Cutting Through Time: A Surgical Comparison of Bosworth, LARS™, and TightRope® for AC Joint Dislocations
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Selection
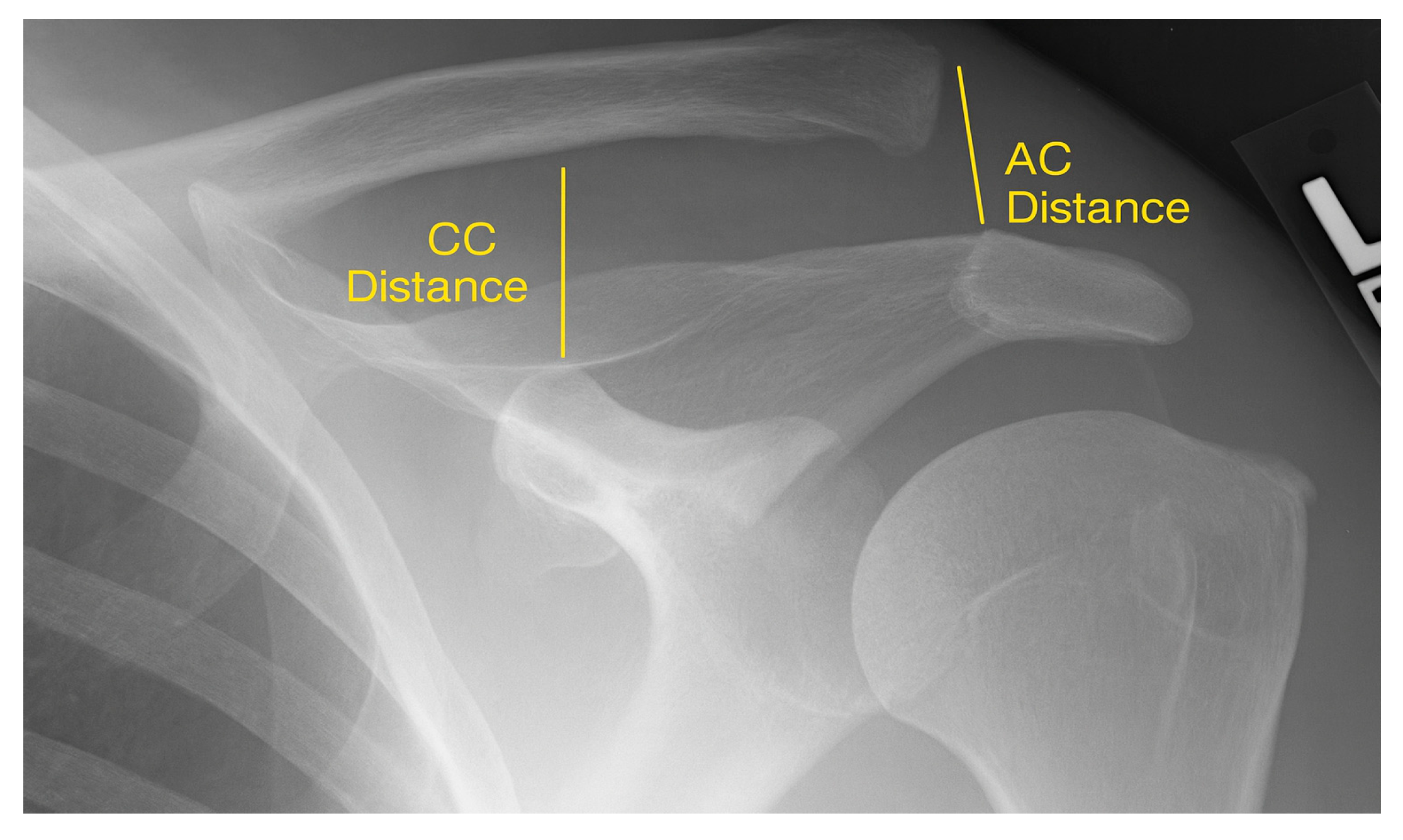
2.2. Radiological Assessment
2.3. Clinical Outcome Measures
2.4. Surgical Procedure
2.4.1. Bosworth Screw
2.4.2. LARS™
2.4.3. TightRope®
2.5. Study Objectives and Statistical Analysis
3. Results
3.1. Epidemiological Data
3.2. Clinical Outcomes
3.3. Radiological Outcome
3.4. Complications
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- North, A.S. Rockwood grade I and II acromioclavicular injuries: As benign as commonly believed? Joints 2016, 4, 171–173. [Google Scholar] [CrossRef]
- Arirachakaran, A.; Boonard, M.; Piyapittayanun, P.; Kanchanatawan, W.; Chaijenkij, K.; Prommahachai, A.; Kongtharvonskul, J. Post-operative outcomes and complications of suspensory loop fixation device versus hook plate in acute unstable acromioclavicular joint dislocation: A systematic review and meta-analysis. J. Orthop. Traumatol. 2017, 18, 293–304. [Google Scholar] [CrossRef]
- Dias, J.J.; Gregg, P.J. Acromioclavicular joint injuries in sport. Recommendations for treatment. Sports Med. 1991, 11, 125–132. [Google Scholar] [CrossRef]
- Pan, X.; Lv, R.Y.; Lv, M.G.; Zhang, D.G. TightRope vs Clavicular Hook Plate for Rockwood III–V Acromioclavicular Dislocations: A Meta-Analysis. Orthop. Surg. 2020, 12, 1045–1052. [Google Scholar] [CrossRef]
- Cisneros, L.N.; Reiriz, J.S. Management of chronic unstable acromioclavicular joint injuries. J. Orthop. Traumatol. 2017, 18, 305–318. [Google Scholar] [CrossRef]
- Morell, D.J.; Thyagarajan, D.S. Sternoclavicular joint dislocation and its management: A review of the literature. World J. Orthop. 2016, 7, 244–250. [Google Scholar] [CrossRef]
- Tamaoki, M.J.; Belloti, J.C.; Lenza, M.; Matsumoto, M.H.; Gomes Dos Santos, J.B.; Faloppa, F. Surgical versus conservative interventions for treating acromioclavicular dislocation of the shoulder in adults. Cochrane Database Syst. Rev. 2010, 2010, Cd007429. [Google Scholar] [CrossRef]
- Barth, J.; Duparc, F.; Andrieu, K.; Duport, M.; Toussaint, B.; Bertiaux, S.; Clavert, P.; Gastaud, O.; Brassart, N.; Beaudouin, E.; et al. Is coracoclavicular stabilisation alone sufficient for the endoscopic treatment of severe acromioclavicular joint dislocation (Rockwood types III, IV, and V)? Orthop. Traumatol. Surg. Res. 2015, 101, S297–S303. [Google Scholar] [CrossRef]
- Darabos, N.; Vlahovic, I.; Gusic, N.; Darabos, A.; Bakota, B.; Miklic, D. Is AC TightRope fixation better than Bosworth screw fixation for minimally invasive operative treatment of Rockwood III AC joint injury? Injury 2015, 46 (Suppl. 6), S113–S118. [Google Scholar] [CrossRef]
- Phadke, A.; Bakti, N.; Bawale, R.; Singh, B. Current concepts in management of ACJ injuries. J. Clin. Orthop. Trauma. 2019, 10, 480–485. [Google Scholar] [CrossRef]
- Pallis, M.; Cameron, K.L.; Svoboda, S.J.; Owens, B.D. Epidemiology of acromioclavicular joint injury in young athletes. Am. J. Sports Med. 2012, 40, 2072–2077. [Google Scholar] [CrossRef]
