Novel Device Used to Monitor Hand Tremors during Nocturnal Hypoglycemic Events
Abstract
:1. Introduction
2. Materials and Methods
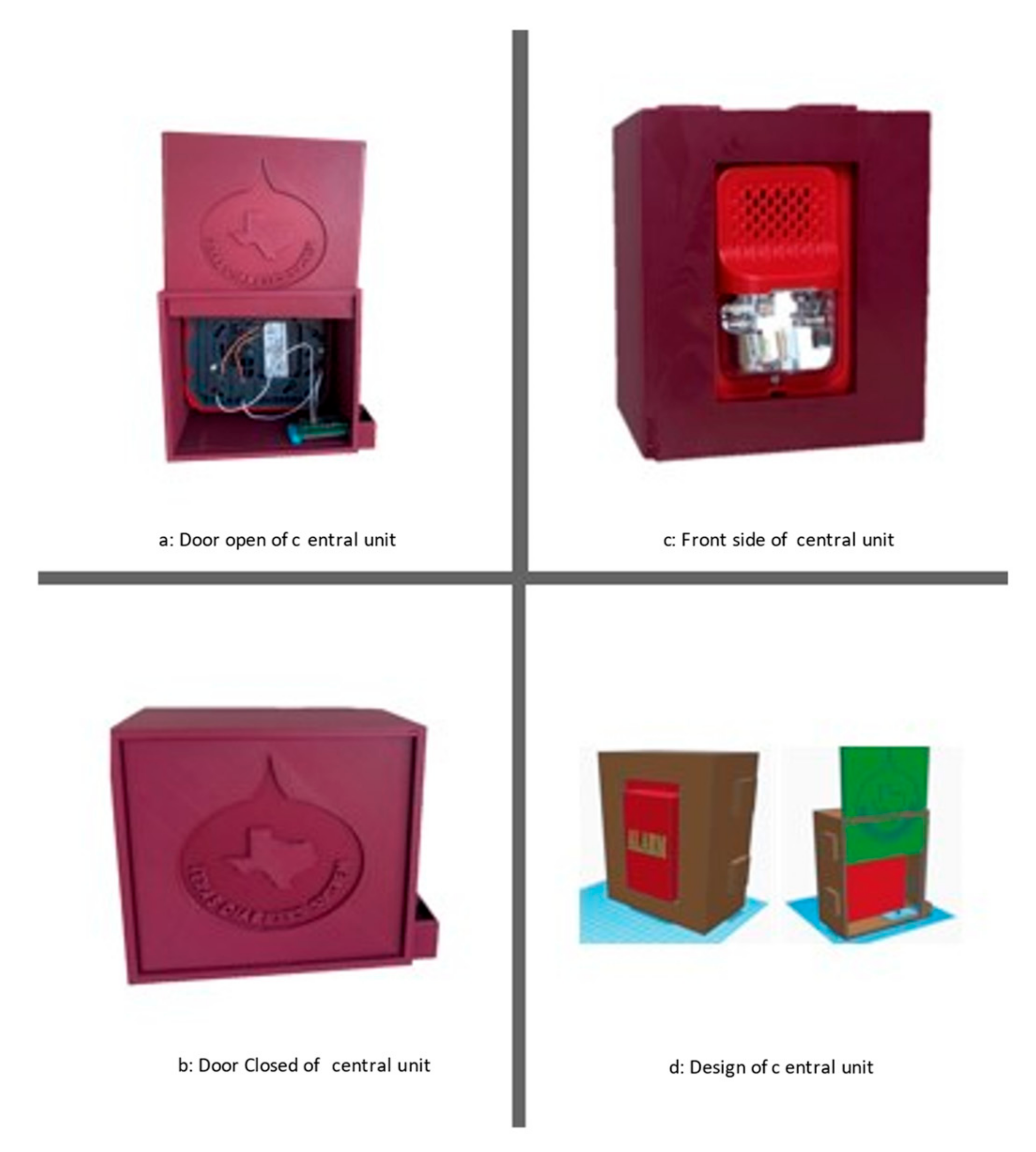
2.1. General Description
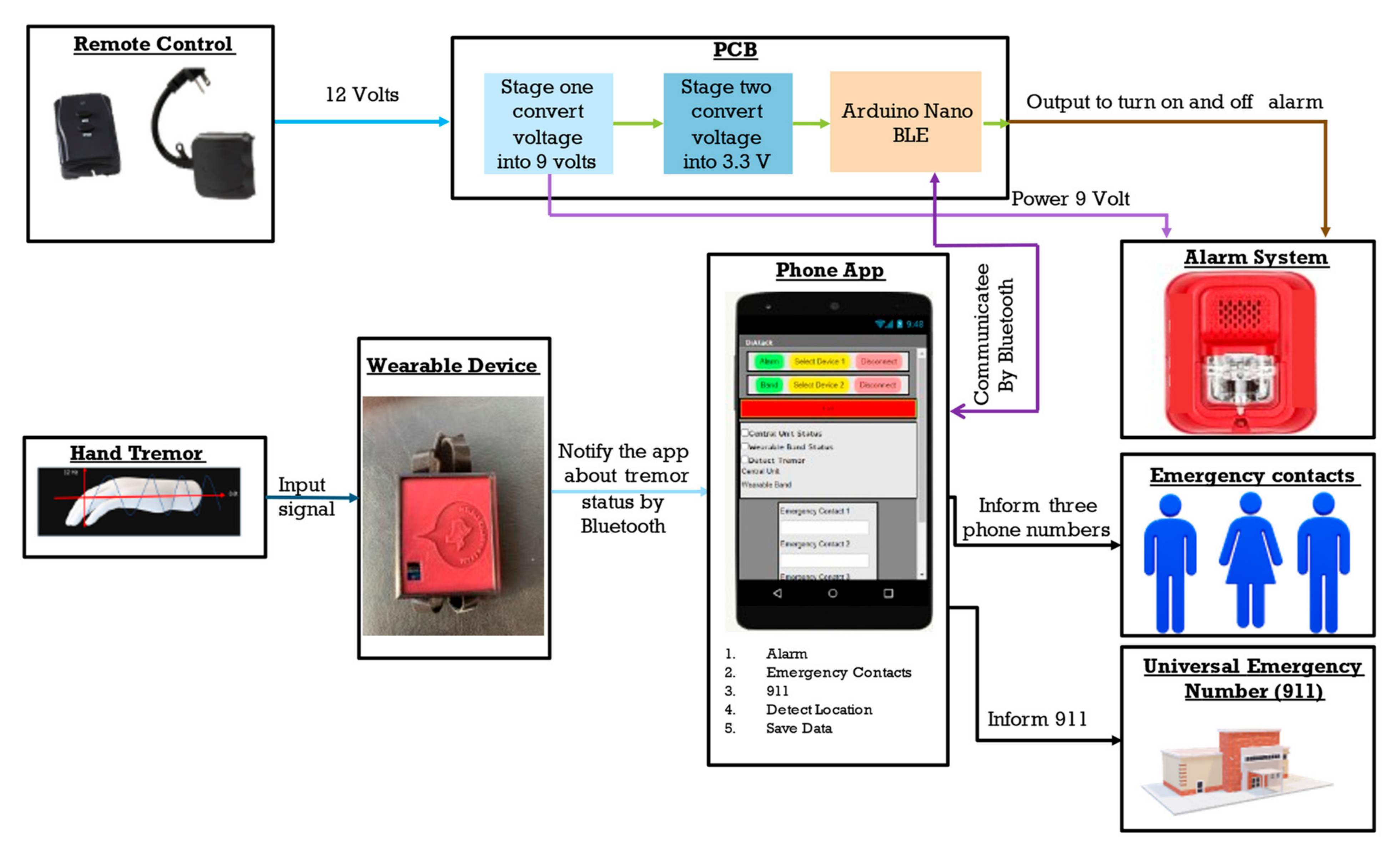
2.2. Conceptual Block Diagram
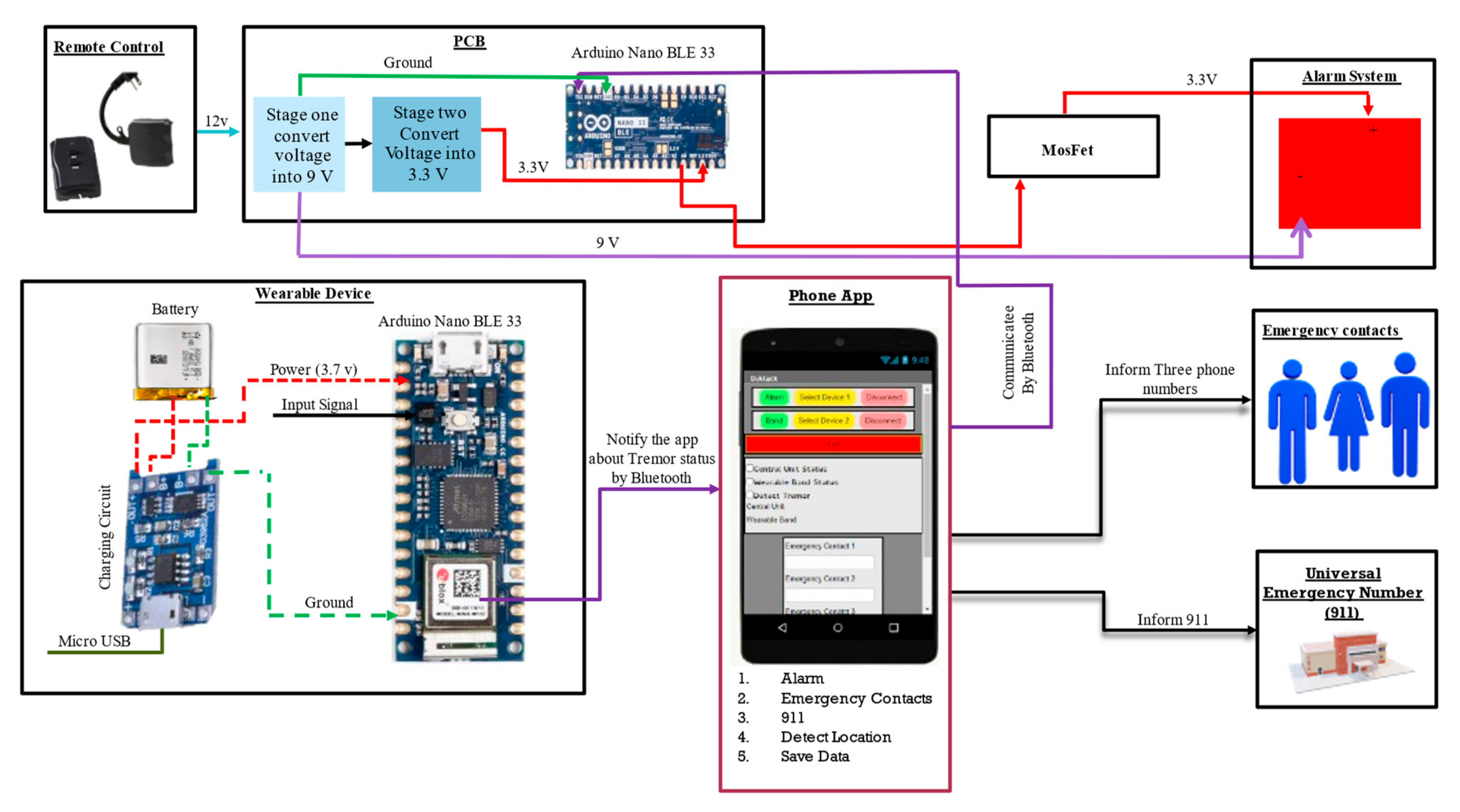
2.3. Functional Block Diagram
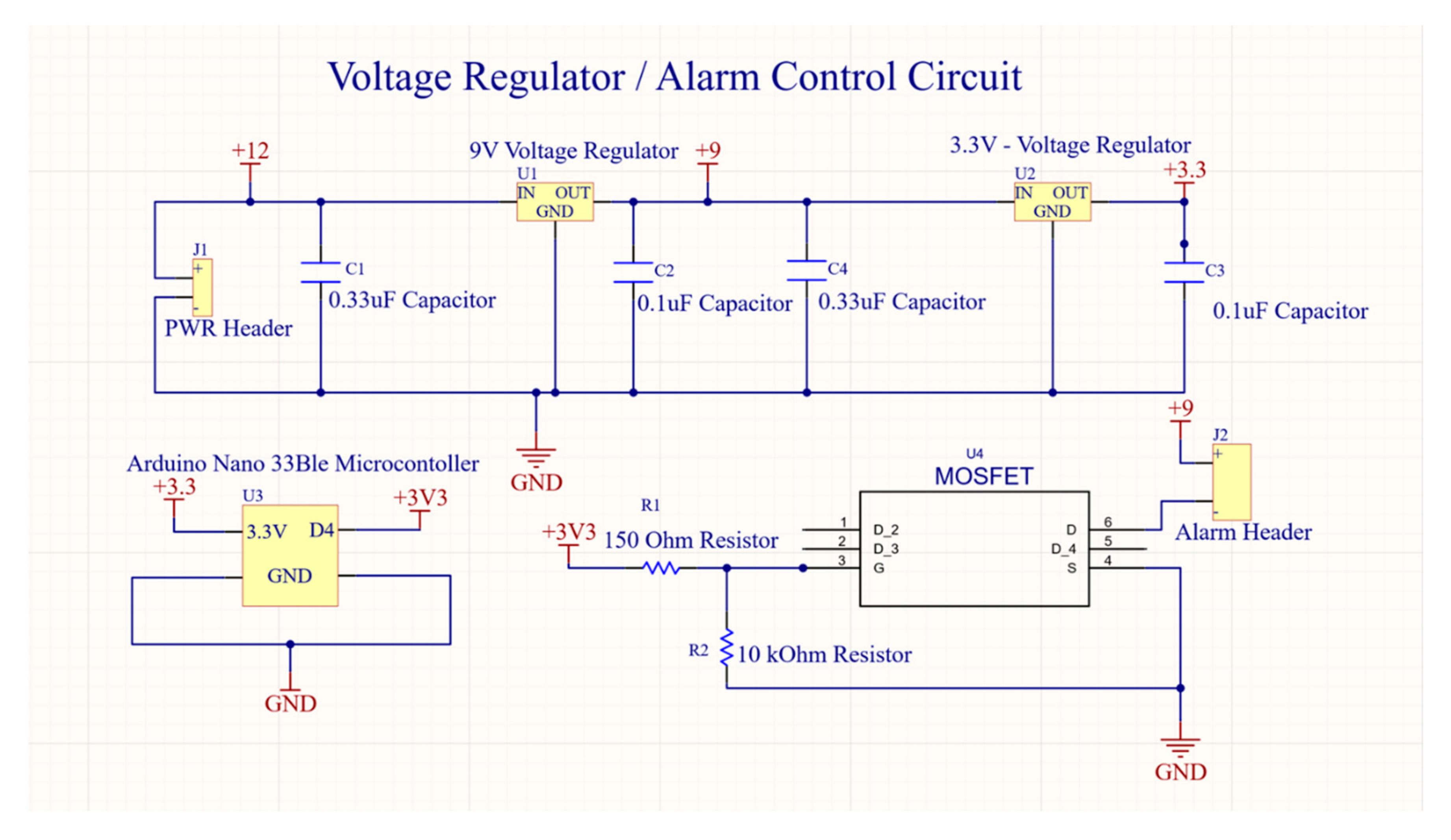
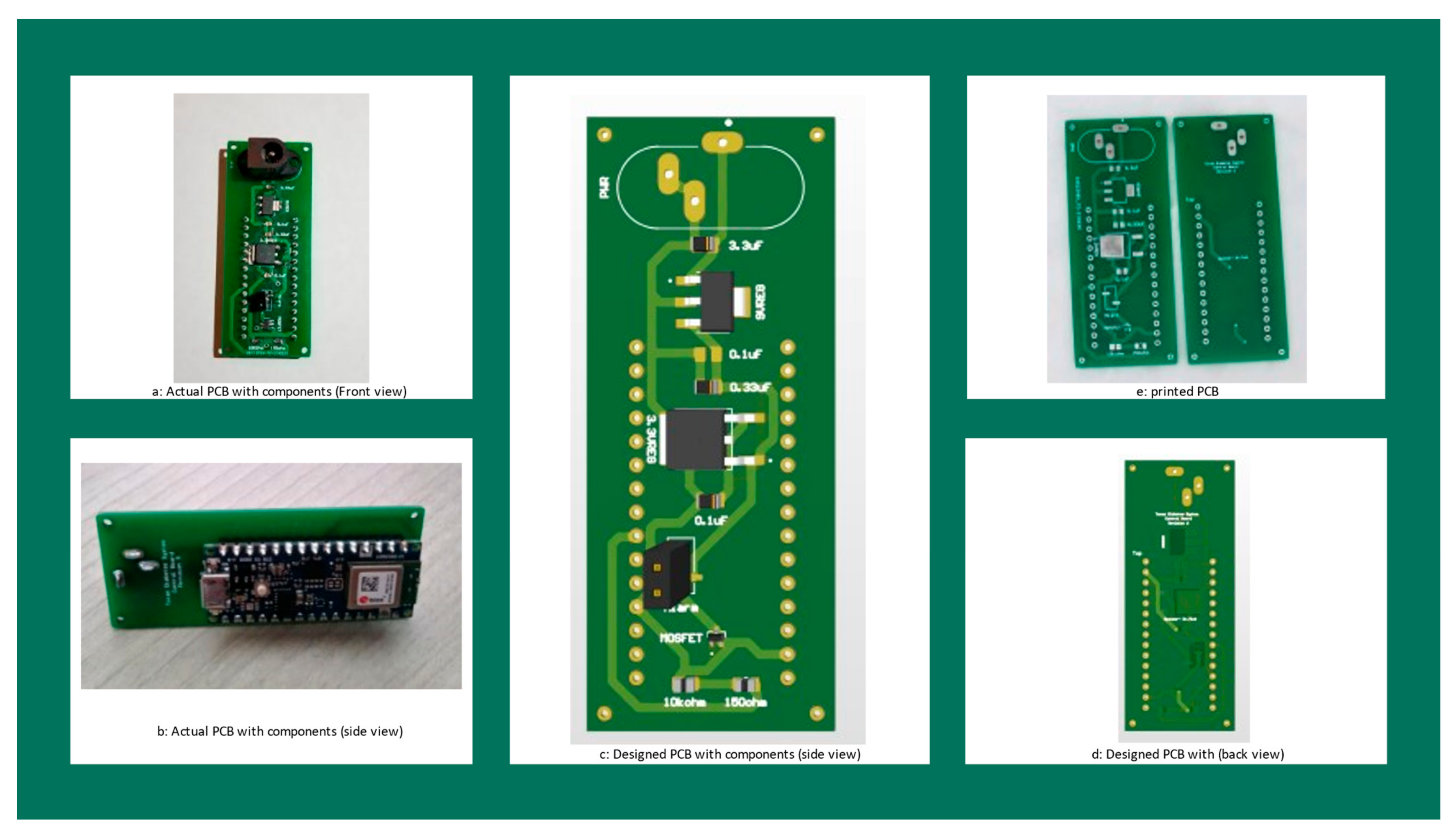
2.4. Printed Circuit Board (PCB)
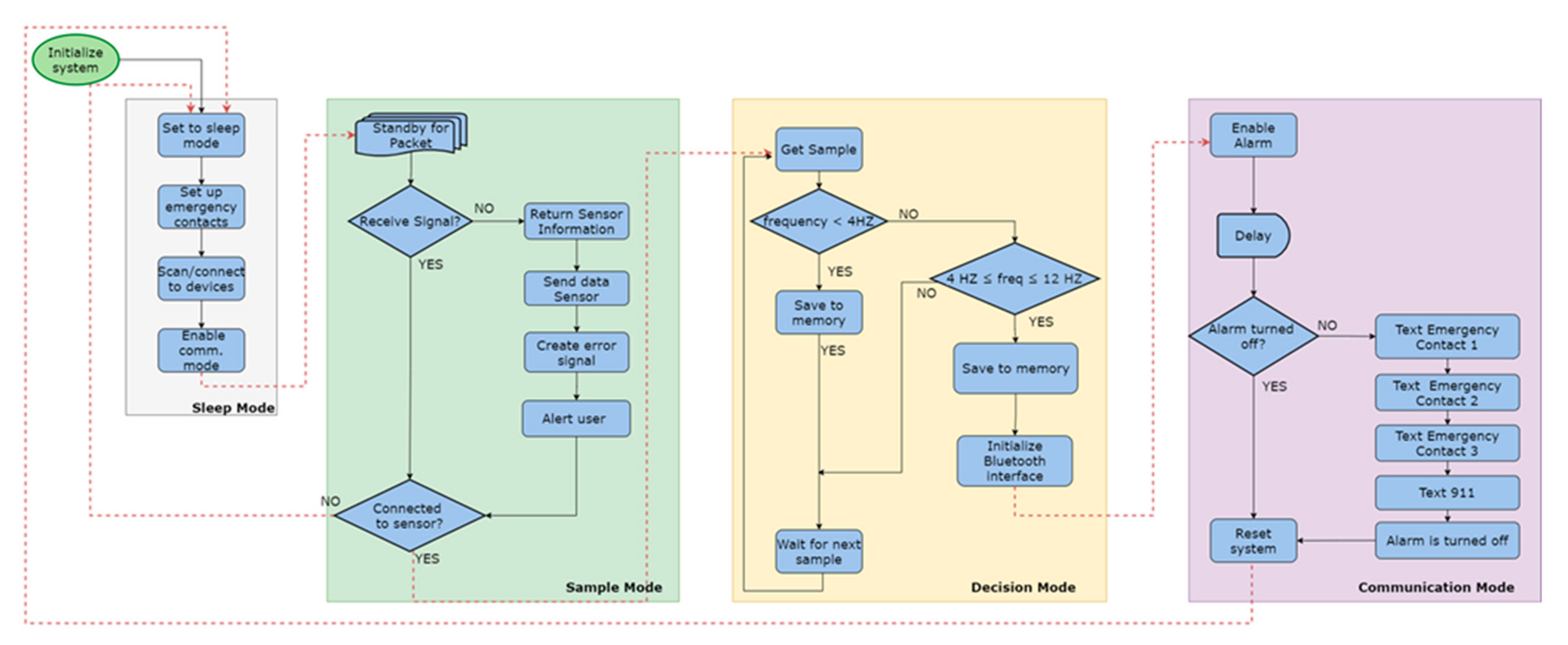
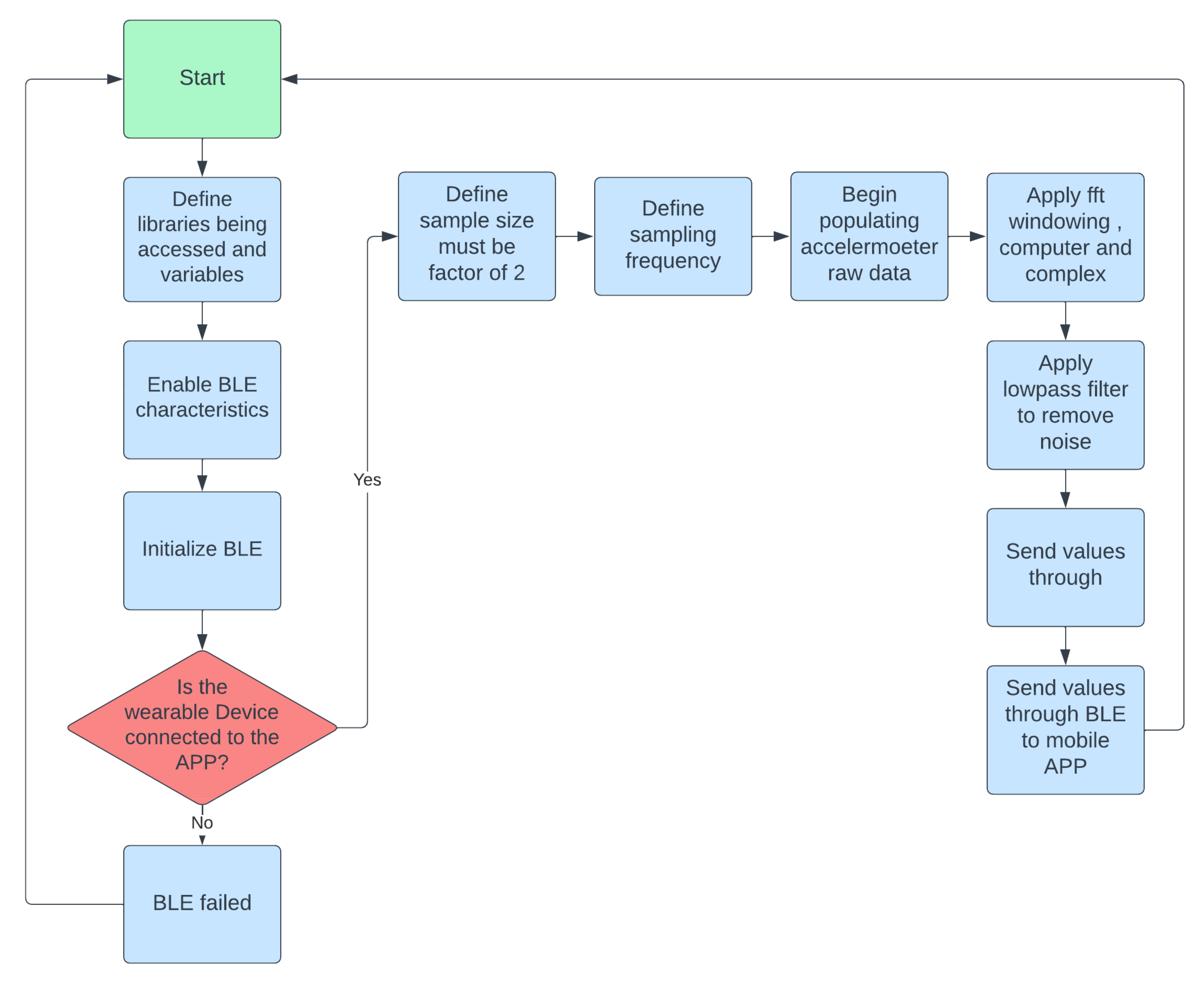
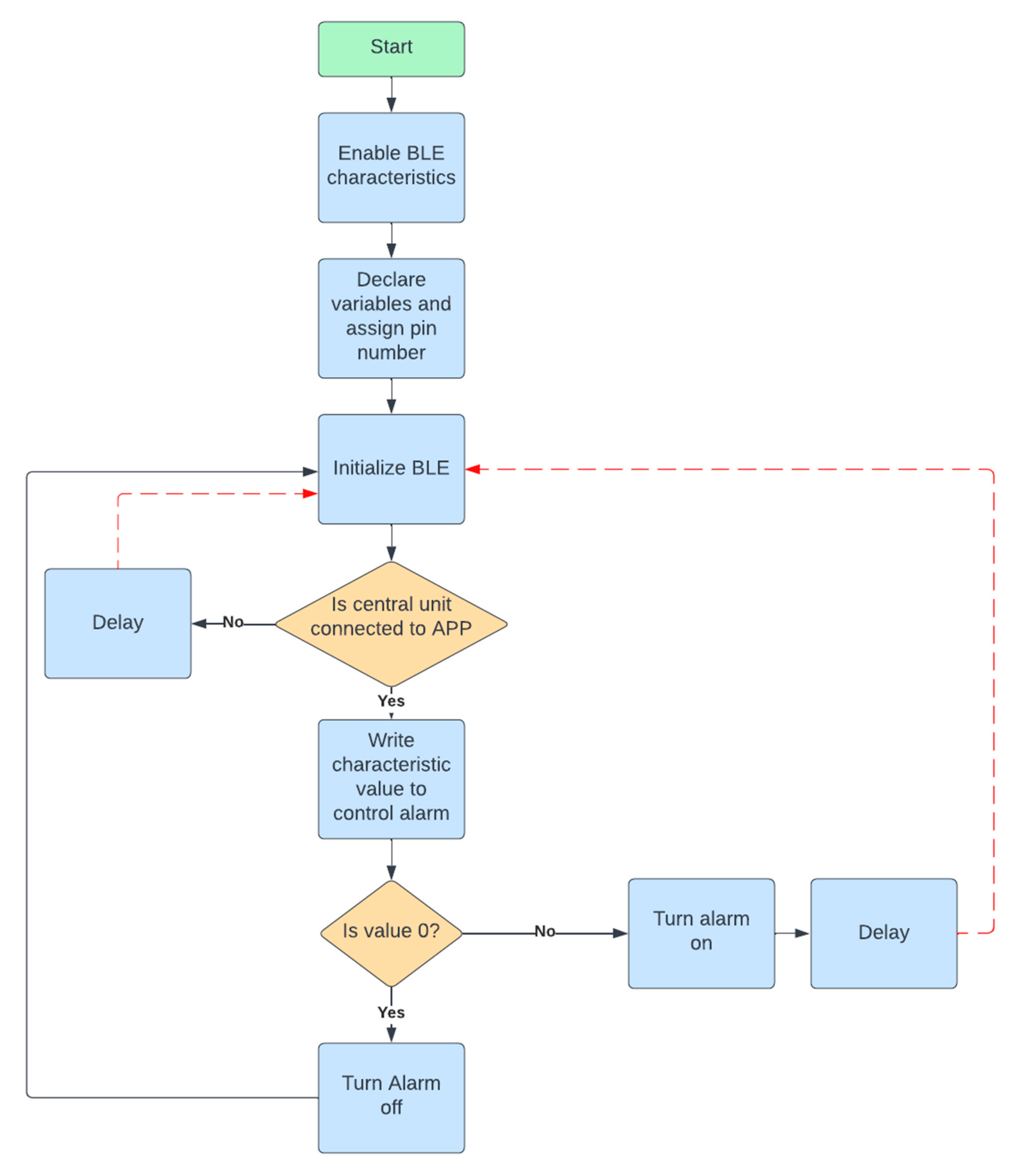
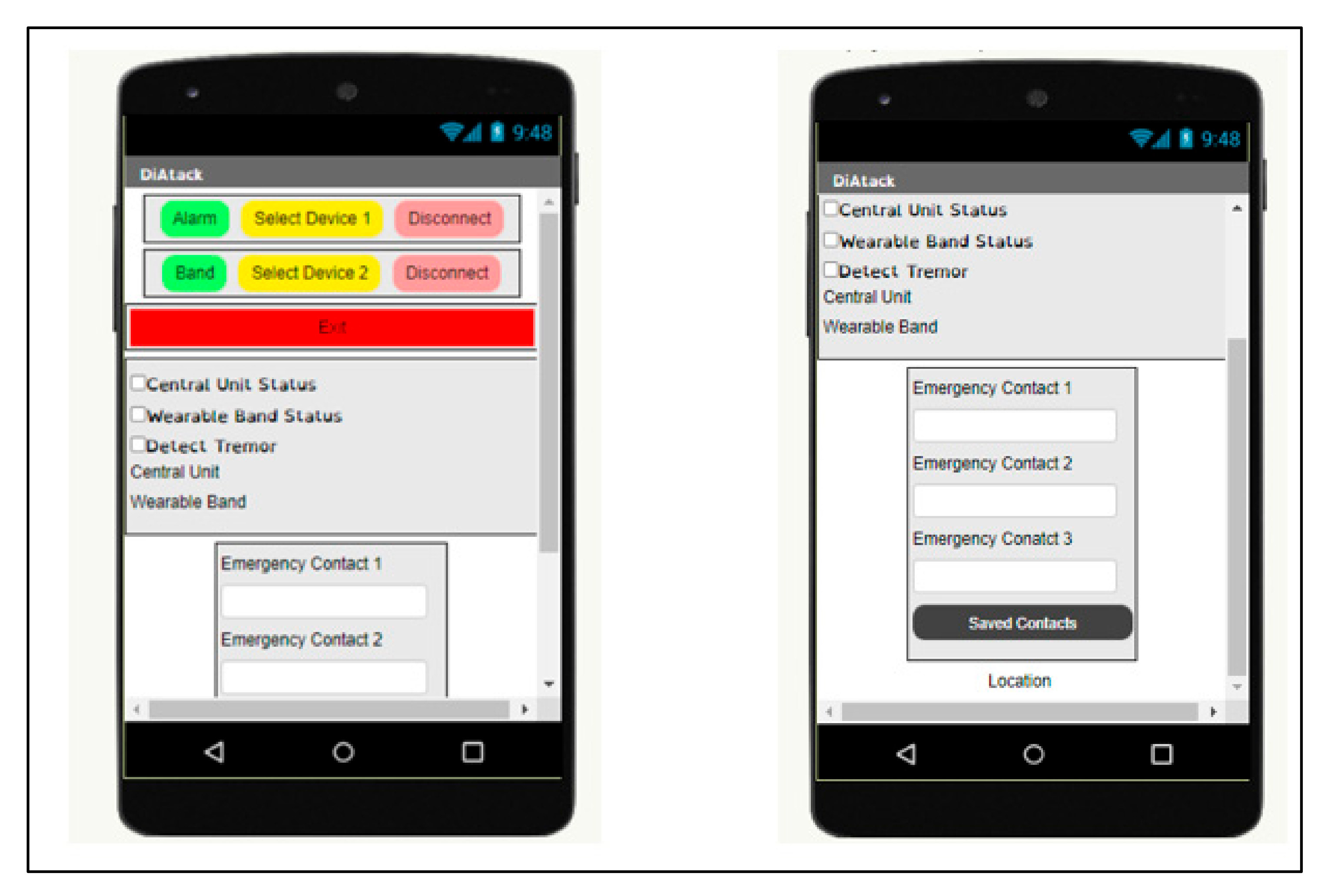
2.5. Software Flowchart/Algorithm
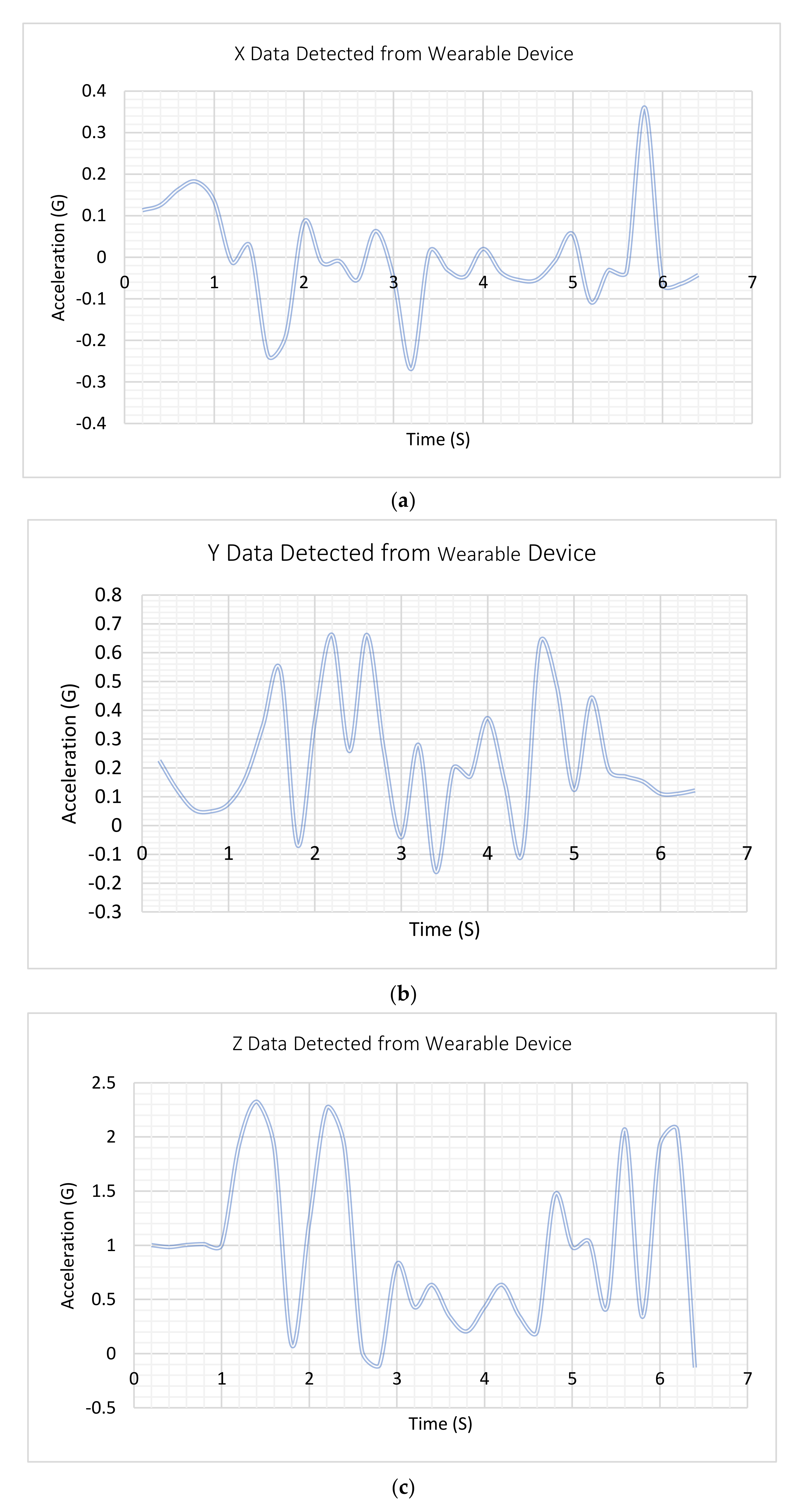
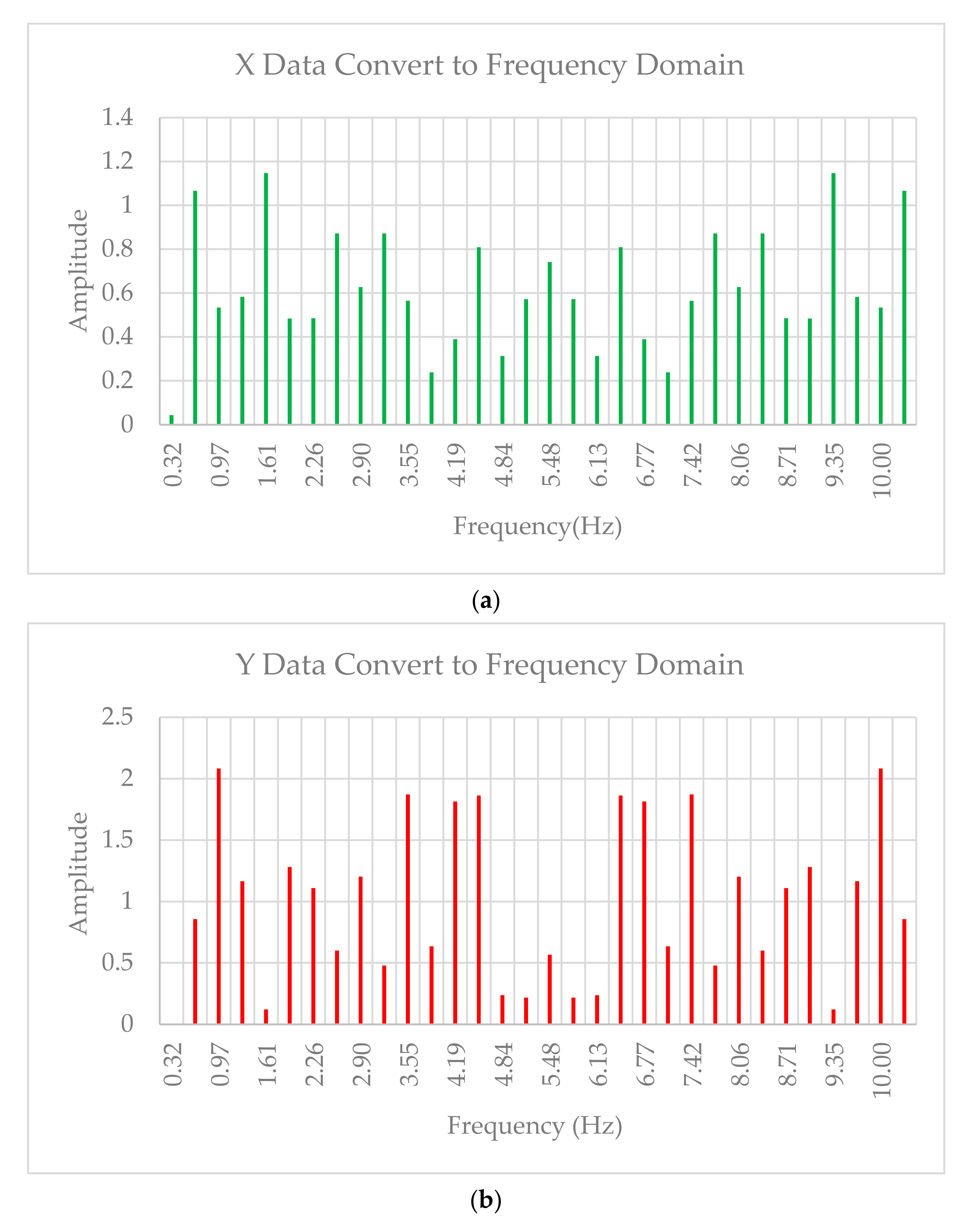
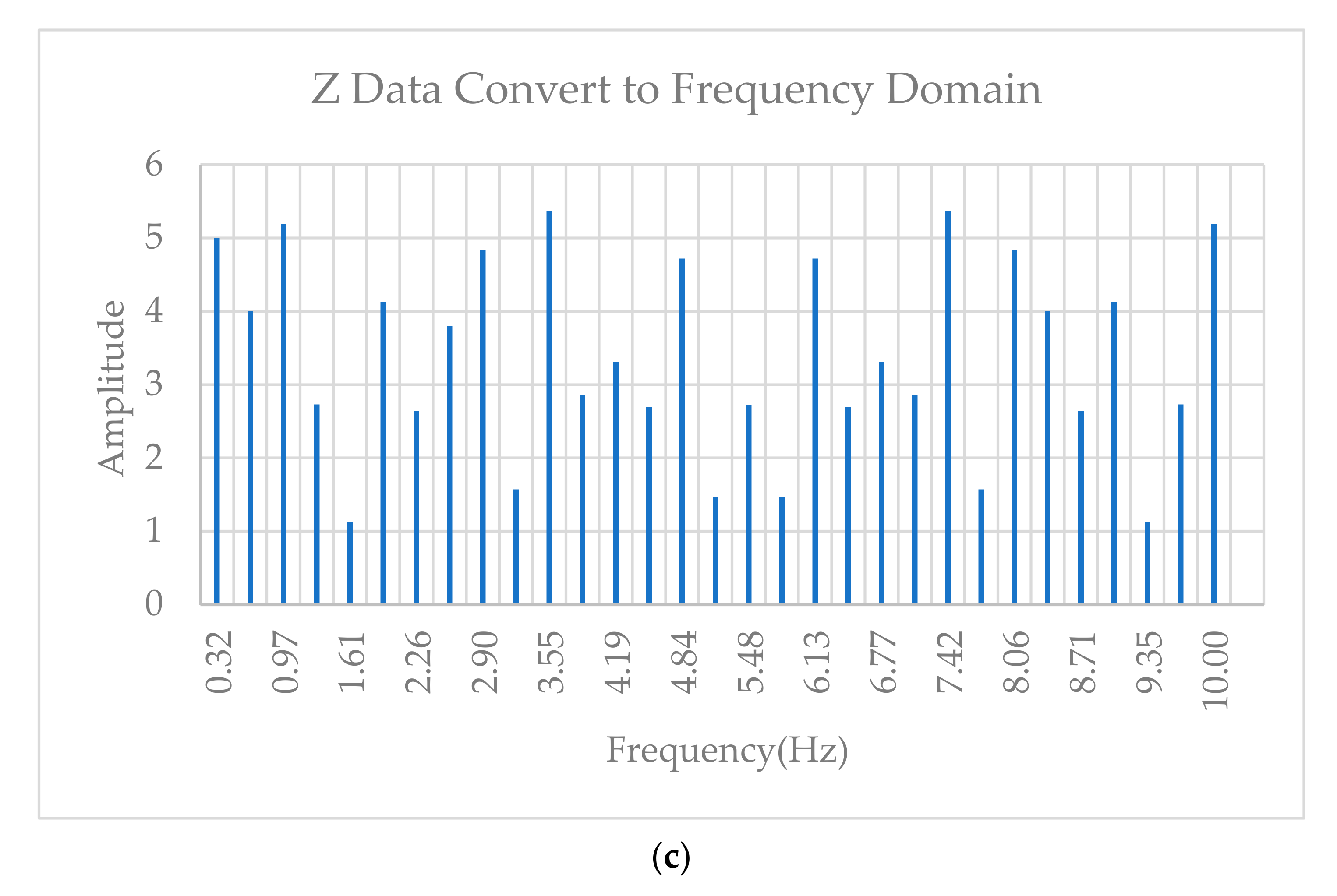
2.6. Frequency-Time Domain Transformation
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Nomenclature
| Fourier transformation | |
| Inverse Fourier Transformation | |
| Discrete Fourier Transformation | |
| Inverse discrete Fourier Transformation | |
| N | Number of samples |
| j | Imaginary numbers |
| fT | Sample frequency |
| Distance between time samples | |
