Description of and Relationships among Potential Variables Supported for the Diagnosis of Delayed Ejaculation
Abstract
1. Introduction
1.1. Criteria Proposed the Diagnosis of Delayed Ejaculation
1.2. Rationale and Goals
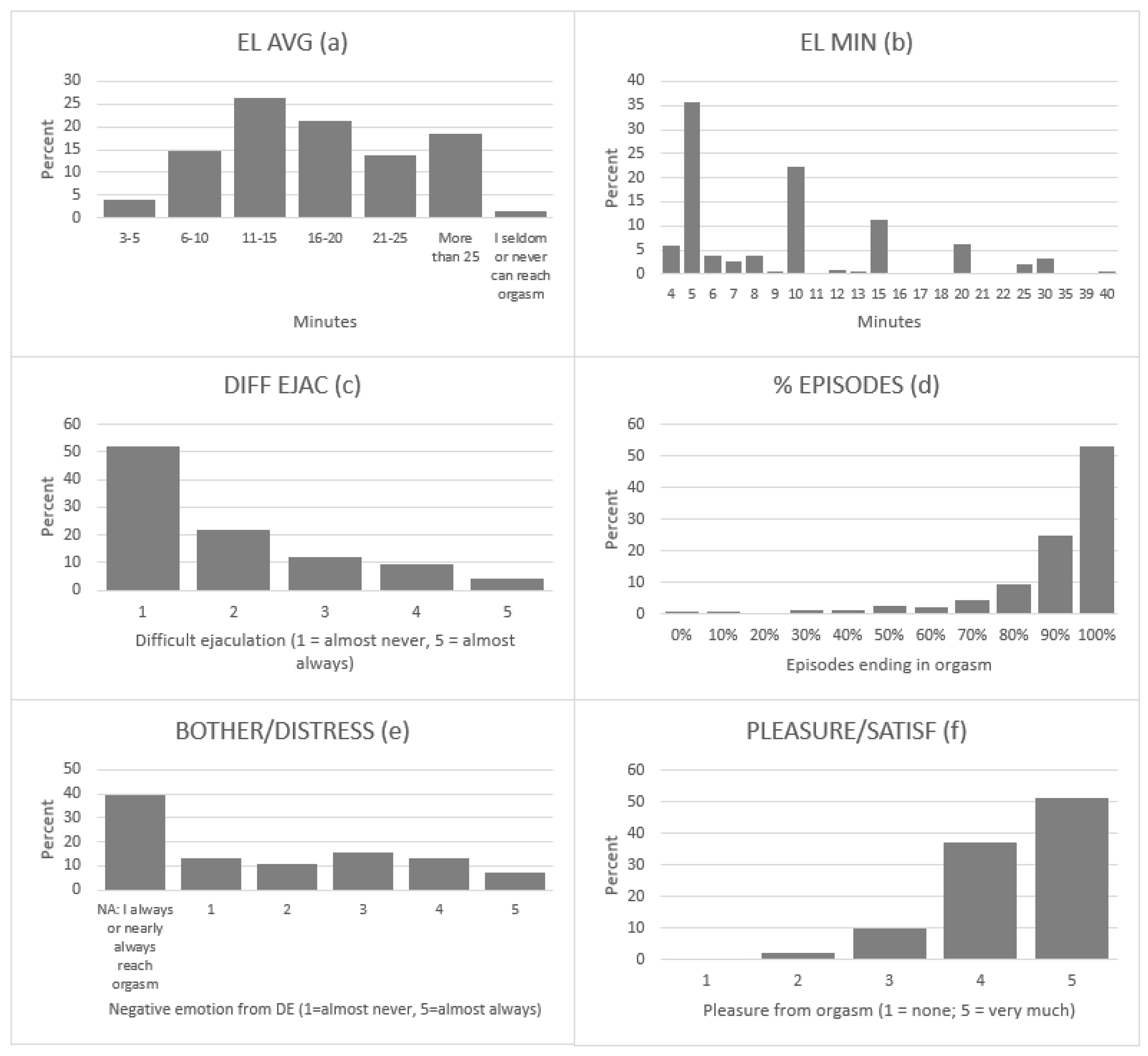
- Generated frequency histograms for each of the six variables to better understand their distribution in men free of comorbid PE and ED (Aim 1);
- Explored the interrelatedness of these variables (Aim 2);
- Evaluated the capacity for each of the six variables to contribute to the diagnosis of DE, with the goal of selecting the three best variables to represent each of the three constructs proposed as diagnostic criteria (Aim 3);
- Determined the unique variance contribution of each of three final variables/items selected as candidates for the diagnosis of DE (Aim 4).
