The Features of Children with Juvenile Idiopathic Arthritis with Cervical Spine Involvement in the Data from a Retrospective Study Cohort
Abstract
1. Introduction
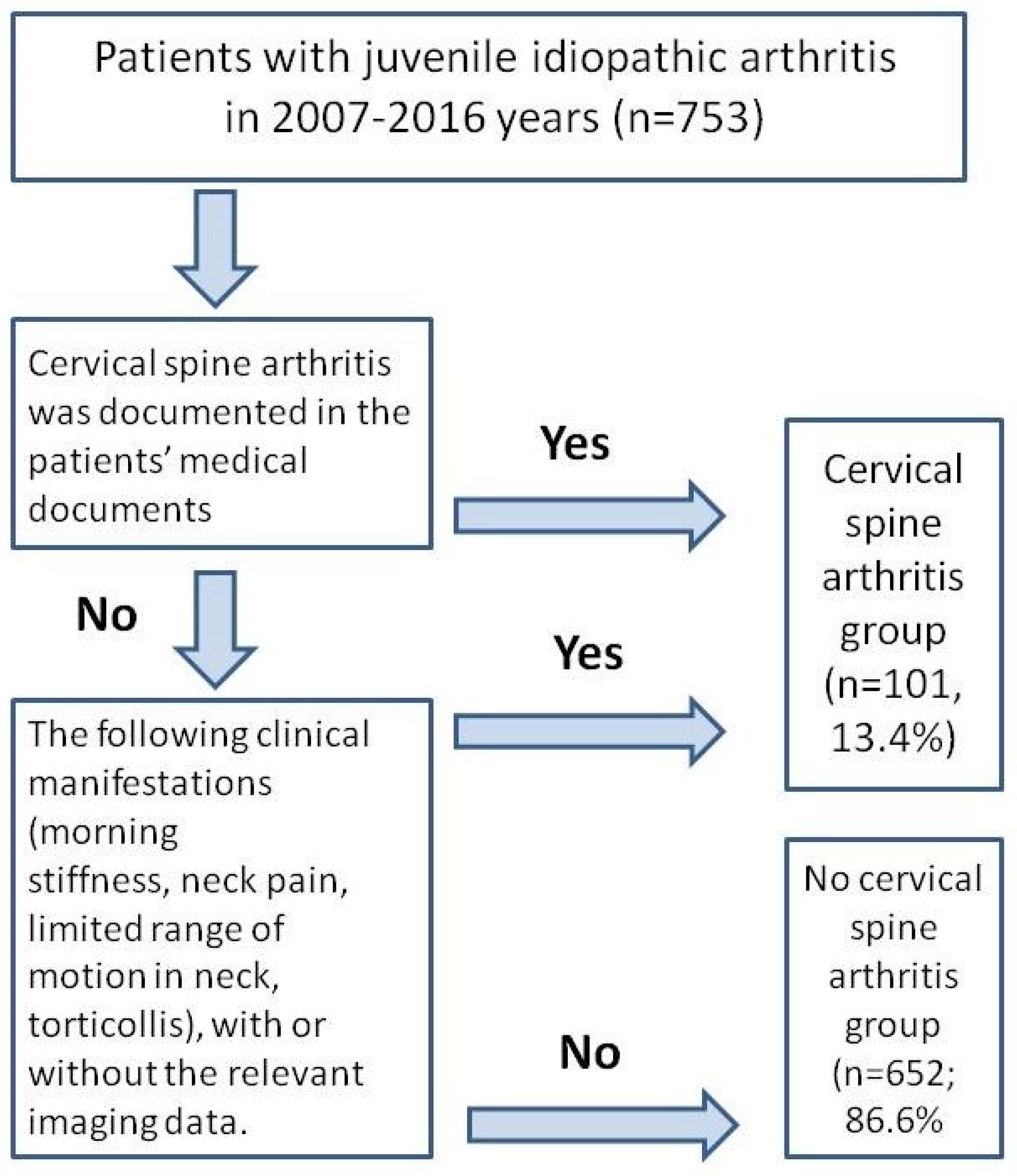
2. Methods and Materials
2.1. Assessment and the Outcomes
- (i)
- Demography: sex, onset age, age of the study inclusion, JIA category according to the ILAR classification [1], presence of the uveitis.
