, r = −0.64, R2 = 0.41) and SLL (p ≤ 0.001, r = −0.70, R2 = 0.50) (Table 1). The overall score incorporating all five stance conditions showed a significant, high, and negative correlation (p < 0.001, r = −0.70, R2 = 0.50) (Figure 2). The SMBA was also validated through the analysis of z-scores showing no significant (p = 1.0) statistical differences for all five stance conditions and the overall score between the two systems (Table 1).

Table 1.
BESS (Balance Error Scoring System) Scores for each device.
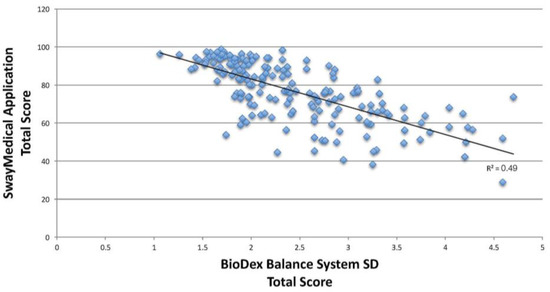
Figure 2.
Pearson’s r correlation, comparing the relationship during the Balance Error Scoring System overall scores between the BioDex Balance System SD and the Sway Medical Application. The overall score incorporating all five stance conditions showed a significant, high, and negative correlation (p < 0.001, r = −0.70).
4. Discussion
The purpose of the study was to investigate the validity of the SMBA smartphone application compared to the BBS during all five testing conditions of the BESS. Our primary findings demonstrate that the SMBA is a valid measure when assessing balance in reference to the BBS in healthy collegiate Division-II athletes. The BBS technology has been commonly used in administering the BESS test in recent years. The current investigation's significant relationship and very high correlation between the two systems validates the SMBA as a valid tool that can be used by practitioners and clinicians to assess balance and postural stability among different athletic populations. To our knowledge, the current investigation is the first to investigate the validation of all five BESS test conditions with the BBS and SMBA, especially with limited literature on using the SMBA device in baseline balance testing. The results from the current study indicate that the SMBA could be used a valid balance assessment tool that is both time- and cost-effective, with easy administration and analysis of the assessment.
In the current investigation, significant correlations were found in both left and right single-leg stance conditions. These findings are supported by previous research where a pilot study was conducted using two of the five BESS test conditions in the SMBA and BBS and it found that the single-leg conditions had significant correlations and no significant differences between devices [13]. However, we found no significant correlation for the tandem right stance condition between the two scoring systems, which is an unexpected result due to previous research showing a strong, inverse correlation between the subjective-practitioner scoring of the BESS test in comparison to the SMBA on a firm and foam surface for three stance conditions including the TR (Tandem Right) stance [12]. However, the current study did not use a subjective scoring system for the BESS, which may have resulted in the difference. Another consideration is the participant populations. Previous studies using the SMBA assessed a healthy college age population [11,12], whereas the current investigation assessed collegiate athletes, which may be a factor in the findings.
One of the critical injuries in athletes, especially in contact sports, is concussion, which negatively impacts the postural control system and ultimately the athletes’ postural stability. Concussion occurs from forces applied to the skull that result in an injury to the brain that can lead to impairments of its neurological functions, including cognitive, mechanical, vision, consciousness, and equilibrium [20,21,22,23,24], which could be either be temporary or permanent [25,26]. It is generally agreed that a comprehensive battery of neurological function and clinical balance tests needs to be administered to assess, diagnose and predict the prognosis of a concussed athlete [27]. One of the many ways to assess an athlete’s return to play following a concussion is to assess their mechanical impairments, which includes motor control and postural stability issues [24,28,29]. The measures collected in our study can be used in addition to and in support of the recommended battery of tests already used for concussion management (i.e., the reaction time test, the cognition test, balance assessments) [28], especially in establishing baseline measures. A contributing factor to knowing when an athlete is ready to “return to play” would be when the new set of measures (post-injury), shows no significant difference from the original baseline measures. It was previously established that athletes with an incidence of concussion will require several days of recovery from postural instability [30]. Therefore, the easy, quick and low-cost tool of the SMBA could potentially be used to monitor postural instability, both as a diagnostic tool and to monitor the prognosis at frequent intervals for such athletes.