2. Materials and Methods
2.1. Participants
2.2. Survey Questionnaire
2.3. Selection of Face-Valid Variables Related to the Constructs for Diagnosing DE
2.3.1. The Construct of Ejaculation Timing/Latency
2.3.2. The Construct of Self-Efficacy/Control Regarding the Timing of Ejaculation
2.3.3. The Construct of Negative Consequences of DE
2.4. Control Covariates
2.4.1. Assessment of Erectile Function
2.4.2. Assessment of Premature Ejaculation
2.5. Procedure
2.6. Analytical Strategy
3. Results
3.1. Description of the Sample and Distribution of Proposed Diagnostic Variables (Aim 1)
3.2. Relationship among Diagnostic Variables (Aim 2)
3.3. Variable Selection for Commonality Analysis (Aim 3)
3.4. Determining Unique and Common Variances Contributing to a DE Diagnosis (Aim 4)
4. Discussion
4.1. Description and Distribution Characteristics of Proposed Diagnostic Variables
4.2. Interrelatedness of Proposed Diagnostic Variables
4.3. Selecting the Best Variables for Diagnosing DE and the Unique Contribution of Each
4.4. Constructing a Diagnostic Procedure for Assessing DE
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Variable Name. | Description in Survey Questionnaire | Response Categories |
|---|---|---|
| Typical Ejaculatory Latency (“EL AVG”) | If you have partnered sex, about how long does it take for you, on average, to reach orgasm, from the time that you begin penile stimulation (i.e., when you initially start trying to move toward orgasm/ejaculation)? | 1 = Less than 1 min 2 = 1–2 min 3 = 3–5 min 4 = 6–10 min 5 = 11–15 min 6 = 16–20 min 7 = 21–25 min 8 = More than 25 min 9 = I have partnered sex but can seldom reach orgasm 10 = I have partnered sex but choose not to ejaculate |
| Shortest Ejaculatory Latency (“EL MIN”) | If you reach orgasm during partnered sex, estimate the typical shortest time in minutes for ejaculation, from the time you begin penile stimulation that moves you toward orgasm. | Self-reported minutes |
| Difficulty Reaching Ejaculation/Orgasm (“DIFF EJAC”) | During sex with your partner, do you ever have difficulty reaching ejaculation/orgasm? | 0 = I chose not to ejaculate due to personal preferences/beliefs 1 = almost never 5 = almost always |
| Frequency of Partnered Sex Ending in Orgasm (“% EPISODES”) | Estimate how often sex with a partner typically ends in (or ended in) orgasm for you. If you have not had any sexual activities with your partner, or if you choose not to reach orgasm, select NA (not applicable). | 0 = 0% 1 = 10% 2 = 20% 3 = 30% 4 = 40% 5 = 50% 6 = 60% 7 = 70% 8 = 80% 9 = 90% 10 = 100% |
| Sexual Dysfunction related (“BOTHER/DISTRESS”) | When you have (or have had) sex with your partner, if you have any difficulties with sex, such as finding it very difficult to reach orgasm, does (or did) this bother, upset, or frustrate you, or make you feel guilty? | 0 = N/A: I nearly always reach orgasm with my partner, so this is not a problem 1 = Almost never 5 = Almost always |
| Orgasmic Pleasure (“PLEASURE/SATISF”) | When you have (or have had) sex with a partner, how pleasurable or satisfying would you rate your typical orgasm? | 0 = N/A: I generally choose not to ejaculate during partnered sex 1 = Not satisfying 5 = Very satisfying |
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- ICD-11 for Mortality and Morbidity Statistics. Available online: https://icd.who.int/browse11/ (accessed on 8 November 2022).