- (ii)
- Clinical data: Joints assessment, active joints number. The joint was considered active if it was swollen or if there was pain and restricted movement. Arthritis of the temporo-mandibular joints (TMJs) was considered if the patient had two or more of the following clinical signs: pain in the TMJs, jaw opening limitations, jaw opening deviations, micrognathia, and other orofacial deformities related to JIA involvement.
- (iii)
- The presence of antinuclear antibodies (ANA) and the HLA B27 antigen, an erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP).
- (iv)
- Treatment: Systemic corticosteroids (oral and intravenous), non-biologic (nb), and biologic (b) disease-modifying anti-rheumatic drugs (DMARDs)
- (v)
- Outcomes: The achievement of remission, the presence of the subsequent flare, and time to JIA remission and JIA flare.
2.2. Ethics
2.3. Statistical Analysis
3. Results
3.1. The Phenotype of Patients with JIA Who Had CSA
3.2. Factors Associated with CSA
4. Discussion
4.1. The Most Typical CS Changes in Patients with JIA Are as Follows
- Ankylosis of the articular joints. Usually, these changes are observed in C2–C3. Ankylosis can result in impaired vertebral body growth, especially in patients with early-onset JIA [3].
- Atlantoaxial instability. Anterior subluxation of the atlas is characterized by an increase in the distance between the anterior C1 semicircle and the dens of C2. The anterior atlantodental interval (AADI) is the horizontal distance between the posterior cortex of the anterior arch of the atlas (C1) and the anterior cortex of the dens in the median (midsagittal) plane.
- 3.
- Atlantoaxial rotational locking. Damage to the joint capsule or ligament apparatus of the atlantoaxial joint can lead to the development of rotational subluxation of C1. With prolonged dislocation, the capsule and ligaments become tightened, which leads to chronic atlantoaxial block. A typical clinical manifestation of a rotational subluxation is a malposition of the head with a slight (about 20°) tilt to one side and rotation to the opposite side. Risk factors for the possible transition of subluxation into chronic block include the contraction of the joint capsule, intra-articular fibrous inclusions, synovitis of the adjacent joint surfaces, formation of C1 and C2 vertebrae bony fusions, and secondary deformity of the surface of the facet joints [20].
- 4.
4.2. Surgical Treatment for CSA in JIA Patients
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Petty, R.E.; Southwood, T.R.; Manners, P.; Baum, J.; Glass, D.N.; Goldenberg, J.; He, X.; Maldonado-Cocco, J.; Orozco-Alcala, J.; Prieur, A.-M.; et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: Second revision, Edmonton, 2001. J. Rheumatol. 2004, 31, 390–392. [Google Scholar] [PubMed]