- Goldstein, Y.; Dolkart, O.; Kaufman, E.; Amar, E.; Sharfman, Z.T.; Rath, E.; Mozes, G.; Maman, E. Bicycle-Related Shoulder Injuries: Etiology and the Need for Protective Gear. Isr. Med. Assoc. J. 2016, 18, 23–26. [Google Scholar]
- Headey, J.; Brooks, J.H.; Kemp, S.P. The epidemiology of shoulder injuries in English professional rugby union. Am. J. Sports Med. 2007, 35, 1537–1543. [Google Scholar] [CrossRef]
- Baren, J.P.; Rowbotham, E.; Robinson, P. Acromioclavicular Joint Injury and Repair. Semin. Musculoskelet. Radiol. 2022, 26, 597–610. [Google Scholar] [CrossRef]
- Berthold, D.P.; Muench, L.N.; Dyrna, F.; Mazzocca, A.D.; Garvin, P.; Voss, A.; Scheiderer, B.; Siebenlist, S.; Imhoff, A.B.; Beitzel, K. Current concepts in acromioclavicular joint (AC) instability—A proposed treatment algorithm for acute and chronic AC-joint surgery. BMC Musculoskelet. Disord. 2022, 23, 1078. [Google Scholar] [CrossRef]
- Yubran, A.P.; Pesquera, L.C.; Juan, E.L.S.; Saralegui, F.I.; Canga, A.C.; Camara, A.C.; Valdivieso, G.M. Presurgical perspective and postsurgical evaluation of acromioclavicular joint instability. Skeletal Radiol. 2024, 53, 847–861. [Google Scholar] [CrossRef]
- Mikek, M. Long-term shoulder function after type I and II acromioclavicular joint disruption. Am. J. Sports Med. 2008, 36, 2147–2150. [Google Scholar] [CrossRef]
- Mouhsine, E.; Garofalo, R.; Crevoisier, X.; Farron, A. Grade I and II acromioclavicular dislocations: Results of conservative treatment. J. Shoulder Elb. Surg. 2003, 12, 599–602. [Google Scholar] [CrossRef]
- Rolf, O.; Hann von Weyhern, A.; Ewers, A.; Boehm, T.D.; Gohlke, F. Acromioclavicular dislocation Rockwood III–V: Results of early versus delayed surgical treatment. Arch. Orthop. Trauma. Surg. 2008, 128, 1153–1157. [Google Scholar] [CrossRef]
- Korsten, K.; Gunning, A.C.; Leenen, L.P. Operative or conservative treatment in patients with Rockwood type III acromioclavicular dislocation: A systematic review and update of current literature. Int. Orthop. 2014, 38, 831–838. [Google Scholar] [CrossRef]
- Lee, Y.M.; Yeo, J.D.; Hwang, Z.O.; Song, S.W.; Sur, Y.J. Reconstruction of the coracoclavicular ligament with palmaris longus tendon and Mersilene tape for acromioclavicular dislocations. BMC Musculoskelet. Disord. 2022, 23, 648. [Google Scholar] [CrossRef]
- Lu, N.; Zhu, L.; Ye, T.; Chen, A.; Jiang, X.; Zhang, Z.; Zhu, Q.; Guo, Q.; Yang, D. Evaluation of the coracoclavicular reconstruction using LARS artificial ligament in acute acromioclavicular joint dislocation. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 2223–2227. [Google Scholar] [CrossRef]
- Gu, F.; Tan, L.; Wang, T.; Wen, Q.; Su, Z.; Sui, Z.; Yu, T. Comparison of single versus double TightRope system in the treatment of acute acromioclavicular joint dislocation. J. Shoulder Elb. Surg. 2021, 30, 1915–1923. [Google Scholar] [CrossRef]
- Frank, R.M.; Cotter, E.J.; Leroux, T.S.; Romeo, A.A. Acromioclavicular Joint Injuries: Evidence-based Treatment. J. Am. Acad. Orthop. Surg. 2019, 27, e775–e788. [Google Scholar] [CrossRef]