- Perelman, M.A.; Rowland, D.L. Retarded and inhibited ejaculation. In Handbook of Sexual and Gender Identity Disorders; Rowland, D.L., Incrocci, L., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2008; pp. 100–121. [Google Scholar]
- Lewis, R.W.; Fugl-Meyer, K.S.; Corona, G.; Hayes, R.D.; Laumann, E.O.; Moreira, E.D., Jr.; Rellini, A.H.; Segraves, T. Definitions/epidemiology/risk factors for sexual dysfunction. J. Sex. Med. 2010, 7, 1598–1607. [Google Scholar] [CrossRef] [PubMed]
- Rowland, D.L.; Cote-Leger, P. Moving toward empirically based standardization in the diagnosis of delayed ejaculation. J. Sex. Med. 2020, 17, 1896–1902. [Google Scholar] [CrossRef] [PubMed]
- Laumann, E.O.; Paik, A.; Rosen, R.C. Sexual dysfunction in the United States: Prevalence and predictors. JAMA 1999, 281, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Perelman, M.A. Reexamining the definitions of PE and DE. J. Sex. Marital Ther. 2017, 43, 633–644. [Google Scholar] [CrossRef] [PubMed]
- Rowland, D.L.; Oosterhouse, L.B.; Kneusel, J.A.; Hevesi, K. Comorbidities among sexual problems in men: Results from an internet convenience sample. Sex. Med. 2021, 9, 100–416. [Google Scholar] [CrossRef]
- Shindel, A.W.; Althof, S.E.; Carrier, S.; Chou, R.; McMahon, C.G.; Mulhall, J.P.; Paduch, D.A.; Pastuszak, A.W.; Rowland, D.; Tapscott, A.H.; et al. Disorders of ejaculation: An AUA/SMSNA guideline. J. Urol. 2022, 207, 504–512. [Google Scholar] [CrossRef] [PubMed]
- Serefoglu, E.C.; McMahon, C.G.; Waldinger, M.D.; Althof, S.E.; Shindel, A.; Adaikan, G.; Becher, E.F.; Dean, J.; Giuliano, F.; Hellstrom, W.J.; et al. An evidence-based unified definition of lifelong and acquired premature ejaculation: Report of the second international society for sexual medicine ad hoc committee for the definition of premature ejaculation. Sex. Med. 2014, 2, 41–59. [Google Scholar] [CrossRef]
- Rowland, D.L. A conceptual approach to understanding and managing men’s orgasmic difficulties. Urol. Clin. N. Am. 2021, 48, 577–590. [Google Scholar] [CrossRef]
- Rowland, D.L.; Attinger, D.; Morrow, A.; Motofei, I.; Hevesi, K. Characteristics of men who report symptoms of delayed ejaculation: Providing support for empirically-derived diagnostic criteria. J. Sex. Med. 2022; in press. [Google Scholar]
- Rowland, D.L.; Althof, S.E.; McMahon, C.G. The unfinished business of defining premature ejaculation: The need for targeted research. Sex. Med. Rev. 2022, 10, 323–340. [Google Scholar] [CrossRef]
- Catania, J.A.; Dolcini, M.M.; Orellana, R.; Narayanan, V. Non-probability and probability-based sampling strategies in sexual science. J. Sex. Res. 2015, 52, 396–411. [Google Scholar] [CrossRef] [PubMed]
- Rosen, R.C.; Cappelleri, J.C.; Smith, D.; Lipsky, J.; Peña, B.M. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int. J. Impot. Res. 1999, 11, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Symonds, T.; Perelman, M.A.; Althof, S.; Giuliano, F.; Martin, M.; May, K.; Abraham, L.; Crossland, A.; Morris, M. Development and validation of a premature ejaculation diagnostic tool. Eur. Urol. 2007, 52, 565–573. [Google Scholar] [CrossRef]
- Patrick, D.A.; Rowland, D.L.; Rothman, M. Interrelationship among measures of premature ejaculation: The central role of perceived control over ejaculation. J. Sex. Med. 2007, 4, 780–788. [Google Scholar] [CrossRef]
- Shabsigh, R.; Patrick, D.L.; Rowland, D.L.; Bull, S.A.; Tesfaye, F.; Rothman, M. Perceived control over ejaculation is central to treatment benefit in men with premature ejaculation: Results from phase III trials with dapoxetine. BJU Int. 2008, 102, 824–828. [Google Scholar] [CrossRef] [PubMed]
- Hoerger, M. Participant dropout as a function of survey length in internet-mediated university studies: Implications for study design and voluntary participation in psychological research. Cyberpsychol. Behav. Soc. Netw. 2010, 13, 697–700. [Google Scholar] [CrossRef]
- Ross, M.W.; Daneback, K.; Mansson, S.A.; Tikkanen, R.; Cooper, A. Characteristics of men and women who complete or exit from an on-line internet sexuality questionnaire: A study of instrument dropout biases. J. Sex. Res. 2003, 40, 396–402. [Google Scholar] [CrossRef]
- How to Estimate the Length of a Survey. Available online: https://verstaresearch.com/newsletters/how-to-estimate-the-length-of-a-survey/ (accessed on 6 November 2022).
