Gender-Based Differences in Biomechanical Walking Patterns of Athletes Using Inertial Sensors
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instrumentations
2.3. Acquisition Protocol
2.4. Data Analysis
- a.
- Global analysis parameters:
- “Cadence” (steps/min): Represents the number of steps taken in one minute.
- “Speed” (m/s): Indicates the average walking speed.
- “Symmetry Index of gait cycle”: Quantifies the percentage (%) of symmetry between the anterior/posterior acceleration curves during the right and left gait cycles.
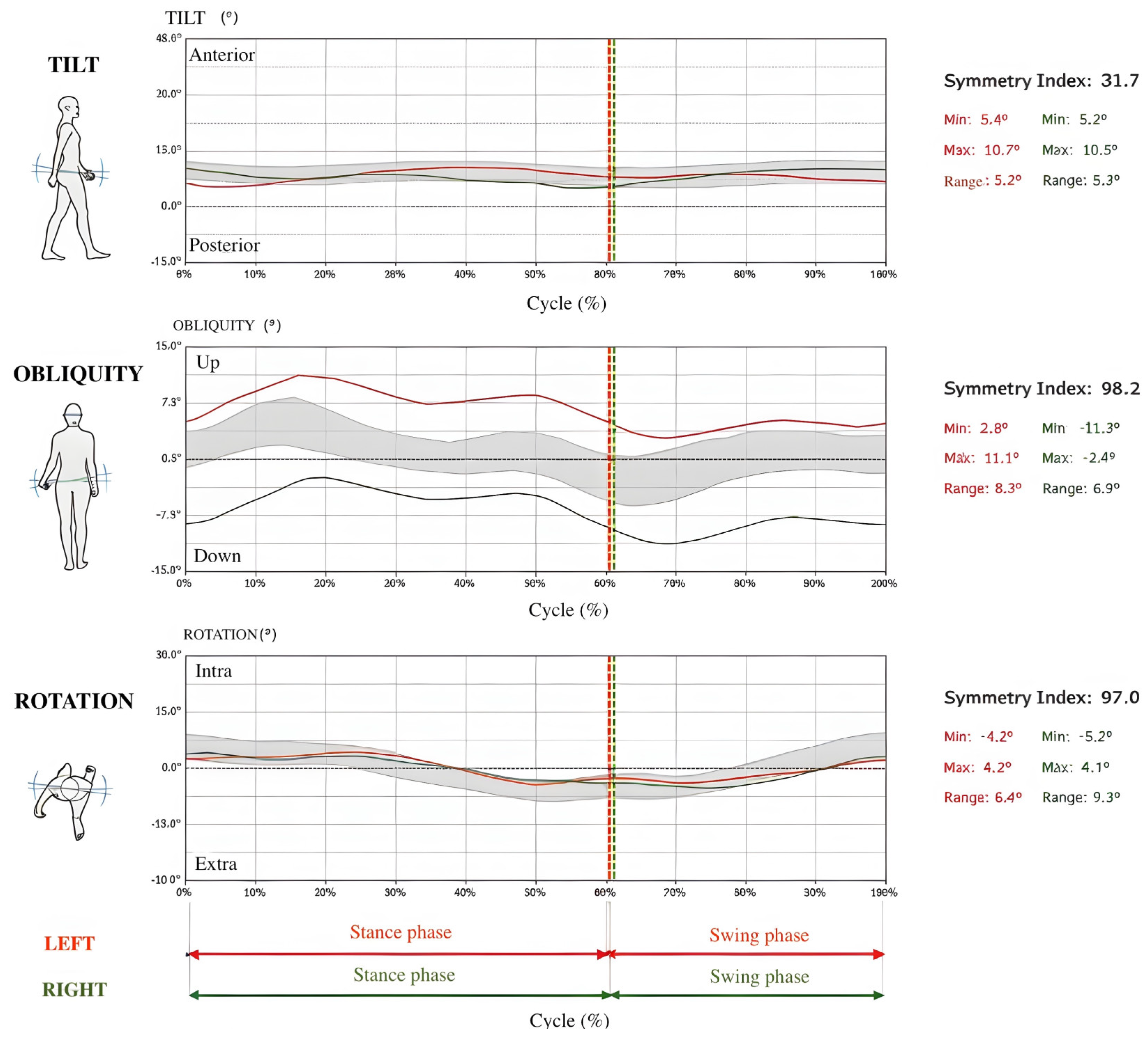
- “Symmetry index of pelvic angles (tilt, obliquity, rotation)”: Evaluates the percentage (%) of similarity or dissimilarity between the pelvic angles recorded during the right and left gait cycles. The pelvic angles are usually measured in three main body planes: sagittal (tilt), frontal (obliquity), and transverse (rotation) (see example in Figure 1).