- Mazzocca, A.D.; Arciero, R.A.; Bicos, J. Evaluation and treatment of acromioclavicular joint injuries. Am. J. Sports Med. 2007, 35, 316–329. [Google Scholar] [CrossRef]
- Takase, K.; Yamamoto, K. Changes in surgical procedures for acromioclavicular joint dislocation over the past 30 years. Orthopedics 2013, 36, e1277–e1282. [Google Scholar] [CrossRef]
- Tiefenboeck, T.M.; Popp, D.; Boesmueller, S.; Payr, S.; Joestl, J.; Komjati, M.; Binder, H.; Schurz, M.; Ostermann, R.C. Acromioclavicular joint dislocation treated with Bosworth screw and additional K-wiring: Results after 7.8 years—Still an adequate procedure? BMC Musculoskelet. Disord. 2017, 18, 339. [Google Scholar] [CrossRef]
- Ochen, Y.; Beks, R.B.; Emmink, B.L.; Wittich, P.; van der Velde, D.; Houwert, R.M.; Keizer, J. Surgical treatment of acute and chronic AC joint dislocations: Five-year experience with conventional and modified LARS fixation by a single surgeon. J. Orthop. 2020, 17, 73–77. [Google Scholar] [CrossRef]
- Koch, M.; Werner, A.; Engel, G.; Huth, J.; Mauch, F. Mini-open vs. arthroscopic double tight-rope reconstruction after acute AC-joint dislocation: A comparison in functional outcome and sports activity. Arch. Orthop. Trauma. Surg. 2023, 143, 5491–5500. [Google Scholar] [CrossRef]
- Nie, S.; Lan, M. Comparison of clinical efficacy between arthroscopically assisted Tight-Rope technique and clavicular hook plate fixation in treating acute high-grade acromioclavicular joint separations. J. Orthop. Surg. 2021, 29, 23094990211010562. [Google Scholar] [CrossRef]
- De Rooij, P.P.; Van Lieshout, E.M.M.; Schurink, I.J.; Verhofstad, M.H.J. Current practice in the management of acromioclavicular joint dislocations; a national survey in the Netherlands. Eur. J. Trauma. Emerg. Surg. 2021, 47, 1417–1427. [Google Scholar] [CrossRef]
- Breivik, H. Fifty years on the Visual Analogue Scale (VAS) for pain-intensity is still good for acute pain. But multidimensional assessment is needed for chronic pain. Scand. J. Pain. 2016, 11, 150–152. [Google Scholar] [CrossRef]
- Ziegler, P.; Kühle, L.; Stöckle, U.; Wintermeyer, E.; Stollhof, L.E.; Ihle, C.; Bahrs, C. Evaluation of the Constant score: Which is the method to assess the objective strength? BMC Musculoskelet. Disord. 2019, 20, 403. [Google Scholar] [CrossRef] [PubMed]
- Padua, R.; de Girolamo, L.; Grassi, A.; Cucchi, D. Choosing patient-reported outcome measures for shoulder pathology. EFORT Open Rev. 2021, 6, 779–787. [Google Scholar] [CrossRef]
- Neto, J.O.; Gesser, R.L.; Steglich, V.; Bonilauri Ferreira, A.P.; Gandhi, M.; Vissoci, J.R.; Pietrobon, R. Validation of the Simple Shoulder Test in a Portuguese-Brazilian population. Is the latent variable structure and validation of the Simple Shoulder Test Stable across cultures? PLoS ONE 2013, 8, e62890. [Google Scholar] [CrossRef] [PubMed]
- Hou, J.; Li, Q.; Yu, M.; Li, F.; Tang, Y.; Long, Y.; Alike, Y.; Zhang, Y.; Ali, M.I.; Zhang, C.; et al. Validation of a Mobile Version of the American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form: An Observational Randomized Crossover Trial. JMIR Mhealth Uhealth 2020, 8, e16758. [Google Scholar] [CrossRef]