- Does Adding One More Question Impact Survey Completion? Available online: https://www.surveymonkey.com/curiosity/survey_questions_and_completion_rates/ (accessed on 6 November 2022).
- Kays, K.; Keith, T.; Broughal, M. Best practice in online survey research with sensitive topics. In Advancing Research Methods with New Technologies; Sappleton, N., Ed.; IGI Global: Hershey, PA, USA, 2013; pp. 157–168. [Google Scholar]
- Reichwein Zientek, L.; Thompson, B. Commonality analysis: Partitioning variance to facilitate better understanding of data. J. Early Interv. 2006, 28, 299–307. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing. MSOR Connect. 2020. Available online: https://www.eea.europa.eu/data-and-maps/indicators/oxygen-consuming-substances-in-rivers/r-development-core-team-2006 (accessed on 1 December 2022).
- R Development Core Team. R: A Language and Environment for Statistical Computing [Computer Software]; R Foundation for Statistical Computing: Vienna, Austria, 2022; Available online: https://www.r-project.org/ (accessed on 1 December 2022).
- Waldinger, M.D.; Quinn, P.; Dillenn, M.; Mundayat, R.; Schweitzer, D.H.; Boolell, M. A multinational population survey of intravaginal ejaculation latency time. J. Sex. Med. 2005, 2, 492–497. [Google Scholar] [CrossRef]
- Nimon, K.F.; Oswald, F.L. Understanding the results of multiple linear regression: Beyond standardized regression coefficients. Organ. Res. Methods 2013, 16, 650–674. [Google Scholar] [CrossRef]
- Nimon, K.; Oswald, F.; Oswald, F.L. Package “Yhat”: Interpreting Regression Effects [Computer Software]. 2022. Available online: https://cran.r-project.org/web/packages/yhat/yhat.pdf (accessed on 1 December 2022).
- Patrick, D.L.; Althof, S.E.; Pryor, J.L.; Rosen, R.; Rowland, D.L.; Ho, K.F.; McNulty, P.; Rothman, M.; Jamieson, C. Premature ejaculation: An observational study of men and their partners. J. Sex. Med. 2005, 2, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Rowland, D.L.; Hamilton, B.D.; Bacys, K.R.; Hevesi, K. Sexual response differs during partnered sex and masturbation in men with and without sexual dysfunction: Implications for treatment. J. Sex. Med. 2021, 18, 1835–1842. [Google Scholar] [CrossRef] [PubMed]
- Rowland, D.L.; Teague, L.G.; Hevesir, K. Premature ejaculation measures during partnered sex and masturbation: What these findings tell us about the nature and rigidity of premature ejaculation. J. Sex. Marital Ther. 2022, 48, 680–693. [Google Scholar] [CrossRef] [PubMed]
- Strauss, M.E.; Smith, G.T. Construct validity: Advances in theory and methodology. Annu. Rev. Clin. Psychol. 2009, 5, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Jern, P.; Gunst, A.; Sandqvist, F.; Sandnabba, N.K.; Santtila, P. Using ecological momentary assessment to investigate associations between ejaculatory latency and control in partnered and non-partnered sexual activities. J. Sex. Res. 2011, 48, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Zhang, X.; Su, P.; Shi, K.; Tang, D.; Hao, Z.; Zhou, J.; Liang, C. Prevalence and impact of premature ejaculation in outpatients complaining of ejaculating prematurely: Using the instruments of intravaginal ejaculatory latency time and patient-reported outcome measures. Int. J. Impot. Res. 2014, 26, 94–99. [Google Scholar] [CrossRef]