- b.
- Parameters categorized for the LEFT and RIGHT sides:
- “Stride length” (m): Represents the average distance between each initial contact and the subsequent contact of the same side during walking.
- “%Stride length” (%height): Represents the normalized stride length over the individual’s height.
- “Gait cycle duration (s)”: Represents the average time interval between two consecutive heel strikes of the same foot.
- “Step length (% str. length)”: Shows the average distance between each initial contact and the next contact made by the opposing side.
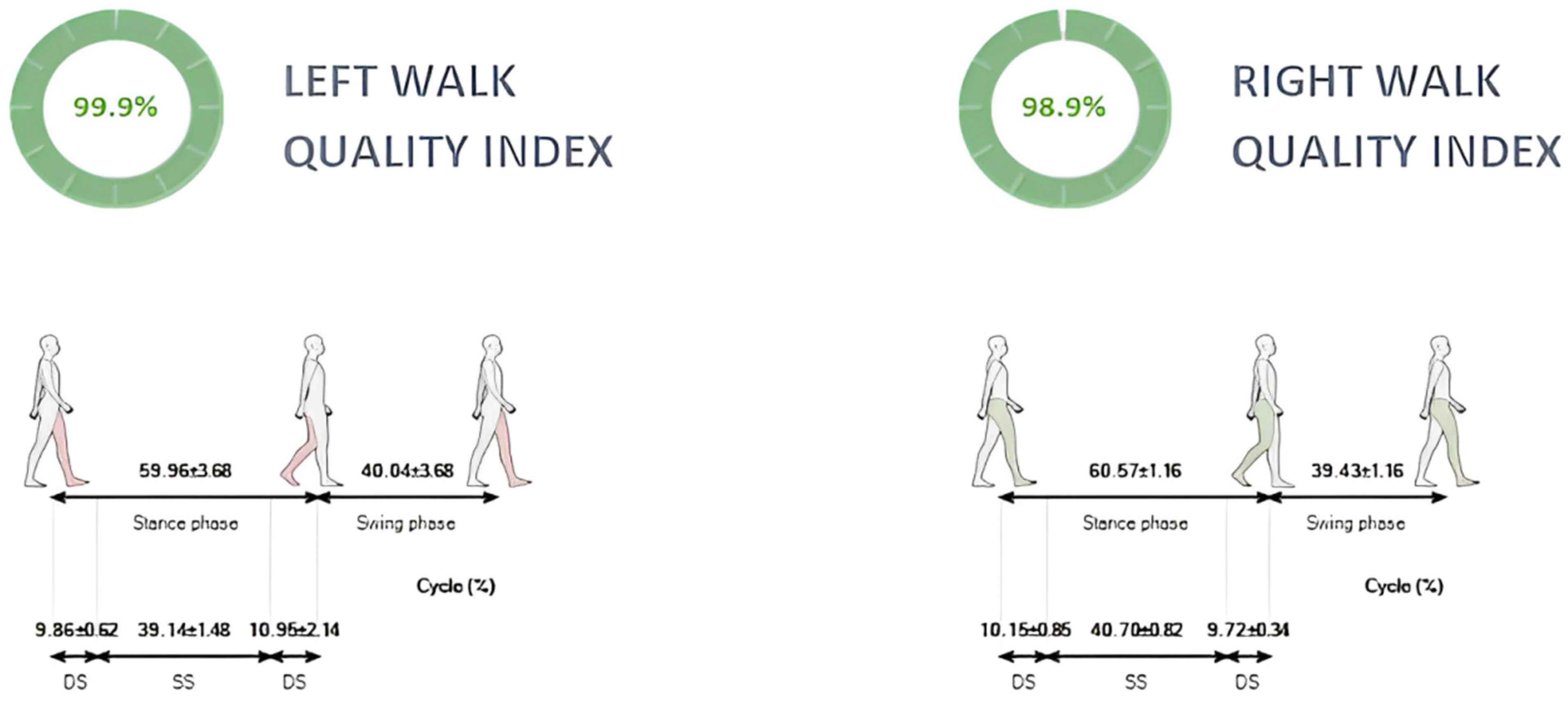
- “Stance phase (% cycle)”: Represents the average duration of the right and left foot support phases as a percentage of the gait cycle.
