Investigating the Role of Exercise in Improving Bone Health Among Elderly Women with Osteopenia
Abstract
1. Introduction
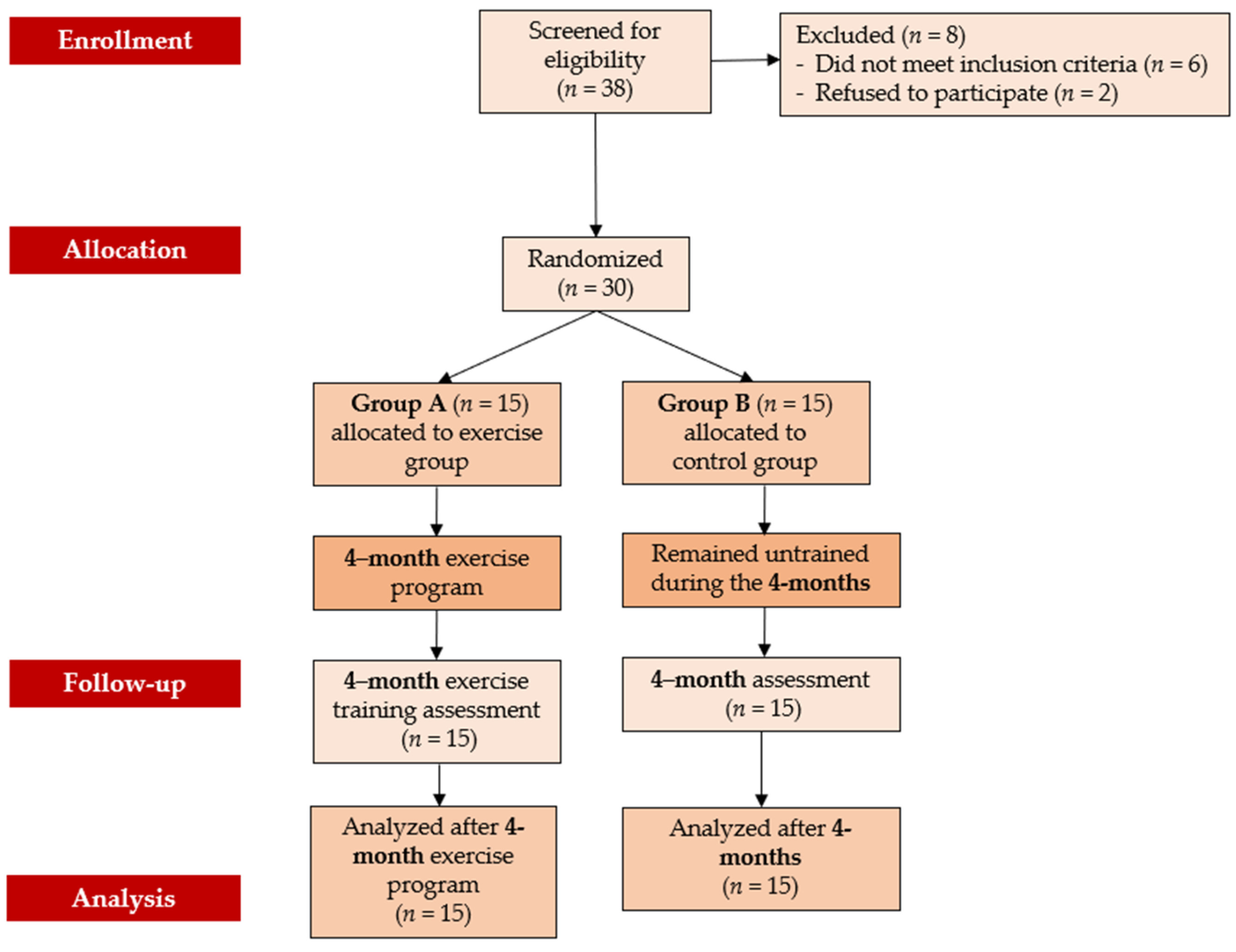
2. Materials and Methods
2.1. Participants
2.2. Sample Size Estimation
2.3. Study Design
2.4. Functional Capacity, Balance and Fall Frequency Measurements
2.5. Biochemical Markers of Bone Metabolism Assessment
2.6. Dual-Energy X-Ray Absorptiometry (DEXA)
2.7. Exercise Program
2.8. Statistical Analysis
3. Results
3.1. Participants’ Characteristics
3.2. Functional Capacity, Balance and Fall Frequency Analysis
3.3. Biochemical Markers of Bone Metabolism Analysis
