Modelling the Application of Telemedicine in Emergency Care
Abstract
:1. Introduction
1.1. Background and Context
1.2. The Problem
1.3. The Process
1.4. The Proposed Solution
2. Materials and Methods
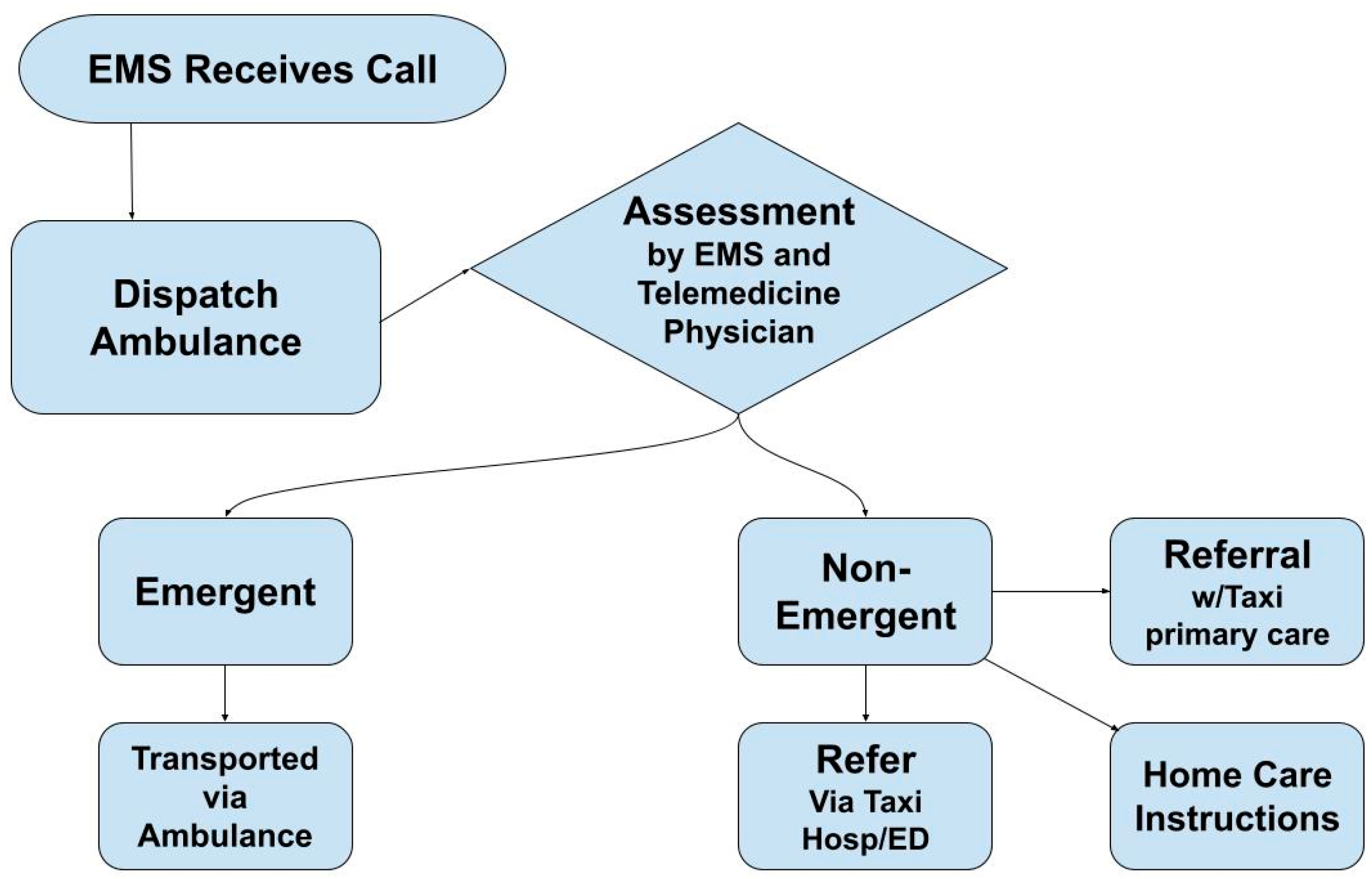
2.1. Modelling
2.1.1. The Process Model
2.1.2. The Technology Model
2.2. Triage
3. Results
3.1. Core Vital Signs
3.1.1. ECG Data Only
3.1.2. ECG Data and Vital Signs
3.1.3. ECG Data, Vital Signs, Rapid Diagnostic Kits and Mobile Scanner
3.2. Tele-Mental Health
3.3. Advanced Mobile Imaging
3.4. Continuous Queue Modelling
4. Discussion
4.1. Barriers to Implementing Telemedical Solutions in Emergency Care
4.1.1. Protocols and Bureaucracy
4.1.2. Data Privacy and Security
4.1.3. Difficulties of Economic Assessment
4.2. Potential Impact of the Proposed Solution
4.3. Machine Learning in Telemedicine
4.4. Model Estimate Uncertainties
5. Conclusions, Recommendations and Further Research
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| AI | Artificial Intelligence |
| CAD | Computer-Aided Dispatch |
| CBRN | Chemical, Biological, Radiological and Nuclear |
| CT | Computer Tomography |
| DICOM | Digital Imaging and Communications in Medicine |
| ECG | Electrocardiography |
| ER | Emergency Room |
| ESTA | Emergency Services Telecommunication Authority |
| GPS | Global Positioning System |
| GSM | Global System for Mobile Communications |
| HL7 | Health Level Seven |
| IT | Information Technology |
| MMS | Multimedia Messaging Service |
| NSW | New South Wales |
| PACS | Picture Archiving and Communication System |
| PCR | Polymerase Chain Reaction |
| SMS | Short Message Service |
| TB | Terabyte |
| TCP/IP | Transmission Control Protocol/Internet Protocol |
| tPA | Tissue Plasminogen Activator |
| EU MDR | European Union Medical Device Regulation |
References
- Australian Bureau of Statistics. National, State and Territory Population. ABS, December 2022. Available online: https://www.abs.gov.au/statistics/people/population/national-state-and-territory-population/latest-release (accessed on 8 May 2023).
- Andrew, E.; Nehme, Z.; Cameron, P.; Smith, K. Drivers of increasing emergency ambulance demand. Prehospital Emerg. Care 2020, 24, 385–393. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Quarterly Population Estimates (ERP), by State/Territory, Sex and Age. ABS, May 2023. Available online: https://explore.data.abs.gov.au (accessed on 8 May 2023).
