Biomechanical Alterations in the Unweight Phase of the Single-Leg Countermovement Jump After ACL Reconstruction
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Consideration and Study Design
2.2. Inclusion and Exclusion Criteria
2.3. Assessments and Instruments
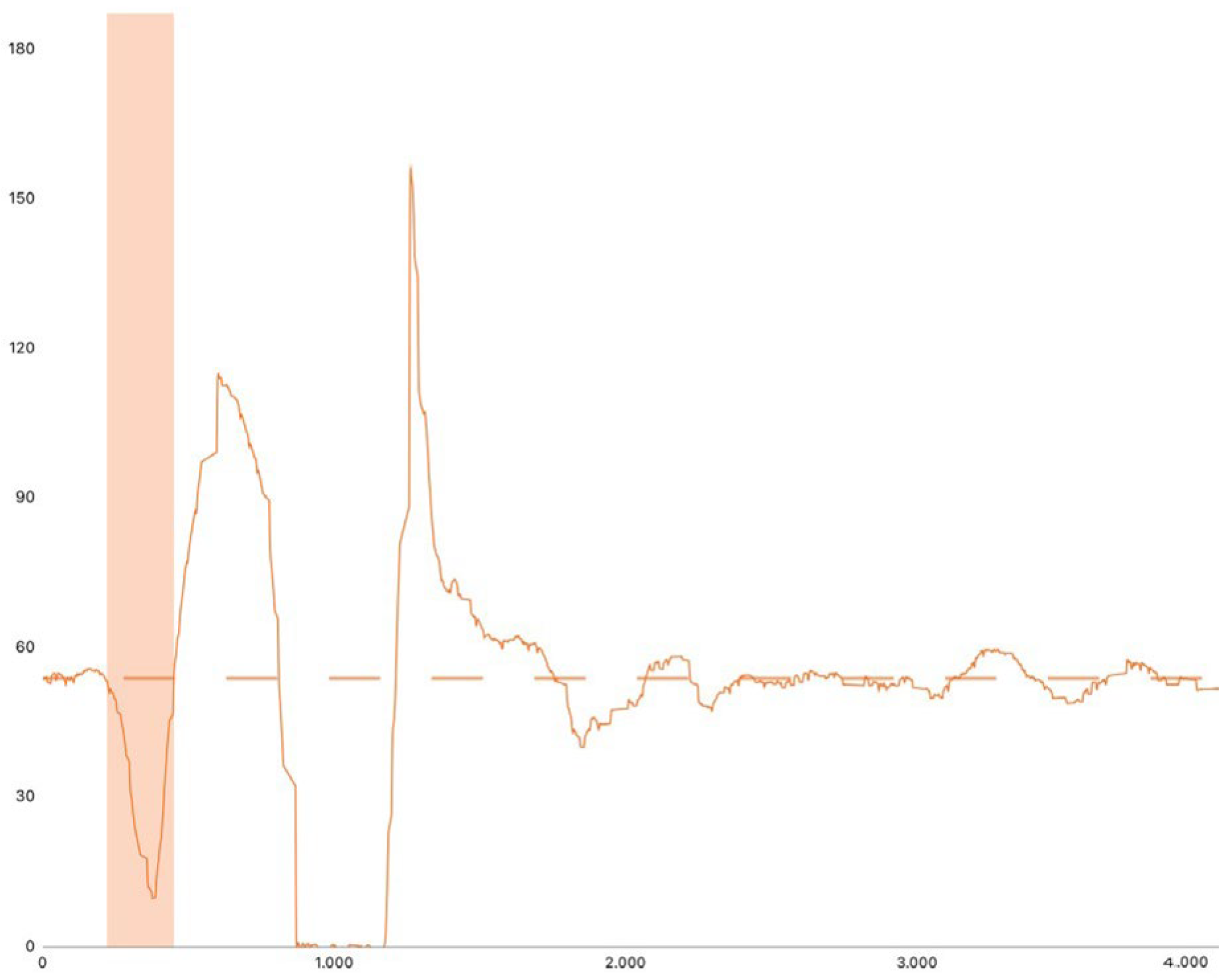
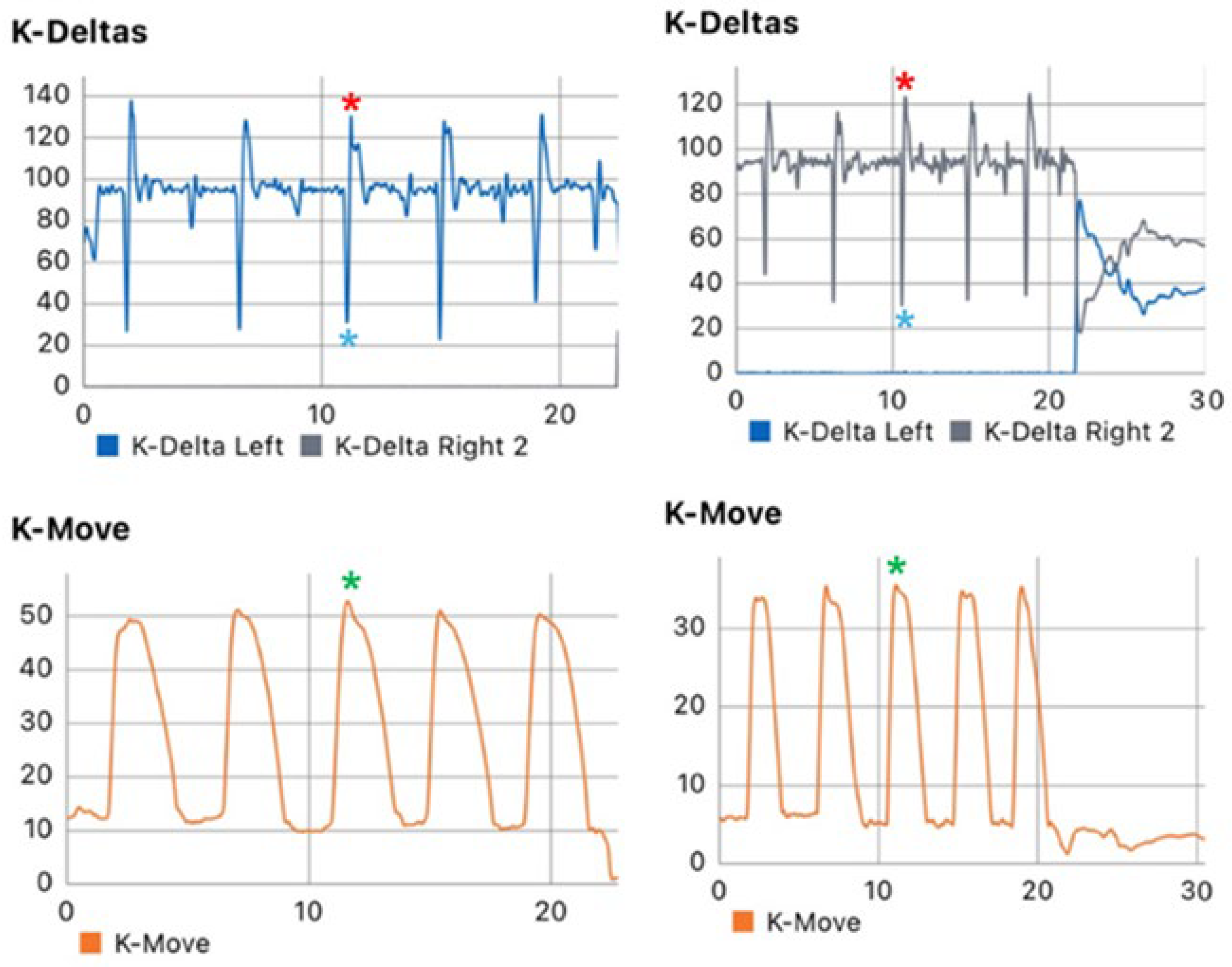
2.4. SLCMJ Metrics
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Limitations
4.2. Practical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACLr | anterior cruciate ligament reconstruction |
| ACL | anterior cruciate ligament |
| BW | body weight |
| CMJ | countermovement jump |
| COM | center of mass |
| MCID | minimum clinically important difference |
| SD | standard deviation |
| SLCMJ | single-leg countermovement jump |
| TAS | Tegner Activity Score |
| VJH | vertical jump height |
References
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Webster, K.E. Fifty-Five per Cent Return to Competitive Sport Following Anterior Cruciate Ligament Reconstruction Surgery: An Updated Systematic Review and Meta-Analysis Including Aspects of Physical Functioning and Contextual Factors. Br. J. Sports Med. 2014, 48, 1543–1552. [Google Scholar] [CrossRef]
- Manojlovic, M.; Ninkovic, S.; Matic, R.; Versic, S.; Modric, T.; Sekulic, D.; Drid, P. Return to Play and Performance After Anterior Cruciate Ligament Reconstruction in Soccer Players: A Systematic Review of Recent Evidence. Sports Med. 2024, 54, 2097–2108. [Google Scholar] [CrossRef]
- Rodriguez-Merchan, E.C.; Valentino, L.A. Return to Sport Activities and Risk of Reinjury Following Primary Anterior Cruciate Ligament Reconstruction. Arch. Bone Jt. Surg. 2022, 10, 648–660. [Google Scholar] [CrossRef]
- Boden, B.P.; Sheehan, F.T. Mechanism of Non-Contact ACL Injury: OREF Clinical Research Award 2021. J. Orthop. Res. 2022, 40, 531–540. [Google Scholar] [CrossRef]
- McBurnie, A.J.; Harper, D.J.; Jones, P.A.; Dos’Santos, T. Deceleration Training Team Sports: Another Potential ‘Vaccine’ for Sports-Related Injury? Sports Med. 2022, 52, 1–12. [Google Scholar] [CrossRef]