3.4. DEXA Measurements
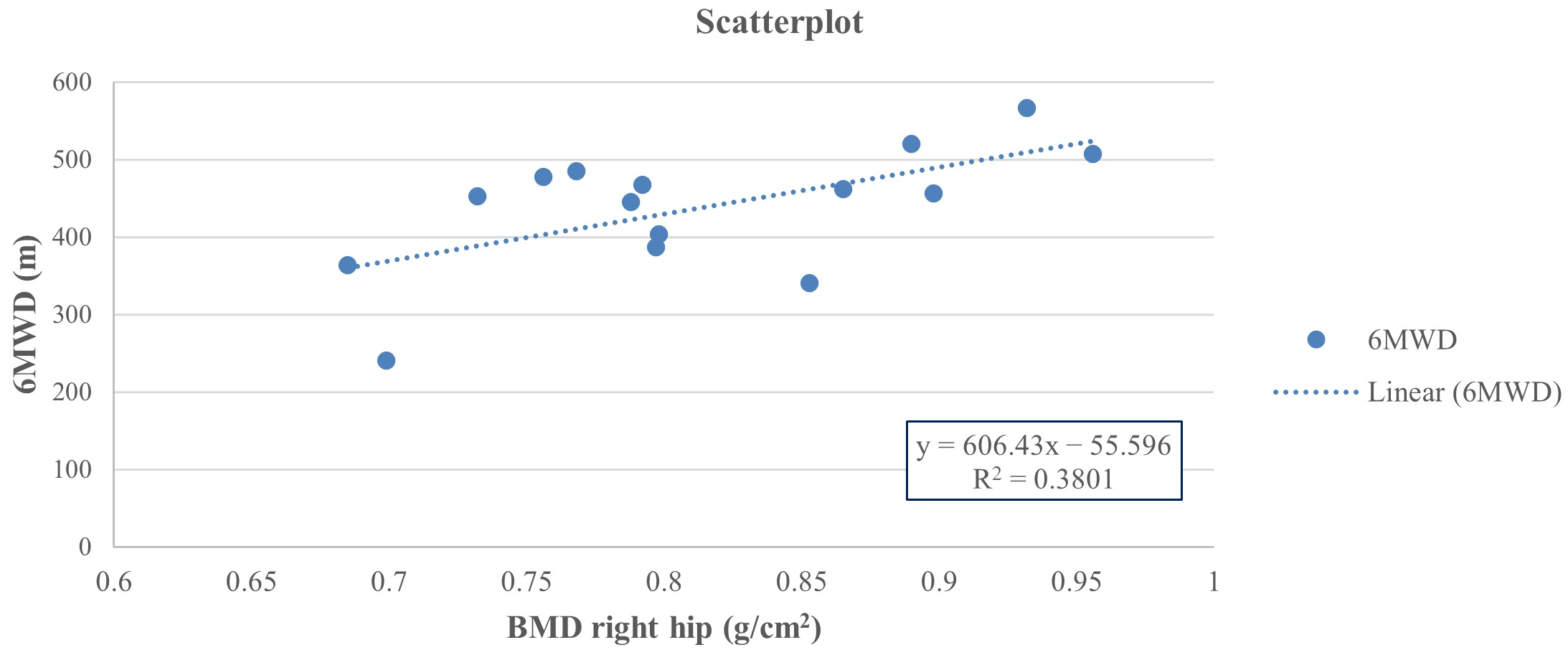
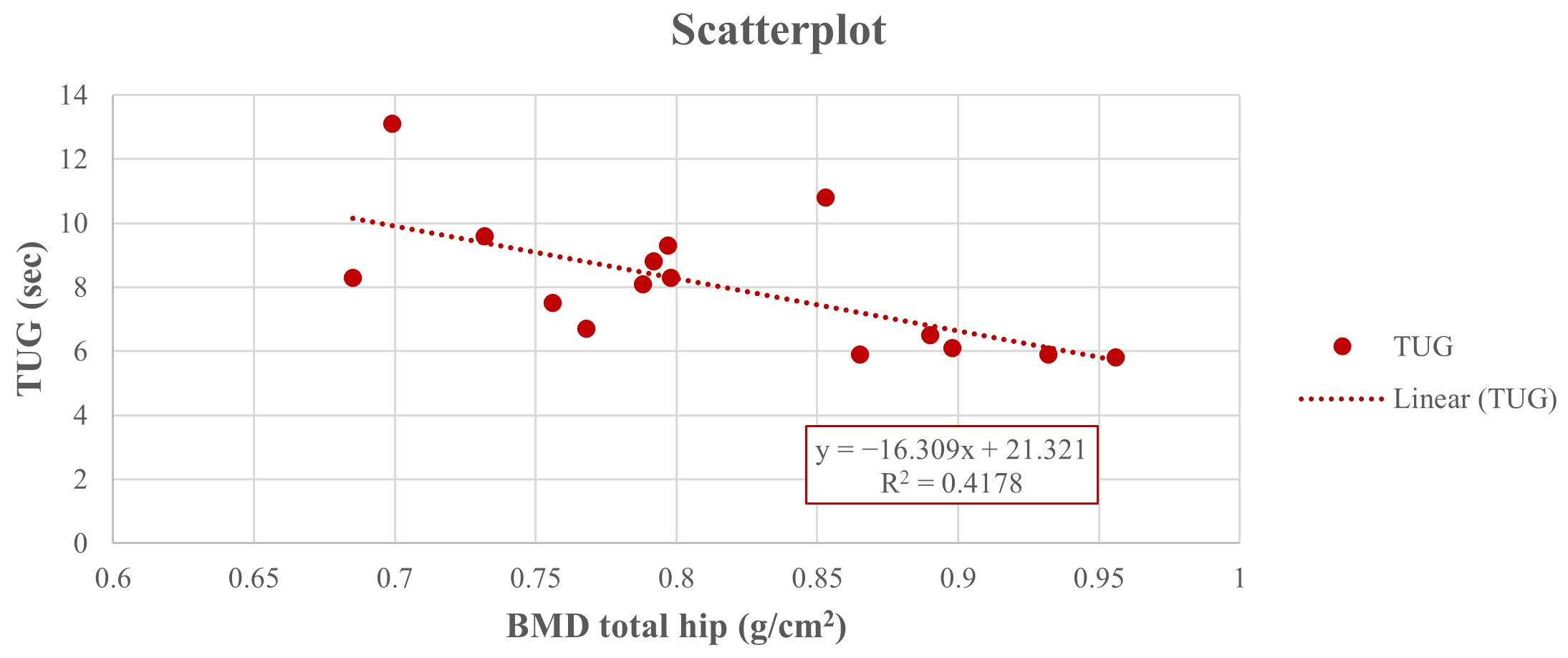
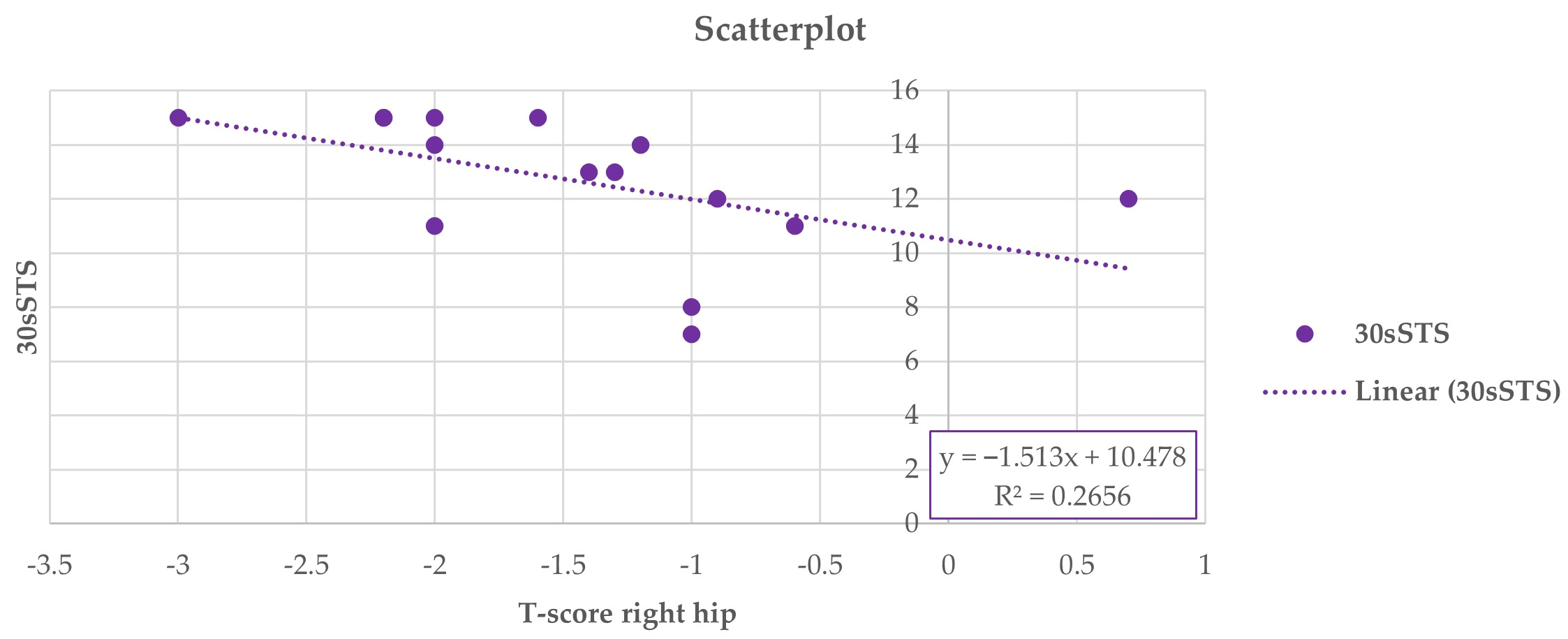
3.5. Associations Between DEXA Results and Functional Performance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhang, J.; Morgan, S.L.; Saag, K.G. Osteopenia: Debates and Dilemmas. Curr. Rheumatol. Rep. 2013, 15, 384. [Google Scholar] [CrossRef]
- World Health Organization. Guidelines for Preclinical Evaluation and Clinical Trials in Osteoporosis. 1998. Available online: https://iris.who.int/bitstream/handle/10665/42088/9241545224_eng.pdf (accessed on 16 November 2025).