- Ambulance Victoria. Annual Report 2020–2021. 2022. Available online: https://www.ambulance.vic.gov.au/wp-content/uploads/2021/10/Ambulance-Victoria-Annual-Report-2020-21.pdf (accessed on 8 May 2023).
- Fermer, D. Victoria’s Hospital and Ambulance System under Record Pressure, Data Shows. ABC News. 2022. Available online: https://www.abc.net.au/news/2022-04-30/victorias-hospital-and-ambulance-system-under-record-pressure/101028042 (accessed on 8 May 2023).
- ESTA. The Emergency Services Telecommunications Authority’s Role in the Community. 2022. Available online: https://www.esta.vic.gov.au/about-esta (accessed on 8 May 2023).
- Victoria Auditor Genera. Emergency Response ICT Systems Audit 2014. 2014. Available online: https://www.audit.vic.gov.au/sites/default/files/20141014-Emergency-ICT.pdf (accessed on 8 May 2023).
- ESTA. Victorian Government Emergency Services Capabilities Review. 2022. Available online: https://www.vic.gov.au/sites/default/files/2022-05/ESTA%20Capability%20and%20Service%20Review%20Final%20Report.pdf (accessed on 8 May 2023).
- Iredale, D. Inquest Document: Iredale Findings. 2006. Available online: http://www.outdoorcouncil.asn.au/wp-content/uploads/2016/08/Iredalefindings.pdf (accessed on 8 May 2023).
- Walker, I. Joanne Wicking Case Detailed. Daily Telegraph. 2011. Available online: https://www.dailytelegraph.com.au/news/nsw/daughters-tell-of-parole-murder-horror-of-their-mother-joanne-wicking/news-story/906111a0939dfd6084ed98a0c557905c (accessed on 8 May 2023).
- Victorian Government. Emergency Department—What to Expect. 2022. Available online: https://www.betterhealth.vic.gov.au/health/servicesandsupport/emergency-department-what-to-expect#triage-explained (accessed on 11 May 2023).
- Dow, A.; Eddie, R. Victorian Patients Languish Longer in Emergency Departments and Ambulance Queues. The Age. 2022. Available online: https://www.theage.com.au/national/victoria/victorian-patients-languish-longer-in-emergency-departments-and-ambulance-queues-20220806-p5b7rp.html (accessed on 11 May 2023).
- Mitchell, N. Strained Ambulance Service Enacts a Code Orange Most Weeks. Nine/3AW. 2022. Available online: https://www.3aw.com.au/ambulance-victoria-enacts-a-code-orange-most-weeks/ (accessed on 11 May 2023).
