Remote Monitoring of Patient Respiration with Mask Attachment—A Pragmatic Solution for Medical Facilities
Abstract
1. Introduction
2. Materials and Methods
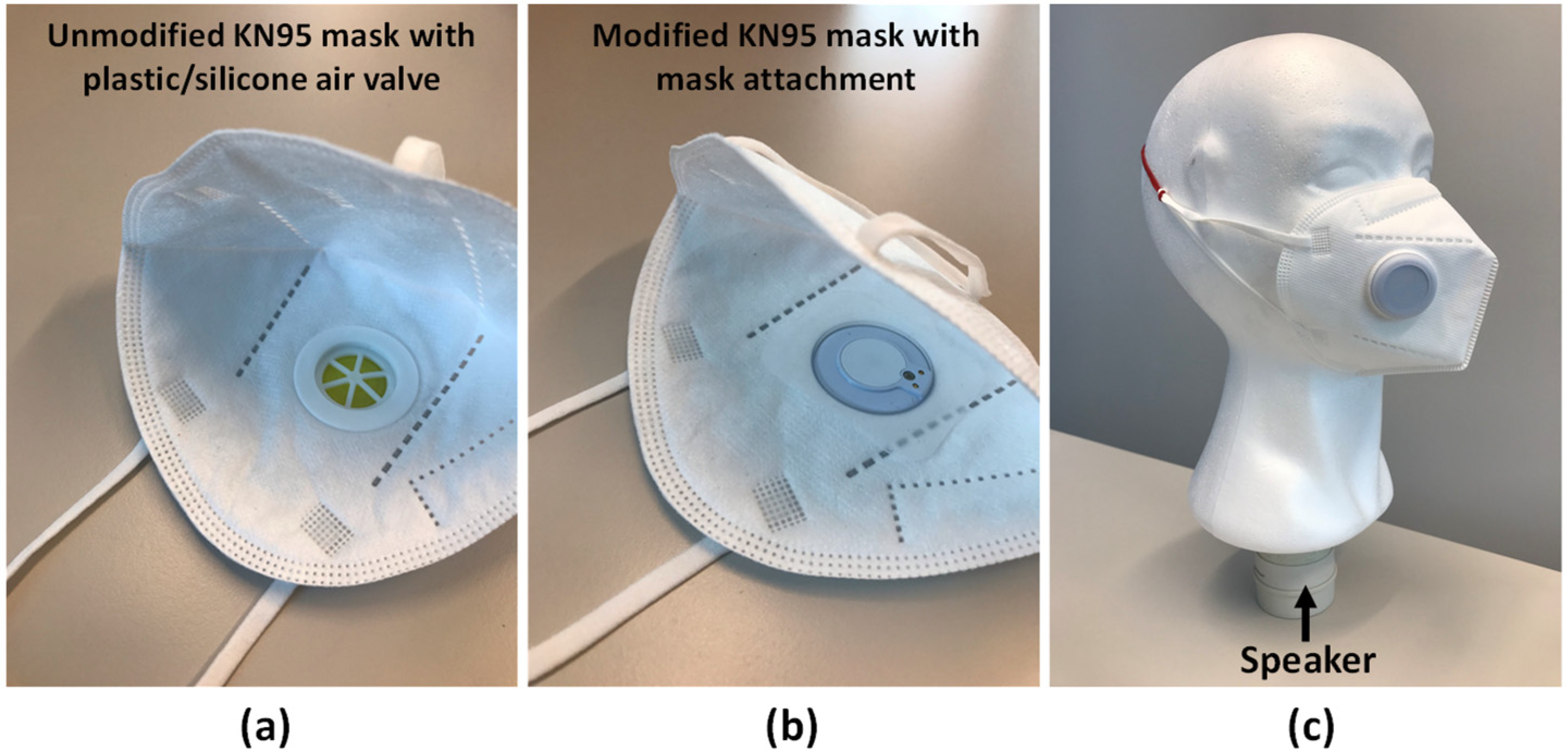
2.1. Sensing Device
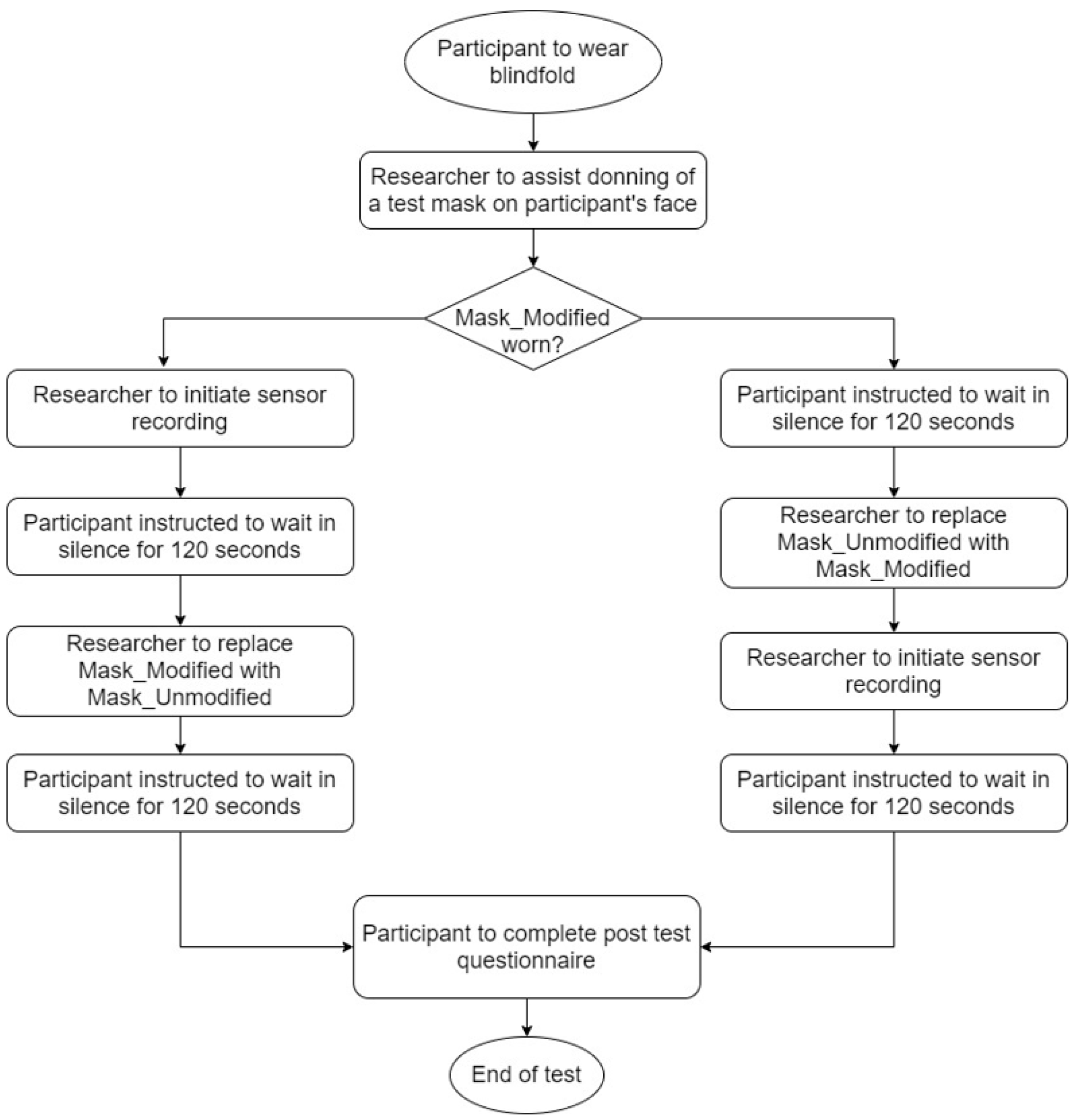
2.2. Experimental Setup
2.3. Human Factor Considerations
2.4. Use Environment
2.5. User
2.6. Use Interface
2.7. Participants
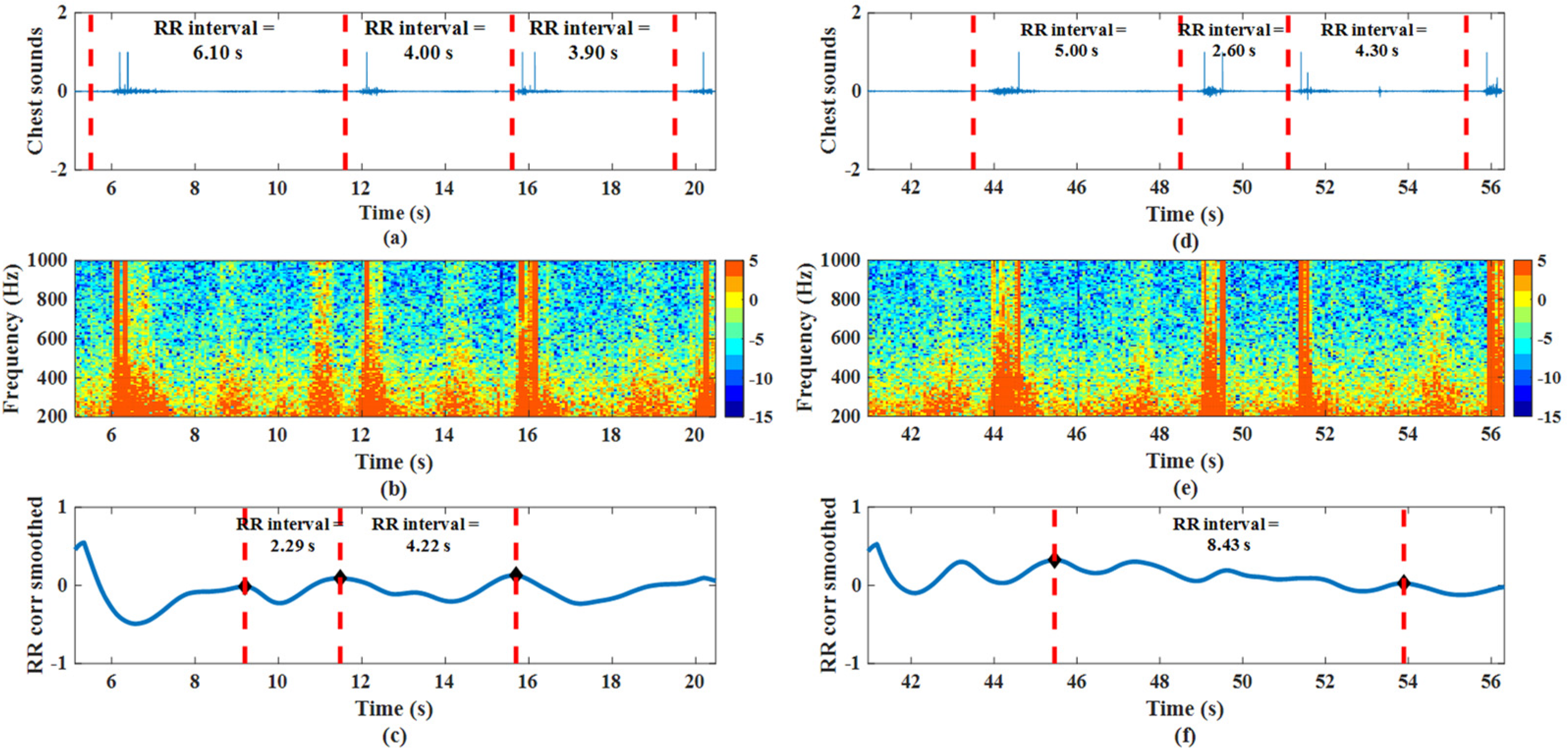
2.8. Respiratory Rate Estimation and Wheeze Detection Algorithms
2.9. Validation of Respiratory Rate Estimation and Wheeze Detection Algorithms
3. Results and Discussion
3.1. Usability
3.2. Respiratory Rate Estimation
3.3. Wheeze Detection
4. Conclusions
5. Patent
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Portnoy, J.; Waller, M.; Elliott, T. Telemedicine in the era of COVID-19. J. Allergy Clin. Immunol. Pract. 2020, 8, 1489–1491. [Google Scholar] [CrossRef]
- Mann, D.M.; Chen, J.; Chunara, R.; Testa, P.A.; Nov, O. COVID-19 transforms health care through telemedicine: Evidence from the field. J. Am. Med. Inform. Assoc. 2020, 27, 1132–1135. [Google Scholar] [CrossRef]