- Cosman, F.; de Beur, S.J.; LeBoff, M.S.; Lewiecki, E.M.; Tanner, B.; Randall, S.; Lindsay, R. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos. Int. 2014, 25, 2359–2381, Erratum in Osteoporos. Int. 2015, 26, 2045–2047. [Google Scholar] [CrossRef]
- Linhares, D.G.; Borba-Pinheiro, C.J.; Castro, J.B.P.d.; Santos, A.O.B.d.; Santos, L.L.d.; Cordeiro, L.d.S.; Drigo, A.J.; Nunes, R.d.A.M.; Vale, R.G.d.S. Effects of Multicomponent Exercise Training on the Health of Older Women with Osteoporosis: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 14195. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.-M.; Bisignano, C.; James, S.L.; Abady, G.G.; Abedi, A.; Abu-Gharbieh, E.; Alhassan, R.K.; Alipour, V.; Arabloo, J.; Asaad, M.; et al. Global, regional, and national burden of bone fractures in 204 countries and territories, 1990–2019: A systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Longev. 2021, 2, e580–e592. [Google Scholar] [CrossRef]
- Morin, S.N.; Leslie, W.D.; Schousboe, J.T. Osteoporosis. JAMA 2025, 334, 894. [Google Scholar] [CrossRef]
- Abrahamsen, B.; van Staa, T.; Ariely, R.; Olson, M.; Cooper, C. Excess mortality following hip fracture: A systematic epidemiological review. Osteoporos. Int. 2009, 20, 1633–1650. [Google Scholar] [CrossRef]
- Cheraghi, Z.; Doosti-Irani, A.; Almasi-Hashiani, A.; Baigi, V.; Mansournia, N.; Etminan, M.; Mansournia, M.A. The effect of alcohol on osteoporosis: A systematic review and meta-analysis. Drug Alcohol Depend. 2019, 197, 197–202. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, Y.; Huang, Y.; Le, S.; Jiang, H.; Ruan, B.; Ao, X.; Shi, X.; Fu, X.; Wang, S. The effect of overweight or obesity on osteoporosis: A systematic review and meta-analysis. Clin. Nutr. 2023, 42, 2457–2467. [Google Scholar] [CrossRef]
- Baheiraei, A.; Pocock, N.A.; Eisman, J.A.; Nguyen, N.D.; Nguyen, T.V. Bone mineral density, body mass index and cigarette smoking among Iranian women: Implications for prevention. BMC Musculoskelet. Disord. 2005, 6, 34. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, W.K.; Silverstein, M.; Wong, J.B.; Barry, M.J.; Chelmow, D.; Coker, T.R.; Davis, E.M.; Jaén, C.R.; Krousel-Wood, M.; Lee, S.; et al. Interventions to Prevent Falls in Community-Dwelling Older Adults. JAMA 2024, 332, 51. [Google Scholar] [CrossRef] [PubMed]
- Montero-Odasso, M.; van der Velde, N.; Martin, F.C.; Petrovic, M.; Tan, M.P.; Ryg, J.; Aguilar-Navarro, S.; Alexander, N.B.; Becker, C.; Blain, H.; et al. World guidelines for falls prevention and management for older adults: A global initiative. Age Ageing 2022, 51, afac205, Erratum in Age Ageing 2023, 15, afad188. Erratum in Age Ageing 2023, 52, afad199. [Google Scholar] [CrossRef]
- Yu, P.-A.; Hsu, W.-H.; Hsu, W.-B.; Kuo, L.-T.; Lin, Z.-R.; Shen, W.-J.; Hsu, R.W.-W. The effects of high impact exercise intervention on bone mineral density, physical fitness, and quality of life in postmenopausal women with osteopenia. Medicine 2019, 98, e14898. [Google Scholar] [CrossRef]
- Borba-Pinheiro, C.J.; Dantas, E.H.M.; Vale, R.G.d.S.; Drigo, A.J.; Carvalho, M.C.G.d.A.; Tonini, T.; Meza, E.I.A.; Figueiredo, N.M.A.d. Resistance training programs on bone related variables and functional independence of postmenopausal women in pharmacological treatment: A randomized controlled trial. Arch. Gerontol. Geriatr. 2016, 65, 36–44. [Google Scholar] [CrossRef]
- Watson, S.L.; Weeks, B.K.; Weis, L.J.; Harding, A.T.; Horan, S.A.; Beck, B.R. High-Intensity Resistance and Impact Training Improves Bone Mineral Density and Physical Function in Postmenopausal Women with Osteopenia and Osteoporosis: The LIFTMOR Randomized Controlled Trial. J. Bone Miner. Res. 2018, 33, 211–220, Erratum in J. Bone Miner. Res. 2019, 34, 572. [Google Scholar] [CrossRef]
- Sobrinho, A.C.d.S.; Almeida, M.L.d.; Rodrigues, G.d.S.; Bertani, R.F.; Lima, J.G.R.; Bueno Junior, C.R. Stretching and Multicomponent Training to Functional Capacities of Older Women: A Randomized Study. Int. J. Environ. Res. Public Health 2021, 19, 27. [Google Scholar] [CrossRef] [PubMed]
- Sobrinho, A.C.d.S.; Almeida, M.L.d.; Rodrigues, G.d.S.; Finzeto, L.C.; Silva, V.R.R.; Bernatti, R.F.; Bueno Junior, C.R. Effect of Flexibility Training Associated with Multicomponent Training on Posture and Quality of Movement in Physically Inactive Older Women: A Randomized Study. Int. J. Environ. Res. Public Health 2021, 18, 10709. [Google Scholar] [CrossRef]
- Moreira, N.B.; Rodacki, A.L.F.; Costa, S.N.; Pitta, A.; Bento, P.C.B. Perceptive–Cognitive and Physical Function in Prefrail Older Adults: Exergaming Versus Traditional Multicomponent Training. Rejuvenation Res. 2021, 24, 28–36. [Google Scholar] [CrossRef]
- Kistler-Fischbacher, M.; Armbrecht, G.; Gängler, S.; Theiler, R.; Rizzoli, R.; Dawson-Hughes, B.; Kanis, J.A.; Hofbauer, L.C.; Schimmer, R.C.; Vellas, B.; et al. Effects of vitamin D3, omega-3s, and a simple strength training exercise program on bone health: The DO-HEALTH randomized controlled trial. J. Bone Miner. Res. 2024, 39, 661–671. [Google Scholar] [CrossRef]