- Moiroux-Sahraoui, A.; Forelli, F.; Mazeas, J.; Rambaud, A.J.M.; Bjerregaard, A.; Riera, J. Quadriceps Activation After Anterior Cruciate Ligament Reconstruction: The Early Bird Gets the Worm! Int. J. Sports Phys. Ther. 2024, 19, 1044–1051. [Google Scholar] [CrossRef]
- Linthorne, N.P. Analysis of Standing Vertical Jumps Using a Force Platform. Am. J. Phys. 2001, 69, 1198–1204. [Google Scholar] [CrossRef]
- Kibele, A. Possibilities and Limitations in the Biomechanical Analysis of Countermovement Jumps: A Methodological Study. J. Appl. Biomech. 1998, 14, 105–117. [Google Scholar] [CrossRef]
- Markström, J.L.; Olsson, C.J. Countermovement Jump Peak Force Relative to Body Weight and Jump Height as Predictors for Sprint Running Performances: (In)Homogeneity of Track and Field Athletes? J. Strength. Cond. Res. 2013, 27, 944–953. [Google Scholar] [CrossRef]
- Comfort, P.; Stewart, A.; Bloom, L.; Clarkson, B. Relationships between Strength, Sprint, and Jump Performance in Well-Trained Youth Soccer Players. J. Strength. Cond. Res. 2014, 28, 173–177. [Google Scholar] [CrossRef]
- Bishop, C.; Turner, A.; Jordan, M.; Harry, J.; Loturco, I.; Lake, J.; Comfort, P. A Framework to Guide Practitioners for Selecting Metrics during the Countermovement and Drop Jump Tests. Strength. Cond. J. 2022, 44, 95–103. [Google Scholar] [CrossRef]
- Labban, W.; Stadnyk, M.; Sommerfeldt, M.; Nathanail, S.; Dennett, L.; Westover, L.; Manaseer, T.; Beaupre, L. Kinetic Measurement System Use in Individuals Following Anterior Cruciate Ligament Reconstruction: A Scoping Review of Methodological Approaches. J. Exp. Orthop. 2021, 8, 81. [Google Scholar] [CrossRef] [PubMed]
- Kotsifaki, A.; Korakakis, V.; Graham-Smith, P.; Sideris, V.; Whiteley, R. Vertical and Horizontal Hop Performance: Contributions of the Hip, Knee, and Ankle. Sports Health 2021, 13, 128–135. [Google Scholar] [CrossRef] [PubMed]
- McMahon, J.J.; Suchomel, T.J.; Lake, J.P.; Comfort, P. Understanding the Key Phases of the Countermovement Jump Force-Time Curve. Strength. Cond. J. 2018, 40, 96–106. [Google Scholar] [CrossRef]