| Distance between frequency samples. |
References
- CDC. New CDC Report: More than 100 Million Americans Have Diabetes or Prediabetes; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2018. [Google Scholar]
- Abdelhamid, Y.A.; Bernjak, A.; Phillips, L.K.; Summers, M.J.; Weinel, L.M.; Lange, K.; Chow, E.; Kar, P.; Horowitz, M.; Heller, S.; et al. Nocturnal Hypoglycemia in Patients With Diabetes Discharged From ICUs: A Prospective Two-Center Cohort Study. Crit. Care Med. 2021, 49, 636–649. [Google Scholar] [CrossRef]
- Jones, A.G.; McDonald, T.J.; Shields, B.M.; Hagopian, W.; Hattersley, A.T. Latent Autoimmune Diabetes of Adults (LADA) Is Likely to Represent a Mixed Population of Autoimmune (Type 1) and Nonautoimmune (Type 2) Diabetes. Diabetes Care 2021, 44, 1243–1251. [Google Scholar] [CrossRef] [PubMed]
- Saito, K.; Okada, Y.; Torimoto, K.; Takamatsu, Y.; Tanaka, Y. Blood glucose dynamics during sleep in patients with obstructive sleep apnea and normal glucose tolerance: Effects of CPAP therapy. Sleep Breath. 2021, 1–11. [Google Scholar] [CrossRef]