- Rowland, D.L.; Strassberg, D.S.; de Gouveia Brazao, C.A.; Slob, A.K. Ejaculatory latency and control in men with premature ejaculation: An analysis across sexual activities using multiple sources of information. J. Psychosom. Res. 2000, 48, 69–77. [Google Scholar] [CrossRef]
- Cote-Leger, P.; Rowland, D.L. Diagnostic criteria for premature ejaculation: Clarifying the role of “ejaculatory control” and “bother/distress”. Sexes 2020, 1, 72–86. [Google Scholar] [CrossRef]
- McMahon, C.G.; Althof, S.E.; Waldinger, M.D.; Porst, H.; Dean, J.; Sharlip, I.; Adaikan, P.G.; Becher, E.; Broderick, G.A.; Buvat, J.; et al. An evidence-based definition of lifelong premature ejaculation: Report of the International Society for Sexual Medicine (ISSM) ad hoc committee for the definition of premature ejaculation. J. Sex. Med. 2008, 5, 1590–1606. [Google Scholar]
- Rosen, R.C.; McMahon, C.G.; Niederberger, C.; Broderick, G.A.; Jamieson, C.; Gagnon, D.D. Correlates to the clinical diagnosis of premature ejaculation: Results from a large observational study of men and their partners. J. Urol. 2007, 177, 1059–1064; discussion 1064. [Google Scholar] [CrossRef]
- Rowland, D.L.; McNabney, S.M.; Hevesi, K. Does bother/distress contribute to the diagnosis of premature ejaculation? Sex. Med. 2022, 10, 100548. [Google Scholar] [CrossRef]
- Côté-Léger, P.; Rowland, D.L. Estimations of typical, ideal, premature ejaculation, and actual latencies by men and female sexual partners of men during partnered sex. J. Sex. Med. 2020, 17, 1448–1456. [Google Scholar] [CrossRef] [PubMed]
- Cote-Leger, P.; Rowland, D.L. Global perspectives on the three criteria for premature ejaculation: An observational study of ejaculatory latency, ejaculatory control and bother/distress. Andrologia 2020, 52, e13796. [Google Scholar] [CrossRef] [PubMed]
- Pryor, J.L.; Broderick, G.A.; Ho, K.F.; Jamieson, C.; Gagnon, D. Comparison of estimated vs. measured intravaginal ejaculation latency time (IELT) in men with and without premature ejaculation (PE). J. Sex. Med. 2005, 3, 126. [Google Scholar]
- Lee, W.K.; Cho, S.T.; Lee, Y.S.; Lee, Y.G.; Oh, C.Y.; Yoo, C.; Cho, J.S.; Shin, T.Y.; Lee, S.K.; Lee, S.H.; et al. Can estimated intravaginal ejaculatory latency time be used interchangeably with stopwatch-measured intravaginal ejaculatory latency time for the diagnosis of lifelong premature ejaculation? Urology 2015, 85, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Tang, D.; Xu, C.; Gao, P.; Hao, Z.; Zhou, J.; Liang, C. The relationship between self-estimated intravaginal ejaculatory latency time and International Prostate Symptom Score in middle-aged men complaining of ejaculating prematurely in China. J. Sex. Med. 2015, 12, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Bhat, G.S.; Shastry, A. Use of a stopwatch to measure ejaculatory latency may not be accurate among Indian patients. Indian J Urol. 2017, 33, 300–303. [Google Scholar] [CrossRef] [PubMed]
| Variable Name | Mean (SD) or Frequency (%) |
|---|---|
| Participant Age | 37.77 (12.65) |
| Level of Education 1 | 3 (IQR: 1–4) |
| Medical Issues (% Yes) | 227 (17.7%) |
| Anxiety/Depression (% Yes) | 247 (19.2%) |
| Interest in Sex (1–5, high) | 4.23 (0.8) |
| Frequency of Partnered Sex (1–10, high) | 6.36 (1.64) |