- Wankhade, P. Different Cultures of Management and Their Relationships with Organizational Performance: Evidence from the UK Ambulance Service. Public Money Manag. 2012, 32, 381–388. [Google Scholar] [CrossRef]
- Dawson, L.P.; Andrew, E.; Stephenson, M.; Nehme, Z.; Bloom, J.; Cox, S.; Anderson, D.; Lefkovits, J.; Taylor, A.J.; Kaye, D. The influence of ambulance offload time on 30-day risks of death and re-presentation for patients with chest pain. Med. J. Aust. 2022, 217, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Fatovich, D.M.; Nagree, Y.; Sprivulis, P. Access block causes emergency department overcrowding and ambulance diversion in Perth, Western Australia. Emerg. Med. J. 2005, 22, 351–354. [Google Scholar] [CrossRef]
- Ascui, L. Ambulance Ramping Is a Signal the Health System Is Floundering. AAPL. 2022. Available online: https://theconversation.com/ambulance-ramping-is-a-signal-the-health-system-is-floundering-solutions-need-to-extend-beyond-eds-187270 (accessed on 11 May 2023).
- Ambulance Victoria. Clinical Guidelines. 2022. Available online: https://www.ambulance.vic.gov.au/wp-content/uploads/2022/02/avcpg.pdf (accessed on 11 May 2023).
- Eastwood, K.; Smith, K.; Morgans, A.; Stoelwinder, J. Appropriateness of cases presenting in the emergency department following ambulance service secondary telephone triage: A retrospective cohort study. BMJ Open 2017, 7, e016845. [Google Scholar] [CrossRef]
- Gillon, S.; Radford, S.; Chalwin, R.; DeVita, M.; Endacott, R.; Jones, D. Crisis resource management, simulation training and the medical emergency team. Crit. Care Resusc. 2012, 14, 227–235. [Google Scholar] [PubMed]
- Arisha, A.; Rashwan, W. Modeling of healthcare systems: Past, current and future trends. In Proceedings of the 2016 Winter Simulation Conference (WSC), Washington, DC, USA, 11–14 December 2016; IEEE: Piscataway, NJ, USA, 2016; pp. 1523–1534. [Google Scholar] [CrossRef]
- Ara, R.; Brazier, J.E. Populating an economic model with health state utility values: Moving toward better practice. Value Health 2010, 13, 509–518. [Google Scholar] [CrossRef] [PubMed]
- Nikakhtar, A.; Hsiang, S.M. Incorporating the dynamics of epidemics in simulation models of healthcare systems. Simul. Model. Pract. Theory 2014, 43, 67–78. [Google Scholar] [CrossRef]
- Ferenczi, G.; Vass, D.I.P.; Csaba, E.; Darago, L. eHealth8 Project: A Complex Telemedicine System Implemented in Hungary. 2008. Available online: http://ehealth8.bzlogi.hu/index.php?lang=en (accessed on 11 May 2023).
- Ferenczi, G.G.; Mahmood, A.N.; Bergmann, R.K. Telemedicine Pre and Post COVID-19: Lessons for Commercialisation Based on Previous Use Cases. J. Int. Soc. Telemed. eHealth 2020, 8, e8-1. [Google Scholar] [CrossRef]
- Kurnia, S.; Lee, H.; Yang, S. Understanding consumers’ expectations of mobile data services in Australia. In Proceedings of the International Conference on the Management of Mobile Business (ICMB 2007), Toronto, ON, Canada, 9–11 July 2007; IEEE: Piscataway, NJ, USA, 2007; p. 14. [Google Scholar] [CrossRef]
- Alesanco, A.; Olmos, S.; Istepanian, R.S.; García, J. Enhanced real-time ECG coder for packetized telecardiology applications. IEEE Trans. Inf. Technol. Biomed. 2006, 10, 229–236. [Google Scholar] [CrossRef]
- Schwindling, L.; Ragoschke-Schumm, A.; Kettner, M.; Helwig, S.; Manitz, M.; Roumia, S.; Lesmeister, M.; Grunwald, I.Q.; Fassbender, K. Prehospital Imaging-Based Triage of Head Trauma with a Mobile Stroke Unit: First Evidence and Literature Review. J. Neuroimaging 2016, 26, 489–493. [Google Scholar] [CrossRef]
- Ferenczi, G. Method of Transmitting Results of Diagnostical Measurements in MMs via GSM. Network. Patent Appl. P1100371/8, A61B 5/00, H04W 4/12, 21 May 2011. [Google Scholar]
- Ferenczi, G. Method of Compressing and Restoring Pulmonological FVC. Graphs. Patent Appl. P1100370/9, A61B 5/08, H03M 7/30, 8 July 2011. [Google Scholar]
- Australian Institute of Health and Welfare. Australian Institute of Health and Welfare Report. 2022. Available online: https://www.aihw.gov.au/reports-data/myhospitals/sectors/emergency-department-care (accessed on 11 May 2023).