- Thamyongkit, S.; Wanitchanont, T.; Chulsomlee, K.; Tuntiyatorn, P.; Vasaruchapong, S.; Vijittrakarnrung, C.; Saengpetch, N. The University of California-Los Angeles (UCLA) shoulder scale: Translation, reliability and validation of a Thai version of UCLA shoulder scale in rotator cuff tear patients. BMC Musculoskelet. Disord. 2022, 23, 65. [Google Scholar] [CrossRef] [PubMed]
- Liegl, G.; Fischer, F.H.; Martin, C.N.; Rönnefarth, M.; Blumrich, A.; Ahmadi, M.; Boldt, L.H.; Eckardt, K.U.; Endres, M.; Edelmann, F.; et al. Converting PROMIS(®)-29 v2.0 profile data to SF-36 physical and mental component summary scores in patients with cardiovascular disorders. Health Qual. Life Outcomes 2024, 22, 64. [Google Scholar] [CrossRef]
- Bosworth, B.M. Complete acromioclavicular dislocation. N. Engl. J. Med. 1949, 241, 221–225. [Google Scholar] [CrossRef]
- Marcheggiani Muccioli, G.M.; Manning, C.; Wright, P.; Grassi, A.; Zaffagnini, S.; Funk, L. Acromioclavicular joint reconstruction with the LARS ligament in professional versus non-professional athletes. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 1961–1967. [Google Scholar] [CrossRef]
- Thiel, E.; Mutnal, A.; Gilot, G.J. Surgical outcome following arthroscopic fixation of acromioclavicular joint disruption with the tightrope device. Orthopedics 2011, 34, e267–e274. [Google Scholar] [CrossRef]
- Peebles, L.A.; Akamefula, R.A.; Kraeutler, M.J.; Mulcahey, M.K. Management of Acromioclavicular Joint Injuries: A Historic Account. Clin. Sports Med. 2023, 42, 539–556. [Google Scholar] [CrossRef]
- Spencer, H.T.; Hsu, L.; Sodl, J.; Arianjam, A.; Yian, E.H. Radiographic failure and rates of re-operation after acromioclavicular joint reconstruction: A comparison of surgical techniques. Bone Jt. J. 2016, 98-b, 512–518. [Google Scholar] [CrossRef]
- Woodmass, J.M.; Esposito, J.G.; Ono, Y.; Nelson, A.A.; Boorman, R.S.; Thornton, G.M.; Lo, I.K. Complications following arthroscopic fixation of acromioclavicular separations: A systematic review of the literature. Open Access J. Sports Med. 2015, 6, 97–107. [Google Scholar] [CrossRef]
- Broos, P.; Stoffelen, D.; Van de Sijpe, K.; Fourneau, I. Surgical management of complete Tossy III acromioclavicular joint dislocation with the Bosworth screw or the Wolter plate. A critical evaluation. Unfallchirurgie 1997, 23, 153–159; discussion 160. [Google Scholar] [CrossRef]
- Trieb, K.; Blahovec, H.; Brand, G.; Sabeti, M.; Dominkus, M.; Kotz, R. In vivo and in vitro cellular ingrowth into a new generation of artificial ligaments. Eur. Surg. Res. 2004, 36, 148–151. [Google Scholar] [CrossRef]