- Boscari, F.; Ferretto, S.; Cavallin, F.; Bruttomesso, D. Switching from predictive low glucose suspend to advanced hybrid closed loop control: Effects on glucose control and patient reported outcomes. Diabetes Res. Clin. Pract. 2022, 185, 109784. [Google Scholar] [CrossRef]
- Yorgason, J.B.; Saylor, J.; Ness, M.; Millett, M.; Floreen, A. Emerging Ideas. Health Technology Use and Perceptions of Romantic Relationships by Emerging Adults With Type 1 Diabetes. Fam. Relat. 2021, 70, 1427–1434. [Google Scholar] [CrossRef]
- Reno, C.M. Severe hypoglycemia-induced sudden death is mediated by both cardiac arrhythmias and seizures. Am. J. Physiol. Endocrinol. Metab. 2018, 315, E240–E249. [Google Scholar]
- Picerno, P.; Iosa, M.; D’Souza, C.; Benedetti, M.G.; Paolucci, S.; Morone, G. Wearable inertial sensors for human movement analysis: A five-year update. Expert Rev. Med. Devices 2021, 18, 79–94. [Google Scholar] [CrossRef]
- Stiles, R.N. Frequency and displacement amplitude relations for normal hand tremor. J. Appl. Physiol. 1976, 40, 44–54. [Google Scholar] [CrossRef]
- Elble, R.J.; Ondo, W. Tremor rating scales and laboratory tools for assessing tremor. J. Neurol. Sci. 2022, 435, 120202. [Google Scholar] [CrossRef]