- PMacfarlane, W.; Kennedy, J. Automated ECG Interpretation—A Brief History from High Expectations to Deepest Networks. Hearts 2021, 2, 433–448. [Google Scholar] [CrossRef]
- Bond, R.R.; Finlay, D.D.; Nugent, C.D.; Moore, G. A review of ECG storage formats. Int. J. Med. Inform. 2011, 80, 681–697. [Google Scholar] [CrossRef]
- Tran, T.; Kim, H.S.; Cho, H. A development of HL7 middleware for medical device communication. In Proceedings of the 5th ACIS International Conference on Software Engineering Research, Management & Applications (SERA 2007), Busan, Republic of Korea, 20–22 August 2007; IEEE: Piscataway, NJ, USA, 2007; pp. 485–492. [Google Scholar] [CrossRef]
- Chen, Y.; Wang, Z.; Liu, Y.; Wang, X.; Li, Y.; Ma, P.; Gu, B.; Li, H. Recent advances in rapid pathogen detection method based on biosensors. Eur. J. Clin. Microbiol. Infect. Dis. 2018, 37, 1021–1037. [Google Scholar] [CrossRef] [PubMed]
- Barnett, J.E.; Kolmes, K. The practice of tele-mental health: Ethical, legal, and clinical issues for practitioners. Pract. Innov. 2016, 1, 53. [Google Scholar] [CrossRef]
- Zhao, H.; Coote, S.; Easton, D.; Langenberg, F.; Stephenson, M.; Smith, K.; Bernard, S.; Cadilhac, D.A.; Kim, J.; Bladin, C.F. Melbourne mobile stroke unit and reperfusion therapy: Greater clinical impact of thrombectomy than thrombolysis. Stroke 2020, 51, 922–930. [Google Scholar] [CrossRef] [PubMed]
- Walter, S.; Kostopoulos, P.; Haass, A.; Keller, I.; Lesmeister, M.; Schlechtriemen, T.; Roth, C.; Papanagiotou, P.; Grunwald, I.; Schumacher, H. Diagnosis and treatment of patients with stroke in a mobile stroke unit versus in hospital: A randomised controlled trial. Lancet Neurol. 2012, 11, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Zanni, G. Telemedicine: Sorting out the benefits and obstacles. Consult. Pharm. 2011, 26, 810–824. [Google Scholar] [CrossRef]
- Brockes, C.; Grischott, T.; Dutkiewicz, M.; Schmidt-Weitmann, S. Evaluation of the education ‘Clinical Telemedicine/e-Health’ in the curriculum of medical students at the University of Zurich. Telemed. e-Health 2017, 23, 899–904. [Google Scholar] [CrossRef] [PubMed]
- Hall, J.L.; McGraw, D. For telehealth to succeed, privacy and security risks must be identified and addressed. Health Aff. 2014, 33, 216–221. [Google Scholar] [CrossRef] [PubMed]
- Gulick, P.G. E-health and the future of medicine: The economic, legal, regulatory, cultural, and organizational obstacles facing telemedicine and cybermedicine programs. Albany Law J. Sci. Technol. 2001, 12, 351. [Google Scholar]
- McIntosh, E.; Cairns, J. A framework for the economic evaluation of telemedicine. J. Telemed. Telecare 1997, 3, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Johnson, P. The clinical and economic advantages of remote, community-based physiological assessment. J. Telemed. Telecare 1998, 4 (Suppl. S1), 64–66. [Google Scholar] [CrossRef]
- Maiolo, C.; Mohamed, E.I.; Fiorani, C.M.; De Lorenzo, A. Home telemonitoring for patients with severe respiratory illness: The Italian experience. J. Telemed. Telecare 2003, 9, 67–71. [Google Scholar] [CrossRef]
- Jennett, P.A.; Affleck Hall, L.; Hailey, D.; Ohinmaa, A.; Anderson, C.; Thomas, R.; Young, B.; Lorenzetti, D.; Scott, R.E. The socio-economic impact of telehealth: A systematic review. J. Telemed. Telecare 2003, 9, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Hersh, W.R.; Hickam, D.H.; Severance, S.M.; Dana, T.L.; Krages, K.P.; Helfand, M. Diagnosis, access and outcomes: Update of a systematic review of telemedicine services. J. Telemed. Telecare 2006, 12 (Suppl. S2), S3–S31. [Google Scholar] [CrossRef]
