Superficial Arterial Variants of the Upper Limb: Clinical Implications of High-Origin Ulnar and Radial Arteries Detected by Ultrasound and Anatomy Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Samples
2.2. Ultrasound Study
2.3. Anatomical Study
3. Results
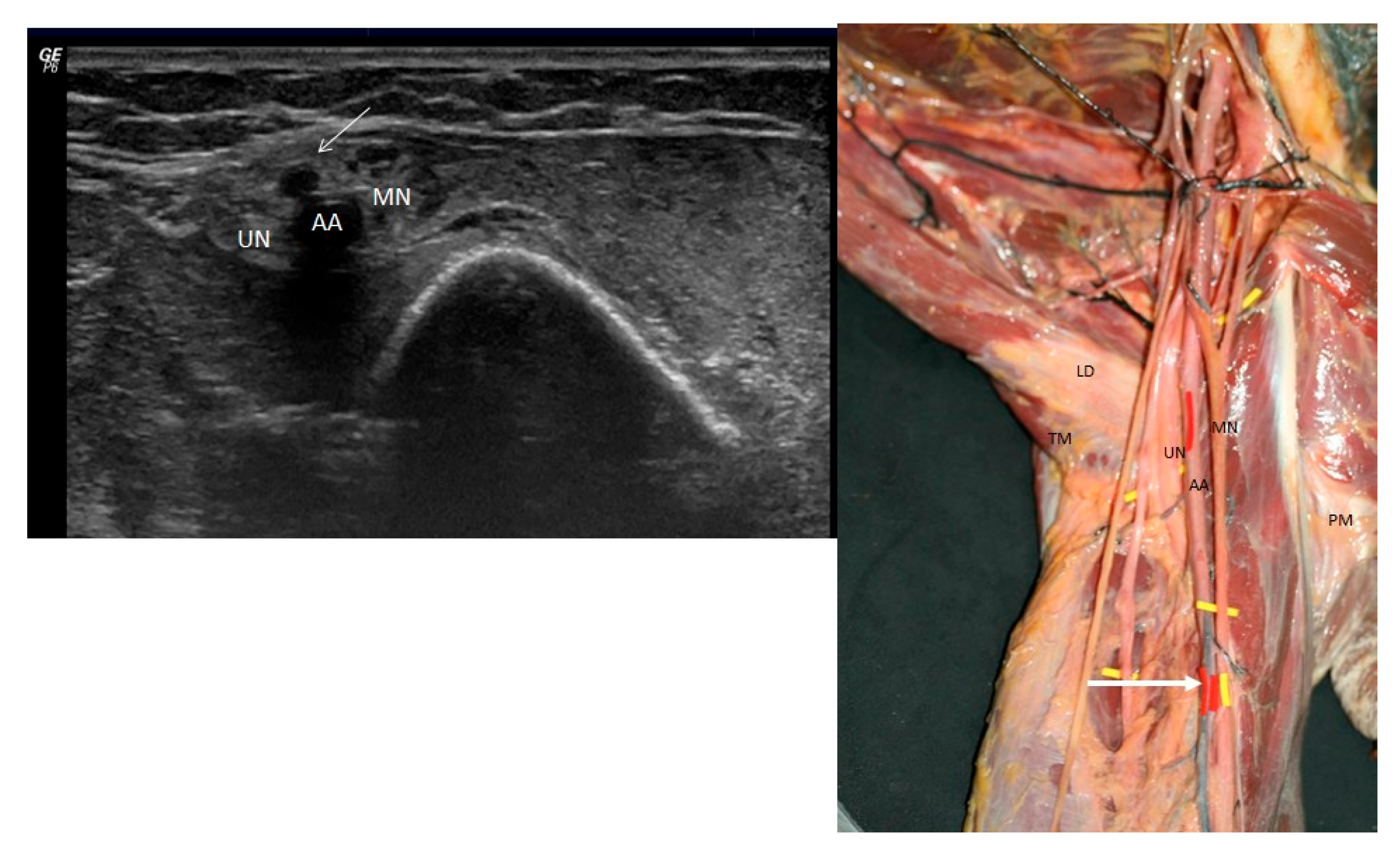
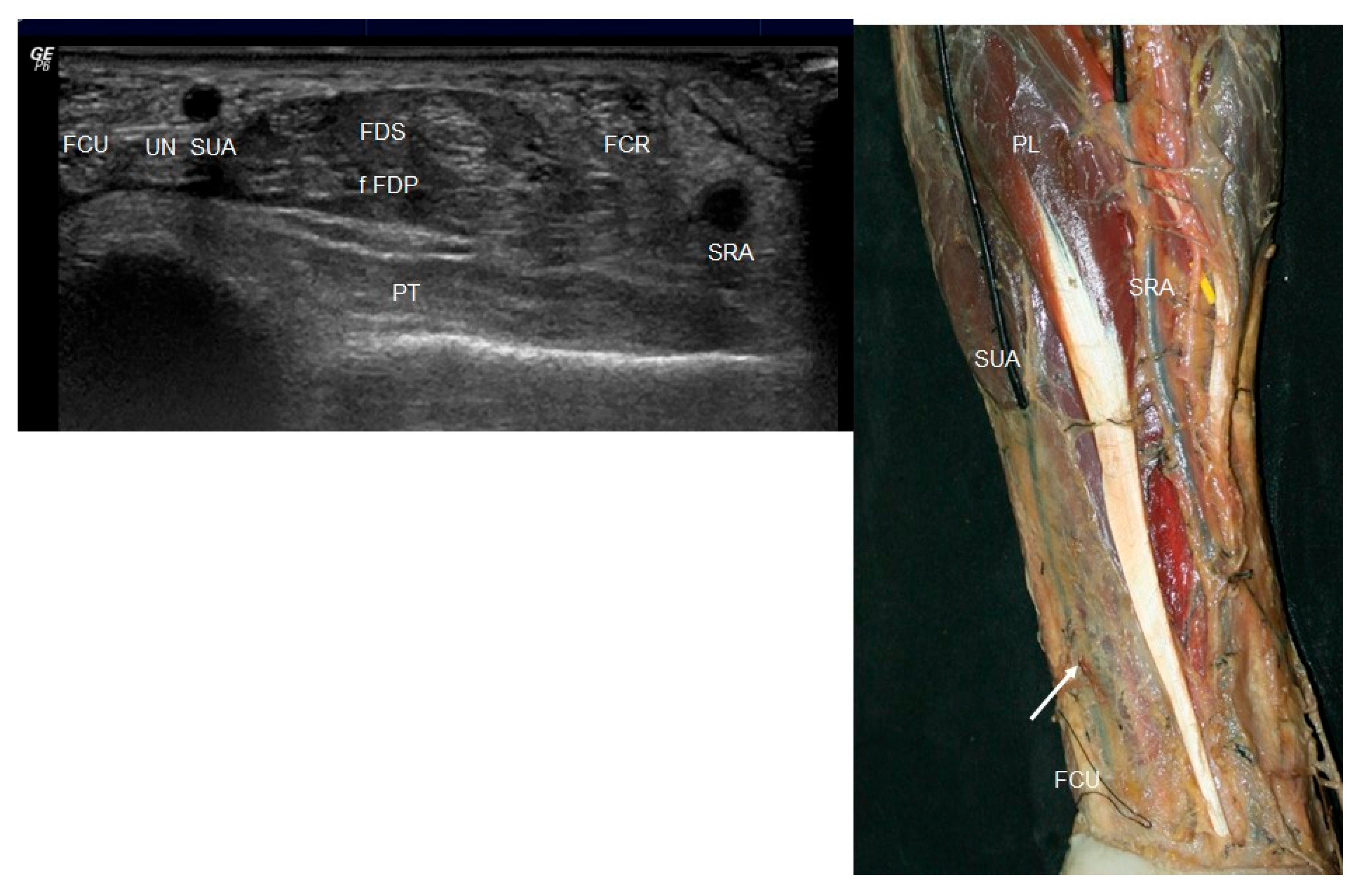
3.1. Ultrasound Study
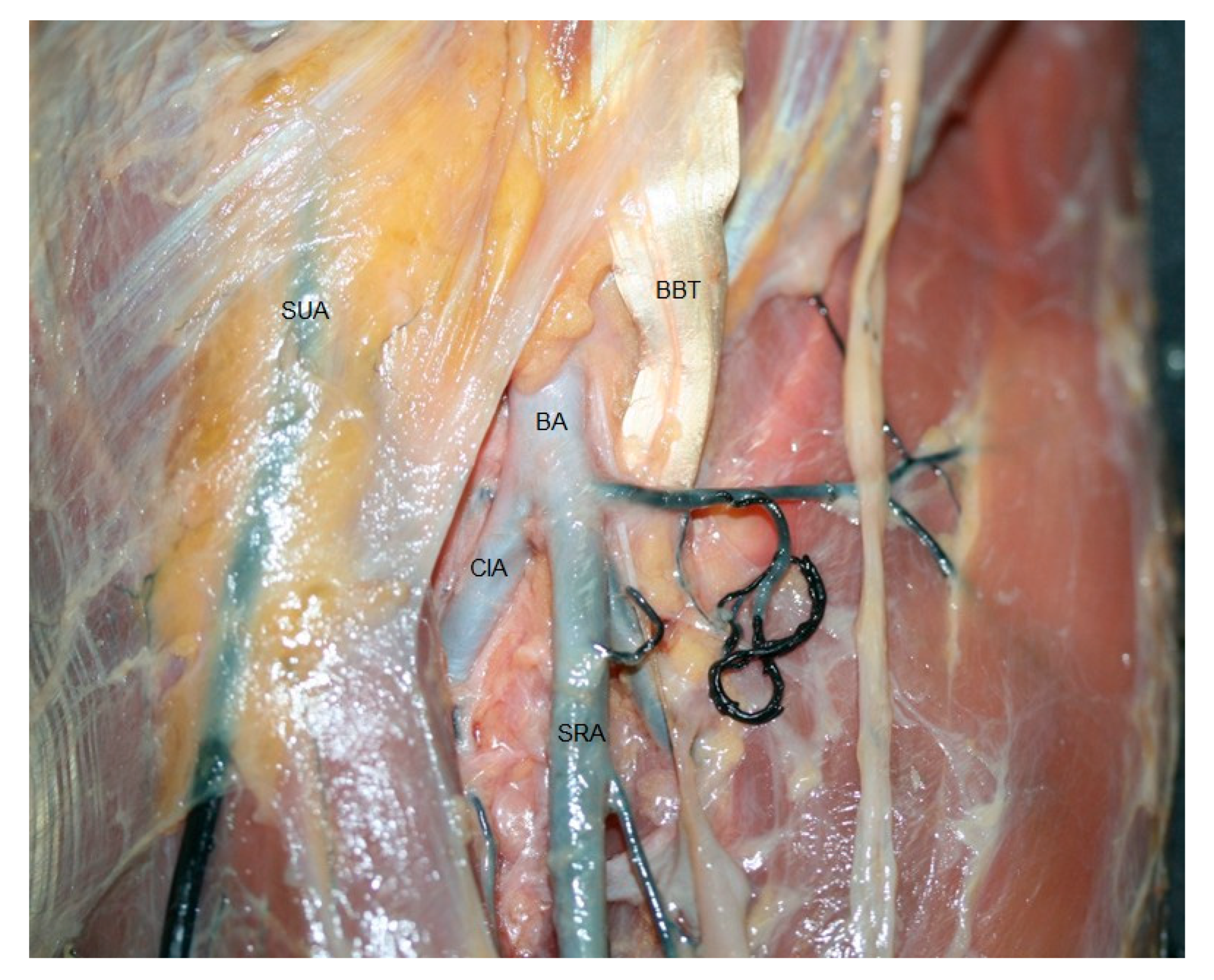
3.2. Anatomical Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CIA | Common interosseous artery |
| US | Ultrasound |
| SRA | Superficial radial artery |
| SUA | Superficial ulnar artery |
References
- Quadros, L.S.; Bhat, N.; D’Souza, A.S. Superficial Ulnar Artery: A Case Report of its Unusual Course. Malays. Med. Sci. 2015, 22, 65–67. [Google Scholar]
- Rodríguez-Niedenführ, M.; Vázquez, T.; Nearn, L.; Ferreira, B.; Parkin, I.; Sañudo, J.R. Variations of the arterial pattern in the upper limb revisited: A morphological and statistical study, with a review of the literature. J. Anat. 2001, 199 Pt 5, 547–566. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Aggarwal, A.; Gupta, T.; Kaur, H.; Gaba, S.; Sahni, D. Superficial upper limb vasculature and its surgical implications. Indian. J. Plast. Surg. 2016, 49, 258–260. [Google Scholar] [CrossRef] [PubMed]