- Liu, Z.T.; Zhang, X.L.; Jiang, Y.; Zeng, B.F. Four-strand hamstring tendon autograft versus LARS artificial ligament for anterior cruciate ligament reconstruction. Int. Orthop. 2010, 34, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Tiefenboeck, T.M.; Boesmueller, S.; Popp, D.; Payr, S.; Joestl, J.; Binder, H.; Schurz, M.; Komjati, M.; Fialka, C.; Ostermann, R.C. The use of the LARS system in the treatment of AC joint instability—Long-term results after a mean of 7.4 years. Orthop. Traumatol. Surg. Res. 2018, 104, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Jensen, G.; Katthagen, J.C.; Alvarado, L.E.; Lill, H.; Voigt, C. Has the arthroscopically assisted reduction of acute AC joint separations with the double tight-rope technique advantages over the clavicular hook plate fixation? Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Dobbelaere, A.; D’Hondt, L.; Harth, A.; Depaepe, Y. Midterm outcome after AC Tightrope fixation. Acta Orthop. Belg. 2020, 86, 502–508. [Google Scholar]
- Flint, J.H.; Wade, A.M.; Giuliani, J.; Rue, J.P. Defining the terms acute and chronic in orthopaedic sports injuries: A systematic review. Am. J. Sports Med. 2014, 42, 235–241. [Google Scholar] [CrossRef]
- Borbas, P.; Churchill, J.; Ek, E.T. Surgical management of chronic high-grade acromioclavicular joint dislocations: A systematic review. J. Shoulder Elb. Surg. 2019, 28, 2031–2038. [Google Scholar] [CrossRef]
- Moatshe, G.; Kruckeberg, B.M.; Chahla, J.; Godin, J.A.; Cinque, M.E.; Provencher, M.T.; LaPrade, R.F. Acromioclavicular and Coracoclavicular Ligament Reconstruction for Acromioclavicular Joint Instability: A Systematic Review of Clinical and Radiographic Outcomes. Arthrosc. J. Arthrosc. Relat. Surg. Off. Publ. Arthrosc. Assoc. N. Am. Int. Arthrosc. Assoc. 2018, 34, 1979–1995.e1978. [Google Scholar] [CrossRef]
- Fauci, F.; Merolla, G.; Paladini, P.; Campi, F.; Porcellini, G. Surgical treatment of chronic acromioclavicular dislocation with biologic graft vs synthetic ligament: A prospective randomized comparative study. J. Orthop. Traumatol. 2013, 14, 283–290. [Google Scholar] [CrossRef]
- Kumar, V.; Garg, S.; Elzein, I.; Lawrence, T.; Manning, P.; Wallace, W.A. Modified Weaver-Dunn procedure versus the use of a synthetic ligament for acromioclavicular joint reconstruction. J. Orthop. Surg. 2014, 22, 199–203. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.M.; Wang, C.H.; Hsu, K.L.; Kuan, F.C.; Chen, Y.; Su, W.R.; Hong, C.K. Does Weaver-Dunn procedure have a role in chronic acromioclavicular dislocations? A meta-analysis. J. Orthop. Surg. Res. 2022, 17, 95. [Google Scholar] [CrossRef] [PubMed]
- Saccomanno, M.F.; Marchi, G.; Mocini, F.; Vismara, V.; Campana, V.; Salvi, A.G.; Scaini, A.; Milano, G. Anatomic reconstruction of the coracoclavicular and acromioclavicular ligaments with semitendinosus tendon graft for the treatment of chronic acromioclavicular joint dislocation provides good clinical and radiological results. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 2356–2363. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, D.M.; McCann, P.D.; McIlveen, S.J.; Flatow, E.L.; Bigliani, L.U. Surgical treatment of complete acromioclavicular dislocations. Am. J. Sports Med. 1995, 23, 324–331. [Google Scholar] [CrossRef]
| Variable | Bosworth | LARS Acute | LARS Chronic | TightRope |
|---|---|---|---|---|