- “Swing phase (% cycle)”: Represents the average duration of the right and left swing phases as a percentage of the gait cycle.
- “Double support phase (% cycle)”: Represents the average duration of the phase in which both feet are in stance position as a percentage of the gait cycle.
- “Single support phase (% cycle)”: Represents the average duration of the phase in which only one foot is in stance position as a percentage of the gait cycle.
- “Elaborated steps”: Refers to the number of strides considered in the analysis.
- “Propulsion index”: Represents the line’s actual inclination following the acceleration pattern’s rising edge.
- “Walk quality index”: A composite measure that quantifies the overall quality of an individual’s walking pattern by incorporating key gait parameters, such as step length, cadence, symmetry, and variability. This index provides a score that reflects the efficiency, stability, and symmetry of a person’s gait. Higher scores indicate more efficient, stable, and symmetrical walking patterns, whereas lower scores reflect less efficient, unstable, or more variable gait characteristics.
2.5. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lord, S.; Galna, B.; Verghese, J.; Coleman, S.; Burn, D.; Rochester, L. Independent Domains of Gait in Older Adults and Associated Motor and Nonmotor Attributes: Validation of a Factor Analysis Approach. J. Gerontol.—Ser. Biol. Sci. Med. Sci. 2013, 68, 820–827. [Google Scholar] [CrossRef] [PubMed]
- Viteckova, S.; Kutilek, P.; Svoboda, Z.; Krupicka, R.; Kauler, J.; Szabo, Z. Gait Symmetry Measures: A Review of Current and Prospective Methods. Biomed. Signal Process. Control 2018, 42, 89–100. [Google Scholar] [CrossRef]
- Verghese, J.; Wang, C.; Lipton, R.B.; Holtzer, R.; Xue, X. Quantitative Gait Dysfunction and Risk of Cognitive Decline and Dementia. J. Neurol. Neurosurg. Psychiatry 2007, 78, 929–935. [Google Scholar] [CrossRef] [PubMed]
- Beauchet, O.; Annweiler, C.; Dubost, V.; Allali, G.; Kressig, R.W.; Bridenbaugh, S.; Berrut, G.; Assal, F.; Herrmann, F.R. Stops Walking When Talking: A Predictor of Falls in Older Adults? Eur. J. Neurol. 2009, 16, 786–795. [Google Scholar] [CrossRef]
- Hirvensalo, M.; Rantanen, T.; Heikkinen, E. Mobility Difficulties and Physical Activity as Predictors of Mortality and Loss of Independence in the Community-Living Older Population. J. Am. Geriatr. Soc. 2000, 48, 493–498. [Google Scholar] [CrossRef]
- Studenski, S.; Perera, S.; Patel, K.; Rosano, C.; Faulkner, K.; Inzitari, M.; Brach, J.; Chandler, J.; Cawthon, P.; Connor, E.B.; et al. Gait Speed and Survival in Older Adults. JAMA 2011, 305, 50–58. [Google Scholar] [CrossRef]
- Lara, J.; Godfrey, A.; Evans, E.; Heaven, B.; Brown, L.J.E.; Barron, E.; Rochester, L.; Meyer, T.D.; Mathers, J.C. Towards Measurement of the Healthy Ageing Phenotype in Lifestyle-Based Intervention Studies. Maturitas 2013, 76, 189–199. [Google Scholar] [CrossRef]
- Buckley, C.; Alcock, L.; McArdle, R.; Ur Rehman, R.Z.; Del Din, S.; Mazzà, C.; Yarnall, A.J.; Rochester, L. The Role of Movement Analysis in Diagnosing and Monitoring Neurodegenerative Conditions: Insights from Gait and Postural Control. Brain Sci. 2019, 9, 34. [Google Scholar] [CrossRef]