- Labban, W.; Manaseer, T.; Golberg, E.; Sommerfeldt, M.; Nathanail, S.; Dennett, L.; Westover, L.; Beaupre, L. Jumping into Recovery: A Systematic Review and Meta-Analysis of Discriminatory and Responsive Force Plate Parameters in Individuals Following Anterior Cruciate Ligament Reconstruction during Countermovement and Drop Jumps. J. Exp. Orthop. 2024, 11, e12018. [Google Scholar] [CrossRef]
- Chavda, S.; Bromley, T.; Jarvis, P.; Williams, S.; Bishop, C.; Turner, A.N.; Lake, J.P.; Mundy, P.D. Force-Time Characteristics of the Countermovement Jump: Analyzing the Curve in Excel. Strength. Cond. J. 2018, 40, 67–77. [Google Scholar] [CrossRef]
- González-García, J.; Conejero, M.; Gutiérrez-Hellín, J. Assessing Jump Performance: Intra- and Interday Reliability and Minimum Difference of Countermovement Jump and Drop Jump Outcomes, Kinetics, Kinematics, and Jump Strategy. Appl. Sci. 2024, 14, 2662. [Google Scholar] [CrossRef]
- O’Malley, E.; Richter, C.; King, E.; Strike, S.; Moran, K.; Franklyn-Miller, A.; Moran, R. Countermovement Jump and Isokinetic Dynamometry as Measures of Rehabilitation Status After Anterior Cruciate Ligament Reconstruction. J. Athl. Train. 2018, 53, 687–695. [Google Scholar] [CrossRef]
- Bishop, C.; Jordan, M.; Torres-Ronda, L.; Loturco, I.; Harry, J.; Virgile, A.; Mundy, P.; Turner, A.; Comfort, P. Selecting Metrics That Matter: Comparing the Use of the Countermovement Jump for Performance Profiling, Neuromuscular Fatigue Monitoring, and Injury Rehabilitation Testing. Strength. Cond. J. 2023, 45, 545–553. [Google Scholar] [CrossRef]
- Kotsifaki, R.; Sideris, V.; King, E.; Bahr, R.; Whiteley, R. Performance and Symmetry Measures during Vertical Jump Testing at Return to Sport after ACL Reconstruction. Br. J. Sports Med. 2023, 57, 1304–1310. [Google Scholar] [CrossRef]
- Maestroni, L.; Turner, A.; Papadopoulos, K.; Pedley, J.; Sideris, V.; Read, P. Single Leg Drop Jump Is Affected by Physical Capacities in Male Soccer Players Following ACL Reconstruction. Sci. Med. Footb. 2024, 8, 201–211. [Google Scholar] [CrossRef]
- Welling, W.; Benjaminse, A.; Seil, R.; Lemmink, K.; Zaffagnini, S.; Gokeler, A. Low Rates of Patients Meeting Return to Sport Criteria 9 Months after Anterior Cruciate Ligament Reconstruction: A Prospective Longitudinal Study. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3636–3644. [Google Scholar] [CrossRef]