| age (years) | ||||
| mean | 38.3 | 35.64 | 34.69 | 34.63 |
| SD | 15.53 | 11.33 | 11.46 | 11.83 |
| median | 33.48 | 33.75 | 31.2 | 29.89 |
| 1st quartile | 25.87 | 27.41 | 27.93 | 25.92 |
| 3rd quartile | 50.1 | 40.68 | 37.34 | 42.47 |
| minimum | 16.13 | 17.22 | 20.11 | 16.64 |
| maximum | 75.76 | 69.64 | 69.4 | 61.04 |
| Rockwood Classification | ||||
| Rockwood III | 23 (79%) | 57 (52%) | 26 (62%) | 41 (63%) |
| Rockwood IV | 4 (14%) | 28 (25%) | 8 (19%) | 17 (26%) |
| Rockwood V | 2 (7%) | 25 (23%) | 8 (19%) | 7 (11%) |
| time to surgery (days) | ||||
| mean | 26.97 | 10.88 | 62.43 | 11.14 |
| SD | 65.52 | 6.2 | 34.55 | 7.15 |
| median | 9 | 10 | 37 | 10 |
| 1st quartile | 4 | 6 | 34.25 | 6 |
| 3rd quartile | 18 | 15 | 93.25 | 13 |
| minimum | 0 | 0 | 30 | 0 |
| maximum | 294 | 25 | 189 | 42 |
| operating time (minutes) | ||||
| mean | 77.41 | 70.73 | 72.71 | 86.48 |
| SD | 24.6 | 21.38 | 23.81 | 34.5 |
| median | 75 | 70 | 65 | 85 |
| 1st quartile | 55 | 55 | 55 | 60 |
| 3rd quartile | 95 | 80 | 75 | 105 |
| minimum | 40 | 40 | 50 | 20 |
| maximum | 135 | 150 | 140 | 170 |
| follow-up (months) | ||||
| mean | 196.9 | 97.5 | 88.1 | 86.4 |
| SD | 55.6 | 10.5 | 11.3 | 12.2 |
| median | 192.5 | 98.6 | 92.6 | 90.3 |
| 1st quartile | 175.9 | 90.4 | 80.5 | 77.9 |
| 3rd quartile | 230 | 104.6 | 95.7 | 94.1 |
| minimum | 160.1 | 51.4 | 49.5 | 66.3 |
| maximum | 266.7 | 181.1 | 182.4 | 108.7 |
| Score | Bosworth (Mean ± SD) | LARS Acute (Mean ± SD) | LARS Chronic (Mean ± SD) | TightRope (Mean ± SD) | p-Value |
|---|---|---|---|---|---|
| VAS | 3.33 ± 1.25 | 1.48 ± 2.00 | 1.62 ± 2.18 | 1.52 ± 2.06 | 0.0003 |
| Constant | 92.54 ± 19.82 | 91.36 ± 16.45 | 95.52 ± 5.45 | 96.83 ± 5.41 | 0.0853 |
| DASH | 9.26 ± 19.39 | 5.40 ± 11.23 | 4.66 ± 6.94 | 4.87 ± 9.60 | 0.7936 |
| ASES | 93.26 ± 8.34 | 92.43 ± 13.50 | 95.39 ± 7.00 | 94.11 ± 11.81 | 0.0610 |
| SST | 96.49 ± 12.82 | 95.79 ± 9.18 | 96.21 ± 7.42 | 95.77 ± 14.37 | 0.4804 |
| UCLA | 35.32 ± 13.35 | 33.59 ± 7.21 | 33.27 ± 2.84 | 33.40 ± 4.57 | 0.3652 |
| SF-PF | 97.50 ± 4.81 | 95.43 ± 8.24 | 94.54 ± 8.18 | 92.85 ± 11.52 | 0.0481 |
| SF-RP | 96.43 ± 8.91 | 96.18 ± 17.20 | 96.02 ± 11.85 | 95.00 ± 17.79 | 0.8123 |
| SF-BP | 94.79 ± 14.31 | 93.75 ± 11.64 | 88.66 ± 17.91 | 93.82 ± 11.45 | 0.0317 |
| SF-GH | 79.68 ± 17.75 | 90.28 ± 10.92 | 86.89 ± 13.75 | 78.15 ± 13.73 | 0.0002 |
| SF-VT | 71.43 ± 12.01 | 73.00 ± 13.84 | 65.68 ± 16.74 | 62.69 ± 17.16 | 0.0021 |
| SF-SF | 97.77 ± 4.88 | 99.14 ± 5.61 | 97.73 ± 10.41 | 95.38 ± 12.80 | 0.0527 |
| SF-RE | 94.95 ± 17.48 | 94.95 ± 20.95 | 89.82 ± 26.58 | 96.41 ± 13.34 | 0.2150 |
| SF-MH | 85.63 ± 11.16 | 87.35 ± 9.64 | 85.10 ± 11.67 | 84.98 ± 8.49 | 0.4336 |
| Measurement (cm) | Mean | SD | Median | Q1 | Q3 | Min | Max |
|---|---|---|---|---|---|---|---|
| Bosworth | |||||||
| CC_final | 1.1471 | 0.3550 | 1.05 | 0.905 | 1.2825 | 0.70 | 1.98 |
| CC_pre | 1.6514 | 0.5538 | 1.59 | 1.24 | 1.95 | 0.84 | 2.77 |
| CC_final_WB | 1.2786 | 0.3182 | 1.21 | 1.07 | 1.3975 | 0.87 | 2.02 |
| CC_pre_WB | 2.0183 | 0.5630 | 2.08 | 1.48 | 2.51 | 1.12 | 2.88 |