Sports medicine practitioners should be aware of additional equipment and technology that is more affordable and convenient to use for balance assessments. The result of this study is the beginning of developing reliable and convenient tools for the assessment of biomechanical impairments in balance [17]. One limitation to this study is that our participants were familiarized with the BESS test protocol on the same day as the testing procedures, which may have had an effect on the results. However, since the two devices were measuring postural sway simultaneously, the measures should still be considered valid based on the observed results. Additionally, previous research has shown that the SMBA is a reliable tool and recommends only one familiarization prior to the testing procedures. The results from the study can be generalized to a healthy athletic population, in which balance assessments are vital and the SMBA can be used as valid tool for such assessments. However, more research should be performed with different populations such the concussed, diseased, and elderly, as well as among different age groups and genders, to validate the SMBA for the general population. Future research should also focus on comparing the two devices in other contact sports and at different performance levels that have high concussion rates such as football, hockey, boxing, etc.
5. Conclusions
In today’s society, electronic devices are widely used, and the SMBA is easily accessible, simple to administer in any setting, and an affordable tool for balance and postural stability assessments, especially using the BESS protocol. The results from the study demonstrate that the SMBA could be used as a valid measure during BESS in healthy collegiate Division-II athletes.
Author Contributions
Nicole C. Dabbs conceived and designed the experiments; Nicole C. Dabbs and Nicole M. Sauls performed the experiments; Nicole C. Dabbs and Nicole M. Sauls analyzed the data; Alice Zayer and Harish Chander contributed reagents/materials/analysis tools; Nicole C. Dabbs, Nicole M. Sauls, Alice Zayer, and Harish Chander wrote the paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Pai, Y.-C.; Patton, J. Center of mass velocity-position predictions for balance control. J. Biomech. 1997, 30, 347–354. [Google Scholar] [CrossRef]
- Manchester, D.; Woollacott, M.; Zederbauer-Hylton, N.; Marin, O.V. Vestibular and Somatosensory Contributions to Balance Control in the Older Adult. J. Gerontol. 1989, 44, M118–M127. [Google Scholar] [CrossRef] [PubMed]
- Winter, D.A. Human balance and posture control during standing and walking. Gait Post. 1995, 3, 193–214. [Google Scholar] [CrossRef]
- Horak, F.B.; Nashner, L.M.; Diener, H.C. Postural strategies associated with somatosensory and vestibular loss. Exp. Brain Res. 1990, 82, 167–177. [Google Scholar] [CrossRef] [PubMed]
- Aartolahti, E.; Häkkinen, A.; Lönnroos, E.; Kautiainen, H.; Sulkava, R.; Hartikainen, S. Relationship between functional vision and balance and mobility performance in community-dwelling older adults. Aging Clin. Exp. Res. 2013, 25, 545–552. [Google Scholar] [CrossRef] [PubMed]
- Susco, T.M.; Valovich McLeod, T.C.; Gansneder, B.M.; Shultz, S.J. Balance recovers within 20 minutes after exertion as measured by the balance error scoring system—proquest. J. Athl. Train. 2004, 39, 241–246. [Google Scholar] [PubMed]
- Freeman, M.A.R. Instability of the foot after injuries to the lateral ligament of the ankle. J. Bone Joint Surg. Br. 1965, 47, 669–677. [Google Scholar] [PubMed]
- Rasool, J.; George, K. The impact of single-leg dynamic balance training on dynamic stability. Phys. Ther. Sport 2007, 8, 177–184. [Google Scholar] [CrossRef]
- Chander, H.; Dabbs, N.C. Balance performance and training among female athletes. J. Strength Cond. Res. 2016, 38, 8–13. [Google Scholar] [CrossRef]
- Chander, H.; MacDonald, C.J.; Dabbs, N.C.; Allen, C.R.; Lamont, H.S.; Garner, J.C. Balance Performance in female collegiate athletes. J. Sports Sci. 2014, 2, 13–20. [Google Scholar]
- Onate, J.A.; Beck, B.C.; Van Lunen, B.L. On-field testing environment and balance error scoring system performance during preseason screening of healthy collegiate baseball players. J. Athl. Train. 2007, 42, 446–451. [Google Scholar] [PubMed]