| Frequency of Masturbation (1–11, high) | 5.65 (2.25) |
| Relationship Satisfaction (1–5, high) | 4.0 (0.97) |
| Sexual Satisfaction (1–5, high) | 3.05 (1.72) |
| Sexual Orientation (% Straight) | 1108 (86.23%) |
| (% Bisexual) | 22 (1.71%) |
| (% Gay) | 155 (12.06%) |
| Variable 1 | Construct | Effect Size 2 | Mean (SD) | Median (IQR) | Min/Max | Kurtosis | Skew |
|---|---|---|---|---|---|---|---|
| EL AVG | Ejaculatory timing | 0.081 | 5.88 (1.5) | 6 (5–7) | 3–9 | −0.9 | 0.1 |
| EL MIN | Ejaculatory timing | 0.071 | 10.01 (6.7) | 8 (5–12) | 4–40 | 2.9 | 1.7 |
| DIFF EJAC | Efficacy/control | NA 3 | 1.92 (1.2) | 1 (1–3) | 1–5 | 0.1 | 1.1 |
| % EPISODES | Efficacy/control | 0.201 | 89.4 (10.7) | 100 (90–100) | 10–100 | 7.2 | −2.5 |
| BOTHER/DISTRESS | Negative effects DE | 0.114 | 2.74 (1.7) | 2 (1–4) | 1–5 | −1.2 | 0.5 |
| PLEASURE/SATISF | Negative effects DE | 0.071 | 4.37 (0.8) | 5 (4–5) | 1–5 | 1.1 | 1.1 |
| Variable | EL AVG | EL MIN | DIFF EJAC | % EPISODES | BOTHER/ DISTRESS |
|---|---|---|---|---|---|
| EL AVG | X | ||||
| EL MIN | 0.583 **/0.689 ** | X | |||
| DIFF EJAC | 0.197 **/0.101 ** | 0.202 **/0.081 ** | X | ||
| % EPISODES | −0.157 **/−0.104 ** | −0.163 **/−0.06 * | −0.459 **/−0.332 ** | X | |
| BOTHER/DISTRESS | 0.067 */0.054 * | 0.091 **/0.034 | 0.439 **/0.382 ** | −0.34 **/−0.266 ** | X |
| PLEASURE/SATISF | −0.039/0.01 | −0.106 **/0.028 | −0.294 **/−0.237 ** | 0.292 **/0.204 ** | −0.21 **/−0.184 ** |
| Sources of Variation in DIFF EJAC | Commonality Coefficient | Model Contribution (%) |
|---|---|---|
| EL MIN | 0.037 | 17.67% |
| BOTHER/DISTRESS | 0.154 | 73.57% |
| Common/Shared Variance | 0.018 | 8.76% |
| Multiple R2 = 0.209 | ||
| Sources of Variation in EL MIN | Commonality Coefficient | Model Contribution (%) |
| DIFF EJAC | 0.0443 | 79.81% |
| BOTHER/DISTRESS | 0.0001 | 0.14% |
| Common/Shared Variance | 0.0111 | 20.05% |
| Multiple R2 = 0.0555 | ||
| Sources of Variation in BOTHER/ DISTRESS | Commonality Coefficient | Model Contribution (%) |
| DIFF EJAC | 0.1616 | 93.51% |
| EL MIN | 0.0001 | 0.04% |
| Common/Shared Variance | 0.0111 | 6.45% |
| Multiple R2 = 0.1728 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rowland, D.L.; McNabney, S.M.; Teague, L.G.; Padilla, S.M.; Bacys, K.R.; Hevesi, K. Description of and Relationships among Potential Variables Supported for the Diagnosis of Delayed Ejaculation. Sexes 2023, 4, 40-54. https://doi.org/10.3390/sexes4010005
Rowland DL, McNabney SM, Teague LG, Padilla SM, Bacys KR, Hevesi K. Description of and Relationships among Potential Variables Supported for the Diagnosis of Delayed Ejaculation. Sexes. 2023; 4(1):40-54. https://doi.org/10.3390/sexes4010005
Chicago/Turabian StyleRowland, David L., Sean M. McNabney, Lijana G. Teague, Sarah M. Padilla, Katelyn R. Bacys, and Krisztina Hevesi. 2023. "Description of and Relationships among Potential Variables Supported for the Diagnosis of Delayed Ejaculation" Sexes 4, no. 1: 40-54. https://doi.org/10.3390/sexes4010005
APA StyleRowland, D. L., McNabney, S. M., Teague, L. G., Padilla, S. M., Bacys, K. R., & Hevesi, K. (2023). Description of and Relationships among Potential Variables Supported for the Diagnosis of Delayed Ejaculation. Sexes, 4(1), 40-54. https://doi.org/10.3390/sexes4010005