- Bergman, D.A.; Sharek, P.J.; Ekegren, K.; Thyne, S.; Mayer, M.; Saunders, M. The use of telemedicine access to schools to facilitate expert assessment of children with asthma. Int. J. Telemed. Appl. 2008, 2008, 159276. [Google Scholar] [CrossRef] [PubMed]
- Huijgen, B.C.; Vollenbroek-Hutten, M.M.; Zampolini, M.; Opisso, E.; Bernabeu, M.; Van Nieuwenhoven, J.; Ilsbroukx, S.; Magni, R.; Giacomozzi, C.; Marcellari, V.; et al. Feasibility of a home-based telerehabilitation system compared to usual care: Arm/hand function in patients with stroke, traumatic brain injury and multiple sclerosis. J. Telemed. Telecare 2008, 14, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Moffatt, J.J.; Eley, D.S. The reported benefits of telehealth for rural Australians. Aust. Health Rev. 2010, 34, 276–281. [Google Scholar] [CrossRef]
- Ekeland, A.G.; Bowes, A.; Flottorp, S. Methodologies for assessing telemedicine: A systematic review of reviews. Int. J. Med. Inform. 2012, 81, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Bolte, R.; Walz, M.; Lehmann, K.J.; Hothorn, T.; Brill, C.; Hothorn, L.; Georgi, M. Teleradiology: Results of a questionnaire of German radiologists. J. Telemed. Telecare 1998, 4 (Suppl. S1), 69–71. [Google Scholar] [CrossRef]
- McLean, S.; Chandler, D.; Nurmatov, U.; Liu, J.; Pagliari, C.; Car, J.; Sheikh, A. Telehealthcare for asthma. Cochrane Database Syst. Rev. 2010, 10, CD007717. [Google Scholar] [CrossRef]
- Liu, W.T.; Huang, C.D.; Wang, C.H.; Lee, K.Y.; Lin, S.M.; Kuo, H.P. A mobile telephone-based interactive self-care system improves asthma control. Eur. Respir. J. 2011, 37, 310–317. [Google Scholar] [CrossRef]
- Roze, R.; Fisk, M. TeleSCoPE; Telemedicine Coventry University: Coventry, UK, 2013. [Google Scholar]
- Davalos, M.E.; French, M.T.; Burdick, A.E.; Simmons, S.C. Economic evaluation of telemedicine: Review of the literature and research guidelines for benefit-cost analysis. Telemed. e-Health 2009, 15, 933–948. [Google Scholar] [CrossRef] [PubMed]
- Moffatt, J.J.; Eley, D.S. Barriers to the up-take of telemedicine in Australia—A view from providers. Rural. Remote Health 2011, 11, 116–121. [Google Scholar] [CrossRef]
- Mehrotra, A.; Bhatia, R.S.; Snoswell, C.L. Paying for Telemedicine After the Pandemic. JAMA J. Am. Med. Assoc. 2021, 325, 431–432. [Google Scholar] [CrossRef] [PubMed]
- Aacharya, R.P.; Gastmans, C.; Denier, Y. Emergency department triage: An ethical analysis. BMC Emerg. Med. 2011, 11, 16. [Google Scholar] [CrossRef]
- Kha, Q.H.; Le, V.H.; Hung, T.N.K.; Nguyen, N.T.K.; Le, N.Q.K. Development and Validation of an Explainable Machine Learning-Based Prediction Model for Drug-Food Interactions from Chemical Structures. Sensors 2023, 23, 3962. [Google Scholar] [CrossRef]
- Kha, Q.H.; Tran, T.O.; Nguyen, T.T.; Nguyen, V.N.; Than, K.; Le, N.Q.K. An interpretable deep learning model for classifying adaptor protein complexes from sequence information. Methods 2022, 207, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Baron, J.A. Uncertainty in Bayes. Med. Decis. Mak. 1994, 14, 46–51. [Google Scholar] [CrossRef] [PubMed]



| Protocol | Characteristics | Modalities |
|---|---|---|
| HL7 | Health Level 7, global med-tech data standard | ECG, respiratory, vital signs |
| XML | General data standard, widely configurable, not only medical data | Vital signs, descriptive health data |
| DICOM | Imaging specific standard | Ultrasound, optical, thermal, X-ray-based and also advanced imaging including mobile CT |
| Video feeds | VGA or any higher-resolution real-time data transfer | Vital signs, general patient observation |
| GDT | GerateDatenTrager, originally German standard, similar to HL7, descriptive | ECG, respiratory, vital signs |