- Mannan, A.; Sarikcioglu, L.; Ghani, S.; Hunter, A. Superficial ulnar artery terminating in a normal ulnar artery. Clin. Anat. 2005, 8, 602–605. [Google Scholar] [CrossRef] [PubMed]
- Sieg, P.; Jacobsen, H.C.; Hakim, S.G.; Hermes, D. Superficial ulnar artery: Curse or blessing in harvesting fasciocutaneous forearm flaps. Head Neck 2006, 28, 447–452. [Google Scholar] [CrossRef] [PubMed]
- Jacquemin, G.; Lemaire, V.; Medot, M.; Fissette, J. Bilateral case of superficial ulnar artery originating from axillary artery. Surg. Radiol. Anat. 2001, 23, 139–143. [Google Scholar] [CrossRef] [PubMed]
- McWilliams, R.G.; Sodha, I. Doppler ultrasound diagnosis of a superficial ulnar artery. Eur. J. Ultrasound. 2000, 12, 155–157. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.A.; Mathangasinghe, Y.; Gonsalvez, D. Rare bilateral vascular variations of the upper limb: A cadaveric case study. J. Cardiothorac. Surg. 2024, 19, 683. [Google Scholar] [CrossRef] [PubMed]
- Vollala, V.R.; Jetti, R.; Soni, S. High origin of an ulnar artery development and surgical significance. Chang. Gung Med. J. 2011, 34, 39–42. [Google Scholar] [PubMed]
- Sato, K.; Murakami, K.; Mimata, Y.; Kikuchi, Y.; Oikawa, R.; Doita, M. Superficial ulnar artery crossing over the palmaris longus thedon at the wrist in a cadaver: A case report. J. Hand Surg. Asian-Pac. Vol. 2018, 23, 137–139. [Google Scholar] [CrossRef] [PubMed]