- Warnecke, B.F.; Richter, C.; King, E.; Paternoster, F.K. Residual Performance and Biomechanical Asymmetries During Jumping Tasks in Female Athletes at 9 Months After Anterior Cruciate Ligament Reconstruction. Orthop. J. Sports Med. 2024, 12. [Google Scholar] [CrossRef]
- Jordan, M.J.; Morris, N.; Nimphius, S.; Aagaard, P.; Herzog, W. Attenuated Lower Limb Stretch-Shorten-Cycle Capacity in ACL Injured vs. Non-Injured Female Alpine Ski Racers: Not Just a Matter of Between-Limb Asymmetry. Front. Sports Act. Living 2022, 4, 853701. [Google Scholar] [CrossRef]
- Read, P.J.; Michael Auliffe, S.; Wilson, M.G.; Graham-Smith, P. Lower Limb Kinetic Asymmetries in Professional Soccer Players with and Without Anterior Cruciate Ligament Reconstruction: Nine Months Is Not Enough Time to Restore “Functional” Symmetry or Return to Performance. Am. J. Sports Med. 2020, 48, 1365–1373. [Google Scholar] [CrossRef] [PubMed]
- Owen, N.J.; Watkins, J.; Kilduff, L.P.; Bevan, H.R.; Bennett, M.A. Development of a Criterion Method to Determine Peak Mechanical Power Output in a Countermovement Jump. J. Strength. Cond. Res. 2014, 28, 1552–1558. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Castilla, A.; Weakley, J.; García-Pinillos, F.; Rojas, F.J.; García-Ramos, A. Influence of Countermovement Depth on the Countermovement Jump-Derived Reactive Strength Index Modified. Eur. J. Sport. Sci. 2021, 21, 1606–1616. [Google Scholar] [CrossRef] [PubMed]
- Bagchi, A.; Raizada, S.; Thapa, R.K.; Stefanica, V.; Ceylan, H.İ. Reliability and Accuracy of Portable Devices for Measuring Countermovement Jump Height in Physically Active Adults: A Comparison of Force Platforms, Contact Mats, and Video-Based Software. Life 2024, 14, 1394. [Google Scholar] [CrossRef]
- Moiroux--Sahraoui, A.; Mazeas, J.; Gold, M.; Kakavas, G.; Forelli, F. Neuromuscular Control Deficits After Anterior Cruciate Ligament Reconstruction: A Pilot Study Using Single-Leg Functional Tests and Electromyography. J. Funct. Morphol. Kinesiol. 2025, 10, 98. [Google Scholar] [CrossRef]
- McMahon, J.J.; Rej, S.J.E.; Comfort, P. Sex Differences in Countermovement Jump Phase Characteristics. Sports 2017, 5, 8. [Google Scholar] [CrossRef]