- El Hassani Sbai, S.; Rostom, S.; Amine, B.; Bahiri, R. The cervical spine in juvenile idiopathic arthritis. Merit Res. J. Med. Med. Sci. 2019, 7, 304–307. [Google Scholar]
- Wolfs, J.F.C.; Arts, M.P.; Peul, W.C. Juvenile Chronic Arthritis and the Craniovertebral Junction in the Paediatric Patient: Review of the Literature and Management Considerations. Adv. Tech. Stand. Neurosurg. 2013, 41, 143–156. [Google Scholar] [CrossRef]
- Reiter, M.F.; Boden, S.D. Inflammatory disorders of the cervical spine. Spine 1998, 23, 2755–2766. [Google Scholar] [CrossRef] [PubMed]
- Hospach, T.; Maier, J.; Műller-Abt, P.; Patel, A.; Horneff, G.; von Kalle, T. Cervical spine involvement in patients with juvenile idiopathic arthritis—MRI follow-up study. Pediatr. Rheumatol. 2014, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- Elhai, M.; Wipff, J.; Bazeli, R.; Freire, V.; Feydy, A.; Drapé, J.-L.; Quartier, P.; Kahan, A.; Job-Deslandre, C. Radiological cervical spine involvement in young adults with polyarticular juvenile idiopathic arthritis. Rheumatology 2012, 52, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Jurik, A.G. Imaging the spine in arthritis—A pictorial review. Insight Imaging 2011, 2, 177–191. [Google Scholar] [CrossRef]
- Joaquim, A.F.; Ghizoni, E.; Tedeschi, H.; Appenzeller, S.; Riew, K.D. Radiological evaluation of cervical spine involvement in rheumatoid arthritis. Neurosurg. Focus 2015, 38, E4. [Google Scholar] [CrossRef]
- Damasio, M.B.; de Horatio, L.T.; Boavida, P.; Lambot-Juhan, K.; Rosendahl, K.; Tomà, P.; Muller, L.O. Imaging in juvenile idiopathic arthritis (JIA): An update with particular emphasis on MRI. Acta Radiol. 2013, 54, 1015–1023. [Google Scholar] [CrossRef]
- Nusman, C.M.; Muller, L.-S.O.; Hemke, R.; Doria, A.S.; Avenarius, D.; Tzaribachev, N.; Malattia, C.; van Rossum, M.A.; Maas, M.; Rosendahl, K. Current Status of Efforts on Standardizing Magnetic Resonance Imaging of Juvenile Idiopathic Arthritis: Report from the OMERACT MRI in JIA Working Group and Health-e-Child. J. Rheumatol. 2016, 43, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Ključevšek, D.; Emeršič, N.; Toplak, N.; Avčin, T. Clinical and MRI outcome of cervical spine lesions in children with juvenile idiopathic arthritis treated with anti-TNFα drugs early in disease course. Pediatr. Rheumatol. 2017, 15, 38. [Google Scholar] [CrossRef] [PubMed]
- Semolič, N.; Toplak, N.; Koder, J.; Ključevšek, D.; Avčin, T. PReS-FINAL-2084: Prevalence of cervical spine involvement in children with juvenile idiopathic arthritis. Pediatr. Rheumatol. 2013, 11 (Suppl. 2), P96. [Google Scholar] [CrossRef]