- Ang, W.T.; Khosla, P.K.; Riviere, C.N. Design of all-accelerometer inertial measurement unit for tremor sensing in hand-held microsurgical instrument. In Proceedings of the 2003 IEEE International Conference on Robotics and Automation (Cat. No.03CH37422), Taipei, China, 14–19 September 2003; Volume 2, pp. 1781–1786. [Google Scholar] [CrossRef] [Green Version]
- Vescio, B.; Quattrone, A.; Nisticò, R.; Crasà, M.; Quattrone, A. Wearable Devices for Assessment of Tremor. Front. Neurol. 2021, 12, 680011. [Google Scholar] [CrossRef]
- Iosa, M.; Picerno, P.; Paolucci, S.; Morone, G. Wearable inertial sensors for human movement analysis. Expert Rev. Med. Devices 2016, 13, 641–659. [Google Scholar] [PubMed]
- Monje, M.H.G.; Foffani, G.; Obeso, J.; Sánchez-Ferro, Á. New sensor and wearable technologies to aid in the diagnosis and treatment monitoring of Parkinson’s disease. Annu. Rev. Biomed. Eng. 2019, 21, 111–143. [Google Scholar] [PubMed]
- Daneault, J.-F.; Carignan, B.; Codère, C.; Sadikot, A.F.; Duval, C. Using a Smart Phone as a Standalone Platform for Detection and Monitoring of Pathological Tremors. Front. Hum. Neurosci. 2013, 6, 357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Premkumar, M.; Ashokkumar, S.; Jeevanantham, V.; Pallavi, S.A.; Mohanbabu, G.; Raaj, R.S. Design of cost-effective real time tremor alerting system for patients of neurodegenerative diseases. Mater. Today Proc. 2021. [Google Scholar] [CrossRef]
- Aviles-Cruz, C.; Rodriguez-Martinez, E.; Cortez, J.V.; Ferreyra-Ramirez, A. Granger-causality: An efficient single user movement recognition using a smartphone accelerometer sensor. Pattern Recognit. Lett. 2019, 125, 576–583. [Google Scholar] [CrossRef]
- Fraiwan, L.; Khnouf, R.; Mashagbeh, A.R. Parkinson’s disease hand tremor detection system for mobile application. J. Med. Eng. Technol. 2016, 40, 127–134. [Google Scholar] [CrossRef]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Mâsse, L.C.; Tilert, T.; Mcdowell, M. Physical Activity in the United States Measured by Accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef]
- Dao, M.-S.; Nguyen-Gia, T.-A.; Mai, V.-C. Daily Human Activities Recognition Using Heterogeneous Sensors from Smartphones. Procedia Comput. Sci. 2017, 111, 323–328. [Google Scholar] [CrossRef]