- Bishop, C.; Turner, A.; Jarvis, P.; Chavda, S.; Read, P. Considerations for Selecting Field-Based Strength and Power Fitness Tests to Measure Asymmetries. J. Strength. Cond. Res. 2017, 31, 2635–2644. [Google Scholar] [CrossRef]
- Legnani, C.; Del Re, M.; Peretti, G.M.; Borgo, E.; Macchi, V.; Ventura, A. Limb Asymmetries Persist 6 Months after Anterior Cruciate Ligament Reconstruction According to the Results of a Jump Test Battery. Front. Med. 2024, 11, 1303172. [Google Scholar] [CrossRef]
- Mengis, N.; Schmidt, S.; Ellermann, A.; Sobau, C.; Egloff, C.; Kreher, M.M.; Ksoll, K.; Schmidt-Lucke, C.; Rippke, J.N. A Novel Sensor-Based Application for Home-Based Rehabilitation Can Objectively Measure Postoperative Outcomes Following Anterior Cruciate Ligament Reconstruction. J. Pers. Med. 2023, 13, 1398. [Google Scholar] [CrossRef]
- Lisee, C.; Lepley, A.S.; Birchmeier, T.; O’Hagan, K.; Kuenze, C. Quadriceps Strength and Volitional Activation After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. Sports Health 2019, 11, 163–179. [Google Scholar] [CrossRef]



| Phase | Description |
|---|---|
| Generalized warm-up | 10 min exercise bike |
| Specific warm-up | 2 sets of 10 bilateral squats, lunges and push-ups (total sets and reps are 6 and 60, respectively) |
| Familiarization trials | 2 SLCMJ trials with each leg |
| Indications | Arms on hips, leg in the front at 45° hip flexion, no swing accepted |
| Execution order | First, healthy leg |
| Cue | “Go down and up as fast as you can and jump as high as you can” |
| Number of trials | 2 |
| Value | Best of two |
| Rest between trials | 30 s |
| Characteristics | Total Sample (n = 53) |
|---|---|
| Age (Yr), mean ± SD | 25.98±5.58 |
| Gender | |
| Male, n (%) | 41 (78.8) |
| Female, n (%) | 11 (21.2) |
| Weight (Kg), mean ± SD | 78.94 ± 8.85 |
| Height (cm), mean ± SD | 177.94 ± 7.77 |
| Graft type | |
| R HT/G, n (%) | 26 (50.0) |
| L HT/G, n (%) | 20 (38.5) |
| R PTBT, n (%) | 4 (7.7) |
| L PTBT | 1 (1.9) |
| Quadriceps (QT), n (%) | 1 (1.9) |
| Time from surgery (months), mean ± SD | 7.73 ± 0.95 |
| Sport Activity | |
| Soccer, n (%) | 20 (38.5) |
| Basketball, n (%) | 12 (23.1) |