- Fried, J.A.; Arhtreya, B.; Gregg, J.R.; Das, M.; Doughty, R. The cervical spine in juvenile rheumatoid arthritis. Clin. Orthop. Relat. Res. 1983, 179, 102–106. [Google Scholar] [CrossRef]
- Oren, B.; Oren, H.; Osma, E.; Cevik, N. Juvenile rheumatoid arthritis: Cervical spine and MRI in early diagnosis. Turk. J. Pediatr. 1996, 38, 189–194. [Google Scholar]
- Munir, S.; Patil, K.; Miller, E.; Uleryk, E.; Twilt, M.; Spiegel, L.; Doria, A.S. Juvenile Idiopathic Arthritis of the Axial Joints: A Systematic Review of the Diagnostic Accuracy and Predictive Value of Conventional MRI. Am. J. Roentgenol. 2014, 202, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Østergaard, M.; Klarlund, M. Importance of timing of post-contrast MRI in rheumatoid arthritis: What happens during the first 60 minutes after IV gadolinium-DTPA? Ann. Rheum. Dis. 2001, 60, 1050–1054. [Google Scholar] [CrossRef]
- Mahmood, K.; Khan, A.; Clinch, J.; Thayagarajan, M.S. Cervical-spine involvement in JIA: A single-centre study. Rheumatology 2015, 54 (Suppl. 2), 117–118. [Google Scholar] [CrossRef][Green Version]
- Locke, G.R.; Gardner, J.I.; Van Epps, E.F. Atlas-dens interval (ADI) in children: A survey based on 200 normal cervical spines. Am. J. Roentgenol. Radium. Ther. Nucl. Med. 1996, 97, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Pennecot, G.F.; Gouraud, D.; Hardy, J.R.; Pouliquen, J.C. Roentgenographical study of the stability of the cervical spine in children. J. Pediatr. Orthop. 1984, 4, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Fusco, M.; Hankinson, T.; Rozzelle, C. Combined occipitoatlantoaxial rotatory fixation: Case report. J. Neurosurg. Pediatr. 2011, 8, 198–204. [Google Scholar] [CrossRef] [PubMed]
- Enden, K.; Laiho, K.; Kautiainen, H.; Arkela, M.; Belt, E.; Kauppi, M. Subaxial cervical vertebrae in patients with juvenile idiopathic arthritis—Something special? Jt. Bone Spine 2009, 76, 519–523. [Google Scholar] [CrossRef]
- Artamonov, A.K.; Kaneva, M.A.; Gordeeva, N.A.; Sorokina, L.S.; Kostik, M.M. Temporomandibular Joint Involvement in Juvenile Idiopathic Arthritis: The Results from a Retrospective Cohort Tertial Center Study. Life 2023, 13, 1164. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Uziel, Y.; Rathaus, V.; Pomeranz, A.; Solan, H.; Wolach, B. Torticollis as the sole initial presenting sign of systemic onset juvenile rheumatoid arthritis. J. Rheumatol. 1998, 25, 166–168. [Google Scholar] [PubMed]
- Kang, J.H. Effects on migraine, neck pain, and head and neck posture, of temporomandibular disorder treatment: Study of a retrospective cohort. Arch. Oral Biol. 2020, 114, 104718. [Google Scholar] [CrossRef] [PubMed]