- Ghosh, A.; Riccardi, G. Recognizing human activities from smartphone sensor signals. In Proceedings of the 22nd ACM International Conference on Multimedia, Orlando, FL, USA, 3–7 November 2014. [Google Scholar]
- Lara, O.D.; Labrador, M.A. A Survey on Human Activity Recognition using Wearable Sensors. IEEE Commun. Surv. Tutor. 2013, 15, 1192–1209. [Google Scholar] [CrossRef]
- Makni, A.; Lefebvre, G. Attitude estimation for posture detection in ehealth services. In Proceedings of the 2018 IEEE 31st International Symposium on Computer-Based Medical Systems (CBMS), Karlstad, Sweden, 18–21 June 2018. [Google Scholar]
- Clifford, M.; Gomez, L. Measuring Tilt with Low-g Accelerometers; Freescale Semiconductor: Austin, TX, USA, 2005. [Google Scholar]
- Puzyrev, V.; Swidinsky, A. Inversion of 1D frequency- and time-domain electromagnetic data with convolutional neural networks. Comput. Geosci. 2020, 149, 104681. [Google Scholar] [CrossRef]
- Wicht, D.; Schneider, M.; Böhlke, T. Anderson-accelerated polarization schemes for fast Fourier transform-based computational homogenization. Int. J. Numer. Methods Eng. 2021, 122, 2287–2311. [Google Scholar]