- Bhat, K.M.; Potu, B.K.; Gowda, S. High origin of ulnar artery on South Indian male cadaver: A case report. Rom. J. Morphol. Embryol. 2008, 49, 573–575. [Google Scholar] [PubMed]
- Chin, K.J.; Singh, K. The superficial ulnar artery—A potential hazard in patients with difficult venous access. Br. J. Anaesth. 2005, 94, 692–693. [Google Scholar] [CrossRef] [PubMed]
- Williams, P.L.; Bannister, L.H.; Berry, M.M.; Collins, P.; Dyson, M.; Dussek, J.E.; Ferguson, M.W. Angiology. Gray’s Anatomy, 38th ed.; Churchill Livingstone: Edinburgh, UK, 1995; p. 1539. [Google Scholar]
- Cherian, S.B.; Nayak, S.B.; Somayaji, N. Superficial course of brachial and ulnar arteries and high origin of common interosseous artery. Int. J. Anat. Var. (IJAV) 2009, 2, 4–6. [Google Scholar]
- Sirasanagandla, S.R.; Pamidi, N.; Nayak, S.B.; Jetti, R.; Thangarajan, R. Superficial ulnar artery associated with anomalous origin of the common interosseous and ulnar recurrent arteries. J. Clin. Diagn. Res. 2016, 10, AD01–AD02. [Google Scholar] [CrossRef] [PubMed]
- Narayanan, S.; Murugan, S. Bifurcation of brachial artery into a common radial-interosseous trunk and superficial ulnar artery: A rare variation. Anat. Sci. Int. 2018, 93, 400–403. [Google Scholar] [CrossRef] [PubMed]