| Volleyball, n (%) | 7 (13.5) |
| Futsal, n (%) | 3 (5.8) |
| CrossFit, n (%) | 3 (5.8) |
| Surf, n (%) | 2 (3.8) |
| Box, n (%) | 2 (3.8) |
| Ski, n (%) | 1 (1.9) |
| Touch rugby, n (%) | 1 (1.9) |
| Surf, n (%) | 1 (1.9) |
| TAS level, mean ± SD | 7.46 ± 1.58 |
| Jump Metrics | Total Sample (n = 53) | p-Value | |
|---|---|---|---|
| ACLr Side | Healthy Side | ||
| Height (cm), n ± SD | 12.90 ± 4.22 | 15.27 ± 4.03 | <0.001 * |
| COM displacement (cm), n ± SD | −17.62 ± 6.25 | −19.73 ± 5.34 | 0.014 * |
| Negative velocity peak (m/s), n ± SD | −0.80 ± 0.40 | −0.94 ± 0.40 | <0.001 ** |
| Minimum force (Kg), n ± SD | 36.75 ± 17.88 | 32.05 ± 17.25 | <0.001 * |
| Eccentric phase duration (ms) | 202.79 ± 83.76 | 212.33 ± 88.11 | 0.290 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ricupito, R.; Bravi, M.; Santacaterina, F.; Campardo, G.; Guarise, R.; Castellucci, R.; Alaoui, I.B.; Forelli, F. Biomechanical Alterations in the Unweight Phase of the Single-Leg Countermovement Jump After ACL Reconstruction. J. Funct. Morphol. Kinesiol. 2025, 10, 296. https://doi.org/10.3390/jfmk10030296
Ricupito R, Bravi M, Santacaterina F, Campardo G, Guarise R, Castellucci R, Alaoui IB, Forelli F. Biomechanical Alterations in the Unweight Phase of the Single-Leg Countermovement Jump After ACL Reconstruction. Journal of Functional Morphology and Kinesiology. 2025; 10(3):296. https://doi.org/10.3390/jfmk10030296
Chicago/Turabian StyleRicupito, Roberto, Marco Bravi, Fabio Santacaterina, Giandomenico Campardo, Riccardo Guarise, Rosalba Castellucci, Ismail Bouzekraoui Alaoui, and Florian Forelli. 2025. "Biomechanical Alterations in the Unweight Phase of the Single-Leg Countermovement Jump After ACL Reconstruction" Journal of Functional Morphology and Kinesiology 10, no. 3: 296. https://doi.org/10.3390/jfmk10030296
APA StyleRicupito, R., Bravi, M., Santacaterina, F., Campardo, G., Guarise, R., Castellucci, R., Alaoui, I. B., & Forelli, F. (2025). Biomechanical Alterations in the Unweight Phase of the Single-Leg Countermovement Jump After ACL Reconstruction. Journal of Functional Morphology and Kinesiology, 10(3), 296. https://doi.org/10.3390/jfmk10030296