- Armijo-Olivo, S.; Fuentes, J.P.; da Costa, B.R.; Major, P.W.; Warren, S.; Thie, N.M.; Magee, D.J. Reduced endurance of the cervical flexor muscles in patients with concurrent temporomandibular disorders and neck disability. Man. Ther. 2010, 15, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Olivo, S.A.; Bravo, J.; Magee, D.J.; Thie, N.M.; Major, P.W.; Flores-Mir, C. The association between head and cervical posture and temporomandibular disorders: A systematic review. J. Orofac. Pain 2006, 20, 9–23. [Google Scholar] [PubMed]
- Cuccia, A.; Caradonna, C. The relationship between the stomatognathic system and body posture. Clinics 2009, 64, 61–66. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chung, M.K.; Wang, S.; Yang, J.; Alshanqiti, I.; Wei, F.; Ro, J.Y. Neural Pathways of Craniofacial Muscle Pain: Implications for Novel Treatments. J. Dent. Res. 2020, 99, 1004–1012. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ringold, S.; Angeles-Han, S.T.; Beukelman, T.; Lovell, D.; Cuello, C.A.; Becker, M.L.; Colbert, R.A.; Feldman, B.M.; Ferguson, P.J.; Gewanter, H.; et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Treatment of Juvenile Idiopathic Arthritis: Therapeutic Approaches for Non-Systemic Polyarthritis, Sacroiliitis, and Enthesitis. Arthritis Care Res. 2019, 71, 717–734. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stoustrup, P.; Glerup, M.; Bilgrau, A.E.; Küseler, A.; Verna, C.; Christensen, A.E.; Kristensen, K.D.; Nørholt, S.E.; Twilt, M.; Herlin, T.; et al. Cumulative Incidence of Orofacial Manifestations in Early Juvenile Idiopathic Arthritis: A Regional, Three-Year Cohort Study. Arthritis Care Res. 2020, 72, 907–916. [Google Scholar] [CrossRef]
- Onel, K.B.; Horton, D.B.; Lovell, D.J.; Shenoi, S.; Cuello, C.A.; Angeles-Han, S.T.; Becker, M.L.; Cron, R.Q.; Feldman, B.M.; Ferguson, P.J.; et al. 2021 American College of Rheumatology Guideline for the Treatment of Juvenile Idiopathic Arthritis: Therapeutic Approaches for Oligoarthritis, Temporomandibular Joint Arthritis, and Systemic Juvenile Idiopathic Arthritis. Arthritis Care Res. 2022, 74, 521–537. [Google Scholar] [CrossRef] [PubMed]
- Yüzbaşıoğlu, Ü.; Kaynak, B.A.; Taş, S. Assessment of Cervical Joint Position Sense and Head Posture in Individuals With Myogenic Temporomandibular Dysfunctions and Identifying Related Factors: A Case-Control Study. J. Oral Rehabil. 2025, 52, 160–168. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- de Oliveira-Souza, A.I.S.; do Valle Sales, L.R.; de Fontes Coutinho, A.D.; de Oliveira, D.A.; Armijo-Olivo, S. Effectiveness of an 8-week neck exercise training on pain, jaw function, and oral health-related quality of life in women with chronic temporomandibular disorders: A randomized controlled trial. J. Oral Facial Pain Headache 2024, 38, 40–51. [Google Scholar] [CrossRef] [PubMed]