- Levine, D.M.; Ouchi, K.; Blanchfield, B.; Diamond, K.; Licurse, A.; Pu, C.T.; Schnipper, J.L. Hospital-level care at home for acutely ill adults: A randomized controlled trial. Ann. Intern. Med. 2020, 172, 77–85. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Advice on the Use of Masks in the Context of COVID-19: Interim Guidance, 6 April 2020; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Verma, S.; Dhanak, M.; Frankenfield, J. Visualizing the effectiveness of face masks in obstructing respiratory jets. Phys. Fluids 2020, 32, 61708. [Google Scholar] [CrossRef]
- Chughtai, A.A.; Seale, H.; Macintyre, C.R. Effectiveness of cloth masks for protection against severe acute respiratory syndrome coronavirus 2. Emerg. Infect. Dis. 2020, 26, e200948. [Google Scholar] [CrossRef] [PubMed]
- Eikenberry, S.E.; Mancuso, M.; Iboi, E.; Phan, T.; Eikenberry, K.; Kuang, Y.; Kostelich, E.; Gumel, A.B. To mask or not to mask: Modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect. Dis. Model. 2020, 5, 293–308. [Google Scholar] [CrossRef]
- Wang, J.; Pan, L.; Tang, S.; Ji, J.S.; Shi, X. Mask use during COVID-19: A risk adjusted strategy. Environ. Pollut. 2020, 266, 115099. [Google Scholar] [CrossRef] [PubMed]
- Cheng, V.C.-C.; Wong, S.-C.; Chuang, V.W.-M.; So, S.Y.C.; Chen, J.H.K.; Sridhar, S.; To, K.K.W.; Chan, J.F.W.; Hung, I.F.N.; Ho, P.L.; et al. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J. Infect. 2020, 81, 107–114. [Google Scholar] [CrossRef]
- Duc, H.T.L. The COVID-19 containment in Vietnam: What are we doing? J. Glob. Health 2020, 10, 010338. [Google Scholar]
- Chiang, C.-H.; Chiang, C.-H.; Chiang, C.-H. Maintaining mask stockpiles in the COVID-19 pandemic: Taiwan as a learning model. Infect. Control. Hosp. Epidemiol. 2021, 42, 244–245. [Google Scholar] [CrossRef]
- Pan, L.; Wang, C.; Jin, H.; Li, J.; Yang, L.; Zheng, Y.; Wen, Y.; Tan, B.H.; Loh, X.J.; Chen, X. Lab-on-Mask for Remote Respiratory Monitoring. ACS Mater. Lett. 2020, 2, 1178–1181. [Google Scholar] [CrossRef]
- Koh, V.C.A.; Tan, R.X.; Ang, Y.Y. A Miniature Wearable Microphone Sensor for Cardiopulmonary Monitoring. In Proceedings of the 2020 IEEE Sensors, Rotterdam, The Netherlands, 25–28 October 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 1–4. [Google Scholar]
- Pereira, C.B.; Yu, X.; Czaplik, M.; Rossaint, R.; Blazek, V.; Leonhardt, S. Remote monitoring of breathing dynamics using infrared thermography. Biomed. Opt. Express 2015, 6, 4378–4394. [Google Scholar] [CrossRef] [PubMed]
- Jakkaew, P.; Onoye, T. Non-contact respiration monitoring and body movements detection for sleep using thermal imaging. Sensors 2020, 20, 6307. [Google Scholar] [CrossRef] [PubMed]
- Ser, W.; Zhang, J.; Yu, J.; Zhang, T. Air Conduction Sensor and a System and a Method for Monitoring a Health Condition. U.S. Patent 9,826,955, 28 November 2017. [Google Scholar]
- Ibrahim, A.; Koh, V.C.A.; Hamidah, S.; Ang, Y.Y.; Tan, R.X.; Ser, W. System and Method for Monitoring a Pluraity of Bio-Signals, and a Gateway Device Operable Therein. 17 May 2021. [Google Scholar]
- Center for Devices & Radiological Health. Human Factors and Usability Engineering to Medical Devices. 2019. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/applying-human-factors-and-usability-engineering-medical-devices (accessed on 1 September 2020).