- Patterson, J.A.; Amick, R.Z.; Pandya, P.D.; Hakansson, N.; Jorgensen, M.J. Comparison of a mobile technology application with the balance error scoring system. Int. J. Athl. Ther. Train. 2014, 10, 4–7. [Google Scholar] [CrossRef]
- Patterson, J.A.; Amick, R.Z.; Thummar, T.; Rogers, M.E. Validation of measures from the smartphone sway balance application: A pilot study. Int. J. Sports Physcial Ther. 2014, 9, 135–139. [Google Scholar]
- Finnoff, J.T.; Peterson, V.J.; Hollman, J.H.; Smith, J. Intrarater and interrater reliability of the balance error scoring system (bess). PM&R 2009, 1, 50–54. [Google Scholar] [CrossRef]
- Chang, J.O.; Levy, S.S.; Seay, S.W.; Goble, D.J. An alternative to the balance error scoring system: Using a low-cost balance board to improve the validity/reliability of sports-related concussion balance testing. Clin. J. Sport Med. 2014, 24, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Bittel, A.J.; Elazzazi, A.; Bittel, D.C. Accuracy and precision of an accelerometer-based smartphone app designed to monitor and record angular movement over time. Telemed. E-Health 2015, 22, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Amick, R.Z.; Chaparro, A.; Patterson, J.A.; Jorgensen, M.J. Test-retest reliability of the sway balance mobile application. J. Mob. Technol. Med. 2015, 4, 40–47. [Google Scholar] [CrossRef]
- Hopkins, W.; Burke, L. Design and analysis of research on sport performance enhancement. Med. Sci. Sports Exerc. 1999, 31, 472–485. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, W. Measures of Reliability in Sports Medicine and Science. Sports Med. 2000, 30, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Collins, M.W.; Lovell, M.R.; Iverson, G.L.; Cantu, R.C.; Maroon, J.C.; Field, M. Cumulative effects of concussion in high school athletes. J. Neurosurg. 2002, 51, 1175–1181. [Google Scholar] [CrossRef]
- Majerske, C.W.; Mihalik, J.P.; Ren, D.; Collins, M.W.; Reddy, C.C.; Lovell, M.R.; Wagner, A.K. Concussion in sports: Postconcussive activity levels, symptoms, and neurocognitive performance. J. Athl. Train. 2008, 43, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Fazio, V.C.; Lovell, M.R.; Pardini, J.E.; Collins, M.W. The relation between post concussion symptoms and neurocognitive performance in concussed athletes. J. Neuorehab. 2007, 22, 207–216. [Google Scholar]
- Wasserman, E.B.; Kerr, Z.Y.; Zuckerman, S.L.; Covassin, T. Epidemiology of sports-related concussions in national collegiate athletic association athletes from 2009–2010 to 2013–2014 symptom prevalence, symptom resolution time, and return-to-play time. Am. J. Sports Med. 2015. [Google Scholar] [CrossRef]
- Register-Mihalik, J.K.; Mihalik, J.P. Guskiewcz balance deficits after sports-related concussions in individuals reporting posttraumatic headache. J. Neurosurg. 2008, 63, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Guskiewicz, K.M.; Marshall, S.W.; Bailes, J.; McCrea, M.; Cantu, R.C.; Randolph, C.; Jordan, B.D. Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery 2005, 719–726. [Google Scholar] [CrossRef]
- Guskiewicz, K.; Marshall, S.; Bailes, J.; McCrea, M.; Harding, H.; Matthews, A.; Mihalik, J.; Cantu, R. Recurrent concussion and risk of depression in retired professional football players. Med. Sci. Sports Exerc. 2007, 39, 903–909. [Google Scholar] [CrossRef] [PubMed]
- Guskiewicz, K.M. Balance assessment in the management of sport-related concussion. Clin. Sports Med. 2011, 30, 89–102. [Google Scholar] [CrossRef] [PubMed]
- Broglio, S.P.; Cantu, R.C.; Gioia, G.A.; Guskiewcz, K.M.; Kutcher, J.; Palm, M.; Valovich McLeod, T.C. National athletic trainers’ association position statement: management of sport concussion. J. Athl. Train. 2014, 49, 245–265. [Google Scholar] [CrossRef] [PubMed]
- Mulligan, I.; Boland, M.; Payette, J. Prevalence of neurocognitive and balance deficits in collegiate football players without clinically diagnosed concussion. J. Orthop. Sports Phys. Ther. 2012, 42, 625–632. [Google Scholar] [CrossRef] [PubMed]
- McCrea, M.; Guskiewicz, K.M.; Marshall, S.W.; Barr, W.; Randolph, C.; Cantu, R.C.; Onate, J.A.; Yang, J.; Kelly, J.P. Acute effects and recovery time following concussion in collegiate football players: the NCAA concussion study. JAMA 2003, 290, 2556–2563. [Google Scholar] [CrossRef] [PubMed]
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).