- Mills, K.; Hunt, M.A.; Ferber, R. Biomechanical Deviations during Level Walking Associated with Knee Osteoarthritis: A Systematic Review and Meta-Analysis. Arthritis Care Res. 2013, 65, 1643–1665. [Google Scholar] [CrossRef]
- Aycardi, L.F.; Cifuentes, C.A.; Múnera, M.; Bayón, C.; Ramírez, O.; Lerma, S.; Frizera, A.; Rocon, E. Evaluation of Biomechanical Gait Parameters of Patients with Cerebral Palsy at Three Different Levels of Gait Assistance Using the CPWalker. J. Neuroeng. Rehabil. 2019, 16, 15. [Google Scholar] [CrossRef]
- Kobsar, D.; Masood, Z.; Khan, H.; Khalil, N.; Kiwan, M.Y.; Ridd, S.; Tobis, M. Wearable Inertial Sensors for Gait Analysis in Adults with Osteoarthritis—A Scoping Review. Sensors 2020, 20, 7143. [Google Scholar] [CrossRef] [PubMed]
- Gianzina, E.; Kalinterakis, G.; Delis, S.; Vlastos, I.; Platon Sachinis, N.; Yiannakopoulos, C.K. Evaluation of Gait Recovery after Total Knee Arthroplasty Using Wearable Inertial Sensors: A Systematic Review. Knee 2023, 41, 190–203. [Google Scholar] [CrossRef] [PubMed]
- Hillel, I.; Gazit, E.; Nieuwboer, A.; Avanzino, L.; Rochester, L.; Cereatti, A.; Croce, U.D.; Rikkert, M.O.; Bloem, B.R.; Pelosin, E.; et al. Is Every-Day Walking in Older Adults More Analogous to Dual-Task Walking or to Usual Walking? Elucidating the Gaps between Gait Performance in the Lab and during 24/7 Monitoring. Eur. Rev. Aging Phys. Act. 2019, 16, 6. [Google Scholar] [CrossRef] [PubMed]
- De Fazio, R.; Stabile, M.; De Vittorio, M.; Velázquez, R.; Visconti, P. An Overview of Wearable Piezoresistive and Inertial Sensors for Respiration Rate Monitoring. Electronics 2021, 10, 2178. [Google Scholar] [CrossRef]
- Al-Ayyad, M.; Owida, H.A.; De Fazio, R.; Al-Naami, B.; Visconti, P. Electromyography Monitoring Systems in Rehabilitation: A Review of Clinical Applications, Wearable Devices and Signal Acquisition Methodologies. Electronics 2023, 12, 1520. [Google Scholar] [CrossRef]
- Kobsar, D.; Charlton, J.M.; Tse, C.T.F.; Esculier, J.F.; Graffos, A.; Krowchuk, N.M.; Thatcher, D.; Hunt, M.A. Validity and Reliability of Wearable Inertial Sensors in Healthy Adult Walking: A Systematic Review and Meta-Analysis. J. Neuroeng. Rehabil. 2020, 17, 62. [Google Scholar] [CrossRef]
- Lopez-Nava, I.H.; Muñoz-Meléndez, A. Wearable Inertial Sensors for Human Motion Analysis: A Review. IEEE Sens. J. 2016, 16, 7821–7834. [Google Scholar] [CrossRef]
- Papi, E.; Murtagh, G.M.; McGregor, A.H. Wearable Technologies in Osteoarthritis: A Qualitative Study of Clinicians’ Preferences. BMJ Open 2016, 6, e009544. [Google Scholar] [CrossRef]
- Prisco, G.; Pirozzi, M.A.; Santone, A.; Esposito, F.; Cesarelli, M.; Amato, F.; Donisi, L. Validity of Wearable Inertial Sensors for Gait Analysis: A Systematic Review. Diagnostics 2025, 15, 36. [Google Scholar] [CrossRef]
- Petraglia, F.; Scarcella, L.; Pedrazzi, G.; Brancato, L.; Puers, R.; Costantino, C. Inertial Sensors versus Standard Systems in Gait Analysis: A Systematic Review and Meta-Analysis. Eur. J. Phys. Rehabil. Med. 2019, 55, 265–280. [Google Scholar] [CrossRef]