- Scheid, J.L.; Lupien, S.P.; Ford, G.S.; West, S.L. Commentary: Physiological and psychological impact of face mask usage during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 6655. [Google Scholar] [CrossRef] [PubMed]
- Rocha, B.M.; Filos, D.; Mendes, L.; Serbes, G.; Ulukaya, S.; Kahya, Y.P.; Jakovljevic, N.; Turukalo, T.L.; Vogiatzis, I.M.; Perantoni, E.; et al. An open access database for the evaluation of respiratory sound classification algorithms. Physiol. Meas. 2019, 40, 35001. [Google Scholar] [CrossRef] [PubMed]
- Chan, P.; Wong, G.; Nguyen, T.D.; Hopper, I. Estimation of respiratory rate using infrared video in an inpatient population: An observational study. J. Clin. Monit. Comput. 2020, 34, 1275–1284. [Google Scholar] [CrossRef]
- Jarchi, D.; Rodgers, S.J.; Tarassenko, L.; Clifton, D.A. Accelerometry-Based Estimation of Respiratory Rate for Post-Intensive Care Patient Monitoring. IEEE Sens. J. 2018, 18, 4981–4989. [Google Scholar] [CrossRef]
- L’Her, E.; Nazir, S.; Pateau, V.; Visvikis, D. Accuracy of noncontact surface imaging for tidal volume and respiratory rate measurements in the ICU. J. Clin. Monit. Comput. 2021, 1–9. [Google Scholar] [CrossRef]
- McGinley, A.; Pearse, R.M. A national early warning score for acutely ill patients. BMJ 2012, 345, e5310. [Google Scholar] [CrossRef]
- Muller, J.L.; Hohlfeld, R.G. System for Measuring the Period of a Quasi-Periodic Signal. U.S. Patent 5,584,295, 7 December 1996. [Google Scholar]
- Subbe, C.P.; Kinsella, S. Continuous monitoring of respiratory rate in emergency admissions: Evaluation of the RespiraSenseTM sensor in acute care compared to the industry standard and gold standard. Sensors 2018, 18, 2700. [Google Scholar] [CrossRef]
- Philip, K.E.J.; Pack, E.; Cambiano, V.; Rollmann, H.; Weil, S.; O’Beirne, J. The accuracy of respiratory rate assessment by doctors in a London teaching hospital: A cross-sectional study. J. Clin. Monit. Comput. 2015, 29, 455–460. [Google Scholar] [CrossRef]
- Erden, F.; Alkar, A.Z.; Cetin, A.E. Contact-free measurement of respiratory rate using infrared and vibration sensors. Infrared Phys. Technol. 2015, 73, 88–94. [Google Scholar] [CrossRef]
- Trimpop, J.; Schenk, H.; Bieber, G.; Lämmel, F.; Burggraf, P. Smartwatch based respiratory rate and breathing pattern recognition in an end-consumer environment. In Proceedings of the 4th international Workshop on Sensor-based Activity Recognition and Interaction, Rostock, Germany, 21–22 September 2017; pp. 1–5. [Google Scholar]
- Laurie, J.; Higgins, N.; Peynot, T.; Fawcett, L.; Roberts, J. An evaluation of a video magnification-based system for respiratory rate monitoring in an acute mental health setting. Int. J. Med. Inform. 2021, 148, 104378. [Google Scholar] [CrossRef]