- Laiho, K.; Savolainen, A.; Kautiainen, H.; Kekki, P.; Kauppi, M. The cervical spine in juvenile chronic arthritis. Spine J. 2002, 2, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Tzaribachev, N.; Tzaribachev, C.; Koos, B. High Prevalence of Cervical Spine and Tempomandibular Joint Involvement in Patients with Juvenile Idiopathic Arthritis. In Proceedings of the 2012 ACR/ARHP Annual Meeting, Washington, DC, USA, 9–14 November 2012. Abstract Number: 2026. [Google Scholar]
- Narváez, J.A.; Narváez, J.; de Albert, M.; De Lama, E.; Serrallonga, M.; Nolla, J.M. Bone marrow edema in the cervical spine of symptomatic rheumatoid arthritis patients. Semin. Arthritis Rheum. 2009, 38, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Lee, E.; Lee, J.W.; Kang, Y.; Ahn, J.M.; Yeom, J.S.; Kang, H.S. Postoperative Regression of Retro-odontoid Pseudotumor After Atlantoaxial Posterior Fixation: 11 Years of Experience in Patients with Atlantoaxial Instability. Spine 2017, 42, 1763–1771. [Google Scholar] [CrossRef] [PubMed]

| Parameters | CSA, Yes (n = 101) | CSA, No (n = 652) | p |
|---|---|---|---|
| Demography | |||
| Girls, n (%) | 69 (68.3) | 388 (59.5) | 0.092 |
| Onset age, years, Me (25%; 75%) | 5.3 (2.7; 10.1) | 6.1 (3.0; 10.4) | 0.241 |
| Duration of disease, years, Me (25%; 75%) | 5.9 (3.2; 9.4) | 4.0 (1.8; 7.2) | 0.0003 |
| JIA category, n (%) Oligoarthritis Polyarthritis Psoriatic arthritis Enthesitis-associated arthritis Systemic arthritis | 5 (5.0) 48 (48.0) 7 (7.0) 22 (21.8) 19 (18.9) | 199 (30.5) 217 (33.3) 33 (5.1) 164 (25.2) 39 (6.0) | <0.001 |
| Uveitis, n (%) | 9/76 (11.9) | 107/444 (24.1) | 0.018 |
| Articular status | |||
| Active joints, Me (25%; 75%) | 16.0 (9.0; 28.0) | 5.0 (3.0; 10.0) | <0.001 |
| Joint involvement: TMJ, n (%) Shoulder joint, n (%) Elbow joint, n (%) Wrist joint, n (%) Metacarpophalangeal joint, n (%) Proximal interphalangeal joint, n (%) Distal interphalangeal joint, n (%) Hip joint, n (%) Knee joint, n (%) | 24 (23.7) 30 (29.7) 35 (34.6) 62 (61.4) 44 (43.6) 53 (52.5) 24 (23.8) 45 (44.6) 61 (60.4) | 19 (2.9) 19 (2.9) 80 (12.2) 142 (21.8) 120 (18.4) 139 (21.3) 46 (7.1) 108 (16.6) 262 (40.2) | <0.001 <0.001 <0.001 <0.001 <0.001 <0.001 <0.001 <0.001 0.0001 |
| Laboratory | |||
| ANA-positivity, n (%) | 22/57 (38.6) | 190/403 (47.2) | 0.226 |
| Erythrocyte sedimentation rate, mm/h, Me (25%; 75%) | 12.0 (5.0; 31.0) | 7.0 (3.0; 18.0) | 0.0006 |
| C-reactive protein, mg/L, Me (25%; 75%) | 3.9 (0.0; 20.0) | 1.1 (0.0; 9.2) | 0.002 |
| Treatment | |||
| Oral corticosteroids, n (%) | 37/101 (36.7) | 115/651 (17.7) | 0.00001 |
| Methylprednisolone pulse therapy, n (%) | 33/100 (33.0) | 102/650 (15.7) | 0.00003 |
| Methotrexate, n (%) | 87/99 (87.9) | 486/568 (85.6) | 0.541 |
| Biologics, n (%) | 68 (67.3) | 283 (43.4) | 0.000007 |
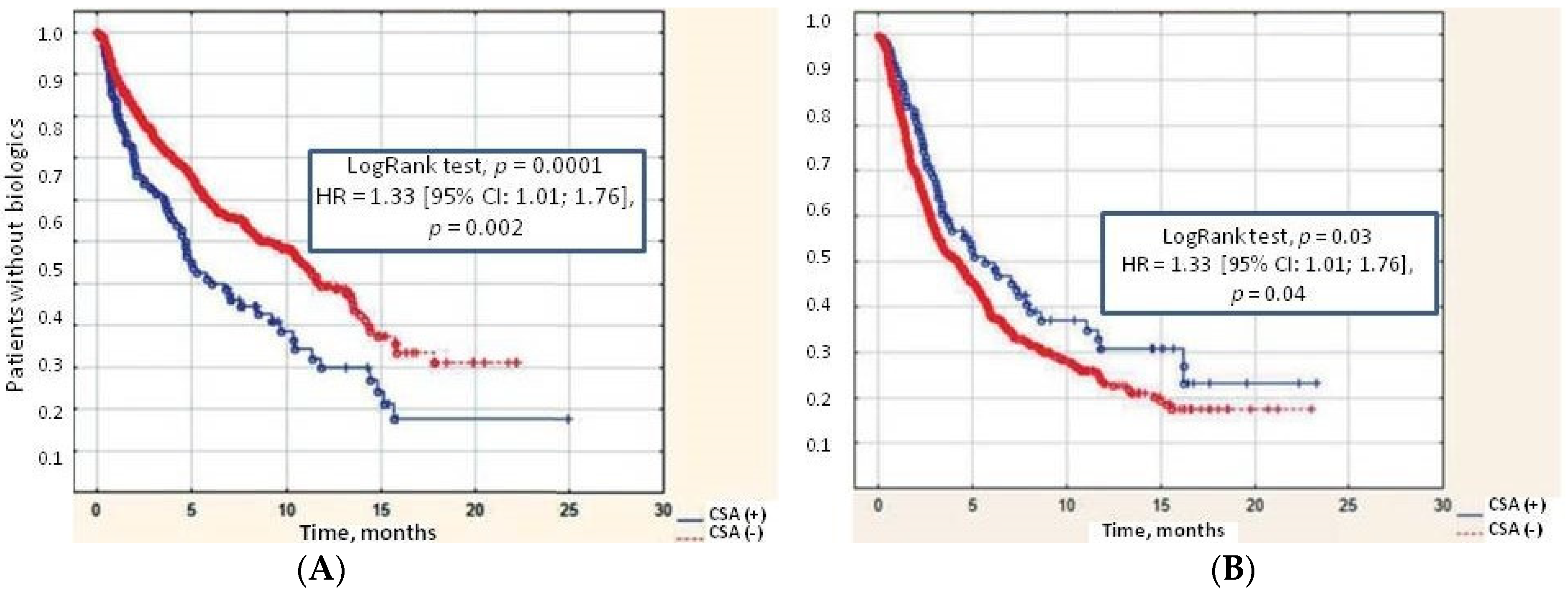