- Yazar, F.; Kirici, Y.; Ozan, H.; Aldur, M.M. An unusual variation of the superficial ulnar artery. Surg. Radiol. Anat. 1999, 21, 155–157. [Google Scholar] [CrossRef] [PubMed]
- Yadav, P.S.; Ahmad, Q.G.; Shankhdhar, V.K.; Nambi, G.I. Absence of the palmaris longus is a warning sign for avoiding the superficial ulnar artery “trap”. Indian. J. Plast. Surg. 2013, 46, 149–150. [Google Scholar] [CrossRef] [PubMed]
- Bondaz, M.; Lepivert, J.C.; Majoufre-Lefebvre, C.; Sessicq, Q. Superficial ulnar artery: Case Report. Rev. Stomalog. Chr. Maxillofac. Chir. Orale 2016, 117, 173–175. [Google Scholar] [CrossRef]
- Jaquemin Ohana, E.; Sheiner, E.; Gurman, G.M. Accidental intra-arterial injection of propofol. Eur. J. Anaesthesiol. 1999, 16, 569–570. [Google Scholar] [CrossRef]
- Goldberg, I.; Bahar, A.; Yosipovitch, Z. Gangrene of upper extremity following intra-arterial injection of drugs. A case report and review of the literature. Clin. Orthop. Relat. Res. 1984, 188, 223–229. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miguel-Pérez, M.; Ortiz-Miguel, S.; Martínez, A.; Ortiz-Sagristà, J.C.; Möller, I.; Martinoli, C.; Pérez-Bellmunt, A. Superficial Arterial Variants of the Upper Limb: Clinical Implications of High-Origin Ulnar and Radial Arteries Detected by Ultrasound and Anatomy Study. J. Funct. Morphol. Kinesiol. 2025, 10, 246. https://doi.org/10.3390/jfmk10030246