- Yilmaz, N.; Kösehasanoğulları, M. The effectiveness of virtual reality exercise games on balance functions and fear of falling in women with osteoporosis. Rheumatol. Int. 2024, 44, 1071–1076. [Google Scholar] [CrossRef]
- Gilani, M.; Torkaman, G.; Bahrami, F.; Bayat, N. Virtual Reality Exergaming Capability to Change Muscle Strategy During the Limits of Stability Test and Reduce Fear of Falling in Primary Osteoporotic Women. Games Health J. 2023, 12, 310–322. [Google Scholar] [CrossRef] [PubMed]
- Canzone, A.; Belmonte, G.; Patti, A.; Vicari, D.S.S.; Rapisarda, F.; Giustino, V.; Drid, P.; Bianco, A. The multiple uses of artificial intelligence in exercise programs: A narrative review. Front. Public Health 2025, 13, 1510801. [Google Scholar] [CrossRef]
- Greco, G.; Poli, L.; Gabriele, M.; Aidar, F.J.; Fischetti, F.; Patti, A.; Cataldi, S. Effectiveness of a 5-week virtual reality versus traditional training on balance and flexibility in healthy adult females. Sport Sci. Health 2025, 21, 289–300. [Google Scholar] [CrossRef]
- Li, S.; Li, Y.; Liang, Q.; Yang, W.-J.; Zi, R.; Wu, X.; Du, C.; Jiang, Y. Effects of tele-exercise rehabilitation intervention on women at high risk of osteoporotic fractures: Study protocol for a randomised controlled trial. BMJ Open 2022, 12, e064328. [Google Scholar] [CrossRef]
- Zhang, S.; Huang, X.; Zhao, X.; Li, B.; Cai, Y.; Liang, X.; Wan, Q. Effect of exercise on bone mineral density among patients with osteoporosis and osteopenia: A systematic review and network meta-analysis. J. Clin. Nurs. 2022, 31, 2100–2111. [Google Scholar] [CrossRef]
- de Oliveira, L.C.; de Oliveira, R.G.; de Almeida Pires-Oliveira, D.A. Effects of Whole-Body Vibration Versus Pilates Exercise on Bone Mineral Density in Postmenopausal Women: A Randomized and Controlled Clinical Trial. J. Geriatr. Phys. Ther. 2019, 42, E23–E31. [Google Scholar] [CrossRef]
- Harada, N.D.; Chiu, V.; Stewart, A.L. Mobility-related function in older adults: Assessment with a 6-minute walk test. Arch. Phys. Med. Rehabil. 1999, 80, 837–841. [Google Scholar] [CrossRef]
- AL-Ghamdi, N.S.; Shaheen, A.A.M. Reference values and regression equations for predicting the 6-minute walk distance in Saudi adults aged 50–80 years: A cross-sectional study. J. Back. Musculoskelet. Rehabil. 2021, 34, 783–793. [Google Scholar] [CrossRef]
- CDC’s STEADI Tools. Assessment with 30-Second Chair Stand. 2017. Available online: https://www.cdc.gov/steadi/media/pdfs/STEADI-Assessment-30Sec-508.pdf (accessed on 17 October 2025).
- Mahato, N.K.; Davis, A. Relationship between sit-to-stand movements and physical function in healthy older adults: Testing duration power and displacement velocities for A 30-second chair-rise test. J. Bodyw. Mov. Ther. 2025, 42, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Rose, D.J.; Jones, C.J.; Lucchese, N. Predicting the Probability of Falls in Community-Residing Older Adults Using the 8-Foot Up-and-Go: A New Measure of Functional Mobility. J. Aging Phys. Act. 2002, 10, 466–475. [Google Scholar] [CrossRef]
- Gadelha, A.B.; Neri, S.G.R.; Oliveira, R.J.d.; Bottaro, M.; David, A.C.d.; Vainshelboim, B.; Lima, R.M. Severity of sarcopenia is associated with postural balance and risk of falls in community-dwelling older women. Exp. Aging Res. 2018, 44, 258–269. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.J.; Rikli, R.E. Measuring functional fitness in older adults. J. Act. Aging 2002, 2, 25–30. [Google Scholar]
- Rikli, R.E.; Jones, C.J. Development and Validation of a Functional Fitness Test for Community-Residing Older Adults. J. Aging Phys. Act. 1999, 7, 129–161. [Google Scholar] [CrossRef]
- Berg, K.O.; Wood-Dauphinee, S.L.; Williams, J.I.; Maki, B. Measuring balance in the elderly: Validation of an instrument. Can. J. Public Health 1992, 83 (Suppl. 2), S7–S11. [Google Scholar] [PubMed]
- World Health Organization. WHO Study Group on Assessment of Fracture Risk and its Application to Screening for Postmenopausal Osteoporosis. Osteoporos. Int. 1994, 4, 368–381. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Zhang, C.; Zeng, Q.; Li, R.; Liu, L.; Hao, Q.; Shi, C.; Zhang, X.; Yan, Y. Mechanical strain promotes osteoblast ECM formation and improves its osteoinductive potential. Biomed. Eng. Online 2012, 11, 80. [Google Scholar] [CrossRef] [PubMed]
- Rossini, M.; Adami, S.; Bertoldo, F.; Diacinti, D.; Gatti, D.; Giannini, S.; Giusti, A.; Malavolta, N.; Minisola, S.; Osella, G.; et al. Guidelines for the diagnosis, prevention and management of osteoporosis. Reumatismo 2016, 68, 1–39. [Google Scholar] [CrossRef]
- Benedetti, M.G.; Furlini, G.; Zati, A.; Letizia Mauro, G. The Effectiveness of Physical Exercise on Bone Density in Osteoporotic Patients. BioMed Res. Int. 2018, 2018, 4840531. [Google Scholar] [CrossRef]
- Daly, R.M.; Dalla Via, J.; Duckham, R.L.; Fraser, S.F.; Helge, E.W. Exercise for the prevention of osteoporosis in postmenopausal women: An evidence-based guide to the optimal prescription. Braz. J. Phys. Ther. 2019, 23, 170–180. [Google Scholar] [CrossRef]