| CC_final_uninjured | 1.0982 | 0.1788 | 1.05 | 0.99 | 1.22 | 0.76 | 1.53 |
| CC_pre_uninjured | 1.1424 | 0.1957 | 1.11 | 1.01 | 1.30 | 0.69 | 1.44 |
| LARS acute | |||||||
| CC_final | 1.2165 | 0.3217 | 1.18 | 1.00 | 1.37 | 0.70 | 2.73 |
| CC_pre | 1.7991 | 0.4466 | 1.75 | 1.45 | 2.07 | 0.98 | 2.87 |
| CC_final_WB | 1.4046 | 0.3334 | 1.37 | 1.14 | 1.57 | 0.82 | 2.83 |
| CC_pre_WB | 2.0612 | 0.4798 | 2.025 | 1.68 | 2.42 | 1.17 | 3.29 |
| CC_final_uninjured | 1.1130 | 0.2048 | 1.10 | 0.99 | 1.22 | 0.75 | 1.87 |
| CC_pre_uninjured | 1.1379 | 0.1960 | 1.12 | 1.00 | 1.24 | 0.77 | 2.21 |
| LARS chronic | |||||||
| CC_final | 1.3981 | 0.3677 | 1.355 | 1.175 | 1.435 | 0.93 | 2.73 |
| CC_pre | 1.6733 | 0.3983 | 1.58 | 1.27 | 1.92 | 1.18 | 2.33 |
| CC_final_WB | 1.5662 | 0.3732 | 1.49 | 1.35 | 1.7175 | 1.10 | 2.83 |
| CC_pre_WB | 2.0838 | 0.4281 | 1.87 | 1.77 | 2.42 | 1.54 | 3.29 |
| CC_final_uninjured | 1.1257 | 0.1539 | 1.13 | 1.01 | 1.20 | 0.84 | 1.45 |
| CC_pre_uninjured | 1.1326 | 0.1652 | 1.11 | 1.00 | 1.19 | 0.84 | 1.53 |
| TightRope® | |||||||
| CC_final | 1.2646 | 0.3838 | 1.18 | 1.02 | 1.49 | 0.51 | 2.09 |
| CC_pre | 1.8983 | 0.6267 | 1.815 | 1.445 | 2.305 | 0.201 | 3.59 |
| CC_final_WB | 1.4153 | 0.4662 | 1.355 | 1.0925 | 1.685 | 0.57 | 2.48 |
| CC_pre_WB | 1.9312 | 0.7139 | 1.86 | 1.73 | 2.235 | 0.169 | 3.38 |
| CC_final_uninjured | 1.1490 | 0.2429 | 1.14 | 0.96 | 1.31 | 0.69 | 1.73 |
| CC_pre_uninjured | 1.0409 | 0.3405 | 1.04 | 0.85 | 1.25 | 0.11 | 2.21 |
| Measurement (cm) | Mean | SD | Median | Q1 | Q3 | Min | Max |
|---|---|---|---|---|---|---|---|
| Bosworth | |||||||
| AC_final | 0.5282 | 0.2597 | 0.485 | 0.3275 | 0.645 | 0.12 | 1.23 |
| AC_pre | 0.7884 | 0.3068 | 0.765 | 0.53 | 0.99 | 0.22 | 1.36 |
| AC_final_WB | 0.7568 | 0.3703 | 0.65 | 0.5075 | 0.955 | 0.36 | 1.89 |
| AC_pre_WB | 1.0228 | 0.2887 | 1.01 | 0.83 | 1.25 | 0.39 | 1.52 |
| AC_final_uninjured | 0.4339 | 0.2046 | 0.42 | 0.28 | 0.53 | 0.12 | 0.86 |
| AC_pre_uninjured | 0.4293 | 0.2180 | 0.39 | 0.29 | 0.57 | 0.10 | 0.90 |
| LARS acute | |||||||
| AC_final | 0.5312 | 0.2864 | 0.46 | 0.33 | 0.65 | 0.11 | 1.63 |
| AC_pre | 0.9489 | 0.4171 | 0.91 | 0.6125 | 1.2175 | 0.34 | 2.75 |
| AC_final_WB | 0.6520 | 0.3022 | 0.55 | 0.44 | 0.77 | 0.25 | 1.82 |
| AC_pre_WB | 1.1862 | 0.4408 | 1.115 | 0.8875 | 1.485 | 0.40 | 2.88 |
| AC_final_uninjured | 0.4590 | 0.1718 | 0.44 | 0.33 | 0.55 | 0.16 | 1.22 |
| AC_pre_uninjured | 0.4981 | 0.1921 | 0.49 | 0.36 | 0.5975 | 0.19 | 1.49 |
| LARS chronic | |||||||
| AC_final | 0.6595 | 0.4078 | 0.49 | 0.38 | 0.97 | 0.11 | 1.69 |
| AC_pre | 1.1362 | 0.5061 | 1.045 | 0.81 | 1.32 | 0.41 | 2.75 |
| AC_final_WB | 0.8145 | 0.4171 | 0.685 | 0.49 | 1.0675 | 0.36 | 1.88 |
| AC_pre_WB | 1.3652 | 0.4728 | 1.17 | 1.0925 | 1.5675 | 0.69 | 2.88 |
| AC_final_uninjured | 0.4638 | 0.1470 | 0.445 | 0.345 | 0.5575 | 0.23 | 0.99 |
| AC_pre_uninjured | 0.4481 | 0.1223 | 0.425 | 0.36 | 0.5575 | 0.20 | 0.69 |
| TightRope® | |||||||
| AC_final | 0.7289 | 0.4853 | 0.525 | 0.44 | 0.955 | 0.26 | 2.77 |