- Hurd, W.J.; Chmielewski, T.L.; Axe, M.J.; Davis, I.; Snyder-Mackler, L. Differences in Normal and Perturbed Walking Kinematics between Male and Female Athletes. Clin. Biomech. 2004, 19, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Bruening, D.A.; Frimenko, R.E.; Goodyear, C.D.; Bowden, D.R.; Fullenkamp, A.M. Sex Differences in Whole Body Gait Kinematics at Preferred Speeds. Gait Posture 2015, 41, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.H.; Park, J.M.; Kwon, O.Y. Gender Differences in Three Dimensional Gait Analysis Data from 98 Healthy Korean Adults. Clin. Biomech. 2004, 19, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Viteckova, S.; Horakova, H.; Polakova, K.; Krupicka, R.; Ruzicka, E.; Brozova, H. Agreement between the GAITRite R System and the Wearable Sensor BTS G-Walk R for Measurement of Gait Parameters in Healthy Adults and Parkinson’s Disease Patients. PeerJ 2020, 8, e8835. [Google Scholar] [CrossRef]
- Volkan-Yazici, M.; Çobanoğlu, G.; Yazici, G. Test-Retest Reliability and Minimal Detectable Change for Measures of Wearable Gait Analysis System (G-Walk) in Children with Cerebral Palsy. Turk. J. Med. Sci. 2022, 52, 658–666. [Google Scholar] [CrossRef]
- De Ridder, R.; Lebleu, J.; Willems, T.; De Blaiser, C.; Detrembleur, C.; Roosen, P. Concurrent Validity of a Commercial Wireless Trunk Triaxial Accelerometer System for Gait Analysis. J. Sport Rehabil. 2019, 28, 1–13. [Google Scholar] [CrossRef]
- Simon, S.R. Quantification of Human Motion: Gait Analysis—Benefits and Limitations to Its Application to Clinical Problems. J. Biomech. 2004, 37, 1869–1880. [Google Scholar] [CrossRef]
- Stebbins, J.; Harrington, M.; Stewart, C. Clinical Gait Analysis 1973–2023: Evaluating Progress to Guide the Future. J. Biomech. 2023, 160, 111827. [Google Scholar] [CrossRef]
- Cicirelli, G.; Impedovo, D.; Dentamaro, V.; Marani, R.; Pirlo, G.; D’Orazio, T.R. Human Gait Analysis in Neurodegenerative Diseases: A Review. IEEE J. Biomed. Health Inform. 2022, 26, 229–242. [Google Scholar] [CrossRef]
- Schwesig, R.; Leuchte, S.; Fischer, D.; Ullmann, R.; Kluttig, A. Inertial Sensor Based Reference Gait Data for Healthy Subjects. Gait Posture 2011, 33, 673–678. [Google Scholar] [CrossRef]
- Malinzak, R.A.; Colby, S.M.; Kirkendall, D.T.; Yu, B.; Garrett, W.E. A Comparison of Knee Joint Motion Patterns Between Men and Women in Selected Athletic Tasks. Clin. Biomech. 2001, 16, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Besson, T.; Macchi, R.; Rossi, J.; Morio, C.Y.M.; Kunimasa, Y.; Nicol, C.; Vercruyssen, F.; Millet, G.Y. Sex Differences in Endurance Running. Sports Med. 2022, 52, 1235–1257. [Google Scholar] [CrossRef] [PubMed]
- Nuzzo, J.L. Narrative Review of Sex Differences in Muscle Strength, Endurance, Activation, Size, Fiber Type, and Strength Training Participation Rates, Preferences, Motivations, Injuries, and Neuromuscular Adaptations. J. Strength Cond. Res. 2023, 37, 494–536. [Google Scholar] [CrossRef]
- Temesi, J.; Arnal, P.J.; Rupp, T.; Onard, L.É.; Asson, F.É.; Gine Cartier, R.É.; Gergelé, L.; Verges, S.; Martin, V.; Millet, G.Y. Are Females More Resistant to Extreme Neuromuscular Fatigue? Med. Sci. Sports Exerc. 2015, 47, 1372–1382. [Google Scholar] [CrossRef]
- Boling, M.C.; Nguyen, A.D.; Padua, D.A.; Cameron, K.L.; Beutler, A.; Marshall, S.W. Gender-Specific Risk Factor Profiles for Patellofemoral Pain. Clin. J. Sport Med. 2021, 31, 49–56. [Google Scholar] [CrossRef]