| USB over TCP/IP | Virtual telemedicine: the remote medical device is emulated to be local | ECG, spirometer, vital signs |
| Sockets over TCP/IP | Suitable for any custom medical device software | Portable diagnostic systems including rapid labs |
| Technology | Characteristics | Means of Use | |
|---|---|---|---|
| Video (Tele-video link) | Resolution adaptive to bandwidth, best-throughput | CINE recording, optimal 30 s CINE shots, the first one triggered by a motion detector | |
| Patient monitoring systems Vital signs sensors | SpO2 | Haemoglobin saturation levels, 60–99% resolution | Blood oxygenation estimation, finger clip or ear clip, feet clip for infants |
| Temperature | Digital thermometer | Surface patch | |
| Pulse | Derived from oximeter, ECG signal or basic sensor | Heart rate detection | |
| Breathing (respiratory rate) | May be derived from ECG signal or surface sensor or mask | Basic respiratory function detection and estimations | |
| Blood pressure | Cuff-based, ABPM preferred | Cyclic automated inflation | |
| Basic ECG | Disposable or reusable electrodes or silicone vest | Cardiovascular function estimations | |
| Advanced ECG | 12-channel advanced ECG with automated diagnostic support system, disposable or reusable electrodes or silicone vest | Detailed cardiac diagnosis, recorded in high-resolution format to be sent ahead to the hospital | |
| Advanced respiratory diagnostics | Portable emergency ventilator-derived respiratory function or CPAP; portable PFT/spirometer | Lung function testing and diagnostics | |
| Defibrillator | Automated AED, portable | Drastic emergency cardiac intervention | |
| Oxygen | Cylinder or oxygen generator | Lung function support | |
| Rapid intervention items | spine boards, cervical (neck), collars, splints, bandages | Rapid manual intervention, temporary stabilisation | |
| Range of drugs and intravenous fluids | e.g., vasodilators, pain killers, antibiotics | Infection control and stabilising drugs | |
| Imaging | Ultrasound, thermal or optical imaging, or in advanced cases, X-ray-based | Unfortunately, as most high-resolution imaging modalities are radiation-based technologies, only a very limited set of choices is available for ambulances | |
| Protocol | Characteristics | Field of Use |
|---|---|---|
| Short Messaging Service/MMS | Fast, inexpensive, widely available | Still has a relevance in Australia as GSM data availability is limited |
| TCP/IP | Mobile Internet | Vital signs, descriptive health data |
| UDP/IP | Short signal-based mobile data | Vital signs, emergency information |
| Urgency | Estimated Number of Ambulances | |||||||
|---|---|---|---|---|---|---|---|---|
| Resuscitation (5) | Emergency (4) | Urgent (3) | Semi-Urgent (2) | Non-Urgent (1) | Total | |||
| Condition type | Injury | 3.1% | 20.9% | 42.3% | 32.4% | 1.2% | 19.9% | 3 |
| Infection | 1.7% | 21.2% | 50.6% | 24.6% | 2.0% | 7.2% | 1 | |
| Mental | 2.8% | 23.9% | 52.0% | 17.4% | 3.9% | 6.4% | 1 | |
| Other | 1.7% | 28.3% | 52.3% | 17.3% | 0.5% | 60.7% | 9 | |
| Cardiac | 9.7% | 53.2% | 32.2% | 4.8% | 0.1% | 5.8% | 1 | |
| TOTAL | 2.5% | 27.5% | 49.0% | 20.1% | 0.9% | 100% | 15 | |
| Sequence Number | Case ID | Case Type | Urgency | Requires Treatment Time upon Arrival | Time to Hospital (Hours) | Est. Minimum Survival Time | Late for Medical Attention |
|---|---|---|---|---|---|---|---|
| 1 | AMB1 | Other | 3 | within 30 min | 0.50 | 6–72 h | no |
| 2 | AMB2 | Other | 2 | within 2 h | 1.00 | 24 h–7 days | no |
| 3 | AMB3 | Injury | 3 | within 30 min | 1.50 | 6–72 h | no |