- Gómez-Cabello, A.; Ara, I.; González-Agüero, A.; Casajús, J.A.; Vicente-Rodríguez, G. Effects of Training on Bone Mass in Older Adults. Sports Med. 2012, 42, 301–325. [Google Scholar] [CrossRef]
- Kemmler, W.; Shojaa, M.; Kohl, M.; von Stengel, S. Effects of Different Types of Exercise on Bone Mineral Density in Postmenopausal Women: A Systematic Review and Meta-analysis. Calcif. Tissue Int. 2020, 107, 409–439. [Google Scholar] [CrossRef]
- Varahra, A.; Rodrigues, I.B.; MacDermid, J.C.; Bryant, D.; Birmingham, T. Exercise to improve functional outcomes in persons with osteoporosis: A systematic review and meta-analysis. Osteoporos. Int. 2018, 29, 265–286. [Google Scholar] [CrossRef]
- Alnasser, S.M.; Babakair, R.A.; Al Mukhlid, A.F.; Al Hassan, S.S.S.; Nuhmani, S.; Muaidi, Q. Effectiveness of Exercise Loading on Bone Mineral Density and Quality of Life Among People Diagnosed with Osteoporosis, Osteopenia, and at Risk of Osteoporosis—A Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 4109. [Google Scholar] [CrossRef]
- Turner, C.H.; Robling, A.G. Mechanisms by which exercise improves bone strength. J. Bone Miner. Metab. 2005, 23, 16–22. [Google Scholar] [CrossRef]
- Haque, I.; Schlacht, T.Z.; Skelton, D.A. The effects of high velocity resistance training on bone mineral density in older adults: A systematic review. Bone 2024, 179, 116986. [Google Scholar] [CrossRef]
- Karlamangla, A.S.; Burnett-Bowie, S.A.M.; Crandall, C.J. Bone Health During the Menopause Transition and Beyond. Obs. Gynecol. Clin. N. Am. 2018, 45, 695–708. [Google Scholar] [CrossRef]
- Black, D.M.; Cauley, J.A.; Wagman, R.; Ensrud, K.; Fink, H.A.; Hillier, T.A.; Lui, L.-Y.; Cummings, S.R.; Schousboe, J.T.; Napoli, N. The Ability of a Single BMD and Fracture History Assessment to Predict Fracture Over 25 Years in Postmenopausal Women: The Study of Osteoporotic Fractures. J. Bone Miner. Res. 2018, 33, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Panahi, N.; Saeedi Moghaddam, S.; Fahimfar, N.; Rezaei, N.; Sanjari, M.; Rashidi, M.M.; Shobeiri, P.; Larijani, B.; Ostovar, A. Trend in global burden attributable to low bone mineral density in different WHO regions: 2000 and beyond, results from the Global Burden of Disease (GBD) study 2019. Endocr. Connect. 2023, 12, e230160. [Google Scholar] [CrossRef] [PubMed]
- Kanis, J.A.; Johnell, O.; Oden, A.; Sernbo, I.; Redlund-Johnell, I.; Dawson, A.; De Laet, C.; Jonsson, B. Long-Term Risk of Osteoporotic Fracture in Malmö. Osteoporos. Int. 2000, 11, 669–674. [Google Scholar] [CrossRef]
- Walker, M.D.; Shane, E. Postmenopausal Osteoporosis. N. Engl. J. Med. 2023, 389, 1979–1991. [Google Scholar] [CrossRef]
- Kumar, S.; Smith, C.; Clifton-Bligh, R.J.; Beck, B.R.; Girgis, C.M. Exercise for Postmenopausal Bone Health—Can We Raise the Bar? Curr. Osteoporos. Rep. 2025, 23, 20. [Google Scholar] [CrossRef]
- Fausto, D.Y.; Martins, J.B.B.; Machado, A.C.; Saraiva, P.S.; Pelegrini, A.; Guimarães, A.C.A. What is the evidence for the effect of physical exercise on bone health in menopausal women? An umbrella systematic review. Climacteric 2023, 26, 550–559. [Google Scholar] [CrossRef]
- Lester, M.E.; Urso, M.L.; Evans, R.K.; Pierce, J.R.; Spiering, B.A.; Maresh, C.M.; Hatfield, D.L.; Kraemer, W.J.; Nindl, B.C. Influence of exercise mode and osteogenic index on bone biomarker responses during short-term physical training. Bone 2009, 45, 768–776. [Google Scholar] [CrossRef]
- Gabr, S.; Al-Ghadir, M.H.; Alghadir, A.; Al-Eisa, E. Correlation between bone mineral density and serum trace elements in response to supervised aerobic training in older adults. Clin. Interv. Aging 2016, 265, 265–273. [Google Scholar] [CrossRef]
- Nikander, R.; Kannus, P.; Dastidar, P.; Hannula, M.; Harrison, L.; Cervinka, T.; Narra, N.G.; Aktour, R.; Arola, T.; Eskola, H.; et al. Targeted exercises against hip fragility. Osteoporos. Int. 2009, 20, 1321–1328. [Google Scholar] [CrossRef]
- Martyn-St James, M.; Carroll, S. A meta-analysis of impact exercise on postmenopausal bone loss: The case for mixed loading exercise programmes. Br. J. Sports Med. 2009, 43, 898–908. [Google Scholar] [CrossRef]
- Kitagawa, T.; Hiraya, K.; Denda, T.; Yamamoto, S. A comparison of different exercise intensities for improving bone mineral density in postmenopausal women with osteoporosis: A systematic review and meta-analysis. Bone Rep. 2022, 17, 101631. [Google Scholar] [CrossRef]
- Hoke, M.; Omar, N.B.; Amburgy, J.W.; Self, D.M.; Schnell, A.; Morgan, S.; Larios, E.A.; Chambers, M.R. Impact of exercise on bone mineral density, fall prevention, and vertebral fragility fractures in postmenopausal osteoporotic women. J. Clin. Neurosci. 2020, 76, 261–263. [Google Scholar] [CrossRef] [PubMed]
- Xiaoya, L.; Junpeng, Z.; Li, X.; Haoyang, Z.; Xueying, F.; Yu, W. Effect of different types of exercise on bone mineral density in postmenopausal women: A systematic review and network meta-analysis. Sci. Rep. 2025, 15, 11740. [Google Scholar] [CrossRef] [PubMed]
- Wen, H.J.; Huang, T.H.; Li, T.L.; Chong, P.N.; Ang, B.S. Effects of short-term step aerobics exercise on bone metabolism and functional fitness in postmenopausal women with low bone mass. Osteoporos. Int. 2017, 28, 539–547. [Google Scholar] [CrossRef]