- Lin, C.Y.; Casey, E.; Herman, D.C.; Katz, N.; Tenforde, A.S. Sex Differences in Common Sports Injuries. PM&R 2018, 10, 1073–1082. [Google Scholar] [CrossRef]
- Lobb, N.J.; Fain, A.L.C.; Seymore, K.D.; Brown, T.N. Sex and Stride Length Impact Leg Stiffness and Ground Reaction Forces When Running with Body Borne Load. J. Biomech. 2019, 86, 96–101. [Google Scholar] [CrossRef]
- Marijančić, V.; Peharec, S.; Starčević-Klasan, G.; Grubić Kezele, T. Gender Differences in the Relationship between Physical Activity, Postural Characteristics and Non-Specific Low Back Pain in Young Adults. J. Funct. Morphol. Kinesiol. 2024, 9, 189. [Google Scholar] [CrossRef]
- Virgile, A.; Bishop, C. A Narrative Review of Limb Dominance: Task Specificity and the Importance of Fitness Testing. J. Strength Cond. Res. 2021, 35, 846–858. [Google Scholar] [CrossRef]
- Rynkiewicz, M.; Rynkiewicz, T.; Żurek, P.; Ziemann, E.; Szymanik, R. Asymmetry of Muscle Mass Distribution in Tennis Players. TRENDS Sport Sci. 2013, 1, 47–53. [Google Scholar]
- Slater, L.V.; Simpson, A.S.; Blemker, S.S.; Hertel, J.; Saliba, S.A.; Weltman, A.L.; Hart, J.M. Biomechanical Adaptations during Running Differ Based on Type of Exercise and Fitness Level. Gait Posture 2018, 60, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Zemková, E.; Kováčiková, Z. Sport-Specific Training Induced Adaptations in Postural Control and Their Relationship with Athletic Performance. Front. Hum. Neurosci. 2023, 16, 1007804. [Google Scholar] [CrossRef] [PubMed]
- Kalata, M.; Maly, T.; Hank, M.; Michalek, J.; Bujnovsky, D.; Kunzmann, E.; Zahalka, F. Unilateral and Bilateral Strength Asymmetry among Young Elite Athletes of Various Sports. Medicina 2020, 56, 683. [Google Scholar] [CrossRef]
| All Individuals (n: 95) | |||
|---|---|---|---|
| Parameter | Men (n: 55) | Women (n: 40) | p-Value |
| Age (year) | 25.13 (8.553) | 23.32 (6.654) | 0.349 |
| Weight (kg) | 76.58 (10.572) | 61.33 (8.716) | <0.001 |
| Height (cm) | 175.62 (19.914) | 166.88 (5.849) | 0.010 |
| Shoe size (EU) | 43.87 (1.504) | 39.38 (1.996) | <0.001 |
| Parameter | Men | Women | p-Value | Effect Size (Cohen’s d) |
|---|---|---|---|---|
| Cadence (steps/min) | 107.71 (6.225) | 110.65 (5.076) | 0.022 | −0.52 |
| Speed (m/s) | 1.30 (0.167) | 1.26 (0.124) | 0.178 | 0.27 |
| Symmetry index of gait cycle | 96.48 (1.950) | 97.08 (1.567) | 0.115 | −0.34 |
| Elaborated steps left | 7.35 (1.126) | 7.70 (0.111) | 0.102 | −0.44 |
| Elaborated steps right | 7.24 (1.138) | 7.23 (0.961) | 0.946 | 0.01 |
| Stride duration left (s) | 1.12 (0.064) | 1.09 (0.050) | 0.025 | 0.52 |
| Stride duration right (s) | 1.12 (0.065) | 1.09 (0.048) | 0.025 | 0.53 |
| Gait cycle duration left (s) | 1.12 (0.064) | 1.09 (0.050) | 0.025 | 0.52 |
| Gait cycle duration right (s) | 1.12 (0.065) | 1.09 (0.048) | 0.024 | 0.53 |
| Stride length left (m) | 1.45 (0.147) | 1.37 (0.115) | 0.005 | 0.61 |
| Stride length right (m) | 1.45 (0.145) | 1.38 (0.116) | 0.009 | 0.53 |
| % Stride length left (% height) | 84.80 (24.486) | 82.15 (7.045) | 0.507 | 0.11 |
| % Stride length right (% height) | 84.72 (23.801) | 82.61 (7.199) | 0.589 | 0.09 |
| Stance duration left (%) | 58.62 (1.550) | 59.36 (1.955) | 0.045 | −0.42 |