- Brown, C.; Morse, J.; Nesvadba, D.; Meldrum, A. Twelve tips for introducing simulation based assessment in the objective structured clinical examination. Med. Teach. 2020, 43, 380–383. [Google Scholar] [CrossRef]
- Pawlowski, J.; Feinstein, D.; Crandall, M.L.; Gala, S. Modernizing Biomedical Training: Replacing Live Animal Laboratories with Human Simulation. Anim. Exp. Work. Towards A Paradig. Chang. 2019, 551–566. [Google Scholar] [CrossRef]
- Armitage, M.; Eddleston, J.; Stokes, T. Recognising and responding to acute illness in adults in hospital: Summary of NICE guidance. BMJ 2007, 335, 258–259. [Google Scholar] [CrossRef][Green Version]
| Attributes | Population n = 16 |
|---|---|
| Age (average) | 24.5 ± 4.0 |
| Gender | |
| Male | 5 |
| Female | 11 |
| Mask Size * | |
| S (<100 mm) | 1 |
| M (100–110 mm) | 11 |
| L (110–125 mm) | 4 |
| Pre-existing chronic respiratory conditions | 1 |
| Participant | Respiratory Rate (brpm) | Mean Absolute Error (brpm) | |
|---|---|---|---|
| Manual Count | Mask Attachment | ||
| 1 | 17.2 | 16.2 | 1.0 |
| 2 | 18.9 | 22.0 | 3.1 |
| 3 | NA | NA | NA |
| 4 | 17.2 | 17.8 | 0.6 |
| 5 | 12.5 | 16.5 | 4.0 |
| 6 | 18.8 | 16.2 | 2.6 |
| 7 | 13.9 | 17.6 | 3.7 |
| 8 | 21.2 | 20.8 | 0.4 |
| 9 | 23.1 | 19.8 | 3.3 |
| 10 | 13.6 | 15.6 | 2.0 |
| 11 | 20.0 | 19.0 | 1.0 |
| 12 | 18.1 | 18.6 | 0.5 |
| 13 | 18.9 | 15.8 | 3.1 |
| 14 | 21.7 | 20.8 | 0.9 |
| 15 | 20.0 | 20.7 | 0.7 |
| 16 | 19.8 | 23.0 | 3.2 |
| Average error | 2.0 ± 1.3 | ||
| Actual Breath Classification | Classification by Wheeze Detection Algorithm | ||
|---|---|---|---|
| Wheeze | Normal Breath | ||
| Wheeze | 469 | 59 | Sensitivity: 88.8% |
| Normal breath | 27 | 501 | Specificity: 94.9% |
| Positive predictive value: 94.6% | Negative predictive value: 89.5% | Accuracy: 91.9% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koh, V.C.A.; Ang, Y.Y.; Ser, W.; Tan, R.X. Remote Monitoring of Patient Respiration with Mask Attachment—A Pragmatic Solution for Medical Facilities. Inventions 2021, 6, 81. https://doi.org/10.3390/inventions6040081
Koh VCA, Ang YY, Ser W, Tan RX. Remote Monitoring of Patient Respiration with Mask Attachment—A Pragmatic Solution for Medical Facilities. Inventions. 2021; 6(4):81. https://doi.org/10.3390/inventions6040081
Chicago/Turabian StyleKoh, Vivian Ci Ai, Yi Yang Ang, Wee Ser, and Rex Xiao Tan. 2021. "Remote Monitoring of Patient Respiration with Mask Attachment—A Pragmatic Solution for Medical Facilities" Inventions 6, no. 4: 81. https://doi.org/10.3390/inventions6040081
APA StyleKoh, V. C. A., Ang, Y. Y., Ser, W., & Tan, R. X. (2021). Remote Monitoring of Patient Respiration with Mask Attachment—A Pragmatic Solution for Medical Facilities. Inventions, 6(4), 81. https://doi.org/10.3390/inventions6040081