- Bragonzoni, L.; Barone, G.; Benvenuti, F.; Ripamonti, C.; Lisi, L.; Benedetti, M.G.; Marini, S.; Dallolio, L.; Mai-etta Latessa, P.; Zinno, R.; et al. Influence of Coaching on Effectiveness, Participation, and Safety of an Exercise Program for Postmenopausal Women with Osteoporosis: A Randomized Trial. Clin. Interv. Aging 2023, 18, 143–155. [Google Scholar] [CrossRef] [PubMed]
- Filipović, T.N.; Lazović, M.P.; Backović, A.N.; Filipović, A.N.; Ignjatović, A.M.; Dimitri-Jević, S.S.; Gopčević, K.R. A 12-week exercise program improves functional status in postmenopausal osteoporotic women: Randomized controlled study. Eur. J. Phys. Rehabil. Med. 2021, 57, 120–130. [Google Scholar] [CrossRef]
- Wei, F.; Hu, Z.; He, R.; Wang, Y. Effects of balance training on balance and fall efficacy in patients with Osteoporosis: A systematic review and meta-analysis with trial sequential analysis. J. Rehabil. Med. 2023, 55, jrm00390. [Google Scholar] [CrossRef]
- Otero, M.; Esain, I.; González-Suarez, Á.M.; Gil, S. The effectiveness of a basic exercise intervention to improve strength and balance in women with osteoporosis. Clin. Interv. Aging 2017, 12, 505–513. [Google Scholar] [CrossRef]
- Babiuch, A.S.; Oestervemb, K.; Lipińska, A.; Stańczak, M.L.; Cholewa, M.; Makulec, K.; Nowakowska, K.; Derengowska, M.H. Differences in the level of physical fitness and mobility among older women with osteoporosis and healthy women—Cross-sectional study. Sci. Rep. 2021, 11, 14179. [Google Scholar] [CrossRef]
- Bianco, A.; Patti, A.; Bellafiore, M.; Battaglia, G.; Sahin, F.N.; Paoli, A.; Cataldo, M.C.; Mammina, C.; Palma, A. Group fitness activities for the elderly: An innovative approach to reduce falls and injuries. Aging Clin. Exp. Res. 2014, 26, 147–152. [Google Scholar] [CrossRef]
- Wang, Q.; Jiang, X.; Shen, Y.; Yao, P.; Chen, J.; Zhou, Y.; Gu, Y.; Qian, Z.; Cao, X. Effectiveness of exercise intervention on fall-related fractures in older adults: A systematic review and meta-analysis of randomized controlled trials. BMC Geriatr. 2020, 20, 322. [Google Scholar] [CrossRef]
- Hoffmann, I.; Shojaa, M.; Kohl, M.; von Stengel, S.; Becker, C.; Gosch, M.; Jakob, F.; Kerschan-Schindl, K.; Kladny, B.; Clausen, J.; et al. Exercise Reduces the Number of Overall and Major Osteoporotic Fractures in Adults. Does Supervision Make a Difference? Systematic Review and Meta-Analysis. J. Bone Miner. Res. 2020, 37, 2132–2148. [Google Scholar] [CrossRef]
- Hoffmann, I.; Kohl, M.; von Stengel, S.; Jakob, F.; Kerschan-Schindl, K.; Lange, U.; Peters, S.; Schoene, D.; Sieber, C.; Thomasius, F.; et al. Exercise and the prevention of major osteoporotic fractures in adults: A systematic review and meta-analysis with special emphasis on intensity progression and study duration. Osteoporos. Int. 2023, 34, 15–28. [Google Scholar] [CrossRef]
- Ishikawa, Y.; Miyakoshi, N.; Hongo, M.; Kasukawa, Y.; Kudo, D.; Shimada, Y. Relationships among spinal mobility and sagittal alignment of spine and lower extremity to quality of life and risk of falls. Gait Posture 2017, 53, 98–103. [Google Scholar] [CrossRef]
- Labata-Lezaun, N.; González-Rueda, V.; Llurda-Almuzara, L.; López-de-Celis, C.; Rodríguez-Sanz, J.; Bosch, J.; Vicente-Rodríguez, G.; Gorczakowska, D.; Araluze-Arizti, P.; Pérez-Bellmunt, A. Effectiveness of multicomponent training on physical performance in older adults: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2023, 104, 104838. [Google Scholar] [CrossRef]
- Schneider, A.; Leite, L.B.; Teixeira, J.; Forte, P.; Barbosa, T.M.; Monteiro, A.M. Multicomponent Exercise and Functional Fitness: Strategies for Fall Prevention in Aging Women. Sports 2025, 13, 159. [Google Scholar] [CrossRef]
- Philippe, A.G.; Goncalves, A.; Martinez, C.; Deshayes, M.; Charbonnier, E. Can an Eight-Session Multicomponent Physical Exercise Program Reduce Fall Risk and Fear of Falling among the Elderly? Int. J. Environ. Res. Public Health 2022, 19, 8262. [Google Scholar] [CrossRef]
- Jepsen, D.B.; Thomsen, K.; Hansen, S.; Jørgensen, N.R.; Masud, T.; Ryg, J. Effect of whole-body vibration exercise in preventing falls and fractures: A systematic review and meta-analysis. BMJ Open 2017, 7, e018342. [Google Scholar] [CrossRef]
- Alghadir, A.H.; Gabr, S.A.; Iqbal, A. Concurrent effects of high-intensity interval training and vitamin D supplementation on bone metabolism among women diagnosed with osteoporosis: A randomized controlled trial. BMC Musculoskelet. Disord. 2025, 26, 381. [Google Scholar] [CrossRef]
- Roghani, T.; Torkaman, G.; Movasseghe, S.; Hedayati, M.; Goosheh, B.; Bayat, N. Effects of short-term aerobic exercise with and without external loading on bone metabolism and balance in postmenopausal women with osteoporosis. Rheumatol. Int. 2013, 33, 291–298. [Google Scholar] [CrossRef]
- Tong, X.; Chen, X.; Zhang, S.; Huang, M.; Shen, X.; Xu, J.; Zou, J. The Effect of Exercise on the Prevention of Osteoporosis and Bone Angiogenesis. BioMed Res. Int. 2019, 2019, 8171897. [Google Scholar] [CrossRef]