- Goda, K.; Solli, D.R.; Tsia, K.K.; Jalali, B. Theory of amplified dispersive Fourier transformation. Phys. Rev. A 2009, 80, 043821. [Google Scholar] [CrossRef] [Green Version]
- Dobróka, M.; Szegedi, H.; Vass, P.; Turai, E. Fourier transformation as inverse problem—An improved algorithm. Acta. Geod. Geophys. Hung. 2012, 47, 185–196. [Google Scholar]
- Kichak, V.; Bortnik, G.; Yblonskiy, V. Discrete fourier transformation of the large implementations of signals. In Proceedings of the International Conference Modern Problems of Radio Engineering, Telecommunications and Computer Science, Lviv-Slavsko, Ukraine, 28 February 2004. [Google Scholar]
- Belega, D.; Zaporojan, S. Assessment of influence of systematic errors on the precision with which the normalized frequency of a sinusoidal signal is determined by means of a discrete fourier transformation with interpolation. Meas. Tech. 2009, 52, 148–154. [Google Scholar] [CrossRef]
- Akcay, H.; Turkay, S. Rational Interpolation of Analytic Functions From Real or Imaginary Parts of Frequency-Response Data: A Subspace-Based Approach. IEEE Signal Process. Lett. 2009, 16, 350–353. [Google Scholar] [CrossRef]




| Test | Conditions to Pass |
|---|---|
| Visual |
|
| Input and output voltage |
|
| Output current |
|
| MOSFET |
|
| Functionality |
|
| BLE connection |
|
| Notification |
|
| Data Storage |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Aboosi, A.F.; Fink, R. Novel Device Used to Monitor Hand Tremors during Nocturnal Hypoglycemic Events. Inventions 2022, 7, 32. https://doi.org/10.3390/inventions7020032
Al-Aboosi AF, Fink R. Novel Device Used to Monitor Hand Tremors during Nocturnal Hypoglycemic Events. Inventions. 2022; 7(2):32. https://doi.org/10.3390/inventions7020032
Chicago/Turabian StyleAl-Aboosi, Abdullah F., and Rainer Fink. 2022. "Novel Device Used to Monitor Hand Tremors during Nocturnal Hypoglycemic Events" Inventions 7, no. 2: 32. https://doi.org/10.3390/inventions7020032
APA StyleAl-Aboosi, A. F., & Fink, R. (2022). Novel Device Used to Monitor Hand Tremors during Nocturnal Hypoglycemic Events. Inventions, 7(2), 32. https://doi.org/10.3390/inventions7020032