| AC_pre | 1.4489 | 0.6159 | 1.315 | 1.065 | 1.74 | 0.34 | 3.27 |
| AC_final_WB | 0.8641 | 0.5276 | 0.675 | 0.535 | 1.085 | 0.30 | 2.92 |
| AC_pre_WB | 1.4658 | 0.5612 | 1.35 | 1.14 | 1.70 | 0.45 | 2.89 |
| AC_final_uninjured | 0.5417 | 0.2543 | 0.49 | 0.38 | 0.61 | 0.10 | 1.41 |
| AC_pre_uninjured | 0.5212 | 0.2570 | 0.48 | 0.31 | 0.63 | 0.10 | 1.30 |
| Measurement (cm) | Injured (Mean ± SD) | Uninjured (Mean ± SD) | p-Value |
|---|---|---|---|
| Bosworth | |||
| ΔAC | 0.2616 ± 0.3413 | 0.0614 ± 0.2693 | p = 0.0182 |
| ΔCC | 0.5086 ± 0.5557 | 0.1377 ± 0.4594 | p = 0.0087 |
| LARS acute | |||
| ΔAC | 0.4323 ± 0.4114 | 0.0491 ± 0.1592 | p < 0.0001 |
| ΔCC | 0.5919 ± 0.5004 | 0.0314 ± 0.1814 | p < 0.0001 |
| LARS chronic | |||
| ΔAC | 0.4767 ± 0.3779 | 0.0157 ± 0.1215 | p < 0.0001 |
| ΔCC | 0.2752 ± 0.5128 | 0.0069 ± 0.1290 | p = 0.0015 |
| TightRope® | |||
| ΔAC | 0.8403 ± 0.6715 | 0.0200 ± 0.1498 | p < 0.0001 |
| ΔCC | 0.7357 ± 0.6088 | 0.0746 ± 0.2183 | p < 0.0001 |
| Complications | Bosworth | LARS Acute | LARS Chronic | TightRope® |
|---|---|---|---|---|
| clavicular elevation | ||||
| double shaft width | 6.9% (n = 2) | 0% | 0% | 0% |
| full shaft width | 20.69% (n = 6) | 10.00% (n = 11) | 26.19% (n = 11) | 9.23% (n = 6) |
| half shaft width | 41.38% (n = 12) | 29.09% (n = 32) | 21.43% (n = 9) | 20.00% (n = 13) |
| none | 31.03% (n = 9) | 60.91% (n = 67) | 52.38% (n = 22) | 70.77% (n = 46) |
| AC joint osteoarthritis | ||||
| yes | 17.24% (n = 5) | 8.18% (n = 9) | 7.14% (n = 3) | 3.08% (n = 2) |
| no | 82.76% (n = 24) | 91.82% (n = 101) | 92.86% (n = 39) | 96.92% (n = 63) |
| CC ligament ossification | ||||
| yes | 37.93% (n = 11) | 21.82% (n = 24) | 19.05% (n = 8) | 7.69% (n = 5) |
| no | 62.07% (n = 18) | 78.18% (n = 86) | 80.95% (n = 34) | 92.31% (n = 60) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Popp, D.; Nia, A.; Silvaieh, S.; Nass, C.; Heisinger, S.; Pichler, L.; Tiefenboeck, T.M. Cutting Through Time: A Surgical Comparison of Bosworth, LARS™, and TightRope® for AC Joint Dislocations. J. Funct. Morphol. Kinesiol. 2025, 10, 375. https://doi.org/10.3390/jfmk10040375
Popp D, Nia A, Silvaieh S, Nass C, Heisinger S, Pichler L, Tiefenboeck TM. Cutting Through Time: A Surgical Comparison of Bosworth, LARS™, and TightRope® for AC Joint Dislocations. Journal of Functional Morphology and Kinesiology. 2025; 10(4):375. https://doi.org/10.3390/jfmk10040375
Chicago/Turabian StylePopp, Domenik, Arastoo Nia, Sara Silvaieh, Cornelia Nass, Stephan Heisinger, Lorenz Pichler, and Thomas M. Tiefenboeck. 2025. "Cutting Through Time: A Surgical Comparison of Bosworth, LARS™, and TightRope® for AC Joint Dislocations" Journal of Functional Morphology and Kinesiology 10, no. 4: 375. https://doi.org/10.3390/jfmk10040375
APA StylePopp, D., Nia, A., Silvaieh, S., Nass, C., Heisinger, S., Pichler, L., & Tiefenboeck, T. M. (2025). Cutting Through Time: A Surgical Comparison of Bosworth, LARS™, and TightRope® for AC Joint Dislocations. Journal of Functional Morphology and Kinesiology, 10(4), 375. https://doi.org/10.3390/jfmk10040375