- McMillan, L.; Zengin, A.; Ebeling, P.; Scott, D. Prescribing Physical Activity for the Prevention and Treatment of Osteoporosis in Older Adults. Healthcare 2017, 5, 85. [Google Scholar] [CrossRef]
- Lindsey, C.; Brownbill, R.A.; Bohannon, R.A.; Ilich, J.Z. Association of Physical Performance Measures with Bone Mineral Density in Postmenopausal Women. Arch. Phys. Med. Rehabil. 2005, 86, 1102–1107. [Google Scholar] [CrossRef]
- Moradell, A.; Gómez-Cabello, A.; Gómez-Bruton, A.; Muniz-Pardos, B.; Puyalto, J.M.; Matute-Llorente, A.; Gónzalez-Agüero, A.; Ara, I.; Casajús, J.A.; Vicente-Rodríguez, G. Associations between Physical Fitness, Bone Mass, and Structure in Older People. BioMed Res. Int. 2020, 2020, 6930682. [Google Scholar] [CrossRef]
- Dai, D.; Xu, F.; Sun, R.; Yuan, L.; Sheng, Z.; Xie, Z. Decreased lower-extremity muscle performance is associated with decreased hip bone mineral density and increased estimated fracture risk in community-dwelling postmenopausal women. Arch. Osteoporos. 2020, 15, 173. [Google Scholar] [CrossRef]
| Group A (nA = 15) | Group B (nB = 15) | A vs. B Group p-Value | |
|---|---|---|---|
| Age (years) | 67.86 ± 5.30 | 66.73 ± 5.18 | p = 0.346 |
| Height (cm) | 158.80 ± 5.95 | 159.10 ± 4.67 | p = 0.445 |
| Weight (kg) | 67.93 ± 13.98 | 69.13 ± 8.32 | p = 0.423 |
| BMI (kg/m2) | 26.98 ± 5.67 | 27.42 ± 4.03 | p = 0.398 |
| Comorbidities (n, %) | |||
| Hypertension | 6 (40.0%) | 5 (33.3%) | p = 0.476 |
| Hyperlipidemia | 4 (26.6%) | 2 (13.3%) | p = 0.290 |
| Group A (nA = 15) | Group B (nB = 15) | Group A vs. B | Analysis of Variance, p Value, ηp2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Change Mean (%), [95% CI: Lower/Higher Bound] | Baseline | Follow-Up | Change Mean (%), [95% CI: Lower/Higher Bound] | Change Mean (%), [95% CI: Lower/Higher Bound] | Group | Time | Group × Time | ||
| Pre | Post | ||||||||||
| 6-MWD (m) | 362.16 ± 61.09 | 437.99 ± 80.94 | +75.83 (20.90%), [95% CI: 60.67, 90.96] | 361.56 ± 70.28 | 361.03 ± 70.44 | −0.53 (−0.15%), [95% CI: −0.95, −0.11] | −0.60 (−0.17%) [95% CI: −47.72, 46.52] | −76.96 (−21.31%) [95% CI: −131.25, −22.66] | F(1,14) = 19.348, p < 0.001 *, ηp2 = 0.580 | F(1,14) = 23.964, p < 0.001 *, ηp2 = 0.628 | F(1,14) = 36.974, p < 0.001 *, ηp2 = 0.701 |
| TUG (s) | 8.81 ± 2.30 | 8.04 ± 2.07 | −0.77 (8.70%), [95% CI: −1.14, −0.37] | 8.78 ± 2.33 | 8.80 ± 2.36 | +0.02 (+0.23%), [95% CI: −0.06, 0.03] | −0.03 (−0.34%) [95% CI: −1.68, 1.62] | +0.76 (+8.64%) [95% CI: −0.82, 2.34] | F(1,14) = 7.488, p = 0.016 *, ηp2 = 0.348 | F(1,14) = 14.025, p = 0.002 *, ηp2 = 0.500 | F(1,14) = 15.727, p = 0.001 *, ηp2 = 0.529 |
| 30 s-STS (number of repetitions) | 10.80 ± 2.67 | 12.66 ± 2.55 | +1.86 (17.20%), [95% CI: 1.32, 2.39] | 10.66 ± 2.25 | 10.53 ± 2.32 | −0.13 (−1.20%), [95% CI: −0.30, 0.04] | −0.14 (−1.31%) [95% CI: −1.90, 1.62] | −2.13 (−20.23%) [95% CI: −3.87, −0.38] | F(1,14) = 17.707, p < 0.001 *, ηp2 = 0.558 | F(1,14) = 37.260, p < 0.001 *, ηp2 = 0.727 | F(1,14) = 46.667, p < 0.001 *, ηp2 = 0.769 |
| 8-FUAG (s) | 8.32 ± 2.11 | 7.76 ± 1.92 | −0.56 (6.70%), %), [95% CI: −0.83, −0.28] | 8.28 ± 2.01 | 8.29 ± 2.03 | +0.01 (+0.12%), [95% CI: −0.02, 0.03] | −0.04 (−0.48%) [95% CI: −1.51, 1.43] | +0.53 (+6.39%) [95% CI: −0.88, 1.94] | F(1,14) = 4.084, p = 0.063, ηp2 = 0.226 | F(1,14) = 14.689, p = 0.002 *, ηp2 = 0.512 | F(1,14) = 15.634, p = 0.001 *, ηp2 = 0.528 |
| BBS score | 51.13 ± 4.68 | 52.46 ± 3.70 | +1.33 (2.60%), [95% CI: 0.62, 2.03] | 50.86 ± 4.62 | 50.82 ± 4.73 | −0.04 (−0.08%), [95% CI: −0.18, 0.06] | −0.27 (−0.53%) [95% CI: −3.59, 3.05] | −1.64 (−3.23%) [95% CI: −4.67, 1.39] | F(1,14) = 19.176, p < 0.001 *, ηp2 = 0.578 | F(1,14) = 13.513, p = 0.002 *, ηp2 = 0.491 | F(1,14) = 13.025, p = 0.003 *, ηp2 = 0.482 |
| Frequency of falls (mean number of falls) | 1.20 ± 1.09 | 0.26 ± 0.19 | −0.94 (78.30%), [95% CI: −1.60, −0.25] | 1.26 ± 1.14 | 1.33 ± 1.28 | +0.07 (+5.60%), [95% CI: −0.06, 0.18] | +0.06 (+4.76%) [95% CI: −0.73, 0.85] | +1.07 (+80.45%) [95% CI: 0.41, 1.72] | F(1,14) = 2.818, p = 0.115, ηp2 = 0.168 | F(1,14) = 6.646, p = 0.022 *, ηp2 = 0.322 | F(1,14) = 7.500, p = 0.016 *, ηp2 = 0.349 |
| Group A (nA = 15) | Group B (nB = 15) | Group A vs. B | Analysis of Variance, p Value, ηp2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Change Mean (%), [95% CI: Lower/Higher Bound] | Baseline | Follow-Up | Change Mean (%), [95% CI: Lower/Higher Bound] | Change Mean (%), [95% CI: Lower/Higher Bound] | Group | Time | Group × Time | ||
| Pre | Post | ||||||||||
| Vitamin D (ng/mL) | 30.79 ± 10.55 | 30.68 ± 9.26 | −0.11 (−0.41%), [95% CI: −3.63, 3.41] | 30.62 ± 10.49 | 30.63 ± 10.58 | +0.01 (+0.03%), [95% CI: −0.18, 0.20] | −0.17 (−0.56%) [95% CI: −7.69, 7.35] | −0.05 (−0.16%) [95% CI: −7.16, 7.06] | F(1,14) = 0.014, p = 0.908, ηp2 = 0.001 | F(1,14) = 0.004, p = 0.953, ηp2 = 0.000 | F(1,14) = 0.005, p = 0.943, ηp2 = 0.000 |
| PLR (ng/mL) | 10.14 ± 9.64 | 9.56 ± 3.28 | −0.58 (−5.70%), [95% CI: −5.05, 3.89] | 10.13 ± 9.65 | 10.12 ± 9.66 | −0.01 (−0.10%), [95% CI: −0.03, 0.01] | −0.01 (−0.10%) [95% CI: −6.91, 6.89] | +0.59 (+5.83%) [95% CI: −4.60, 5.72] | F(1,14) = 0.059, p = 0.812, ηp2 = 0.004 | F(1,14) = 0.068, p = 0.799, ηp2 = 0.005 | F(1,14) = 0.062, p = 0.807, ηp2 = 0.004 |