| Outcomes | |||
| Remission of JIA, n (%) | 57 (56.4) | 428 (65.6) | 0.072 |
| Time to JIA remission, years, Me (25%; 75%) | 2.9 (1.5–5.1) | 2.2 (1.1–4.6) | 0.046 |
| Flares of JIA, n (%) | 10 (9.9) | 128 (19.7) | 0.018 |
| Risk Factors | Se | Sp | OR (95% CI) | p-Value |
|---|---|---|---|---|
| Oral corticosteroids | 0.37 | 0.82 | 5.3 (3.1; 8.7) | <0.001 |
| Methylprednisolone pulse therapy | 0.33 | 0.84 | 2.7 (1.7; 4.2) | <0.001 |
| Biologics | 0.67 | 0.57 | 2.7 (1.7; 4.2) | <0.001 |
| Polyarticular JIA category | 0.48 | 0.67 | 1.8 (1.2; 2.7) | <0.001 |
| Systemic JIA category | 0.19 | 0.94 | 3.6 (2.0; 6.6) | <0.001 |
| TMJ arthritis | 0.24 | 0.97 | 10.4 (5.4; 19.8) | <0.001 |
| Shoulder arthritis | 0.3 | 0.97 | 14.1 (7.5; 26.3) | <0.001 |
| Elbow arthritis | 0.35 | 0.88 | 3.8 (2.4; 6.1) | <0.001 |
| Wrist arthritis | 0.61 | 0.78 | 5.7 (3.7; 8.9) | <0.001 |
| Metacarpophalangeal arthritis | 0.44 | 0.82 | 3.4 (2.2; 5.3) | <0.001 |
| Proximal interphalangeal arthritis | 0.53 | 0.79 | 4.1 (2.6; 6.3) | <0.001 |
| Distal interphalangeal arthritis | 0.24 | 0.93 | 4.1 (2.4; 7.1) | <0.001 |
| Hip arthritis | 0.45 | 0.83 | 4.1 (2.6; 6.3) | <0.001 |
| Knee arthritis | 0.55 | 0.6 | 1.8 (1.2; 2.7) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sorokina, L.S.; Artamonov, A.K.; Kaneva, M.A.; Gordeeva, N.A.; Raupov, R.K.; Mushkin, A.Y.; Ivanov, D.O.; Kostik, M.M. The Features of Children with Juvenile Idiopathic Arthritis with Cervical Spine Involvement in the Data from a Retrospective Study Cohort. J. Funct. Morphol. Kinesiol. 2025, 10, 68. https://doi.org/10.3390/jfmk10010068
Sorokina LS, Artamonov AK, Kaneva MA, Gordeeva NA, Raupov RK, Mushkin AY, Ivanov DO, Kostik MM. The Features of Children with Juvenile Idiopathic Arthritis with Cervical Spine Involvement in the Data from a Retrospective Study Cohort. Journal of Functional Morphology and Kinesiology. 2025; 10(1):68. https://doi.org/10.3390/jfmk10010068
Chicago/Turabian StyleSorokina, Lubov S., Artem K. Artamonov, Maria A. Kaneva, Natalia A. Gordeeva, Rinat K. Raupov, Alexander Yu. Mushkin, Dmitri O. Ivanov, and Mikhail M. Kostik. 2025. "The Features of Children with Juvenile Idiopathic Arthritis with Cervical Spine Involvement in the Data from a Retrospective Study Cohort" Journal of Functional Morphology and Kinesiology 10, no. 1: 68. https://doi.org/10.3390/jfmk10010068
APA StyleSorokina, L. S., Artamonov, A. K., Kaneva, M. A., Gordeeva, N. A., Raupov, R. K., Mushkin, A. Y., Ivanov, D. O., & Kostik, M. M. (2025). The Features of Children with Juvenile Idiopathic Arthritis with Cervical Spine Involvement in the Data from a Retrospective Study Cohort. Journal of Functional Morphology and Kinesiology, 10(1), 68. https://doi.org/10.3390/jfmk10010068