| 4 | AMB4 | Other | 3 | within 30 min | 2.00 | 6–72 h | no |
| 5 | AMB5 | Mental | 3 | within 30 min | 2.50 | 6–72 h | no |
| 6 | AMB6 | Other | 3 | within 30 min | 3.00 | 6–72 h | no |
| 7 | AMB7 | Injury | 4 | withing 10 min | 3.50 | <4 h | no |
| 8 | AMB8 | Other | 4 | withing 10 min | 4.00 | <4 h | at risk |
| 9 | AMB9 | Infection | 3 | within 30 min | 4.50 | 6–72 h | no |
| 10 | AMB10 | Other | 4 | withing 10 min | 5.00 | <4 h | yes |
| 11 | AMB11 | Injury | 2 | within 2 h | 5.50 | 24 h–7 days | no |
| 12 | AMB12 | Other | 4 | withing 10 min | 6.00 | <4 h | yes |
| 13 | AMB13 | Cardiac | 5 | immediately | 6.50 | <30 min | yes |
| 14 | AMB14 | Other | 3 | within 30 min | 7.00 | 6–72 h | at risk |
| 15 | AMB15 | Other | 3 | within 30 min | 7.50 | 6–72 h | at risk |
| Sequence Number | Case ID | Case Type | Urgency | Requires Treatment Time upon Arrival | Time to Hospital (Hours) | Est. Minimum Survival Time | Late for Medical Attention |
|---|---|---|---|---|---|---|---|
| 1 | AMB13 | Cardiac | 5 | immediately | 0.50 | <30 min | no |
| … | |||||||
| 7 | AMB6 | Other | 3 | within 30 min | 3.50 | 6–72 h | no |
| 8 | AMB7 | Injury | 4 | within 10 min | 4.00 | <4 h | at risk |
| 9 | AMB8 | Other | 4 | within 10 min | 4.50 | <4 h | yes |
| 10 | AMB9 | Infection | 3 | within 30 min | 5.00 | 6–72 h | no |
| 11 | AMB10 | Other | 4 | within 10 min | 5.50 | <4 h | yes |
| 12 | AMB11 | Injury | 2 | within 2 h | 6.00 | 24 h–7 days | no |
| 13 | AMB12 | Other | 4 | within 10 min | 6.50 | <4 h | yes |
| 14 | AMB14 | Other | 3 | within 30 min | 7.00 | 6–72 h | at risk |
| 15 | AMB15 | Other | 3 | within 30 min | 7.50 | 6–72 h | at risk |
| Sequence Number | Case ID | Case Type | Urgency | Requires Treatment Time upon Arrival | Time to Hospital (Hours) | Est. Minimum Survival Time | Late for Medical Attention |
|---|---|---|---|---|---|---|---|
| 1 | AMB13 | Cardiac | 5 | immediately | 0.50 | <30 min | no |
| 2 | AMB8 | Other | 4 | within 10 min | 1.00 | <4 h | no |
| 3 | AMB7 | Injury | 4 | within 10 min | 1.50 | <4 h | no |
| 4 | AMB9 | Other | 4 | within 10 min | 2.00 | <4 h | no |
| 5 | AMB12 | Other | 4 | within 10 min | 2.50 | <4 h | no |
| 6 | AMB1 | Other | 3 | within 30 min | 3.00 | 6–72 h | no |
| … | |||||||
| 11 | AMB6 | Other | 3 | within 30 min | 5.50 | 6–72 h | no |
| 12 | AMB10 | Infection | 3 | within 30 min | 6.00 | 6–72 h | at risk |
| 13 | AMB11 | Injury | 2 | within 2 h | 6.50 | 24 h–7 days | no |
| 14 | AMB14 | Other | 3 | within 30 min | 7.00 | 6–72 h | at risk |
| 15 | AMB15 | Other | 3 | within 30 min | 7.50 | 6–72 h | at risk |
| Sequence Number | Case ID | Case Type | Urgency | Requires Treatment Time upon Arrival | Time to Hospital (Hours) | Est. Minimum Survival Time | Late for Medical Attention |
|---|---|---|---|---|---|---|---|
| 1 | AMB13 | Cardiac | 5 | immediately | 0.50 | <30 min | no |
| 2 | AMB8 | Other | 4 | within 10 min | 1.00 | <4 h | no |
| 3 | AMB7 | Injury | 4 | within 10 min | 1.50 | <4 h | no |
| 4 | AMB9 | Other | 4 | within 10 min | 2.00 | <4 h | no |
| 5 | AMB12 | Other | 4 | within 10 min | 2.50 | <4 h | no |
| 6 | AMB10 | Infection | 3 | within 30 min | 3.00 | 6–72 h | no |
| 7 | AMB1 | Other | 3 | within 30 min | 3.50 | 6–72 h | no |
| … | |||||||
| 12 | AMB6 | Other | 3 | within 30 min | 6.00 | 6–72 h | no |
| 13 | AMB11 | Injury | 2 | within 2 h | 6.50 | 24 h–7 days | no |
| 14 | AMB14 | Other | 3 | within 30 min | 7.00 | 6–72 h | at risk |
| 15 | AMB15 | Other | 3 | within 30 min | 7.50 | 6–72 h | at risk |
| Sequence Number | Case ID | Case Type | Urgency | Requires Treatment Time upon Arrival | Time to Hospital (Hours) | Est. Minimum Survival Time | Late for Medical Attention |