| PTH (pg/mL) | 71.28 ± 36.11 | 69.06 ± 26.85 | −2.22 (−3.10%), [95% CI: −10.92, 6.50] | 71.13 ± 35.87 | 71.18 ± 35.85 | +0.05 (+0.07%), [95% CI: −0.09, 0.19] | −0.15 (−0.21%) [95% CI: −25.90, 25.60] | +2.12 (+2.98%) [95% CI: −20.54, 24.78] | F(1,14) = 0.212, p = 0.652, ηp2 = 0.015 | F(1,14) = 0.237, p = 0.634, ηp2 = 0.017 | F(1,14) = 0.259, p = 0.618, ηp2 = 0.018 |
| Phosphorus (mg/dL) | 3.49 ± 0.58 | 3.63 ± 0.51 | +0.14 (+4.00%), [95% CI: −0.02, 0.30] | 3.48 ± 0.55 | 3.47 ± 0.54 | −0.01 (−0.29%), [95% CI: −0.02, 0.00] | −0.01 (−0.29%) [95% CI: −0.41, 0.39] | −0.16 (−4.61%) [95% CI: −0.53, 0.21] | F(1,14) = 3.706, p = 0.075, ηp2 = 0.209 | F(1,14) = 2.621, p = 0.128, ηp2 = 0.158 | F(1,14) = 2.660, p = 0.125, ηp2 = 0.160 |
| ALP (U/L) | 54.00 ± 14.30 | 54.66 ± 14.20 | +0.66 (+1.20%), [95% CI: −3.23, 3.75] | 54.00 ± 14.73 | 54.06 ± 14.71 | +0.06 (+0.11%), [95% CI: −0.23, 0.35] | 0.00 (0.00%) [95% CI: −10.38, 10.38] | −0.60 (−1.11%) [95% CI: −10.94, 9.74] | F(1,14) = 0.513, p = 0.485, ηp2 = 0.035 | F(1,14) = 0.847, p = 0.373, ηp2 = 0.057 | F(1,14) = 0.920, p = 0.354, ηp2 = 0.062 |
| Group A (nA = 15) | Group B (nB = 15) | Group A vs. B | Analysis of Variance, p Value, ηp2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Change Mean (%), [95% CI: Lower/Higher Bound] | Baseline | Follow-Up | Change Mean (%), [95% CI: Lower/Higher Bound] | Change Mean (%), [95% CI: Lower/Higher Bound] | Group | Time | Group × Time | ||
| Pre | Post | ||||||||||
| BMD lumbar spine (L1–L4) (g/cm2) | 0.84 ± 0.09 | 0.85 ± 0.10 | +0.01 (+1.19%), [95% CI: 0.00, 0.02] | 0.83 ± 0.10 | 0.83 ± 0.11 | ≈0.00 (0.0%), [95% CI: −0.01, 0.00] | +0.01 (+1.20%) [95% CI: −0.05, 0.07] | −0.02 (−2.40%) [95% CI: −0.09, 0.05] | F(1,14) = 3.689, p = 0.075, ηp2 = 0.209 | F(1,14) = 0.868, p = 0.367, ηp2 = 0.209 | F(1,14) = 2.494, p = 0.137, ηp2 = 0.151 |
| BMD total hip (left) (g/cm2) | 0.74 ± 0.10 | 0.77 ± 0.11 | +0.02 (+4.05%), [95% CI: 0.01, 0.03] | 0.74 ± 0.11 | 0.73 ± 0.09 | −0.01 (−1.35%), [95% CI: −0.02, 0.00] | 0.00 (0.00%) [95% CI: −0.07, 0.07] | −0.04 (−5.50%) [95% CI: −0.11, 0.03] | F(1,14) = 3.457, p = 0.084, ηp2 = 0.198 | F(1,14) = 1.759, p = 0.206, ηp2 = 0.112 | F(1,14) = 10.717, p = 0.006 *, ηp2 = 0.434 |
| BMD total hip (right/dominant) (g/cm2) | 0.76 ± 0.08 | 0.81 ± 0.08 | +0.05 (+6.57%), [95% CI: 0.03, 0.06] | 0.75 ± 0.08 | 0.75 ± 0.07 | ≈ 0.00 (0.0%), [95% CI: −0.01, 0.00] | −0.01 (−1.30%) [95% CI: −0.06, 0.04] | −0.06 (−8.00% [95% CI: −0.11, −0.01] | F(1,14) = 14.057, p = 0.002 *, ηp2 = 0.501 | F(1,14) = 32.834, p < 0.001 *, ηp2 = 0.701 | F(1,14) = 36.974, p < 0.001 *, ηp2 = 0.725 |
| Total spine Τ-score | −2.37 ± 0.97 | −2.32 ± 1.06 | +0.05 (+2.1%), [95% CI: −0.12, 0.22] | −2.30 ± 0.81 | −2.34 ± 0.82 | −0.05 (−1.7%), [95% CI: −0.08, −0.01] | +0.07 (+3.00%) [95% CI: −0.57, 0.71] | −0.02 (−0.90%) [95% CI: −0.69, 0.66] | F(1,14) = 1.711, p = 0.212, ηp2 = 0.109 | F(1,14) = 2.373, p = 0.146, ηp2 = 0.145 | F(1,14) = 2.400, p = 0.144, ηp2 = 0.146 |
| Total hip (left) Τ-score | −1.84 ± 0.74 | −1.47 ± 1.09 | +0.37 (+20.1%), [95% CI: 0.01, 0.73] | −1.90 ± 0.70 | −1.92 ± 0.69 | −0.02 (−1.1%), [95% CI: −0.05, 0.01] | −0.06 (−3.20%) [95% CI: −0.57,0.71] | −0.45 (−23.40%) [95% CI: −1.10, 0.20] | F(1,14) = 5.598, p = 0.033 *, ηp2 = 0.286 | F(1,14) = 3.430, p = 0.085, ηp2 = 0.197 | F(1,14) = 4.387, p = 0.055, ηp2 = 0.239 |
| Total hip (right) Τ-score | −1.90 ± 0.69 | −1.44 ± 0.87 | +0.46 (+24.2%), [95% CI: 0.26, 0.66] | −2.06 ± 0.78 | −2.10 ± 0.79 | −0.04 (−1.9%), [95% CI: −0.08, 0.01] | −0.16 (−7.80%) [95% CI: −0.68, 0.37] | −0.66 (−31.40%) [95% CI: −1.25, −0.06] | F(1,14) = 14.611, p = 0.002 *, ηp2 = 0.511 | F(1,14) = 15.578, p = 0.001 *, ηp2 = 0.527 | F(1,14) = 22.246, p < 0.001, ηp2 = 0.614 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kotsili, K.; Michou, V.; Koutlianos, N.; Dalkiranis, A.; Kouidi, E.; Deligiannis, A. Investigating the Role of Exercise in Improving Bone Health Among Elderly Women with Osteopenia. J. Funct. Morphol. Kinesiol. 2025, 10, 451. https://doi.org/10.3390/jfmk10040451
Kotsili K, Michou V, Koutlianos N, Dalkiranis A, Kouidi E, Deligiannis A. Investigating the Role of Exercise in Improving Bone Health Among Elderly Women with Osteopenia. Journal of Functional Morphology and Kinesiology. 2025; 10(4):451. https://doi.org/10.3390/jfmk10040451
Chicago/Turabian StyleKotsili, Kyriaki, Vasiliki Michou, Nikolaos Koutlianos, Anastasios Dalkiranis, Evangelia Kouidi, and Asterios Deligiannis. 2025. "Investigating the Role of Exercise in Improving Bone Health Among Elderly Women with Osteopenia" Journal of Functional Morphology and Kinesiology 10, no. 4: 451. https://doi.org/10.3390/jfmk10040451
APA StyleKotsili, K., Michou, V., Koutlianos, N., Dalkiranis, A., Kouidi, E., & Deligiannis, A. (2025). Investigating the Role of Exercise in Improving Bone Health Among Elderly Women with Osteopenia. Journal of Functional Morphology and Kinesiology, 10(4), 451. https://doi.org/10.3390/jfmk10040451