Miguel-Pérez M, Ortiz-Miguel S, Martínez A, Ortiz-Sagristà JC, Möller I, Martinoli C, Pérez-Bellmunt A. Superficial Arterial Variants of the Upper Limb: Clinical Implications of High-Origin Ulnar and Radial Arteries Detected by Ultrasound and Anatomy Study. Journal of Functional Morphology and Kinesiology. 2025; 10(3):246. https://doi.org/10.3390/jfmk10030246
Chicago/Turabian StyleMiguel-Pérez, Maribel, Sara Ortiz-Miguel, Ana Martínez, Juan Carlos Ortiz-Sagristà, Ingrid Möller, Carlo Martinoli, and Albert Pérez-Bellmunt. 2025. "Superficial Arterial Variants of the Upper Limb: Clinical Implications of High-Origin Ulnar and Radial Arteries Detected by Ultrasound and Anatomy Study" Journal of Functional Morphology and Kinesiology 10, no. 3: 246. https://doi.org/10.3390/jfmk10030246
APA StyleMiguel-Pérez, M., Ortiz-Miguel, S., Martínez, A., Ortiz-Sagristà, J. C., Möller, I., Martinoli, C., & Pérez-Bellmunt, A. (2025). Superficial Arterial Variants of the Upper Limb: Clinical Implications of High-Origin Ulnar and Radial Arteries Detected by Ultrasound and Anatomy Study. Journal of Functional Morphology and Kinesiology, 10(3), 246. https://doi.org/10.3390/jfmk10030246