|---|---|---|---|---|---|---|---|
| 1 | AMB13 | Cardiac | 5 | immediately | 0.50 | <30 min | no |
| 2 | AMB8 | Other | 4 | within 10 min | 1.00 | <4 h | no |
| 3 | AMB7 | Injury | 4 | within 10 min | 1.50 | <4 h | no |
| 4 | AMB9 | Other | 4 | within 10 min | 2.00 | <4 h | no |
| 5 | AMB12 | Other | 4 | within 10 min | 2.50 | <4 h | no |
| 6 | AMB10 | Infection | 3 | within 30 min | 3.00 | 6–72 h | no |
| 7 | AMB14 | Other | 3 | within 30 min | 3.50 | 6–72 h | no |
| 8 | AMB15 | Other | 3 | within 30 min | 4.00 | 6–72 h | no |
| 9 | AMB5 | Mental | 3 | within 30 min | 4.50 | 6–72 h | no |
| 10 | AMB1 | Other | 3 | within 30 min | 5.00 | 6–72 h | no |
| 11 | AMB2 | Other | 2 | within 2 h | 5.50 | 24 h–7 days | no |
| 12 | AMB3 | Injury | 3 | within 30 min | 6.00 | 6–72 h | no |
| 13 | AMB4 | Other | 3 | within 30 min | 6.50 | 6–72 h | at risk |
| 14 | AMB6 | Other | 3 | within 30 min | 7.00 | 6–72 h | at risk |
| 15 | AMB11 | Injury | 2 | within 2 h | 7.50 | 24 h–7 days | no |
| Urgency | |||||||
|---|---|---|---|---|---|---|---|
| P(A) | Resuscitation (5) | Emergency (4) | Urgent (3) | Semi-urgent (2) | Non-urgent (1) | Total | |
| Condition type | Injury | 0.63% | 4.17% | 8.43% | 6.45% | 0.24% | 19.9% |
| Infection | 0.12% | 1.52% | 3.63% | 1.76% | 0.14% | 7.2% | |
| Mental | 0.18% | 1.53% | 3.34% | 1.12% | 0.25% | 6.4% | |
| Other | 1.00% | 17.21% | 31.74% | 10.48% | 0.29% | 60.7% | |
| Cardiac | 0.56% | 3.07% | 1.86% | 0.27% | 0.01% | 5.8% | |
| TOTAL | 2.50% | 27.50% | 49.00% | 20.10% | 0.90% | 100.00% | |
| P(A15) | Resuscitation (5) | Emergency (4) | Urgent (3) | Semi-urgent (2) | Non-urgent (1) | ||
| Condition type | Injury | 0.04% | 0.27% | 0.54% | 0.42% | 0.02% | |
| Infection | 0.01% | 0.10% | 0.24% | 0.12% | 0.01% | ||
| Mental | 0.01% | 0.10% | 0.22% | 0.07% | 0.02% | ||
| Other | 0.07% | 1.07% | 1.86% | 0.67% | 0.02% | ||
| Cardiac | 0.04% | 0.20% | 0.12% | 0.02% | 0.00% | ||
| Probability of Case Occurring | |||||
|---|---|---|---|---|---|
| Overall | In any One Step of a Sequence of 15 | Not in the First Step of a Sequence of 15 | |||
| Cardiac—level 5 | 0.56% | 0.04% | 0.52% | ||
| Cardiac—levels 4/5 | 3.63% | 0.24% | 3.27% | ||
| Cardiac—levels 3/4/5 | 5.48% | 0.36% | 4.50% | ||
| Injury—level 5 | 0.63% | 0.04% | 0.58% | ||
| Injury—levels 4/5 | 4.80% | 0.31% | 4.28% | ||
| Injury—levels 3/4/5 | 13.23% | 0.83% | 10.12% | ||
| Infection—level 5 | 0.12% | 0.01% | 0.11% | ||
| Infection—levels 4/5 | 1.64% | 0.11% | 1.51% | ||
| Infection—levels 3/4/5 | 5.27% | 0.34% | 4.34% | ||
| Mental—level 5 | 0.18% | 0.01% | 0.17% | ||
| Mental—levels 4/5 | 1.71% | 0.11% | 1.57% | ||
| Mental—levels 3/4/5 | 5.05% | 0.33% | 4.17% | ||
| Other—level 5 | 1.00% | 0.07% | 0.93% | ||
| Other—levels 4/5 | 18.22% | 1.12% | 14.45% | ||
| Other—levels 3/4/5 | 49.96% | 2.74% | 28.66% | ||
| Total | - | - | 2.31% | 25.1% | 51.8% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferenczi, G.L.; Perényi, Á. Modelling the Application of Telemedicine in Emergency Care. Inventions 2023, 8, 115. https://doi.org/10.3390/inventions8050115
Ferenczi GL, Perényi Á. Modelling the Application of Telemedicine in Emergency Care. Inventions. 2023; 8(5):115. https://doi.org/10.3390/inventions8050115
Chicago/Turabian StyleFerenczi, Gyoergy (George) L., and Áron Perényi. 2023. "Modelling the Application of Telemedicine in Emergency Care" Inventions 8, no. 5: 115. https://doi.org/10.3390/inventions8050115
APA StyleFerenczi, G. L., & Perényi, Á. (2023). Modelling the Application of Telemedicine in Emergency Care. Inventions, 8(5), 115. https://doi.org/10.3390/inventions8050115