| Stance duration right (%) | 58.42 (1.830) | 59.13 (2.084) | 0.081 | −0.36 |
| Swing duration left (%) | 41.38 (1.550) | 40.64 (1.955) | 0.045 | 0.42 |
| Swing duration right (%) | 41.58 (1.830) | 40.87 (2.084) | 0.081 | 0.36 |
| First double support left (%) | 8.62 (1.554) | 9.06 (1.727) | 0.198 | −0.27 |
| First double support right (%) | 8.63 (1.586) | 9.45 (2.128) | 0.030 | −0.44 |
| Single support left (% cycle) | 41.45 (1.703) | 40.86 (2.013) | 0.123 | 0.32 |
| Single support right (% cycle) | 41.36 (1.513) | 40.88 (1.834) | 0.163 | 0.29 |
| Propulsion index left | 8.14 (1.890) | 9.38 (1.584) | 0.001 | −0.71 |
| Propulsion index right | 8.06 (1.935) | 9.33 (1.495) | 0.001 | −0.73 |
| Walk quality index left | 96.61 (2.389) | 96.86 (2.628) | 0.638 | −0.10 |
| Walk quality index right | 96.10 (2.832) | 96.32 (2.593) | 0.692 | −0.08 |
| Symmetry index of pelvic angles—tilt | 70.52 (22.820) | 67.48 (24.990) | 0.539 | 0.13 |
| Symmetry index of pelvic angles—obliquity | 96.57 (8.609) | 98.51 (0.612) | 0.157 | −0.32 |
| Symmetry index of pelvic angles—rotation | 97.37 (2.905) | 96.93 (4.002) | 0.535 | 0.13 |
| Pair | Comparison | t-Value | p-Value | Effect Size (Cohen’s d) |
|---|---|---|---|---|
| Pair 1 | Gait cycle duration left (s) vs. right (s) | 1.727 | 0.087 | 0.04 |
| Pair 2 | Elaborated steps (number) left vs. right | 2.367 | 0.020 | 0.24 |
| Pair 3 | Stride duration left (s) vs. right (s) | 1.821 | 0.072 | 0.04 |
| Pair 4 | Stride length left (m) vs. right (m) | −1.372 | 0.173 | −0.02 |
| Pair 6 | % Stride length left (% height) vs. % right (% height) | −1.053 | 0.295 | −0.01 |
| Pair 7 | Stance duration left (%) vs. right (%) | 1.388 | 0.169 | 0.11 |
| Pair 8 | Swing duration left (%) vs. right (%) | −1.388 | 0.169 | −0.11 |
| Pair 9 | First double Support left (%) vs. right (%) | −1.115 | 0.268 | −0.10 |
| Pair 10 | Single support left (%) vs. right (%) | 0.280 | 0.780 | 0.03 |
| Pair 11 | Propulsion index left vs. right | 0.660 | 0.511 | 0.04 |
| Pair 12 | Walk quality index left vs. right | 1.938 | 0.056 | 0.20 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gianzina, E.; Yiannakopoulos, C.K.; Kalinterakis, G.; Delis, S.; Chronopoulos, E. Gender-Based Differences in Biomechanical Walking Patterns of Athletes Using Inertial Sensors. J. Funct. Morphol. Kinesiol. 2025, 10, 82. https://doi.org/10.3390/jfmk10010082
Gianzina E, Yiannakopoulos CK, Kalinterakis G, Delis S, Chronopoulos E. Gender-Based Differences in Biomechanical Walking Patterns of Athletes Using Inertial Sensors. Journal of Functional Morphology and Kinesiology. 2025; 10(1):82. https://doi.org/10.3390/jfmk10010082
Chicago/Turabian StyleGianzina, Elina, Christos K. Yiannakopoulos, Georgios Kalinterakis, Spilios Delis, and Efstathios Chronopoulos. 2025. "Gender-Based Differences in Biomechanical Walking Patterns of Athletes Using Inertial Sensors" Journal of Functional Morphology and Kinesiology 10, no. 1: 82. https://doi.org/10.3390/jfmk10010082
APA StyleGianzina, E., Yiannakopoulos, C. K., Kalinterakis, G., Delis, S., & Chronopoulos, E. (2025). Gender-Based Differences in Biomechanical Walking Patterns of Athletes Using Inertial Sensors. Journal of Functional Morphology and Kinesiology, 10(1), 82. https://doi.org/10.3390/jfmk10010082







